Emergency Endoscopic Interventions in Acute Upper Gastrointestinal Bleeding: A Cohort Study
Abstract
:1. Introduction
2. Material and Methods
2.1. Patients
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Antunes, C.; Copelin, I.E. Upper Gastrointestinal Bleeding; StatPearls: Treasure Island, FL, USA, 2023. [Google Scholar]
- Gralnek, I.M.; Stanley, A.J.; Morris, A.J.; Camus, M.; Lau, J.; Lanas, A.; Laursen, S.B.; Radaelli, F.; Papanikolaou, I.S.; Gonçalves, T.C.; et al. Endoscopic diagnosis and management of nonvariceal upper gastrointestinal hemorrhage (NVUGIH): European Society of Gastrointestinal Endoscopy (ESGE) Guideline—Update 2021. Endoscopy 2021, 53, 300–332. [Google Scholar] [CrossRef]
- De Franchis, R.; Bosch, J.; Garcia-Tsao, G.; Reiberger, T.; Ripoll, C.; Baveno, V.I.I.F. Baveno VII—Renewing consensus in portal hypertension. J. Hepatol. 2022, 76, 959–974. [Google Scholar] [CrossRef]
- Marek, T.; Baniukiewicz, A.; Wallner, G.; Rydzewska, G.; Dąbrowski, A. Wytyczne postępowania w krwawieniu z górnego odcinka przewodu pokarmowego pochodzenia nieżylakowego. Gastroenterol. Rev./Przegląd Gastroenterol. 2008, 3, 1–22. [Google Scholar]
- Kherad, O.; Restellini, S.; Martel, M.; Barkun, A. Proton pump inhibitors for upper gastrointestinal bleeding. Best Pract. Res. Clin. Gastroenterol. 2019, 42–43, 101609. [Google Scholar] [CrossRef] [PubMed]
- Lau, J.Y.; Sung, J.J.; Lee, K.K.; Yung, M.-Y.; Wong, S.K.; Wu, J.C.; Chan, F.K.; Ng, E.K.; You, J.H.; Lee, C.; et al. Effect of intravenous omeprazole on recurrent bleeding after endoscopic treatment of bleeding peptic ulcers. N. Engl. J. Med. 2000, 343, 310–316. [Google Scholar] [CrossRef] [PubMed]
- Barkun, A.N.; Bardou, M.; Kuipers, E.J.; Sung, J.; Hunt, R.H.; Martel, M.; Sinclair, P. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann. Intern. Med. 2010, 152, 101–113. [Google Scholar] [CrossRef]
- Sung, J.J.Y.; Barkun, A.; Kuipers, E.J.; Mössner, J.; Jensen, D.M.; Stuart, R.; Lau, J.Y.; Ahlbom, H.; Kilhamn, J.; Lind, T.; et al. Intravenous esomeprazole for prevention of recurrent peptic ulcer bleeding: A randomized trial. Ann. Intern. Med. 2009, 150, 455–464. [Google Scholar] [CrossRef] [PubMed]
- Laine, L.; Barkun, A.N.; Saltzman, J.R.; Martel, M.; Leontiadis, G.I. ACG Clinical Guideline: Upper Gastrointestinal and Ulcer Bleeding. Am. J. Gastroenterol. 2021, 116, 899–917. [Google Scholar] [CrossRef] [PubMed]
- Fujishiro, M.; Iguchi, M.; Kakushima, N.; Kato, M.; Sakata, Y.; Hoteya, S.; Kataoka, M.; Shimaoka, S.; Yahagi, N.; Fujimoto, K. Guidelines for endoscopic management of non-variceal upper gastrointestinal bleeding. Dig. Endosc. 2016, 28, 363–378. [Google Scholar] [CrossRef] [PubMed]
- Kuipers, E.J. Improved risk assessment in upper GI bleeding. Gastrointest. Endosc. 2011, 74, 1225–1229. [Google Scholar] [CrossRef]
- Stanley, A.; Ashley, D.; Dalton, H.; Mowat, C.; Gaya, D.R.; Thompson, E.; Warshow, U.; Groome, M.; Cahill, A.; Benson, G.; et al. Outpatient management of patients with low-risk upper-gastrointestinal haemorrhage: Multicentre validation and prospective evaluation. Lancet 2009, 373, 42–47. [Google Scholar] [CrossRef]
- Jung, D.H.; Huh, C.W.; Kim, N.J.; Kim, B.-W. Optimal endoscopy timing in patients with acute variceal bleeding: A systematic review and meta-analysis. Sci. Rep. 2020, 10, 4046. [Google Scholar] [CrossRef]
- Rockall, T.A.; Logan, R.F.; Devlin, H.B.; Northfield, T.C. Risk assessment after acute upper gastrointestinal haemorrhage. Gut 1996, 38, 316–321. [Google Scholar] [CrossRef] [PubMed]
- Stanley, A.J.; Laine, L.; Dalton, H.R.; Ngu, J.H.; Schultz, M.; Abazi, R.; Zakko, L.; Thornton, S.; Wilkinson, K.; Khor, C.J.L.; et al. Comparison of risk scoring systems for patients presenting with upper gastrointestinal bleeding: International multicentre prospective study. BMJ 2017, 356, i6432. [Google Scholar] [CrossRef]
