Efficacy of Handheld Ultrasound in Medical Education: A Comprehensive Systematic Review and Narrative Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
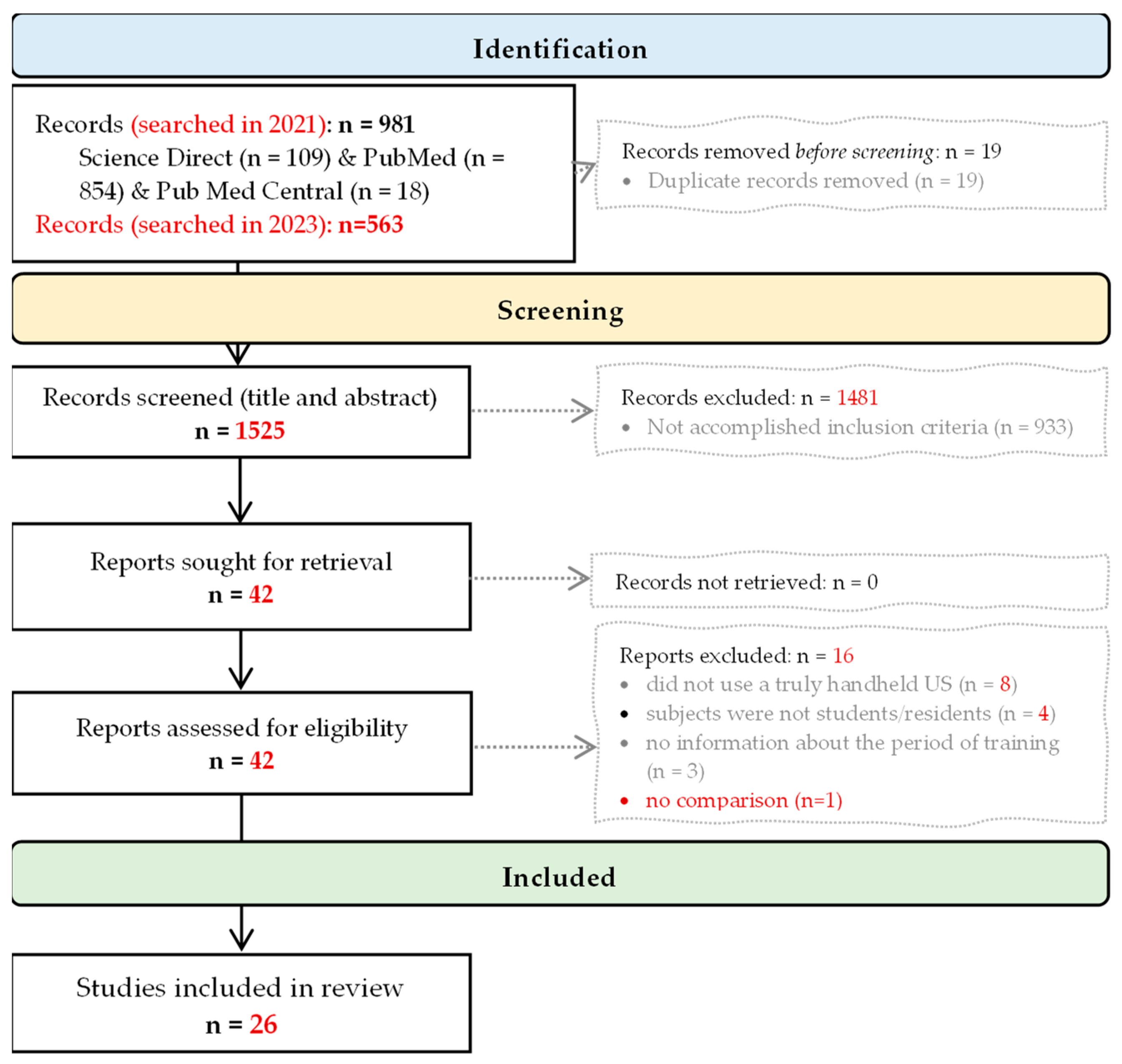
- Problem: medical students and residents lack of competence in performing ultrasounds.
- Intervention: ultraportable (handheld) ultrasound-based training program.
- Comparisons: pre- and post-tests given to study subjects; comparison between two groups (experimental group: handheld training vs. a group of experts or a group of novices who underwent a different intervention or no intervention).
- Outcome: skills in acquiring and interpreting ultrasound images.
- Study design: any exceptional case reports.
