Assessment of Periodontitis Risk Factors in Endodontically Treated Teeth: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ricucci, D.; Loghin, S.; Siqueira, J.F., Jr. Correlation between clinical and histologic pulp diagnoses. J. Endod. 2014, 40, 1932–1939. [Google Scholar] [CrossRef] [PubMed]
- Rossi-Fedele, G.; Ng, Y.L. Effectiveness of root canal treatment for vital pulps compared with necrotic pulps in the presence or absence of signs of periradicular pathosis: A systematic review and meta-analysis. Int. Endod. J. 2023, 56 (Suppl. S3), 370–394. [Google Scholar] [CrossRef] [PubMed]
- Gomes, B.P.F.A.; Herrera, D.R. Etiologic role of root canal infection in apical periodontitis and its relationship with clinical symptomatology. Braz. Oral Res. 2018, 32 (Suppl. S1), e69. [Google Scholar] [CrossRef] [PubMed]
- Josic, U.; Mazzitelli, C.; Maravic, T.; Fidler, A.; Breschi, L.; Mazzoni, A. Biofilm in Endodontics: In Vitro Cultivation Possibilities, Sonic-, Ultrasonic- and Laser-Assisted Removal Techniques and Evaluation of the Cleaning Efficacy. Polymers 2022, 14, 1334. [Google Scholar] [CrossRef] [PubMed]
- Guo, H.J.; Wang, J.D. Bacterial biofilm on the apical external root surfaces of human teeth associated with chronic periradicular lesions. J. Peking Univ. Health Sci. 2009, 41, 571–574. [Google Scholar]
- Leonardo, M.R.; Rossi, M.A.; Silva, L.A.; Ito, I.Y.; Bonifácio, K.C. EM evaluation of bacterial biofilm and microorganisms on the apical external root surface of human teeth. J. Endod. 2002, 28, 815–818. [Google Scholar] [CrossRef]
- Karamifar, K.; Tondari, A.; Saghiri, M.A. Endodontic Periapical Lesion: An Overview on the Etiology, Diagnosis and Current Treatment Modalities. Eur. Endod. J. 2020, 5, 54. [Google Scholar] [CrossRef]
- Abusrewil, S.; Alshanta, O.A.; Albashaireh, K.; Alqahtani, S.; Nile, C.J.; Scott, J.A.; McLean, W. Detection, treatment and prevention of endodontic biofilm infections: What’s new in 2020? Crit. Rev. Microbiol. 2020, 46, 194–212. [Google Scholar] [CrossRef]
- Jurič, I.B.; Anić, I. The Use of Lasers in Disinfection and Cleanliness of Root Canals: A Review. Acta Stomatol. Croat. 2014, 48, 6–15. [Google Scholar] [CrossRef]
- Giuroiu, C.L.; Andrian, S.; Stoleriu, S.; Scurtu, M.; Tanculescu, O.; Poroch, V.; Salceanu, M. The combination of diode laser and ozonated water in the treatment of complicated pulp gangrene. Appl. Sci. 2020, 10, 4203. [Google Scholar] [CrossRef]
- Aminov, L.; Moscalu, M.; Melian, A.; Salceanu, M.; Hamburda, T.; Vataman, M. Clinical-radiological study on the role of biostimulating materials in iatrogenic furcation lesions. Rev. Med. Chir. Soc. Med. Nat. Iasi 2012, 116, 907–913. [Google Scholar]
- Corbella, S.; Walter, C.; Tsesis, I. Effectiveness of root resection techniques compared with root canal retreatment or apical surgery for the treatment of apical periodontitis and tooth survival: A systematic review. Int. Endod. J. 2023, 56 (Suppl. S3), 487–498. [Google Scholar] [CrossRef] [PubMed]
- Budacu, C.; Cioranu, S.V.I.; Chiscop, I.; Salceanu, M.; Melian, A. Apicoectomy—Endodontical surgical procedure. Rev. Chim. 2017, 68, 2654–2657. [Google Scholar] [CrossRef]
- Uraba, S.; Ebihara, A.; Komatsu, K.; Ohbayashi, N.; Okiji, T. Ability of cone-beam computed tomography to detect periapical lesions that were not detected by periapical radiography: A retrospective assessment according to tooth group. J. Endod. 2016, 42, 1186–1190. [Google Scholar] [CrossRef] [PubMed]
- Song, M.; Kim, H.C.; Lee, W.; Kim, E. Analysis of the cause of failure in nonsurgical endodontic treatment by microscopic inspection during endodontic microsurgery. J. Endod. 2011, 37, 1516–1519. [Google Scholar] [CrossRef] [PubMed]
- Holland, R.; Gomes Filho, J.E.; Cintra, L.T.A.; Queiroz, Í.O.D.A.; Estrela, C. Factors affecting the periapical healing process of endodontically treated teeth. J. Appl. Oral Sci. 2017, 25, 465–476. [Google Scholar] [CrossRef]
- Fransson, H.; Dawson, V. Tooth survival after endodontic treatment. Int. Endod. J. 2023, 56 (Suppl. S2), 140–153. [Google Scholar] [CrossRef]
- Rawski, A.A.; Brehmer, B.; Knutsson, K.; Petersson, K.; Reit, C.; Rohlin, M. The major factors that influence endodontic retreatment decisions. Swed. Dent. J. 2003, 27, 23–29. [Google Scholar]
