Risk Assessment of Nasal Cavity Perforation in the Maxilla: A Virtual Implant Placement Study Using Cone Beam Computed Tomography
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Radiographic Measurements
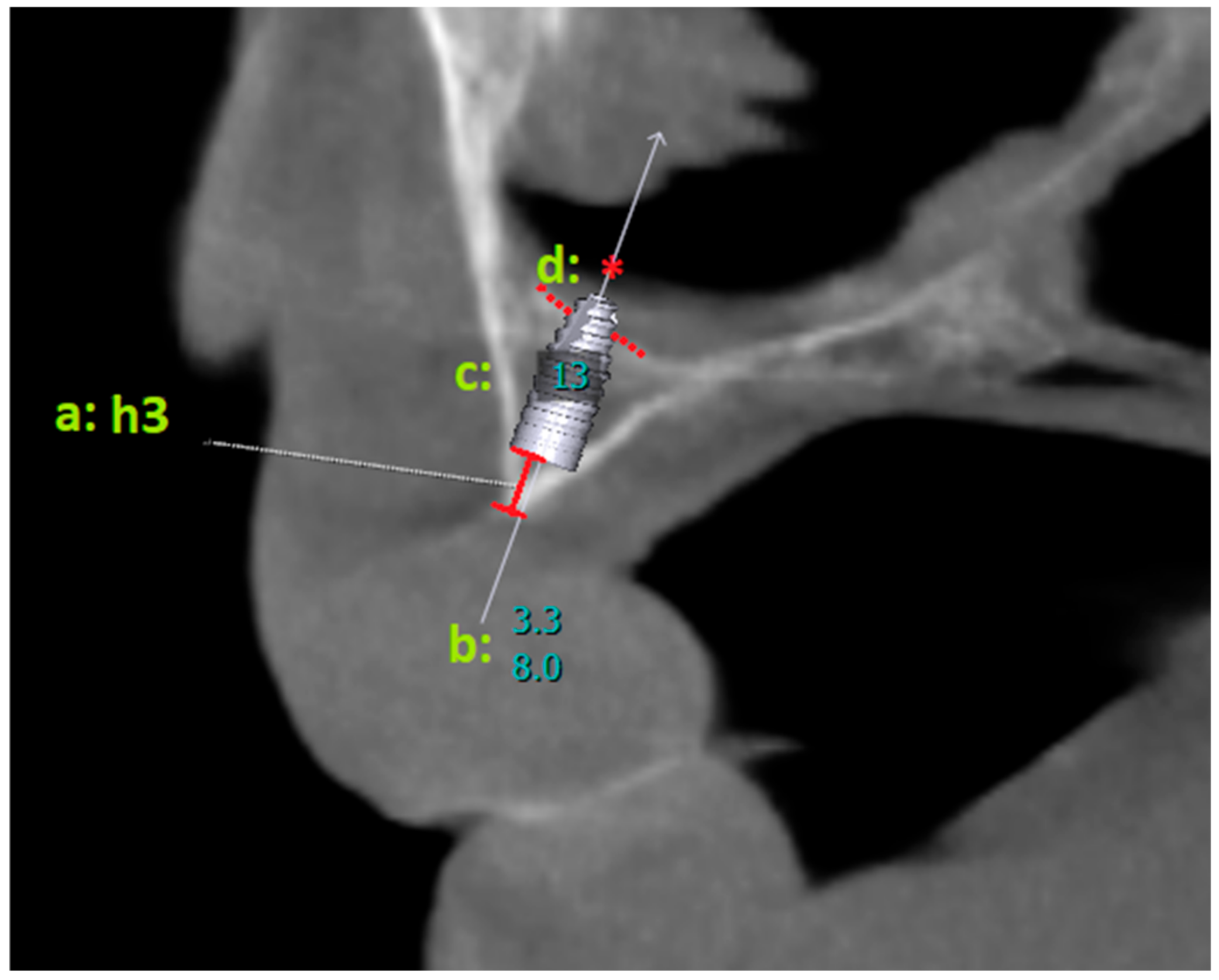
2.2.1. Virtual Implant Placement
2.2.2. Parameter Measurement
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Park, W.-B.; Kim, Y.-J.; Han, J.-Y.; Park, J.-S.; Kang, P. Radiographic and Nasal Endoscopic Observation of Accidentally Perforated Anterior Nasal Cavity with Dental Implants: Case Reports with 5–23 Years of Follow-Up. J. Oral Implant. 2021, 47, 492–497. [Google Scholar] [CrossRef] [PubMed]
- Sanchis, J.; Díaz, J. Accidental migration of dental implant into the nasal cavity: Spontaneous expulsion through the nose. J. Clin. Exp. Dent. 2021, 13, e1057–e1060. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Xing, Z.; Yu, L. Accidental migration of a dental implant into the nasal cavity. J. Int. Med. Res. 2020, 48, 300060520948736. [Google Scholar] [CrossRef] [PubMed]
- Wolff, J.; Karagozoglu, K.H.; Bretschneider, J.H.; Forouzanfar, T.; Schulten, E.A.J.M. Altered nasal airflow: An unusual complication following implant surgery in the anterior maxilla. Int. J. Implant. Dent. 2016, 2, 6. [Google Scholar] [CrossRef] [PubMed]
- Raghoebar, G.; van Weissenbruch, R.; Vissink, A. Rhino-sinusitis related to endosseous implants extending into the nasal cavity: A case report. Int. J. Oral Maxillofac. Surg. 2004, 33, 312–314. [Google Scholar] [CrossRef] [PubMed]
- Tal, H.; Moses, O. A comparison of panoramic radiography with computed tomography in the planning of implant surgery. Dentomaxillofac. Radiol. 1991, 20, 40–42. [Google Scholar] [CrossRef] [PubMed]
- Reddy, M.S.; Mayfield-Donahoo, T.; Vanderven, F.J.J.; Jeffcoat, M.K. A comparison of the diagnostic advantages of panoramic radiography and computed tomography scanning for placement of root form dental implants. Clin. Oral Implant. Res. 1994, 5, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Dreiseidler, T.; Mischkowski, R.A.; Neugebauer, J.; Ritter, L.; Zöller, J.E. Comparison of cone-beam imaging with orthopantomography and computerized tomography for assessment in presurgical implant dentistry. Int. J. Oral Maxillofac. Implant. 2009, 24, 216–225. [Google Scholar]