2.2. Article Selection
2.3. Data Extraction
2.4. Quality of Reporting Assessment
2.5. Presentation of the Findings
3. Results
3.1. The Trainees
3.2. The Handheld Ultrasound Devices
3.3. Training
3.4. Outcomes
3.5. Medical Education Research Study Quality Assessment
4. Discussion
4.1. Rethinking Medical Education
4.2. Handheld Ultrasound Devices in the Future
4.3. Limitations
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Epstein, D.; Petersiel, N.; Klein, E.; Marcusohn, E.; Aviran, E.; Harel, R.; Azzam, Z.S.; Neuberger, A.; Fuchs, L. Pocket-size point-of-care ultrasound in rural Uganda—A unique opportunity “to see”, where no imaging facilities are available. Travel Med. Infect. Dis. 2018, 23, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Handheld Portable Ultrasound Machine, Advanced Pocus Solutions. Available online: https://www.butterflynetwork.com (accessed on 10 August 2023).
- Johri, A.M. Generation iUltrasound: Bedside diagnostic imaging with Hand-Held Cardiac Ultrasound. Cardiol. J. 2014, 21, 98–99. [Google Scholar] [CrossRef] [PubMed]
- Mollenkopf, M.; Tait, N. Is it time to include point-of-care ultrasound in general surgery training? A review to stimulate discussion. ANZ J. Surg. 2013, 83, 908–911. [Google Scholar] [CrossRef] [PubMed]
- Medical Devices. World Health Organization. Available online: https://www.who.int/health-topics/medical-devices#tab=tab_1 (accessed on 10 August 2023).
- Butterfly iQ. Available online: https://www.butterflynetwork.com/ (accessed on 16 September 2023).
- Echonous Platform. Available online: https://echonous.com/en_us/ (accessed on 8 October 2022).
- Le, M.T.; Voigt, L.; Nathanson, R.; Maw, A.M.; Johnson, G.; Dancel, R.; Mathews, B.; Moreira, A.; Sauthoff, H.; Gelabert, C.; et al. Comparison of four handheld point-of-care ultrasound devices by expert users. Ultrasound J. 2022, 14, 27. [Google Scholar] [CrossRef] [PubMed]
- Mancusi, C.; Carlino, M.V.; Sforza, A. Point-of-care ultrasound with pocket-size devices in emergency department. Echocardiography 2019, 36, 1755–1764. [Google Scholar] [CrossRef]
- Malik, A.N.; Rowland, J.; Haber, B.D.; Thom, S.; Jackson, B.; Volk, B.; Ehrman, R.R. The Use of Handheld Ultrasound Devices in Emergency Medicine. Curr. Emerg. Hosp. Med. Rep. 2021, 9, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Nelson, B.P.; Melnick, E.R.; Li, J. Portable ultrasound for remote environments, Part I: Feasibility of field deployment. J. Emerg. Med. 2011, 40, 190–197. [Google Scholar] [CrossRef] [PubMed]
- Shorter, M.; Macias, D.J. Portable handheld ultrasound in austere environments: Use in the Haiti disaster. Prehosp. Disaster Med. 2012, 7, 172–177. [Google Scholar] [CrossRef]
- Bornemann, P.; Bornemann, G. Military family physicians’ perceptions of a pocket point-of-care ultrasound device in clinical practice. Mil. Med. 2014, 179, 1474–1477. [Google Scholar] [CrossRef]
- Baribeau, Y.; Sharkey, A.; Chaudhary, O.; Krumm, S.; Fatima, H.; Mahmood, F.; Matyal, R. Handheld Point-of-Care Ultrasound Probes: The New Generation of POCUS. J. Cardiothorac. Vasc. Anesth. 2020, 34, 3139–3145. [Google Scholar] [CrossRef]
- Toscano, M.; Szlachetka, K.; Whaley, N.; Thornburg, L.L. Evaluating sensitivity and specificity of handheld point-of-care ultrasound testing for gynecologic pathology: A pilot study for use in low resource settings. BMC Med. Imaging 2020, 20, 121. [Google Scholar] [CrossRef] [PubMed]
- Sethi, S.K.; Raina, R.; Koratala, A.; Rad, A.H.; Vadhera, A.; Badeli, H. Point-of-care ultrasound in pediatric nephrology. Pediatr. Nephrol. 2023, 38, 1733–1751. [Google Scholar] [CrossRef] [PubMed]
- Istrail, L. Instant Endocarditis Diagnosis Using Point-of-Care Ultrasound (POCUS) in a Patient Diagnosedwithh Pneumonia. Cureus 2023, 15, e36043. [Google Scholar] [CrossRef] [PubMed]