- Gulabivala, K.; Ng, Y.L. Factors that affect the outcomes of root canal treatment and retreatment-A reframing of the principles. Int. Endod. J. 2023, 56 (Suppl. S2), 82–115. [Google Scholar] [CrossRef]
- Ricucci, D.; Siqueira, J.F., Jr. Biofilms and apical periodontitis: Study of prevalence and association with clinical and histopathologic findings. J. Endod. 2010, 36, 1277–1288. [Google Scholar] [CrossRef]
- Bürklein, S.; Schäfer, E.; Jöhren, H.P.; Donnermeyer, D. Quality of root canal fillings and prevalence of apical radiolucencies in a German population: A CBCT analysis. Clin. Oral Investig. 2020, 24, 1217–1227. [Google Scholar] [CrossRef]
- Tibúrcio-Machado, C.S.; Michelon, C.; Zanatta, F.B.; Gomes, M.S.; Marin, J.A.; Bier, C.A. The global prevalence of apical periodontitis: A systematic review and meta-analysis. Int. Endod. J. 2021, 54, 712–735. [Google Scholar] [CrossRef] [PubMed]
- Chala, S.; Abouqal, R.; Abdallaoui, F. Prevalence of apical periodontitis and factors associated with the periradicular status. Acta Odontol. Scand. 2011, 69, 355–359. [Google Scholar] [CrossRef]
- Jakovljevic, A.; Nikolic, N.; Jacimovic, J.; Pavlovic, O.; Milicic, B.; Beljic-Ivanovic, K.; Miletic, M.; Andric, M.; Milasin, J. Prevalence of Apical Periodontitis and Conventional Nonsurgical Root Canal Treatment in General Adult Population: An Updated Systematic Review and Meta-Analysis of Cross-Sectional Studies Published between 2012 and 2020. J Endod. 2020, 46, 1371–1386.e8. [Google Scholar] [CrossRef]
- El Ouarti, I.; Chala, S.; Sakout, M.; Abdallaoui, F. Prevalence and risk factors of Apical periodontitis in endodontically treated teeth: Cross-sectional study in an Adult Moroccan subpopulation. BMC Oral Health 2021, 21, 124. [Google Scholar] [CrossRef] [PubMed]
- Prada, I.; Micó-Muñoz, P.; Giner-Lluesma, T.; Micó-Martínez, P.; Collado-Castellano, N.; Manzano-Saiz, A. Influence of microbiology on endodontic failure. Literature review. Med. Oral Patol. Oral Cir. Bucal. 2019, 24, e364–e372. [Google Scholar] [CrossRef]
- Burt, B.A. Definitions of risk. J. Dent. Educ. 2001, 65, 1007–1008. [Google Scholar] [CrossRef] [PubMed]
- Baseri, M.; Radmand, F.; Milani, A.S.; Gavgani, L.F.; Salehnia, F.; Dianat, O. The effect of periapical lesion size on the success rate of different endodontic treatments: A systematic review and meta-analysis. Evid. Based Dent. 2023, 24, 43. [Google Scholar] [CrossRef]
- Iqbal, M.K.; Kim, S. A review of factors influencing treatment planning decisions of single-tooth implants versus preserving natural teeth with nonsurgical endodontic therapy. J. Endod. 2008, 34, 519–529. [Google Scholar] [CrossRef]
- Chugal, N.M.; Clive, J.M.; Spångberg, L.S. Endodontic treatment outcome: Effect of the permanent restoration. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 104, 576–582. [Google Scholar] [CrossRef]
- Orstavik, D.; Kerekes, K.; Eriksen, H.M. The periapical index: A scoring system for radiographic assessment of apical periodontitis. Endod. Dent. Traumatol. 1986, 2, 20–34. [Google Scholar] [CrossRef] [PubMed]
- Nur, B.G.; Ok, E.; Altunsoy, M.; Ağlarci, O.S.; Çolak, M.; Güngör, E. Evaluation of technical quality and periapical health of root-filled teeth by using cone-beam CT. J. Appl. Oral Sci. 2014, 22, 502–508. [Google Scholar] [CrossRef] [PubMed]
- Bergenholtz, G. Assessment of treatment failure in endodontic therapy. J. Oral Rehabil. 2016, 43, 753–758. [Google Scholar] [CrossRef]
- Frisk, F.; Hugosson, A.; Kvist, T. Is apical periodontitis in root filled teeth associated with the type of restoration? Acta Odontol. Scand. 2015, 73, 169–175. [Google Scholar] [CrossRef]
- Hussain, M.A.; Singh, S.K.; Naz, S.; Haque, M.; Shah, H.K.; Singh, A. Predictors of apical periodontitis in root canal treated teeth from an adult Nepalese subpopulation: A cross-sectional study. BMC Oral Health 2024, 24, 400. [Google Scholar] [CrossRef] [PubMed]
- Estrela, C.; Holland, R.; Estrela, C.R.; Alencar, A.H.; Sousa-Neto, M.D.; Pécora, J.D. Characterization of successful root canal treatment. Braz. Dent. J. 2014, 25, 3–11. [Google Scholar] [CrossRef]
- Godiny, M.; Jalali, S.K.; Khavid, A.; Fatahy, A. Simulated Evaluation of Tooth Fracture Resistance during Instrumentation with Single-and Multi-file Rotary Systems. Iran. Endod. J. 2021, 16, 232–237. [Google Scholar]
