Pathological Characteristics, Management, and Prognosis of Rectal Neuroendocrine Tumors: A Retrospective Study from a Tertiary Hospital
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
3.1. Demographics and Baseline Characteristics
3.2. Diagnostic Work-Up
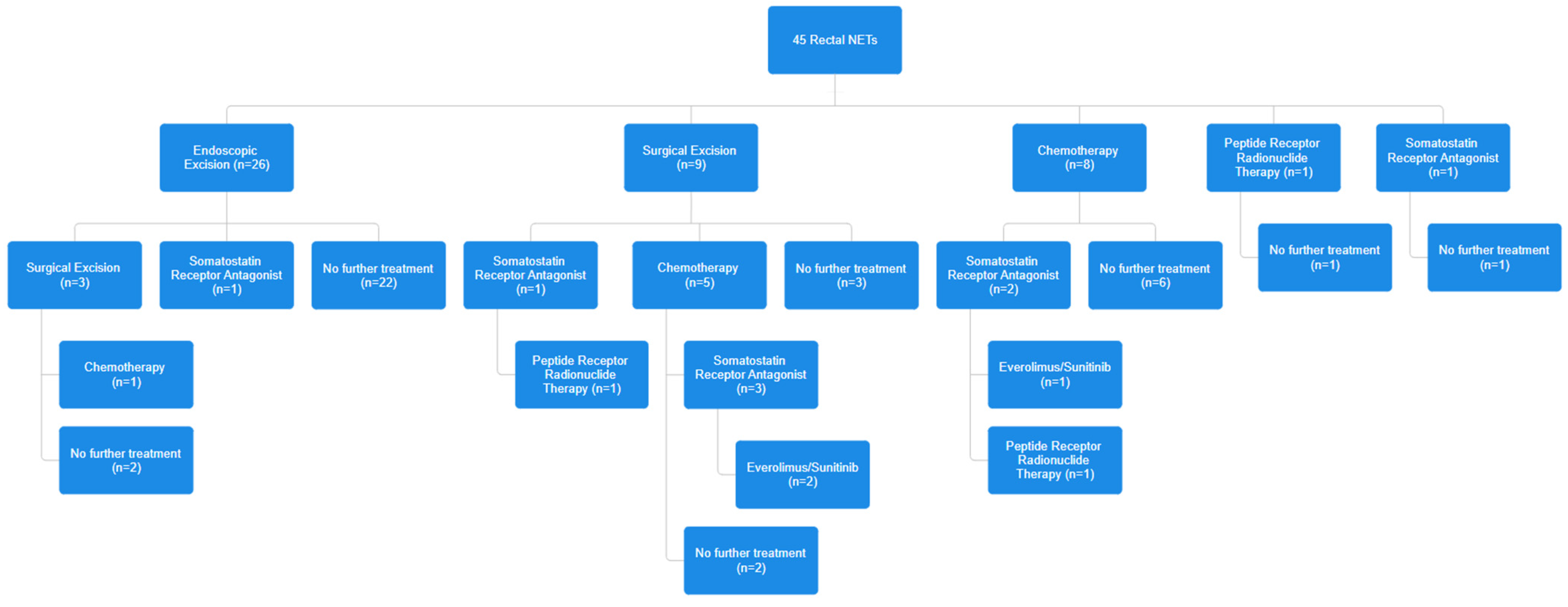
3.3. Individual Patient Management
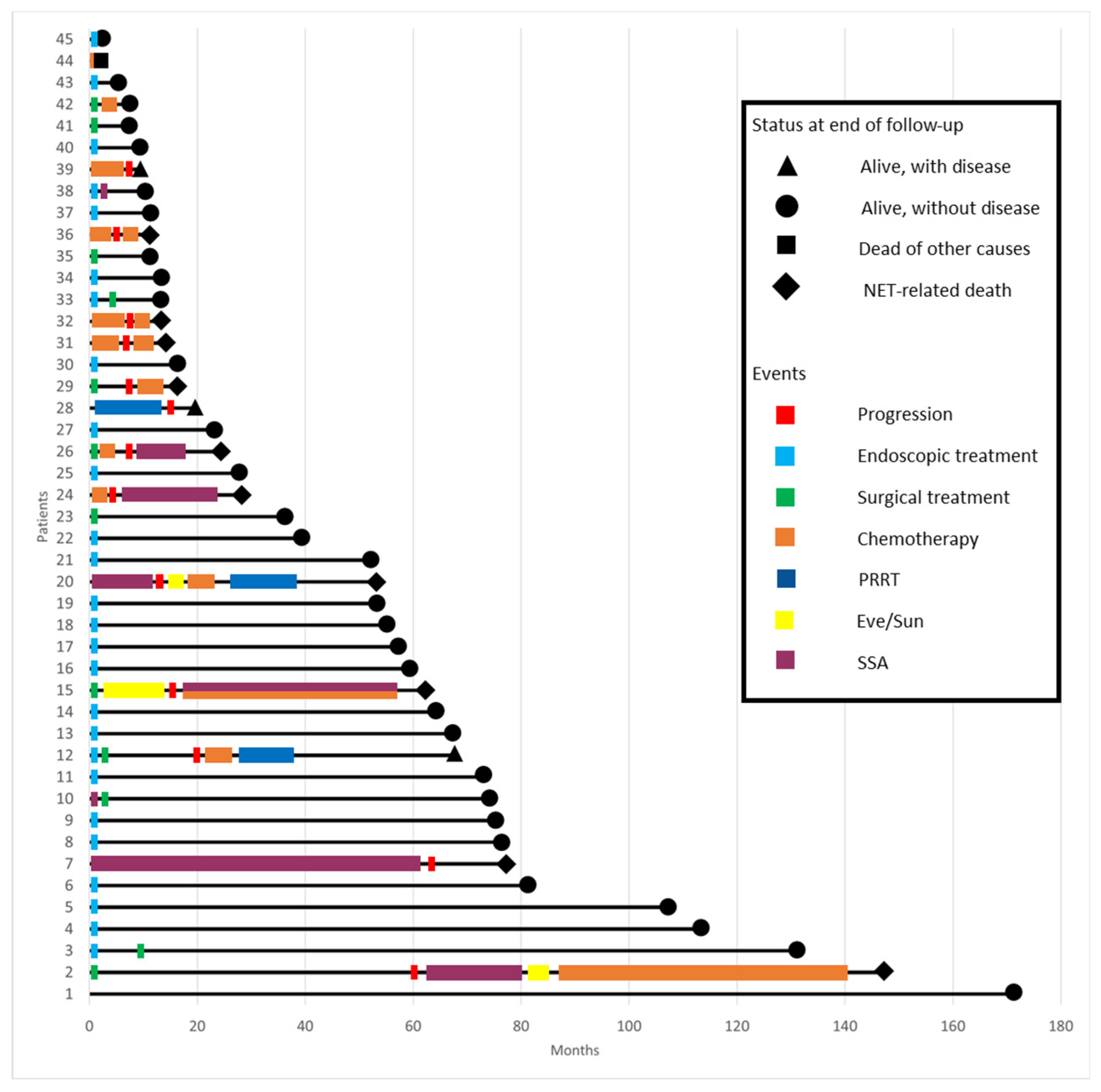
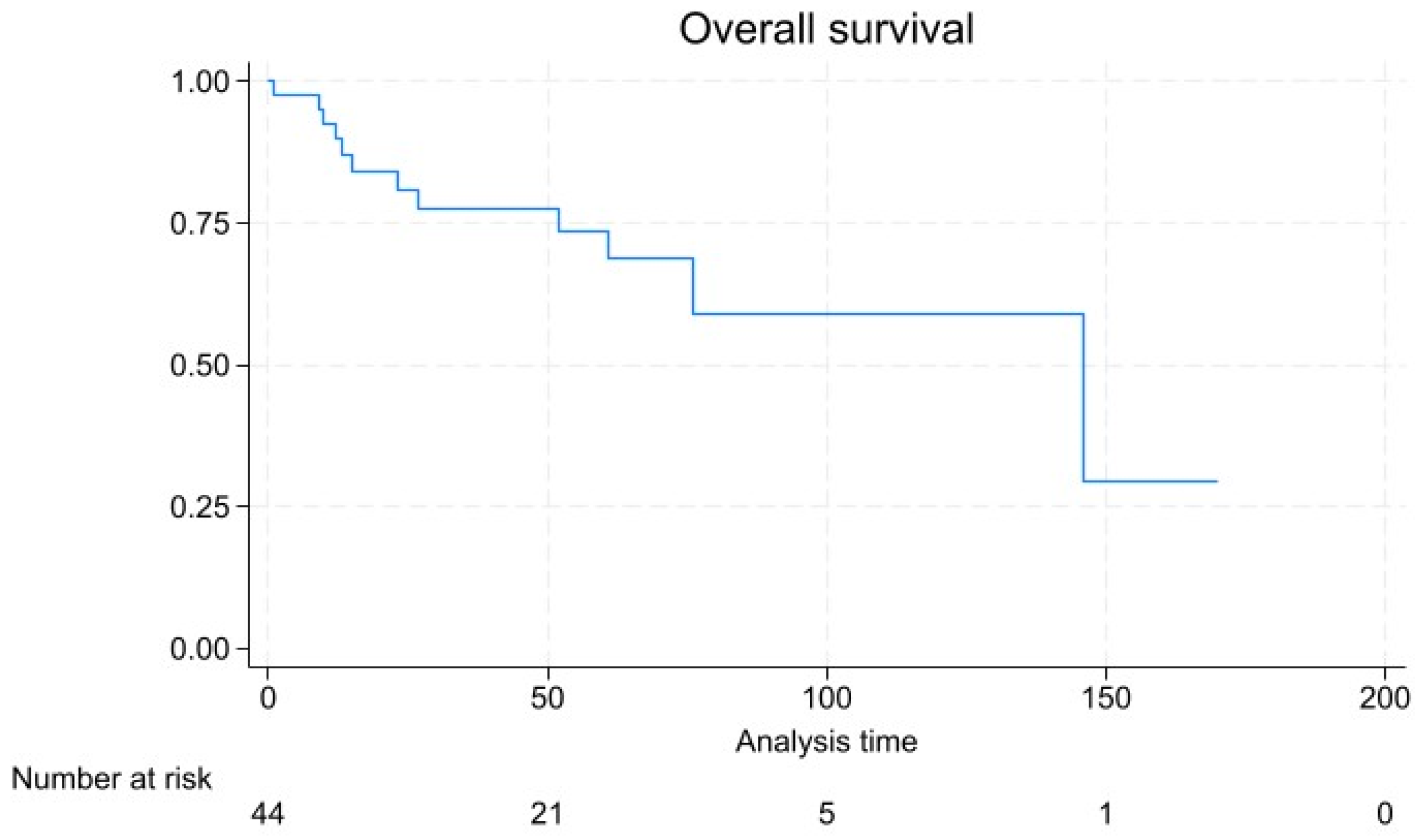
3.4. Patient Outcomes and Survival Analysis
3.5. Risk Factors for Disease Progression
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dasari, A.; Shen, C.; Halperin, D.; Zhao, B.; Zhou, S.; Xu, Y.; Shih, T.; Yao, J.C. Trends in the Incidence, Prevalence, and Survival Outcomes in Patients with Neuroendocrine Tumors in the United States. JAMA Oncol. 2017, 3, 1335–1342. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Maschmeyer, G.; Mügge, L.O.; Kämpfe, D.; Kreibich, U.; Wilhelm, S.; Aßmann, M.; Schwarz, M.; Kahl, C.; Köhler, S.; Grobe, N.; et al. A retrospective review of diagnosis and treatment modalities of neuroendocrine tumors (excluding primary lung cancer) in 10 oncological institutions of the East German Study Group of Hematology and Oncology (OSHO), 2010–2012. J. Cancer Res. Clin. Oncol. 2015, 141, 1639–1644. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, K.; Kojima, M.; Saito, N.; Sakuyama, N.; Koushi, K.; Watanabe, T.; Sugihara, K.; Akimoto, T.; Ito, M.; Ochiai, A. Current status of the histopathological assessment, diagnosis, and reporting of colorectal neuroendocrine tumors: A Web survey from the Japanese Society for Cancer of Colon and Rectum. Pathol. Int. 2016, 66, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Rinke, A.; Ambrosini, V.; Dromain, C.; Garcia-Carbonero, R.; Haji, A.; Koumarianou, A.; van Dijkum, E.N.; O’Toole, D.; Rindi, G.; Scoazec, J.; et al. European Neuroendocrine Tumor Society (ENETS) 2023 guidance paper for colorectal neuroendocrine tumours. J. Neuroendocrinol. 