- Shokoohi, H.; Raymond, A.; Fleming, K.; Scott, J.; Kerry, V.; Haile-Mariam, T.; Sayeed, S.; Boniface, K.S. Assessment of Point-of-Care Ultrasound Training for Clinical Educators in Malawi, Tanzania and Uganda. Ultrasound Med. Biol. 2019, 45, 1351–1357. [Google Scholar] [CrossRef] [PubMed]
- Webb, E.M.; Cotton, J.B.; Kane, K.; Straus, C.M.; Topp, K.S.; Naeger, D.M. Teaching point of care ultrasound skills in medical school: Keeping radiology in the driver’s seat. Acad. Radiol. 2014, 21, 893–901. [Google Scholar] [CrossRef] [PubMed]
- Bell, G.; Wachira, B.; Denning, G. A pilot training program for point-of-care ultrasound in Kenya. Afr. J. Emerg. Med. 2016, 6, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Cullen, M.W.; Geske, J.B.; Anavekar, N.S.; Askew, J.W., 3rd; Lewis, B.R.; Oh, J.K. Handheld echocardiography during hospitalization for acute myocardial infarction. Clin. Cardiol. 2017, 40, 993–999. [Google Scholar] [CrossRef] [PubMed]
- Blume, G.G.; Lechinewski, L.D.; Vieira, I.P.; Clausell, N.; Bertinato, G.P.; Machado-Júnior, P.A.B.; Berro, P.G.; Zytynski Moura, L.A.; Tsang, T. Handheld Echocardiography in a Clinical Practice Scenario: Concordances Compared to Standard Echocardiographic Reports. J. Cardiovasc. Imaging 2022, 30, 25–34. [Google Scholar] [CrossRef]
- Haji-Hassan, M.; Duțu, B.; Bolboacă, S.D. Handheld Echocardiography Measurements Concordance and Findings Agreement: An Exploratory Study. Diagnostics 2023, 13, 853. [Google Scholar] [CrossRef]
- UC Irvine Medical School Gifts Butterfly Handheld Ultrasounds to Its Whole Class of 2023. Available online: https://www.mobihealthnews.com/news/north-america/uc-irvine-medical-school-gifts-butterfly-handheld-ultrasounds-its-whole-class (accessed on 10 August 2023).
- Breithardt, O.A. Hand-held ultrasound-the real stethoscope. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 471–472. [Google Scholar] [CrossRef][Green Version]
- Galusko, V.; Khanji, M.Y.; Bodger, O.; Weston, C.; Chambers, J.; Ionescu, A. Hand-held Ultrasound Scanners in Medical Education: A Systematic Review. J. Cardiovasc. Ultrasound 2017, 25, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Aki, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Cook, D.A.; Reed, D.A. Appraising the quality of medical education research methods: The Medical Education Research Study Quality Instrument and the Newcastle-Ottawa Scale-Education. Acad. Med. 2015, 90, 1067–1076. [Google Scholar] [CrossRef]
- Gogalniceanu, P.; Sheena, Y.; Kashef, E.; Purkayastha, S.; Darzi, A.; Paraskeva, P. Is basic emergency ultrasound training feasible as part of standard undergraduate medical education? J. Surg. Educ. 2010, 67, 152–156. [Google Scholar] [CrossRef] [PubMed]
- Swamy, M.; Searle, R.F. Anatomy teaching with portable ultrasound to medical students. BMC Med. Educ. 2012, 12, 99. [Google Scholar] [CrossRef]
- Bonnafy, T.; Lacroix, P.; Désormais, I.; Labrunie, A.; Marin, B.; Leclerc, A.; Oueslati, A.; Rollé, F.; Vignon, P.; Aboyans, V. Reliability of the measurement of the abdominal aortic diameter by novice operators using a pocket-sized ultrasound system. Arch. Cardiovasc. Dis. 2013, 106, 644–650. [Google Scholar] [CrossRef] [PubMed]
- Cawthorn, T.R.; Nickel, C.; O’Reilly, M.; Kafka, H.; Tam, J.W.; Jackson, L.C.; Sanfilippo, A.J.; Johri, A.M. Development and evaluation of methodologies for teaching focused cardiac ultrasound skills to medical students. J. Am. Soc. Echocardiogr. 2014, 27, 302–309. [Google Scholar] [CrossRef]
- Andersen, G.N.; Viset, A.; Mjølstad, O.C.; Salvesen, Ø.; Dalen, H.; Haugen, B.O. Feasibility and accuracy of point-of-care pocket-size ultrasonography performed by medical students. BMC Med. Educ. 2014, 14, 156. [Google Scholar] [CrossRef]