- Taşdemir, I.; Kalabalık, F.; Aytuğar, E.; Sağlam, M. Risk assessment of mandibular incisive canal perforation during dental implant surgery in the anterior edentulous mandible: A virtual implant placement study using cone beam computed tomography. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2023, 136, 681–685. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Wang, W.; Gu, X. Three-dimensional alveolar bone assessment of mandibular molars for immediate implant placement: A virtual implant placement study. BMC Oral Health 2021, 21, 478. [Google Scholar] [CrossRef] [PubMed]
- Alkanderi, A.; Al Sakka, Y.; Koticha, T.; Li, J.; Masood, F.; del Amo, F.S. Incidence of nasopalatine canal perforation in relation to virtual implant placement: A cone beam computed tomography study. Clin. Implant. Dent. Relat. Res. 2020, 22, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Xu, C.; Wang, N.; Wu, Y.; Liu, Y.; Fan, S.; Wang, F. Virtual pterygoid implant planning in maxillary atrophic patients: Prosthetic-driven planning and evaluation. Int. J. Implant. Dent. 2023, 9, 9. [Google Scholar] [CrossRef] [PubMed]
- Park, W.; Kim, Y.; Kang, K.L.; Lim, H.; Han, J. Long-term outcomes of the implants accidentally protruding into nasal cavity extended to posterior maxilla due to inferior meatus pneumatization. Clin. Implant. Dent. Relat. Res. 2020, 22, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Adell, R. Tissue integrated prostheses in clinical dentistry. Int. Dent. J. 1985, 35, 259–265. [Google Scholar] [PubMed]
- Keller, E.E.; Tolman, D.E.; Eckert, S.E. Maxillary antral-nasal inlay autogenous bone graft reconstruction of compromised maxilla: A 12-year retrospective study. Int. J. Oral Maxillofac. Implant. 1999, 14, 707–721. [Google Scholar]
- Garg, A.K. Nasal sinus lift: An innovative technique for implant insertions. Dent. Implant. Update 1997, 8, 49–53. [Google Scholar]
- Garcia-Denche, J.T.; Abbushi, A.; Hernández, G.; Fernández-Tresguerres, I.; Lopez-Cabarcos, E.; Tamimi, F. Nasal Floor Elevation for Implant Treatment in the Atrophic Premaxilla: A Within-Patient Com-parative Study. Clin. Implant Dent. Relat. Res. 2015, 17 (Suppl. 2), e520–e530. [Google Scholar] [CrossRef] [PubMed]