2023, 35, e13309. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.J.; Hong, S.J.; Han, J.P.; Kim, H.S.; Jeong, G.A.; Cho, G.S.; Kim, H.K.; Ko, B.M.; Lee, M.S. Long-term outcome of endoscopic and surgical resection for foregut neuroendocrine tumors. J. Dig. Dis. 2015, 16, 595–600. [Google Scholar] [CrossRef] [PubMed]
- Öberg, K.; Knigge, U.; Kwekkeboom, D.; Perren, A.; Group, E.G.W. Neuroendocrine gastro-entero-pancreatic tumors: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2012, 23 (Suppl. S7), vii124–vii130. [Google Scholar] [CrossRef] [PubMed]
- Fendrich, V.; Bartsch, D.K. Surgical treatment of gastrointestinal neuroendocrine tumors. Langenbecks Arch. Surg. 2011, 396, 299–311. [Google Scholar] [CrossRef] [PubMed]
- Erickson, J.A.; Grenache, D.G. A chromogranin A ELISA absent of an apparent high-dose hook effect observed in other chromogranin A ELISAs. Clin. Chim. Acta 2016, 452, 120–123. [Google Scholar] [CrossRef] [PubMed]
- Nagtegaal, I.D.; Odze, R.D.; Klimstra, D.; Paradis, V.; Rugge, M.; Schirmacher, P.; Washington, K.M.; Carneiro, F.; Cree, I.A.; the WHO Classification of Tumours Editorial Board. The 2019 WHO classification of tumours of the digestive system. Histopathology 2020, 76, 182–188. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Brierley, J.D.; Gospodarowicz, M.K.; Wittekind, C. TNM Classification of Malignant Tumours; John Wiley & Sons: Hoboken, NJ, USA, 2017. [Google Scholar]