- Stokke, T.M.; Ruddox, V.; Sarvari, S.I.; Otterstad, J.E.; Aune, E.; Edvardsen, T. Brief group training of medical students in focused cardiac ultrasound may improve diagnostic accuracy of physical examination. J. Am. Soc. Echocardiogr. 2014, 27, 1238–1246. [Google Scholar] [CrossRef]
- Yan, B.; Wong, H.; Fok, J.; Cheung, W.; Kwan, T.; Tan, V.; Chui, K.; Kam, K.; Lee, A. Medical student performed pocket-sized ultrasound echocardiography after brief training compared to physical examination to detect significant valvular heart disease: A medical student project. Heart Lung Circ. 2015, 24, S350. [Google Scholar] [CrossRef][Green Version]
- Kapur, J.; Han, T.; Quek, S.; Kanagasuntheram, R.; Ng, Y.K.; Lim, A.; Chong, Y.S.; Yeoh, K.G.; Lee, S.S.; Samarasekera, D. The Role of Ultrasound in teaching Clinical Anatomy to First year Medical Students. MedEdPublish 2016, 5, 2. [Google Scholar] [CrossRef]
- Yan, B.P.; Fok, J.C.; Wong, T.H.; Tse, G.; Lee, A.P.W.; Yang, X.S.; Sun, J.-P. Junior medical student performed focused cardiac ultrasound after brief training to detect significant valvular heart disease. Int. J. Cardiol. Heart Vasc. 2018, 19, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Galusko, V.; Bodger, O.; Rees, E.; Ionescu, A. Hand-held ultrasonography: An opportunity for “hands-on” teaching of medicine. MedEdPublish 2018, 7, 103. [Google Scholar] [CrossRef] [PubMed]
- Jerg, A.; Denkinger, M.; Jerg-Bretzke, L. Development of an innovative physical examination course involving handheld ultrasound devices. MedEdPublish 2018, 7, 26. [Google Scholar] [CrossRef]
- Nausheen, F. Perception of students and faculty of integrated learning of basic sciences and clinical skills with the use of wireless portable ultrasound scanners. Ultrasound Med. Biol. 2019, 45, S110. [Google Scholar] [CrossRef]
- Kameda, T.; Koibuchi, H.; Konno, K.; Taniguchi, N. Self-learning followed by telepresence instruction of focused cardiac ultrasound with a handheld device for medical students: A preliminary study. J. Med. Ultrason 2022, 49, 415–423. [Google Scholar] [CrossRef] [PubMed]
- Nausheen, F.; Young, C.; Brazil, J.; Dunagan, T.; Bhupathy, R.; Elango, S.; Crowley, J. Confidence Level and Ability of Medical Students to Identify Abdominal Structures After Integrated Ultrasound Sessions. Ultrasound Int. Open 2020, 6, E7–E13. [Google Scholar] [CrossRef]
- Kaiser, U.; Dropco, I.; Reuthner, K.; Ertl, M.; Schlitt, H.J.; Herr, W.; Stroszczynski, C.; Jung, E.M. Wireless handheld focused ultrasound in student teaching during the COVID-19 pandemic: Initial results of a pilot study. Clin. Hemorheol. Microcirc. 2022. [Google Scholar] [CrossRef]
- Jujo, S.; Sakka, B.I.; Lee-Jayaram, J.J.; Kataoka, A.; Izumo, M.; Kusunose, K.; Nakahira, A.; Oikawa, S.; Kataoka, Y.; Berg, B.W. Medical student medium-term skill retention following cardiac point-of-care ultrasound training based on the American Society of Echocardiography curriculum framework. Cardiovasc Ultrasound 2022, 20, 26. [Google Scholar] [CrossRef]
- Slader, M.; Young, H.; Barker, M.; Prentice, K.; Bogaard, K.; Yuan, C.; Saadat, S.; Lahham, S. A comparison of handheld and standard ultrasound in Swiss medical students. World J. Emerg. Med. 2022, 13, 85–90. [Google Scholar] [CrossRef]
- Edwards, H.; Jones, H.; Garner, P.; Hardy, M.; Wilshaw, S.P.; Bielby-Clarke, K.; Farrow, M. Assessing student perception of the integration of portable wireless ultrasound imaging in undergraduate anatomy education. Clin. Anat. 2023, 36, 742–753. [Google Scholar] [CrossRef] [PubMed]