- Camargo, I.B.; Oliveira, D.M.; Fernandes, A.V.; Van Sickels, J.E. The nasal lift technique for augmentation of the maxillary ridge: Technical note. Br. J. Oral Maxillofac. Surg. 2015, 53, 771–774. [Google Scholar] [CrossRef] [PubMed]
- Pietrokovski, J.; Starinsky, R.; Arensburg, B.; Kaffe, I. Morphologic characteristics of bony edentulous jaws. J. Prosthodont. 2007, 16, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Yeom, H.-G.; Huh, K.-H.; Yi, W.-J.; Heo, M.-S.; Lee, S.-S.; Choi, S.-C.; Kim, J.-E. Nasal cavity perforation by implant fixtures: Case series with emphasis on panoramic imaging of nasal cavity extending posteriorly. Head Face Med. 2023, 19, 37. [Google Scholar] [CrossRef] [PubMed]






| Mean | Median | Standard Deviation | |
|---|---|---|---|
| Age | 60.81 | 60.00 | 11.39 |
| Count | Percentage | ||
| Gender | Male | 28 | 47.5% |
| Female | 31 | 52.5% |
| Overall h3 | F | p | ||
|---|---|---|---|---|
| Mean | Standard Deviation | |||
| Central | 2.42 a | 1.58 | 9.880 | <0.001 |
| Lateral | 2.36 a | 1.88 | ||
| Canine | 3.17 b | 1.84 | ||
| First premolar | 2.25 a | 1.42 | ||
| Implant Length and Region | Perforation Condition | Chi Square | p | |||
|---|---|---|---|---|---|---|
| Perforation Exists | No Perforation | |||||
| 8 mm | Region | Central | 15 (25.9%) | 103 (24.9%) | 2.752 | 0.431 |
| Lateral | 11 (19.0%) | 107 (25.8%) | ||||
| Canine | 19 (32.8%) | 99 (23.9%) | ||||
| 1st Premolar | 13 (22.4%) | 105 (25.4%) | ||||
| Total | 58 | 414 | ||||
| 10 mm | Region | Central | 53 (29.9%) | 65 (22.0%) | 7.620 | 0.055 |
| Lateral | 44 (24.9%) | 74 (25.1%) | ||||
| Canine | 47 (26.6%) | 71 (24.1%) | ||||
| 1st Premolar | 33 (18.6%) | 85 (28.8%) | ||||
| Total | 177 | 295 | ||||
| 12 mm | Region | Central | 85 (27.6%) | 33 (20.1%) | 8.073 | 0.045 |
| Lateral | 79 (25.6%) | 39 (23.8%) | ||||
| Canine | 79 (25.6%) | 39 (23.8%) | ||||
| 1st Premolar | 65 (21.1%) | 53 (32.3%) | ||||
| Total | 308 | 164 | ||||
| 14 mm | Region | Central | 105 (26.8%) | 13 (16.3%) | 13.727 | 0.003 |
| Lateral | 105 (26.8%) | 13 (16.3%) | ||||
| Canine | 95 (24.2%) | 23 (28.7%) | ||||
| 1st Premolar | 87 (22.2%) | 31 (38.8%) | ||||
| Total | 392 | 80 | ||||