- Lin, H.H.; Lin, J.K.; Jiang, J.K.; Lin, C.C.; Lan, Y.T.; Yang, S.H.; Wang, H.S.; Chen, W.S.; Lin, T.C.; Liang, W.Y.; et al. Clinicopathological analysis of colorectal carcinoid tumors and patient outcomes. World J. Surg. Oncol. 2014, 12, 366. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kim, J.; Kim, J.H.; Lee, J.Y.; Chun, J.; Im, J.P.; Kim, J.S. Clinical outcomes of endoscopic mucosal resection for rectal neuroendocrine tumor. BMC Gastroenterol. 2018, 18, 77. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Takatsu, Y.; Fukunaga, Y.; Nagasaki, T.; Akiyoshi, T.; Konishi, T.; Fujimoto, Y.; Nagayama, S.M.; Ueno, M.M. Short- and Long-term Outcomes of Laparoscopic Total Mesenteric Excision for Neuroendocrine Tumors of the Rectum. Dis. Colon. Rectum. 2017, 60, 284–289. [Google Scholar] [CrossRef] [PubMed]
- Fields, A.C.; McCarty, J.C.; Ma-Pak, L.; Lu, P.; Irani, J.; Goldberg, J.E.; Bleday, R.; Chan, J.; Melnitchouk, N. New lymph node staging for rectal neuroendocrine tumors. J. Surg. Oncol. 2019, 119, 156–162. [Google Scholar] [CrossRef] [PubMed]
- Witzke, O.; Sommerer, C.; Arns, W. Everolimus immunosuppression in kidney transplantation: What is the optimal strategy? Transplant. Rev. 2016, 30, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Calomino, N.; Poto, G.E.; Carbone, L.; Bagnacci, G.; Piccioni, S.; Andreucci, E.; Nenci, L.; Marano, L.; Verre, L.; Petrioli, R.; et al. Neuroendocrine tumors’ patients treated with somatostatin analogue could complicate with emergency cholecystectomy. Ann. Ital. Chir. 2023, 94, 518–522. [Google Scholar] [PubMed]
- Rinke, A.; Müller, H.H.; Schade-Brittinger, C.; Klose, K.J.; Barth, P.; Wied, M.; Mayer, C.; Aminossadati, B.; Pape, U.-F.; Bläker, M.; et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: A report from the PROMID Study Group. J. Clin. Oncol. 2009, 27, 4656–4663. [Google Scholar] [CrossRef] [PubMed]