- Bui, M.; Fernandez, A.; Ramsukh, B.; Noel, O.; Prashad, C.; Bayne, D. Training and implementation of handheld ultrasound technology at Georgetown Public Hospital Corporation in Guyana: A virtual learning cohort study. J. Educ. Eval. Health Prof. 2023, 20, 11. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, J.S.; Barake, W.; Smith, C.; Thakrar, A.; Johri, A.M. A cautionary tale: A comparison of condensed teaching strategies to develop handheld cardiac ultrasound skills in internal medicine residents. Can. J. Cardiol. 2014, 30, S313–S314. [Google Scholar] [CrossRef][Green Version]
- Andersen, G.N.; Graven, T.; Skjetne, K.; Mjølstad, O.C.; Kleinau, J.O.; Olsen, Ø.; Haugen, B.O.; Dalen, H. Diagnostic influence of routine point-of-care pocket-size ultrasound examinations performed by medical residents. J. Ultrasound Med. 2015, 34, 627–636. [Google Scholar] [CrossRef] [PubMed]
- Maetani, T.H.; Schwartz, C.; Ward, R.J.; Nissman, D.B. Enhancement of Musculoskeletal Radiology Resident Education with the Use of an Individual Smart Portable Ultrasound Device (iSPUD). Acad. Radiol. 2018, 25, 1659–1666. [Google Scholar] [CrossRef] [PubMed]
- Bar, A.; Lin, G.; Lazar, L.O.; Blanka-Deak, J.; Khalayleh, H.; Pines, G. Immediate Pneumothorax Diagnosis by Surgical Residents Using Portable Ultrasound. Innovations 2021, 16, 152–156. [Google Scholar] [CrossRef] [PubMed]
- Acheampong, B.; Starnes, J.R.; Awuku, Y.A.; Parra, D.; Aliyu, M.H.; Soslow, J. Feasibility of focused cardiac ultrasound training for non-cardiologists in a resource-limited setting using a handheld ultrasound machine. Cardiovasc. J. Afr. 2022, 14, 1–5. [Google Scholar] [CrossRef]
- Panoulas, V.F.; Daigeler, A.L.; Malaweera, A.S.; Lota, A.S.; Baskaran, D.; Rahman, S.; Nihoyannopoulos, P. Pocket-size handheld cardiac ultrasound as an adjunct to clinical examination in the hands of medical students and junior doctors. Eur. Heart J. Cardiovasc. Imaging 2013, 14, 323–330. [Google Scholar] [CrossRef]
- Mai, T.V.; Ahn, D.T.; Phillips, C.T.; Agan, D.L.; Kimura, B.J. Feasibility of remote real-time guidance of a cardiac examination performed by novices using a pocket-sized ultrasound device. Emerg. Med. Int. 2013, 2013, 627230. [Google Scholar] [CrossRef]
- Nielsen, M.B.; Søgaard, S.B.; Bech Andersen, S.; Skjoldbye, B.; Hansen, K.L.; Rafaelsen, S.; Nørgaard, N.; Carlsen, J.F. Highlights 0of the development in ultrasound during the last 70 years: A historical review. Acta Radiol. 2021, 62, 1499–1514. [Google Scholar] [CrossRef]
- Liu, D.; Roth, E.; Pathak, A. Introduction to Point-of-Care Ultrasonography. AACN Adv. Crit. Care 2023, 34, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Duminuco, A.; Cupri, A.; Massimino, R.; Leotta, S.; Milone, G.A.; Garibaldi, B.; Giuffrida, G.; Garretto, O.; Milone, G. Handheld Ultrasound or Conventional Ultrasound Devices in Patients Undergoing HCT: A Validation Study. J. Clin. Med. 2023, 12, 520. [Google Scholar] [CrossRef] [PubMed]
- Haji-Hassan, M.; Călinici, T.; Drugan, T.; Bolboacă, S.D. Effectiveness of Ultrasound Cardiovascular Images in Teaching Anatomy: A Pilot Study of an Eight-Hour Training Exposure. Int. J. Environ. Res. Public Health 2022, 19, 3033. [Google Scholar] [CrossRef] [PubMed]
- Gibson, L.E.; White-Dzuro, G.A.; Lindsay, P.J.; Berg, S.M.; Bittner, E.A.; Chang, M.G. Ensuring competency in focused cardiac ultrasound: A systematic review of training programs. J. Intensive Care 2020, 8, 93. [Google Scholar] [CrossRef] [PubMed]
- Hellmann, D.B.; Whiting-O’Keefe, Q.; Shapiro, E.P.; Martin, L.D.; Martire, C.; Ziegelstein, R.C. The rate at which residents learn to use handheld echocardiography at the bedside. Am. J. Med. 2005, 118, 1010–1018. [Google Scholar] [CrossRef] [PubMed]
- Kimura, B.J.; Shaw, D.J.; Agan, D.L.; Amundson, S.A.; Ping, A.C.; DeMaria, A.N. Value of a cardiovascular limited US examination using a hand-carried US device on clinical management in an outpatient medical clinic. Am. J. Cardiol. 2007, 100, 321–325. [Google Scholar] [CrossRef] [PubMed]