- Sequeira-Byron, P.; Fedorowicz, Z.; Carter, B.; Nasser, M.; Alrowaili, E.F. Single crowns versus conventional fillings for the restoration of root-filled teeth. Cochrane Database Syst. Rev. 2015, 2015, CD009109. [Google Scholar] [CrossRef]
- Tiron, B.; Forna, N.; Topoliceanu, C.; Ghiorghe, A.; Stoleriu, S.; Pancu, G.; Nica, I.; Georgescu, A.; Brânzan, R.; Iovan, G. Assessment of factors influencing the esthetic, functional and biological status of posterior composite resins restorations. Rom. J. Oral Rehabil. 2023, 15, 29–41. [Google Scholar]
- Pancu, G.; Georgescu, A.; Moldovanu, A.; Ghiorghe, A.; Stoleriu, S.; Nica, I.; Tărăboanţă, I.; Iovan, A.; Andrian, S.; Topoliceanu, C. Non-intervention versus repair/replacement decisions in posterior composite restorations aged 3–5 years: A retrospective study. Rom. J. Oral Rehabil. 2024, 16, 186–195. [Google Scholar]
- Dawson, V.S.; Petersson, K.; Wolf, E.; Åkerman, S. Periapical Status of Root-filled Teeth Restored with Composite, Amalgam, or Full Crown Restorations: A Cross-sectional Study of a Swedish Adult Population. J. Endod. 2016, 42, 1326–1333. [Google Scholar] [CrossRef] [PubMed]
- Boucher, Y.; Matossian, L.; Rilliard, F.; Machtou, P. Radiographic evaluation of the prevalence and technical quality of root canal treatment in a French subpopulation. Int. Endod. J. 2002, 35, 229–238. [Google Scholar] [CrossRef]
- Ferreira, M.L.; Buligon, M.P.; Sfreddo, C.S.; Liedke, G.S.; Morgental, R.D. Factors related to apical periodontitis in a southern Brazilian population: A multilevel analysis. Braz. Oral Res. 2022, 36, e112. [Google Scholar] [CrossRef]
- Suzuki, P.; de Souza, V.; Holland, R.; Gomes-Filho, J.E.; Murata, S.S.; Dezan Junior, E.; Passos, T.R. Tissue reaction to Endométhasone sealer in root canal fillings short of or beyond the apical foramen. J. Appl. Oral Sci. 2011, 19, 511–516. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Suzuki, P.; de Souza, V.; Holland, R.; Murata, S.S.; Gomes-Filho, J.E.; Dezan Junior, E.; Rodrigues Dos Passos, T. Tissue reaction of the EndoREZ in root canal fillings short of or beyond an apical foramen-like communication. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 109, e94–e99. [Google Scholar] [CrossRef] [PubMed]
- Alves Dos Santos, G.N.; Faria-E-Silva, A.L.; Ribeiro, V.L.; Pelozo, L.L.; Candemil, A.P.; Oliveira, M.L.; Lopes-Olhê, F.C.; Mazzi-Chaves, J.F.; Sousa-Neto, M.D. Is the quality of root canal filling obtained by cone-beam computed tomography associated with periapical lesions? A systematic review and meta-analysis. Clin. Oral Investig. 2022, 26, 5105–5116. [Google Scholar] [CrossRef]
- Ali, A.H.; Mahdee, A.F.; Fadhil, N.H.; Shihab, D.M. Prevalence of periapical lesions in non-endodontically and endodontically treated teeth in an urban Iraqi adult subpopulation: A retrospective CBCT analysis. J. Clin. Exp. Dent. 2022, 14, e953–e958. [Google Scholar] [CrossRef] [PubMed]
- Meirinhos, J.; Martins, J.; Pereira, B.; Baruwa, A.; Gouveia, J.; Quaresma, S.; Monroe, A.; Ginjeira, A. Prevalence of apical periodontitis and its association with previous root canal treatment, root canal filling length and type of coronal restoration—A cross-sectional study. Int. Endod. J. 2020, 53, 573–584. [Google Scholar] [CrossRef] [PubMed]
- Keratiotis, G.; Spineli, L.; De Bruyne, M.A.A.; De Moor, R.J.G.; Meire, M.A. A 22-year follow-up cross-sectional study on periapical health in relation to the quality of root canal treatment in a Belgian population. Int. Endod. J. 2024, 57, 533–548. [Google Scholar] [CrossRef]
- Song, M.; Park, M.; Lee, C.Y.; Kim, E. Periapical status related to the quality of coronal restorations and root fillings in a Korean population. J. Endod. 2014, 40, 182–186. [Google Scholar] [CrossRef]
- Nascimento, E.H.L.; Gaêta-Araujo, H.; Andrade, M.F.S.; Freitas, D.Q. Prevalence of technical errors and periapical lesions in a sample of endodontically treated teeth: A CBCT analysis. Clin. Oral Investig. 2018, 22, 2495–2503. [Google Scholar] [CrossRef] [PubMed]
- Di Filippo, G.; Sidhu, S.; Chong, B. Apical periodontitis and the technical quality of root canal treatment in an adult sub-population in London. Br. Dent. J. 2014, 216, E22. [Google Scholar] [CrossRef] [PubMed]