- Caplin, M.E.; Pavel, M.; Phan, A.T.; Ćwikła, J.B.; Sedláčková, E.; Thanh, X.T.; Wolin, E.M.; Ruszniewski, P.; on behalf of the CLARINET Investigators. Lanreotide autogel/depot in advanced enteropancreatic neuroendocrine tumours: Final results of the CLARINET open-label extension study. Endocrine 2021, 71, 502–513. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gallo, C.; Rossi, R.E.; Cavalcoli, F.; Barbaro, F.; Boškoski, I.; Invernizzi, P.; Massironi, S. Rectal neuroendocrine tumors: Current advances in management, treatment, and surveillance. World J. Gastroenterol. 2022, 28, 1123–1138. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ahmed, M. Gastrointestinal neuroendocrine tumors in 2020. World J. Gastrointest. Oncol. 2020, 12, 791–807. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- McConnell, Y.J. Surgical management of rectal carcinoids: Trends and outcomes from the Surveillance, Epidemiology, and End Results database (1988 to 2012). Am. J. Surg. 2016, 211, 877–885. [Google Scholar] [CrossRef] [PubMed]
- Capurso, G.; Gaujoux, S.; Pescatori, L.C.; Panzuto, F.; Panis, Y.; Pilozzi, E.; Terris, B.; de Mestier, L.; Prat, F.; Rinzivillo, M.; et al. The ENETS TNM staging and grading system accurately predict prognosis in patients with rectal NENs. Dig. Liver Dis. 2019, 51, 1725–1730. [Google Scholar] [CrossRef] [PubMed]
- Violante, T.; Murphy, B.; Ferrari, D.; Graham, R.P.; Navin, P.; Merchea, A.; Larson, D.W.; Dozois, E.J.; Halfdanarson, T.R.; Perry, W.R. Presacral Neuroendocrine Neoplasms: A Multi-site Review of Surgical Outcomes. Ann. Surg. Oncol. 2024, 31, 4551–4557. [Google Scholar] [CrossRef] [PubMed]

| Demographics | n = 45 |
|---|---|
| Male | 24 (53.3) |
| Female | 21 (46.7) |
| Age at diagnosis, mean ± SD (years) | 57.5 ± 13.5 |
| BMI, mean ± SD (kg/m2) | 24.6 ± 5.3 |
| Smoker | 7 (15.6) |
| Presentation | |
| Incidental finding | 34 (75.6) |
| Symptomatic | 11 (24.4) |
| Rectal bleeding | 4 (8.9) |
| Abdominal pain | 5 (11.1) |
| Back pain | 1 (2.2) |
| Mass presence | 1 (2.2) |