- Alpert, J.S.; Mladenovic, J.; Hellmann, D.B. Should a hand-carried US machine become standard equipment for every internist? Am. J. Med. 2009, 122, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Fu, J.Y.; Krause, C.; Krause, R.; Mccoy, J.; Schindler, A.; Udrea, D.S.; Villarreal, L.A.; Jafry, Z.; Dinh, V.A. Integration of Point-of-Care Ultrasound Training into Undergraduate Medical Curricula—A Perspective from Medical Students. J. Med. Educ. Curric. Dev. 2016, 3, JMECD-S38240. [Google Scholar] [CrossRef]
- Dinh, V.A.; Dukes, W.S.; Prigge, J.; Avila, M. Ultrasound Integration in Undergraduate Medical Education: Comparison of Ultrasound Proficiency Between Trained and Untrained Medical Students. J. Ultrasound Med. 2015, 34, 1819–1824. [Google Scholar] [CrossRef]
- Park, K.E.; Mehta, P.; Tran, C.; Parikh, A.O.; Zhou, Q.; Zhang-Nunes, S. A comparison of five point-of-care ultrasound devices for use in ophthalmology and facial aesthetics. Ultrasound 2023. ahead of print. [Google Scholar] [CrossRef]
- Blaivas, M.; Brannam, L.; Theodoro, D. Ultrasound image quality comparison between an inexpensive handheld emergency department (ED) ultrasound machine and a large mobile ED ultrasound system. Acad. Emerg. Med. 2004, 11, 778–781. [Google Scholar] [CrossRef] [PubMed]
- Salimi, N.; Gonzalez-Fiol, A.; Yanez, N.D.; Fardelmann, K.L.; Harmon, E.; Kohari, K.; Abdel-Razeq, S.; Magriples, U.; Alian, A. Ultrasound Image Quality Comparison Between a Handheld Ultrasound Transducer and Mid-Range Ultrasound Machine. POCUS J. 2022, 21, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Elliott-Burke, T.; Dillon, T.; Bailey, J.; Miller, S.; Joos, R.; Buros Stein, A. Lumbar multifidus muscle ultrasound imaging: Is handheld technology reliable? Musculoskelet. Sci. Pract. 2023, 65, 102771. [Google Scholar] [CrossRef] [PubMed]
- Rothberg, J.M.; Ralston, T.S.; Rothberg, A.G.; Martin, J.; Zahorian, J.S.; Alie, S.A.; Sanchez, N.J.; Chen, K.; Chen, C.; Thiele, K.; et al. Ultrasound-on-chip platform for medical imaging, analysis, and collective intelligence. Proc. Natl. Acad. Sci. USA 2021, 118, e2019339118. [Google Scholar] [CrossRef] [PubMed]
- Kukla, P.; Maciejewska, K.; Strojna, I.; Zapał, M.; Zwierzchowski, G.; Bąk, B. Extended Reality in Diagnostic Imaging—A Literature Review. Tomography 2023, 9, 1071–1082. [Google Scholar] [CrossRef] [PubMed]
- Brattain, L.J.; Telfer, B.A.; Dhyani, M.; Grajo, J.R.; Samir, A.E. Machine learning for medical ultrasound: Status, methods, and future opportunities. Abdom. Radiol. 2018, 43, 786–799. [Google Scholar] [CrossRef]
- Rykkje, A.; Carlsen, J.F.; Nielsen, M.B. Hand-Held Ultrasound Devices Compared with High-End Ultrasound Systems: A Systematic Review. Diagnostics 2019, 9, 61. [Google Scholar] [CrossRef]
- Murray, S.; Trinder, K.; Kolbenson, L.; Katulka, J.; Olszynski, P. Virtual Supervision of Third Year Medical Students Using Handheld POCUS Devices and Cloud-based Image Archiving Provides Opportunity for Feedback and Skill Improvement. POCUS J. 2023, 8, 60–64. [Google Scholar] [CrossRef]
| Author/Year [ref] | What Was Studied? | Which Anatomical Structures/Pathologies? | No. of Participants (Specialty) | US Performed on … |
|---|---|---|---|---|
| Panoulas et al., 2013 [53] | clinical diagnosis skills and limited HHUS training | LV (systolic dysfunction, hypertrophy), dilated RV, valvular disease, pericardial effusion, Ao | 5 final-year medical std and 3 junior doctors | 122 patients |
| Mai et al., 2013 [54] | feasibility—cardiac ultrasound exams performed by novice users | LV systolic dysfunction, LA enlargement, lung comet-tail artifacts, inferior vena cava diameter, and collapse | 1 (medical std), 1 (intern), 1 (pharmacy resident) | 27 subjects (22 outpatients, 5 normal volunteers) |