- Kalender, A.; Orhan, K.; Aksoy, U.; Basmaci, F.; Er, F.; Alankus, A. Influence of the quality of endodontic treatment and coronal restorations on the prevalence of apical periodontitis in a Turkish Cypriot population. Med. Princ. Pract. 2013, 22, 173–177. [Google Scholar] [CrossRef] [PubMed]
- Jersa, I.; Kundzina, R. Periapical status and quality of root fillings in a selected adult Riga population. Stomatologija 2013, 15, 73–77. [Google Scholar]
- Gillen, B.M.; Looney, S.W.; Gu, L.S.; Loushine, B.A.; Weller, R.N.; Loushine, R.J.; Pashley, D.H.; Tay, F.R. Impact of the quality of coronal restoration versus the quality of root canal fillings on success of root canal treatment: A systematic review and meta-analysis. J. Endod. 2011, 37, 895–902. [Google Scholar] [CrossRef]
- Nicolae, V.; Neamtu, B.; Picu, O.; Stefanache, M.A.M.; Cioranu, V.S.I. The comparative evaluation of salivary biomarkers (Calcium, Phosphate, Salivary pH) in Cario-resistance versus Cario-activity. Rev. Chim. 2016, 67, 821–824. [Google Scholar]
- Popa, C.G.; Luchian, I.; Ioanid, N.; Goriuc, A.; Martu, I.; Bosinceanu, D.; Martu, M.A.; Tirca, T.; Martu, S. ELISA Evaluation of RANKL Levels in Gingival Fluid in Patients with Periodontitis and Occlusal Trauma. Rev. Chim. 2018, 69, 1578–1580. [Google Scholar] [CrossRef]
- Cristea, I.; Agop-Forna, D.; Martu, M.-A.; Dascălu, C.; Topoliceanu, C.; Török, R.; Török, B.; Bardis, D.; Bardi, P.M.; Forna, N. Oral and Periodontal Risk Factors of Prosthetic Success for 3-Unit Natural Tooth-Supported Bridges versus Implant-Supported Fixed Dental Prostheses. Diagnostics 2023, 13, 852. [Google Scholar] [CrossRef]
- Solomon, S.M.; Timpu, D.; Forna, D.A.; Stefanache, M.A.; Martu, S.; Stoleriu, S. AFM comparative study of root surface morphology after three methods of scaling. Mater. Plast. 2016, 53, 546–549. [Google Scholar]
- Solomon, S.M.; Stoleriu, S.; Agop Forna, D.; Timpu, D.; Martu Stefanache, M.A.; Ursarescu, I.G.; Martu, S. The quantitative and qualitative assessment of dental substance loss as consequence of root planing by three different techniques. Mater. Plast. 2016, 53, 305–307. [Google Scholar]
- Mârtu, S.; Amalinei, C.; Tatarciuc, M.; Rotaru, M.; Potârnichie, O.; Liliac, L.; Caruntu, I.D. Healing process and laser therapy in the superficial periodontium: A histological study. Rom. J. Morphol. Embryol. 2012, 53, 111–116. [Google Scholar] [PubMed]
- Martu, M.-A.; Luchian, I.; Mares, M.; Solomon, S.; Ciurcanu, O.; Danila, V.; Rezus, E.; Foia, L. The Effectiveness of Laser Applications and Photodynamic Therapy on Relevant Periodontal Pathogens (Aggregatibacter actinomycetemcomitans) Associated with Immunomodulating Anti-Rheumatic Drugs. Bioengineering 2023, 10, 61. [Google Scholar] [CrossRef]
- Nicolae, V.D.; Chiscop, I.; Cioranu, V.S.I.; Mârțu, M.-A.; Luchian, A.I.; Mârțu, S.; Solomon, S.M. The use of photoactivated blue-O toluidine for periimplantitis treatment in patients with periodontal disease. Rev. Chim. 2016, 66, 2121–2123. [Google Scholar]
- Martu, M.-A.; Maftei, G.-A.; Luchian, I.; Stefanescu, O.M.; Scutariu, M.M.; Solomon, S.M. The Effect of Acknowledged and Novel Anti-Rheumatic Therapies on Periodontal Tissues—A Narrative Review. Pharmaceuticals 2021, 14, 1209. [Google Scholar] [CrossRef]
- Budala, D.G.; Martu, M.-A.; Maftei, G.-A.; Diaconu-Popa, D.A.; Danila, V.; Luchian, I. The Role of Natural Compounds in Optimizing Contemporary Dental Treatment—Current Status and Future Trends. J. Funct. Biomater. 2023, 14, 273. [Google Scholar] [CrossRef]
- Sufaru, I.-G.; Martu, M.-A.; Luchian, I.; Stoleriu, S.; Diaconu-Popa, D.; Martu, C.; Teslaru, S.; Pasarin, L.; Solomon, S.M. The Effects of 810 nm Diode Laser and Indocyanine Green on Periodontal Parameters and HbA1c in Patients with Periodontitis and Type II Diabetes Mellitus: A Randomized Controlled Study. Diagnostics 2022, 12, 1614. [Google Scholar] [CrossRef] [PubMed]
- Martu, M.-A.; Surlin, P.; Lazar, L.; Maftei, G.A.; Luchian, I.; Gheorghe, D.-N.; Rezus, E.; Toma, V.; Foia, L.-G. Evaluation of Oxidative Stress before and after Using Laser and Photoactivation Therapy as Adjuvant of Non-Surgical Periodontal Treatment in Patients with Rheumatoid Arthritis. Antioxidants 2021, 10, 226. [Google Scholar] [CrossRef]