| Constipation | 1 (2.2) |
| Distance from anal verge, mean ± SD (cm) | 7.0 ± 4.2 |
| Intervention | n = 45 |
|---|---|
| Endoscopic resection | 26 (57.8) |
| Polypectomy | 15 (57.7) |
| EMR | 8 (30.8) |
| ESD | 3 (11.5) |
| Surgical resection | 9 (20) |
| TAMIS | 5 (55.6) |
| LAR | 3 (33.3) |
| Proctocolectomy | 1 (11.1) |
| No intervention | 9 (20.0) |
| Tumor characteristics and pathology | |
| Size, mean ± SD (mm) | 14.5 ± 16.8 |
| Size ≤ 1 cm | 26 (57.8) |
| Size 1–2 cm | 8 (17.8) |
| Size ≥ 2 cm | 11 (24.4) |
| Endocrine function | 0 (0) |
| Vascular invasion | 3 (6.7) |
| Lymphatic invasion | 3 (6.7) |
| Abnormal chromogranin A (>95 ng/mL) | 5 (11.1) |
| Tumor grade | |
| Grade 1 (Ki-67 ≤ 3%) | 27 (60.0) |
| Grade 2 (Ki-67 3–20%) | 6 (13.3) |
| Grade 3 (Ki-67 ≥ 20%) | 12 (26.7) |
| Tumor stage | |
| Stage 1 | 28 (62.2) |
| Stage 2 | 1 (2.2) |
| Stage 3 | 5 (11.1) |
| Stage 4 | 11 (24.4) |
| Resection margin R1 | 3 (6.7) |
| Resection margin R2 | 2 (4.4) |
| Systemic treatments | |
| Somatostatin receptor antagonist | 8 (17.8) |
| Peptide receptor radionuclide therapy | 3 (6.7) |
| Chemotherapy | 14 (31.1) |
| Everolimus/Sunitinib | 3 (6.7) |
| Outcomes | |
| Local recurrence | 4 (8.9) |
| Disease progression | 13 (28.9) |
| De novo metastases | 11 (24.4) |
| Tumor-related mortality | 10 (22.2) |
| Overall mortality | 11 (24.4) |
| Follow-up (months), mean ± SD | 46.6 ± 41.0 |
| Overall survival (months), mean ± SD | 46.1 ± 41.0 |
| Disease free survival (months), mean ± SD | 40 ± 39.4 |
| Univariable p-Value | Multivariable Analysis | ||||
|---|---|---|---|---|---|
| OR (95% CI) | B | SE | p-Value | ||
| Tumor grade | <0.001 | 6.422 (0.129–318.540) | 1.860 | 1.992 | 0.350 |
| Tumor stage | <0.001 | 7.230 (1.105–47.321) | 1.978 | 0.959 | 0.039 |
| Symptomatic presentation | 0.007 | 10.929 (0.548–218.038) | 2.391 | 1.527 | 0.117 |