| Bonnafy et al., 2013 [31] | Ao diameter measurements—short HHUS training | abdominal Ao | n/a | 56 patients |
| Wilkinson et al., 2014 [48] | diagnostic and technical skills with HHUS | cardiac US | 24 (internal medicine) | n/a |
| Andersen et al., 2015 [49] | goal-directed US with HHUS; half of the randomly selected participants used HHUS | cardiac a, pleural, and pericardial effusion; liver and gallbladder abnormalities; urinary system | 12 residents | 199 patients |
| Maetani et al., 2018 [50] | musculoskeletal HHUS | 10 wrist structures | 20 (radiology) | n/a |
| Bar et al., 2021 [51] | pneumothorax | lung/pleura | 4 (general surgery residents) | 85 patients |
| Acheampong et al., 2022 [52] | echocardiography | LV and RV structure and function, presence of effusion | 2 (internal medicine residents) * | 100 patients |
| Author, Year [ref] | What Was Studied? | Which Anatomical Structures/Pathologies? | No. of Participants and Their Year of Study | US Performed on … |
|---|---|---|---|---|
| Gogalniceanu et al., 2010 [29] | feasibility—basic US skills | FAST US protocol a | 26 (3rd and 5th) | n/a |
| Swamy et al., 2012 [30] | cadaveric anatomy teaching | upper and lower limbs b | 215 (2nd) | on each other |
| Cawthorn et al., 2014 [32] | focus cardiac examination | focused cardiac US | 12 (1st) and 45 (3rd) | n/a |
| Andersen et al., 2014 [33] | effectiveness of HHUS training | LV function, pericardial effusion, lung comets, inferior vena cava diameter, hydronephrosis, gallstones, chelocystitis, bladder distension, abdominal Ao diameter, abdominal free fluid | 30 (5th) | 211 patients |
| Stokke et al., 2014 [34] | the effectiveness of HHUS to detect clinically relevant cardiac lesions | valvular disease, LV and RV dysfunction, atrial diameters, pericardial effusion, Ao diameter | 21 (n/a) | 72 patients |
| Yan et al., 2015 [35] | feasibility (4 weeks) HHUS training | valvular heart disease | 4 (3rd) | 49 patients |
| Kapur et al., 2016 [36] | HHUS in teaching clinical anatomy | liver, spleen, kidneys, gallbladder, pancreas, urinary bladder, aorta | 100 (1st) | mannequins |
| Yan et al., 2018 [37] | focused cardiac US | valvular heart disease c | 10 (3rd) | 107 patients |
| Galusko et al., 2018 [38] | cardiac HHUS training | heart anatomy and pathology | 40 (n/a) | n/a |
| Jerg et al., 2018 [39] | HHUS as an adjuvant to physical examinations | heart and vessels, lungs and thorax, and abdomen in emergency examination | 10 (n/a) | n/a |
| Nausheen et al., 2019 [40] | teaching and learning basic sciences and clinical skills with HHUS | localization of liver, kidneys, Morison’s pouch, gall bladder, spleen, pancreas, aorta, and IVC, Doppler scan and the FAST exam | 60 (1st) | simulated patients |
| Nausheen et al., 2020 [42] | abdominal anatomy structures | liver, kidney, urinary bladder, inferior vena cava and aorta, spleen, gallbladder | 25 (1st) | standardized patients |
| Kameda et al., 2022 [41] | feasibility and efficacy of self-learning and telepresence instructions | focused cardiac ultrasound | 8 (3rd) +16 (4th) | on themselves |
| Kaiser et al., 2022 [43] | ultrasound image quality | portal vein, liver spleen, kidneys, aorta, Douglas/rectovesical space, portal vein, pancreas, FAS Trauma, hepatic artery and hepatic veins | 100 (n/a) | each other |
| Edwards et al., 2022 [46] | teaching sessions for anatomy education | upper and lower limb musculoskeletal structures, vessels and nerves, heart, liver, gallbladder | 107 (*) | each other |
| Jujo et al., 2022 [44] | to independently obtain basic cardiac POCUS views and to identify normal anatomic structures | heart ultrasound—cardiac POCUS | 54 (1st and 2nd) | healthy volunteer |
| Slader et al., 2022 [45] | US fundamentals | pulmonary US, abdominal US, cardiac US, and the Focused Assessment with Sonography for Trauma (FAST) | 119 (n/a) | n/a |