- Anton, D.-M.; Martu, M.-A.; Maris, M.; Maftei, G.-A.; Sufaru, I.-G.; Tatarciuc, D.; Luchian, I.; Ioanid, N.; Martu, S. Study on the Effects of Melatonin on Glycemic Control and Periodontal Parameters in Patients with Type II Diabetes Mellitus and Periodontal Disease. Medicina 2021, 57, 140. [Google Scholar] [CrossRef]
- Stassen, I.G.; Hommez, G.M.; De Bruyn, H.; De Moor, R.J. The relation between apical periodontitis and root-filled teeth in patients with periodontal treatment need. Int. Endod. J. 2006, 39, 299–308. [Google Scholar] [CrossRef]
- Ruiz, X.F.; Duran-Sindreu, F.; Shemesh, H.; García Font, M.; Vallés, M.; Roig Cayón, M.; Olivieri, J.G. Development of Periapical Lesions in Endodontically Treated Teeth with and without Periodontal Involvement: A Retrospective Cohort Study. J. Endod. 2017, 43, 1246–1249. [Google Scholar] [CrossRef]
- Buligon, M.P.; Marin, J.A.; Wolle, C.F.B.; Liedke, G.S.; Sfreddo, C.S.; Bier, C.A.S.; Moreira, C.H.C.; Morgental, R.D. Apical periodontitis and associated factors in a rural population of southern Brazil: A multilevel analysis. Clin. Oral Investig. 2023, 27, 2887–2897. [Google Scholar] [CrossRef] [PubMed]
- Kato, T.; Fujiwara, N.; Kuraji, R.; Numabe, Y. Relationship between periodontal parameters and non-vital pulp in dental clinic patients: A cross-sectional study. BMC Oral Health 2020, 20, 109. [Google Scholar] [CrossRef]
- Zaharescu, A.; Solomon, S.M.; Luca, M.G.; Toma, V.; Luchian, I.; Sufaru, I.G.; Martu, S. Quantification of proinflammatory molecules (IL1-α, IL1-β, IL2, IL12, IFN-γ, TNF-α) in crevicular fluid and serum in patients with endo-periodontal lesions. Rev. Chim. 2019, 70, 2252–2255. [Google Scholar] [CrossRef]
- Martu, C.; Martu, M.-A.; Maftei, G.-A.; Diaconu-Popa, D.A.; Radulescu, L. Odontogenic Sinusitis: From Diagnosis to Treatment Possibilities—A Narrative Review of Recent Data. Diagnostics 2022, 12, 1600. [Google Scholar] [CrossRef] [PubMed]
- Nardi, C.; Calistri, L.; Grazzini, G.; Desideri, I.; Lorini, C.; Occhipinti, M.; Mungai, F.; Colagrande, S. Is Panoramic Radiography an Accurate Imaging Technique for the Detection of Endodontically Treated Asymptomatic Apical Periodontitis? J. Endod. 2018, 44, 1500–1508. [Google Scholar] [CrossRef] [PubMed]
- Antohi, C.; Salceanu, M.; Aminov, L.; Martu, M.-A.; Dascalu, C.G.; Dodi, G.; Stoica, G.; Bandol, G.; Iancu, D.; Dobrovat, B.; et al. Assessment of Systemic and Maxillary Bone Loss in Cancer Patients with Endo-Periodontal Lesions Using Dkk-1 Biomarker and Dental Radiological Examinations. Appl. Sci. 2022, 12, 5235. [Google Scholar] [CrossRef]
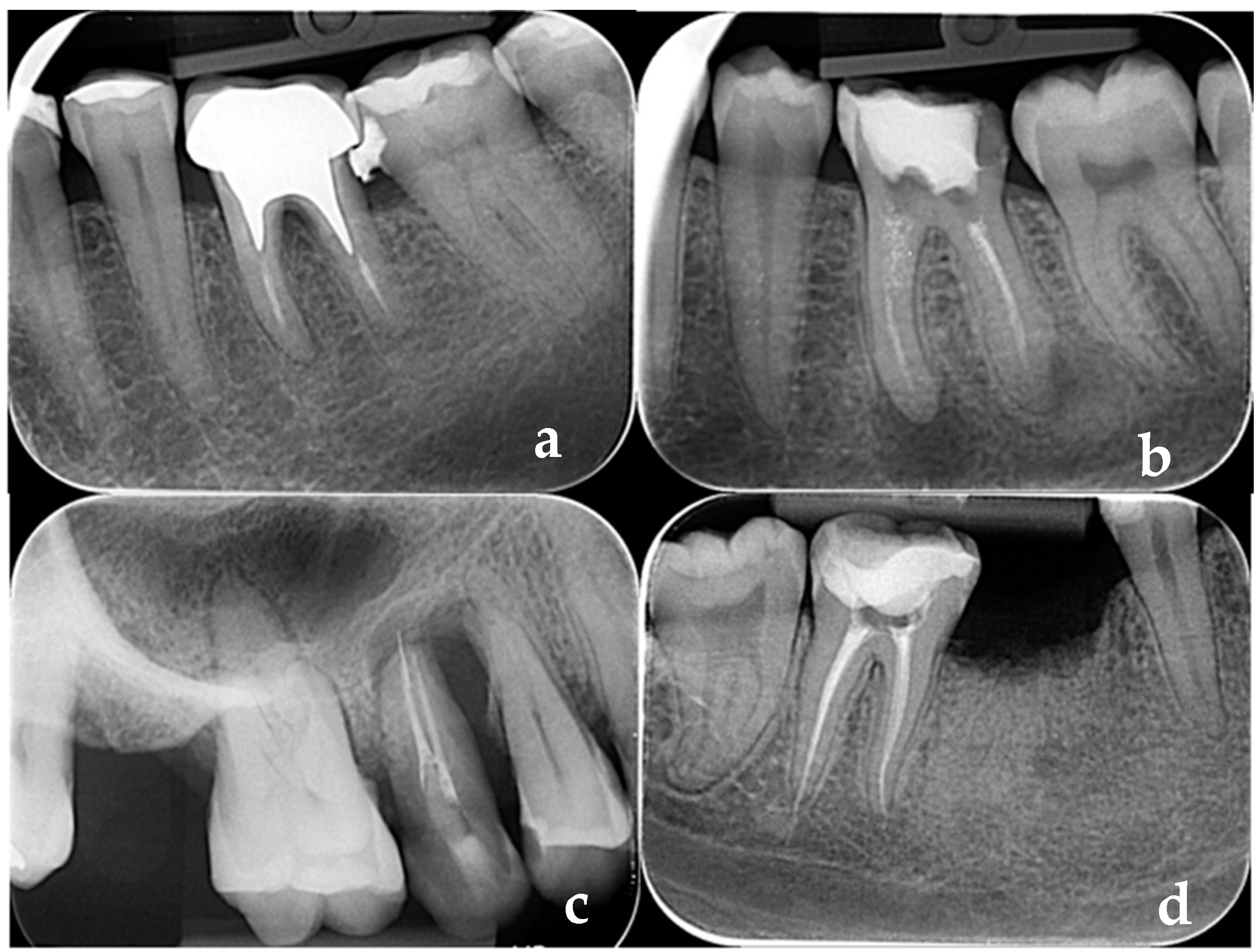
- Sălceanu, M.; Vataman, M.; Aminov, L.; Giuroiu, C.; Topoliceanu, C.; Decolli, Y.; Ghiorghe, C.-A.; Melian, A. Diagnosis and follow-up of the periapical lesions in the non-surgical endodontic treatment: A CBCT study. Rom. J. Oral Rehabil. 2017, 9, 32–36. [Google Scholar]
- Leonardi Dutra, K.; Haas, L.; Porporatti, A.L.; Flores-Mir, C.; Nascimento Santos, J.; Mezzomo, L.A.; Corrêa, M.; De Luca Canto, G. Diagnostic Accuracy of Cone-beam Computed Tomography and Conventional Radiography on Apical Periodontitis: A Systematic Review and Meta-analysis. J. Endod. 2016, 42, 356–364. [Google Scholar] [CrossRef]
- Siqueira Junior, J.F.; Rôças, I.D.N.; Marceliano-Alves, M.F.; Pérez, A.R.; Ricucci, D. Unprepared root canal surface areas: Causes, clinical implications, and therapeutic strategies. Braz. Oral Res. 2018, 32 (Suppl. S1), e65. [Google Scholar] [CrossRef]
- Kazimierczak, W.; Wajer, R.; Wajer, A.; Kiian, V.; Kloska, A.; Kazimierczak, N.; Janiszewska-Olszowska, J.; Serafin, Z. Periapical Lesions in Panoramic Radiography and CBCT Imaging-Assessment of AI’s Diagnostic Accuracy. J. Clin. Med. 2024, 13, 2709. [Google Scholar] [CrossRef]
- Ahmed, H.M.; Cohen, S.; Lévy, G.; Steier, L.; Bukiet, F. Rubber dam application in endodontic practice: An update on critical educational and ethical dilemmas. Aust. Dent. J. 2014, 59, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Zaharescu, A.; Mârțu, I.; Luchian, A.I.; Mârțu, M.A.; Șufaru, I.G.; Mârțu, C.; Solomon, S.M. Role of adjunctive therapy with subantimicrobial doses of doxycycline in glycemic control (HbA1c) in patients with diabetes and endo-periodontal lesions to prevent sinus complications. Exp. Ther. Med. 2021, 21, 277. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Vital Pulp | Necrotic Pulp | Total | p-Value | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Global | 52 | 100.0 | 99 | 100.0 | 151 | 100.0 | |