| Distance from anal verge | 0.240 | - | - | - | - |
| Size | 0.041 | 0.863 (0.737–1.009) | −0.148 | 0.080 | 0.065 |
| Ki-67 | 0.004 | 1.010 (0.933–1.094) | 0.010 | 0.041 | 0.798 |
| Basal chromogranin | 0.335 | - | - | - | - |
| Positive margins (R1 or R2) | 0.014 * | - | - | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cavalcoli, F.; Rausa, E.; Ferrari, D.; Rosa, R.; Maccauro, M.; Pusceddu, S.; Sabella, G.; Cantù, P.; Vitellaro, M.; Coppa, J.; et al. Pathological Characteristics, Management, and Prognosis of Rectal Neuroendocrine Tumors: A Retrospective Study from a Tertiary Hospital. Diagnostics 2024, 14, 1881. https://doi.org/10.3390/diagnostics14171881
Cavalcoli F, Rausa E, Ferrari D, Rosa R, Maccauro M, Pusceddu S, Sabella G, Cantù P, Vitellaro M, Coppa J, et al. Pathological Characteristics, Management, and Prognosis of Rectal Neuroendocrine Tumors: A Retrospective Study from a Tertiary Hospital. Diagnostics. 2024; 14(17):1881. https://doi.org/10.3390/diagnostics14171881
Chicago/Turabian StyleCavalcoli, Federica, Emanuele Rausa, Davide Ferrari, Roberto Rosa, Marco Maccauro, Sara Pusceddu, Giovanna Sabella, Paolo Cantù, Marco Vitellaro, Jorgelina Coppa, and et al. 2024. "Pathological Characteristics, Management, and Prognosis of Rectal Neuroendocrine Tumors: A Retrospective Study from a Tertiary Hospital" Diagnostics 14, no. 17: 1881. https://doi.org/10.3390/diagnostics14171881
APA StyleCavalcoli, F., Rausa, E., Ferrari, D., Rosa, R., Maccauro, M., Pusceddu, S., Sabella, G., Cantù, P., Vitellaro, M., Coppa, J., & Mazzaferro, V. (2024). Pathological Characteristics, Management, and Prognosis of Rectal Neuroendocrine Tumors: A Retrospective Study from a Tertiary Hospital. Diagnostics, 14(17), 1881. https://doi.org/10.3390/diagnostics14171881