| Total | Region | Central | 258 (27.6%) | 214 (22.5%) | 16.381 | <0.001 |
| Lateral | 239 (25.6%) | 233 (24.4%) | ||||
| Canine | 240 (25.7%) | 232 (24.3%) | ||||
| 1st Premolar | 198 (21.2%) | 274 (28.8%) | ||||
| Total | 935 | 953 | ||||
| Central | Lateral | Canine | 1st Premolar | |
|---|---|---|---|---|
| Mean | −0.2021 | 0.0778 | 3.5331 | 3.7251 |
| Minimum | −3.15 | −3.00 | 0.80 | 0.40 |
| Maximum | 2.30 | 1.90 | 7.00 | 7.65 |
| Range | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| −4 < hdif < −3 | −3 < hdif < −2 | −2 < hdif < −1 | −1 < hdif < −0 | 0 < hdif < 1 | 1 < hdif < 2 | 2 < hdif < 3 | 3 < hdif < 4 | 4 < hdif | X2 | p | cc | ||
| Region | Central | 3 a | 5 a | 5 a,b | 21 a | 17 a | 5 a,b | 2 a,b,c | 1 b,c | 0 c | 201.627 | <0.001 | 0.679 |
| Lateral | 2 a,b | 3 a,b,c | 9 b | 14 a,b | 18 a,b | 11 a,b | 1 a,b,c | 0 c,d | 1 d | ||||
| Canine | 0 a,b,c | 0 a,b,c | 0 b,c | 0 c | 1 c | 4 a,b,c | 8 a | 13 a | 33 a,b | ||||
| 1st Premolar | 0 a,b,c | 0 a,b,c | 0 b,c | 0 c | 1 c | 5 a,b,c | 4 a,b,c | 10 a,b | 39 a | ||||
| Total | 5 | 8 | 14 | 35 | 37 | 25 | 15 | 24 | 73 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaya, D.I.; Şatır, S.; Öztaş, B.; Yıldırım, H.; Aktı, A. Risk Assessment of Nasal Cavity Perforation in the Maxilla: A Virtual Implant Placement Study Using Cone Beam Computed Tomography. Diagnostics 2024, 14, 1479. https://doi.org/10.3390/diagnostics14141479
Kaya DI, Şatır S, Öztaş B, Yıldırım H, Aktı A. Risk Assessment of Nasal Cavity Perforation in the Maxilla: A Virtual Implant Placement Study Using Cone Beam Computed Tomography. Diagnostics. 2024; 14(14):1479. https://doi.org/10.3390/diagnostics14141479
Chicago/Turabian StyleKaya, Doğan Ilgaz, Samed Şatır, Beyza Öztaş, Hasan Yıldırım, and Ahmet Aktı. 2024. "Risk Assessment of Nasal Cavity Perforation in the Maxilla: A Virtual Implant Placement Study Using Cone Beam Computed Tomography" Diagnostics 14, no. 14: 1479. https://doi.org/10.3390/diagnostics14141479
APA StyleKaya, D. I., Şatır, S., Öztaş, B., Yıldırım, H., & Aktı, A. (2024). Risk Assessment of Nasal Cavity Perforation in the Maxilla: A Virtual Implant Placement Study Using Cone Beam Computed Tomography. Diagnostics, 14(14), 1479. https://doi.org/10.3390/diagnostics14141479