| Gender | 0.295 | ||||||
| M | 15 | 28.8 | 37 | 37.4 | 52 | 34.4 | |
| F | 37 | 71.2 | 62 | 62.6 | 99 | 65.6 | |
| Age (yrs.) (mean, SD) | Globally: 52.81 ± 18.647 M: 48.67 ± 24.839/F: 54.49 ± 15.577 p = 0.316 | Globally: 46.02 ± 12.326 M: 42.27 ± 12.055/F: 48.26 ± 12.030 p = 0.116 | Globally: 48.36 ± 15.098 M: 44.12 ± 16.748/F: 50.59 ± 13.725 p = 0.012 * | 0.042 * | |||
| Age groups (yrs.) | <0.001 ** | ||||||
| 20–39 | 13 | 25.0 | 28 | 28.3 | 41 | 27.2 | |
| 40–59 | 21 | 40.4 | 63 | 63.6 | 84 | 55.6 | |
| ≥60 | 18 | 34.6 | 8 | 8.1 | 26 | 17.2 | |
| Parameter | Vital Pulp | Necrotic Pulp | Total | p-Value | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Global | 127 | 100.0 | 264 | 100.0 | 391 | 100.0 | |
| Gender | 0.181 | ||||||
| M | 43 | 33.9 | 72 | 27.3 | 115 | 29.4 | |
| F | 84 | 66.1 | 192 | 72.7 | 276 | 70.6 | |
| Age | <0.001 ** | ||||||
| 20–39 yrs. | 32 | 25.2 | 50 | 18.9 | 82 | 21.0 | |
| 40–59 yrs. | 43 | 33.9 | 192 | 72.7 | 235 | 60.1 | |
| ≥60 yrs. | 52 | 40.9 | 22 | 8.3 | 74 | 18.9 | |
| Follow-up (yrs.) (mean ± SD) | 5.16 ± 1.716 | 5.29 ± 1.781 | 5.25 ± 1.759 | 0.863 | |||
| Tooth type | 0.905 | ||||||
| Anterior | 47 | 37.0 | 103 | 39.0 | 150 | 38.4 | |
| Premolar | 38 | 29.9 | 79 | 29.9 | 117 | 29.9 | |
| Molar | 42 | 33.1 | 82 | 31.1 | 124 | 31.7 | |
| Location (MX/MD) | 0.955 | ||||||
| MX | 79 | 62.2 | 165 | 62.5 | 244 | 62.4 | |
| MD | 48 | 37.8 | 99 | 37.5 | 147 | 37.6 | |
| Dental crown restoration | |||||||
| Composite direct restoration | 20 | 15.7 | 72 | 27.3 | 92 | 23.5 | 0.012 * |
| Class Black I | 10 | 50.0 | 20 | 27.8 | 30 | 7.7 | 0.158 |
| Class Black II | 8 | 40.0 | 44 | 61.1 | 52 | 13.3 | |
| Class Black III | 2 | 10.0 | 4 | 5.6 | 6 | 1.5 | |
| Class Black IV | - | - | 4 | 5.6 | 4 | 1.0 | |
| Complete coverage crown | 107 | 84.3 | 192 | 72.7 | 299 | 76.5 | |
| Intracanal posts | 14 | 11.0 | 95 | 36.0 | 109 | 27.9 | <0.001 ** |
| Coronal restoration quality | 0.056 | ||||||
| Adequate | 57 | 44.9 | 92 | 34.8 | 149 | 38.1 | |
| Poor | 70 | 55.1 | 172 | 65.2 | 242 | 61.9 | |
| Root canal filling status | <0.001 ** | ||||||
| Proper | 42 | 33.1 | 42 | 15.9 | 84 | 21.5 | |
| Poor | 85 | 66.9 | 222 | 84.1 | 307 | 78.5 | |
| Short filling | 65 | 51.2 | 159 | 60.2 | 224 | 57.3 | 0.090 |
| Canal overfilling | 14 | 11.0 | 19 | 7.2 | 33 | 8.4 | 0.202 |
| Poor homogeneity | 65 | 51.2 | 200 | 75.8 | 265 | 67.8 | <0.001 ** |
| Inadequate taper (conicity) | 67 | 52.8 | 192 | 72.7 | 259 | 66.2 | <0.001 ** |
| Antagonist tooth | 0.158 | ||||||
| YES | 99 | 78.0 | 188 | 71.2 | 287 | 73.4 | |
| NO | 28 | 22.0 | 76 | 28.8 | 104 | 26.6 | |
| Caries adjacent to restoration | 0.028 * | ||||||
| YES | 66 | 52.0 | 168 | 63.6 | 234 | 59.8 | |
| NO | 61 | 48.0 | 96 | 36.4 | 157 | 40.2 | |
| Periodontal pathology | 0.004 ** | ||||||
| Absent | 54 | 42.5 | 153 | 58.0 | 207 | 52.9 | |
| Present (BOP, PPD ≥ 3 mm) | 73 | 57.5 | 111 | 42.0 | 184 | 47.1 | |
| Endo-periodontal lesions | 0.510 | ||||||
| YES | 2 | 1.6 | 8 | 3.0 | 10 | 2.6 | |
| NO | 125 | 98.4 | 256 | 97.0 | 381 | 97.4 | |
| Periapical status | <0.001 ** | ||||||
| Healthy | 92 | 72.4 | 118 | 44.7 | 210 | 53.7 | |
| Apical periodontitis | 35 | 27.6 | 146 | 55.3 | 181 | 46.3 | |
| Parameters of the Root Canal Fillings | Criteria | Description |
|---|---|---|
| Density | Adequate | Gaps are absent in the canal root filling or at the interface between the root filling and root canal walls |
| Poor | Gaps are present in the canal root filling or at the interface between the root filling and root canal walls | |
| Length | Adequate | Root filling ends below 2 mm from the radiographic apex |
| Poor | Root filling extends over the radiographic apex or ends > 2 mm from the radiographic apex | |
| Taper (conicity) | Adequate | Root canal preparation is continuously tapered, being funneled from the canal entrance to the apex, while the cross-sectional diameter is narrower at every point apically |
| Poor | Taper (conicity) is inconsistent from the canal entrance to the apical part, or root filling was deviated from the original canal | |
| Parameters of the tooth crown restoration | ||