| Bui et al., 2023 [47] | urologic US | differentiating urine from peritoneal fluid, knowing the criteria for hydronephrosis, and deciding when to use catheterization over bladder POCUS volume measurement | 14 (n/a) | patients |
| Author, Year | Main Features of Training | Key Findings |
| Wilkinson et al., 2014 [48] |
|
|
| Andersen et al., 2015 [49] |
|
|
| Maetani et al., 2018 [50] |
|
|
| Panoulas et al., 2013 [53] |
|
|
| Mai et al., 2013 [54] |
|
|
| Bonnafy et al., 2013 [31] |
|
|
| Gogalniceanu et al., 2010 [29] |
|
|
| Swamy et al., 2012 [30] |
|
|
| Cawthorn et al., 2014 [32] |
|
|
| Andersen et al., 2014 [33] |
|
|
| Stokke et al., 2014 [34] |
|
|
| Yan et al., 2015 [35] |
|
|
| Kapur et al., 2016 [36] |
|
|
| Yan et al., 2018 [37] |
|
|
| Galusko et al., 2018 [38] |
|
|
| Jerg et al., 2018 [39] |
|
|
| Nausheen et al., 2019 [40] |
|
|
| Nausheen et al., 2020 [42] |
|
|
| Bar et al., 2021 [51] |
|
|
| Kameda et al., 2022 [41] |
|
|
| Kaiser et al., 2022 [43] |
|
|
| Edwards et al., 2022 [46] |
|
|
| Acheampong et al., 2022 [52] |
|
|
| Jujo et al., 2022 [44] |
|
|
| Slader et al., 2022 [45] |
|
|
| Bui et al., 2023 [47] |
|
|
| Domain | MERSQI Item | MERSQI Sub-Item | No (%) |
|---|---|---|---|
| Study design | Single-group cross-sectional or single group post-test only | 13 (50.0) | |
| Single-group pretest and posttest | 8 (30.8) | ||
| Non-randomized (two or more groups) | 3 (11.5) | ||
| Randomized controlled trial | 2 (7.7) | ||
| Sampling | No. of institutions studied | 1 | 23 (88.5) |
| 2 | 1 (3.8) | ||
| >2 | 1 (3.8) | ||
| Response rate percentage | <50% or not reported | 22 (84.6) | |
| 50–74% | 0 (0) | ||
| >75% | 1 (0) | ||
| Not applicable | 3 (11.5) | ||
| Type of data | Assessment by study participant (knowledge self-report) | 7 (26.9) | |
| Objective measurement (knowledge test) | 20 (76.9) | ||
| Validity of evaluation instrument | Internal structure | Not applicable | 3 (11.5) |
| Not reported | 23 (88.5) | ||
| Reported | 0 (0) | ||
| Content validity | Not applicable | 3 (11.5) | |
| Not reported | 23 (88.5) | ||
| Reported | 0 (0) | ||
| Relationships to other variables | Not applicable | 3 (11.5) | |
| Not reported | 23 (88.5) | ||
| Reported | 0 (0) | ||
| Data analysis | Appropriateness of analysis for study design or type of data | Inappropriate | 2 (7.7) |
| Appropriate | 24 (92.3) | ||
| Complexity of analysis | Descriptive analysis only | 9 (34.6) | |
| Beyond descriptive analysis | 17 (65.4) | ||
| Outcomes | Satisfaction, attitudes, perceptions, opinions, general facts | 5 (19.2) | |
| Knowledge, skills | 19 (73.1) | ||
| Behaviors | 1 (3.8) | ||
| Patient/healthcare outcomes | 3 (11.8) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haji-Hassan, M.; Capraș, R.-D.; Bolboacă, S.D. Efficacy of Handheld Ultrasound in Medical Education: A Comprehensive Systematic Review and Narrative Analysis. Diagnostics 2023, 13, 3665. https://doi.org/10.3390/diagnostics13243665
Haji-Hassan M, Capraș R-D, Bolboacă SD. Efficacy of Handheld Ultrasound in Medical Education: A Comprehensive Systematic Review and Narrative Analysis. Diagnostics. 2023; 13(24):3665. https://doi.org/10.3390/diagnostics13243665
Chicago/Turabian StyleHaji-Hassan, Mariam, Roxana-Denisa Capraș, and Sorana D. Bolboacă. 2023. "Efficacy of Handheld Ultrasound in Medical Education: A Comprehensive Systematic Review and Narrative Analysis" Diagnostics 13, no. 24: 3665. https://doi.org/10.3390/diagnostics13243665
APA StyleHaji-Hassan, M., Capraș, R.-D., & Bolboacă, S. D. (2023). Efficacy of Handheld Ultrasound in Medical Education: A Comprehensive Systematic Review and Narrative Analysis. Diagnostics, 13(24), 3665. https://doi.org/10.3390/diagnostics13243665