| Adequate | Permanent direct or indirect restoration with an intact radiographic aspect | |
| Poor | Permanent direct or indirect restoration with visible signs of caries adjacent to restoration, open margins, or the presence of temporary coronal restoration | |
| Missing | Absence of direct or indirect coronal restoration |
| Group A—VITAL PULP | AP | p-Value * | |||
|---|---|---|---|---|---|
| Parameter | Present | Absent | |||
| N | % | N | % | ||
| Gender | 0.232 | ||||
| M | 9 | 20.9 | 34 | 79.1 | |
| F | 26 | 31.0 | 58 | 69.0 | |
| Age | 0.795 | ||||
| 20–39 yrs. | 8 | 25.0 | 24 | 75.0 | |
| 40–59 yrs. | 11 | 25.6 | 32 | 74.4 | |
| ≥60 yrs. | 16 | 30.8 | 36 | 69.2 | |
| Follow-up | 0.238 | ||||
| 2–4 yrs. | 12 | 35.3 | 22 | 64.7 | |
| 5–8 yrs | 23 | 24.7 | 70 | 75.3 | |
| Tooth type | 0.111 | ||||
| Anterior | 17 | 36.2 | 30 | 63.8 | |
| Premolar | 6 | 15.8 | 32 | 84.2 | |
| Molar | 12 | 28.6 | 30 | 71.4 | |
| Location (MX/MD) | 0.752 | ||||
| MX | 21 | 26.6 | 58 | 73.4 | |
| MD | 14 | 29.2 | 34 | 70.8 | |
| Dental crown restoration | 0.014 * | ||||
| Composite direct restoration | 10 | 50.0 | 10 | 50.0 | |
| Complete coverage crown | 25 | 23.4 | 82 | 76.6 | |
| Composite direct restoration | 0.111 | ||||
| Class Black I | 6 | 60.0 | 4 | 40.0 | |
| Class Black II | 2 | 25.0 | 6 | 75.0 | |
| Class Black III | 2 | 100.0 | - | - | |
| Class Black IV | - | - | - | - | |
| Intracanal posts | 2 | 14.3 | 12 | 85.7 | 0.347 |
| Coronal marginal sealing | 0.007 ** | ||||
| Adequate | 9 | 15.8 | 48 | 84.2 | |
| Poor | 26 | 37.1 | 44 | 62.9 | |
| Root canal filling status | <0.001 ** | ||||
| Proper | - | - | 42 | 100.0 | |
| Poor | 35 | 41.2 | 50 | 58.8 | |
| Short filling | 23 | 35.4 | 42 | 64.6 | 0.043 * |
| Canal overfilling | 10 | 71.4 | 4 | 28.6 | <0.001 ** |
| Poor homogeneity | 33 | 50.8 | 32 | 49.2 | <0.001 ** |
| Inadequate taper (conicity) | 29 | 43.3 | 38 | 56.7 | <0.001 ** |
| Antagonist tooth | 0.040 * | ||||
| YES | 23 | 23.2 | 76 | 76.8 | |
| NO | 12 | 42.9 | 16 | 57.1 | |
| Caries adjacent to restoration | <0.001 ** | ||||
| YES | 28 | 42.4 | 38 | 57.6 | |
| NO | 7 | 11.5 | 54 | 88.5 | |
| Periodontal pathology | <0.001 ** | ||||
| Absent | 4 | 7.4 | 50 | 92.6 | |
| Present (BOP, PPD ≥3 mm) | 31 | 42.5 | 42 | 57.5 | |
| Endo-periodontal lesions | 0.074 | ||||
| YES | 2 | 100.0 | - | - | |
| NO | 33 | 26.4 | 92 | 73.6 | |
| Group B—NECROTIC PULP | PAC | p-value * | |||
| Parameter | Present | Absent | |||
| N | % | N | % | ||
| Gender | 0.613 | ||||
| M | 38 | 52.8 | 34 | 47.2 | |
| F | 108 | 56.3 | 84 | 43.8 | |
| Age | 0.024 * | ||||
| 20–39 yrs. | 24 | 48.0 | 26 | 52.0 | |
| 40–59 yrs. | 104 | 54.2 | 88 | 45.8 | |
| ≥60 yrs. | 18 | 81.8 | 4 | 18.2 | |
| Follow-up | 0.072 | ||||
| 2–4 yrs | 68 | 61.8 | 42 | 38.2 | |
| 5–8 yrs | 78 | 50.6 | 76 | 49.4 | |
| Tooth type | 0.046 * | ||||
| Anterior | 59 | 57.3 | 44 | 42.7 | |
| Premolar | 35 | 44.3 | 44 | 55.7 | |
| Molar | 52 | 63.4 | 30 | 36.6 | |
| Location (MX/MD) | 0.110 | ||||
| MX | 85 | 51.5 | 80 | 48.5 | |
| MD | 61 | 61.6 | 38 | 38.4 | |
| Coronal restoration type | 0.289 | ||||
| Composite direct restoration | 36 | 50.0 | 36 | 50.0 | |
| Complete coverage crown | 110 | 57.3 | 82 | 42.7 | |
| Direct composite restoration | 0.225 | ||||
| Class Black I | 10 | 50.0 | 10 | 50.0 | |
| Class Black II | 24 | 54.5 | 20 | 45.5 | |
| Class Black III | 2 | 50.0 | 2 | 50.0 | |
| Class Black IV | - | - | 4 | 100.0 | |
| Intracanal posts | 63 | 66.3 | 32 | 33.7 | 0.007 ** |
| Coronal marginal sealing | <0.001** | ||||
| Adequate | 36 | 39.1 | 56 | 60.9 | |
| Poor | 110 | 64.0 | 62 | 36.0 | |
| Root canal filling status | <0.001 ** | ||||
| Proper | 12 | 28.6 | 30 | 71.4 | |
| Poor | 134 | 60.4 | 88 | 39.6 | |
| Short filling | 101 | 63.5 | 58 | 36.5 | <0.001 ** |
| Canal overfilling | 19 | 100.0 | - | - | <0.001 ** |
| Poor homogeneity | 126 | 63.0 | 74 | 37.0 | <0.001 ** |
| Inadequate taper (conicity) | 122 | 63.5 | 70 | 36.5 | <0.001 ** |
| Antagonist tooth | 0.579 | ||||
| YES | 106 | 56.4 | 82 | 43.6 | |
| NO | 40 | 52.6 | 36 | 47.4 | |
| Caries adjacent to restoration | 0.019 * | ||||
| YES | 102 | 60.7 | 66 | 39.3 | |
| NO | 44 | 45.8 | 52 | 54.2 | |
| Periodontal pathology | <0.001 ** | ||||
| Absent | 63 | 41.2 | 90 | 58.8 | |
| Present (BOP, PPD ≥ 3 mm) | 83 | 74.8 | 28 | 25.2 | |
| Endo-periodontal lesions | 0.009 ** | ||||
| YES | 8 | 100.0 | - | - | |
| NO | 138 | 53.9 | 118 | 46.1 | |
| Group A—VITAL PULP Parameter | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| Dental crown restoration | ||||||
| Composite direct restoration | 1 | |||||
| Complete coverage crown | 3.280 | 1.226 ÷ 8.777 | 0.014 * | 0.000 | - | 0.990 |
| Coronal marginal sealing | ||||||
| Adequate | 1 | |||||
| Poor | 3.152 | 1.332 ÷ 7.458 | 0.007 ** | 0.000 | - | 0.989 |
| Root canal filling status | - | |||||
| Proper | ||||||
| Poor | - | <0.001 ** | 0.147 | - | 1.000 | |
| Short filling | 2.282 | 1.015 ÷ 5.127 | 0.043 * | 3.185 × 1014 | - | 0.999 |
| Canal overfilling | 8.800 | 2.542 ÷ 30.461 | <0.001 ** | 1.800 × 1031 | - | 0.999 |
| Poor homogeneity | 30.938 | 6.970 ÷ 137.324 | <0.001 ** | 5.082 × 1050 | - | 0.989 |
| Inadequate taper (conicity) | 6.868 | 2.598 ÷ 18.156 | <0.001 ** | 0.000 | - | 0.999 |
| Antagonist tooth | ||||||
| NO | 1 | |||||
| YES | 2.478 | 1.026 ÷ 5.986 | 0.040 * | 3.554 × 107 | - | 0.995 |
| Caries adjacent to restoration | ||||||
| Absent | 1 | |||||
| Present | 5.684 | 2.251 ÷ 14.355 | <0.001 ** | 0.000 | - | 0.996 |
| Periodontal pathology | ||||||
| Absent | 1 | |||||
| Present (BOP, PPD ≥ 3 mm) | 9.226 | 3.013 ÷ 28.254 | <0.001 ** | 3.873 × 1043 | - | 0.989 |
| Group B—NECROTIC PULP Parameter | Univariate analysis | Multivariate analysis | ||||
| OR | 95% CI | p-value | OR | 95% CI | p-value | |
| Age | ||||||
| 20–39 yrs. | 1 | 1 | 0.047 * | |||
| 40–59 yrs. | 1.280 | 0.687 ÷ 2.388 | 0.437 | 2.159 | 0.856 ÷ 5.442 | 0.103 |
| ≥60 yrs. | 4.875 | 1.443 ÷ 16.466 | 0.007 ** | 6.464 | 1.423 ÷ 29.365 | 0.016 * |
| Tooth type | ||||||
| Premolar | 1 | 1 | 0.014 * | |||
| Anterior | 1.686 | 0.933 ÷ 3.045 | 0.082 | 1.834 | 0.874 ÷ 3.847 | 0.109 |
| Molar | 2.179 | 1.159 ÷ 4.098 | 0.015 * | 3.583 | 1.514 ÷ 8.476 | 0.004 ** |
| Intracanal posts | 2.040 | 1.211 ÷ 3.436 | 0.007 ** | 2.023 | 1.010 ÷ 4.054 | 0.047 * |
| Coronal marginal sealing | ||||||
| Adequate | 1 | 1 | ||||
| Poor | 2.760 | 1.638 ÷ 4.650 | <0.001 ** | 2.684 | 1.096 ÷ 6.572 | 0.031 * |
| Root canal filling status | ||||||
| Proper | 1 | 1 | ||||
| Poor | 3.807 | 1.850 ÷ 7.832 | <0.001 ** | 1.583 | 0.407 ÷ 6.161 | 0.508 |
| Short filling | 2.322 | 1.403 ÷ 3.842 | <0.001 ** | 3.578 | 1.406 ÷ 9.107 | 0.007 ** |
| Canal overfilling | - | - | <0.001 ** | 4.313 × 109 | - | 0.998 |
| Poor homogeneity | 3.746 | 2.053 ÷ 6.836 | <0.001 ** | 1.800 | 0.515 ÷ 6.294 | 0.358 |
| Inadequate taper (conicity) | 3.486 | 1.969 ÷ 6.172 | <0.001 ** | 0.358 | 0.095 ÷ 1.356 | 0.131 |
| Caries adjacent to restoration | ||||||
| Absent | 1 | |||||
| Present | 1.826 | 1.100 ÷ 3.032 | 0.019 * | 0.440 | 0.168 ÷ 1.149 | 0.094 |
| Periodontal pathology | ||||||
| Absent | 1 | |||||
| Present (BOP, PPD ≥ 3 mm) | 4.235 | 2.478 ÷ 7.237 | <0.001 ** | 4.372 | 1.942 ÷ 9.843 | <0.001 ** |
| Endo-periodontal lesions | ||||||
| NO | ||||||
| YES | - | - | 0.009 ** | 1.696 × 108 | 0.000 | 0.999 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sălceanu, M.; Dascălu, C.; Melian, A.; Giuroiu, C.; Antohi, C.; Concita, C.; Hamburda, T.; Topoliceanu, C.; Mârţu, M.-A. Assessment of Periodontitis Risk Factors in Endodontically Treated Teeth: A Cross-Sectional Study. Diagnostics 2024, 14, 1972. https://doi.org/10.3390/diagnostics14171972
Sălceanu M, Dascălu C, Melian A, Giuroiu C, Antohi C, Concita C, Hamburda T, Topoliceanu C, Mârţu M-A. Assessment of Periodontitis Risk Factors in Endodontically Treated Teeth: A Cross-Sectional Study. Diagnostics. 2024; 14(17):1972. https://doi.org/10.3390/diagnostics14171972
Chicago/Turabian StyleSălceanu, Mihaela, Cristina Dascălu, Anca Melian, Cristian Giuroiu, Cristina Antohi, Corina Concita, Tudor Hamburda, Claudiu Topoliceanu, and Maria-Alexandra Mârţu. 2024. "Assessment of Periodontitis Risk Factors in Endodontically Treated Teeth: A Cross-Sectional Study" Diagnostics 14, no. 17: 1972. https://doi.org/10.3390/diagnostics14171972
APA StyleSălceanu, M., Dascălu, C., Melian, A., Giuroiu, C., Antohi, C., Concita, C., Hamburda, T., Topoliceanu, C., & Mârţu, M.-A. (2024). Assessment of Periodontitis Risk Factors in Endodontically Treated Teeth: A Cross-Sectional Study. Diagnostics, 14(17), 1972. https://doi.org/10.3390/diagnostics14171972