- Kim, J.S.; Kim, B.-W.; Kim, D.H.; Park, C.H.; Lee, H.; Joo, M.K.; Jung, D.H.; Chung, J.W.; Choi, H.S.; Baik, G.H.; et al. Guidelines for Nonvariceal Upper Gastrointestinal Bleeding. Gut Liver 2020, 14, 560–570. [Google Scholar] [CrossRef]
- Sung, J.J.; Chiu, P.W.; Chan, F.K.L.; Lau, J.Y.; Goh, K.-L.; Ho, L.H.; Jung, H.-Y.; Sollano, J.D.; Gotoda, T.; Reddy, N.; et al. Asia-Pacific working group consensus on non-variceal upper gastrointestinal bleeding: An update 2018. Gut 2018, 67, 1757–1768. [Google Scholar] [CrossRef] [PubMed]
- Gralnek, I.M.; Dumonceau, J.-M.; Kuipers, E.J.; Lanas, A.; Sanders, D.S.; Kurien, M.; Rotondano, G.; Hucl, T.; Dinis-Ribeiro, M.; Marmo, R.; et al. Diagnosis and management of nonvariceal upper gastrointestinal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 2015, 47, a1–a46. [Google Scholar] [CrossRef] [PubMed]
- Lau, J.Y.; Yu, Y.; Tang, R.S.; Chan, H.C.; Yip, H.-C.; Chan, S.M.; Luk, S.W.; Wong, S.H.; Lau, L.H.; Lui, R.N.; et al. Timing of Endoscopy for Acute Upper Gastrointestinal Bleeding. N. Engl. J. Med. 2020, 382, 1299–1308. [Google Scholar] [CrossRef] [PubMed]
- Hearnshaw, S.A.; Logan, R.F.A.; Lowe, D.; Travis, S.P.L.; Murphy, M.F.; Palmer, K.R. Use of endoscopy for management of acute upper gastrointestinal bleeding in the UK: Results of a nationwide audit. Gut 2010, 59, 1022–1029. [Google Scholar] [CrossRef]
- Huh, C.W.; Kim, J.S.; Jung, D.H.; Yang, J.D.; Nam, S.W.; Kwon, J.H.; Kim, B.-W. Optimal endoscopy timing according to the severity of underlying liver disease in patients with acute variceal bleeding. Dig. Liver Dis. 2019, 51, 993–998. [Google Scholar] [CrossRef]
- Laursen, S.B.; Leontiadis, G.I.; Stanley, A.J.; Møller, M.H.; Hansen, J.M.; de Muckadell, O.B.S. Relationship between timing of endoscopy and mortality in patients with peptic ulcer bleeding: A nationwide cohort study. Gastrointest. Endosc. 2017, 85, 936–944.e3. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.-H.; Lee, Y.-S.; Kim, Y.-J.; Sohn, C.H.; Ahn, S.; Seo, D.-W.; Kim, W.Y.; Lee, J.H.; Lim, K.S. Outcomes and Role of Urgent Endoscopy in High-Risk Patients With Acute Nonvariceal Gastrointestinal Bleeding. Clin. Gastroenterol. Hepatol. 2018, 16, 370–377. [Google Scholar] [CrossRef] [PubMed]
- Spiegel, B.M.; Vakil, N.B.; Ofman, J.J. Endoscopy for acute nonvariceal upper gastrointestinal tract hemorrhage: Is sooner better? A systematic review. Arch. Intern. Med. 2001, 161, 1393–1404. [Google Scholar] [CrossRef] [PubMed]
- Tsoi, K.K.; Ma, T.K.; Sung, J.J. Endoscopy for upper gastrointestinal bleeding: How urgent is it? Nat. Rev. Gastroenterol. Hepatol. 2009, 6, 463–469. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.G.; Turnipseed, S.; Romano, P.S.; Vigil, H.; Azari, R.; Melnikoff, N.; Hsu, R.; Kirk, D.; Sokolove, P.; Leung, J.W. Endoscopy-based triage significantly reduces hospitalization rates and costs of treating upper GI bleeding: A randomized controlled trial. Gastrointest. Endosc. 1999, 50, 755–761. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.-J.; Wang, K.; Perng, C.-L.; Chua, R.T.; Lee, F.-Y.; Lee, C.-H.; Lee, S.-D. Early or Delayed Endoscopy for Patients with Peptic Ulcer Bleeding. J. Clin. Gastroenterol. 1996, 22, 267–271. [Google Scholar] [CrossRef]
- Bjorkman, D.J.; Zaman, A.; Fennerty, M.; Lieberman, D.; DiSario, J.A.; Guest-Warnick, G. Urgent vs. elective endoscopy for acute non-variceal upper-GI bleeding: An effectiveness study. Gastrointest. Endosc. 2004, 60, 1–8. [Google Scholar] [CrossRef]
- Edelson, J.; Basso, J.E.; Rockey, D.C. Updated strategies in the management of acute variceal haemorrhage. Curr. Opin. Gastroenterol. 2021, 37, 167–172. [Google Scholar] [CrossRef]
- Guo, C.L.T.; Wong, S.H.; Lau, L.H.S.; Lui, R.N.S.; Mak, J.W.Y.; Tang, R.S.Y.; Yip, T.C.F.; Wu, W.K.K.; Wong, G.L.H.; Chan, F.K.L.; et al. Timing of endoscopy for acute upper gastrointestinal bleeding: A territory-wide cohort study. Gut 2022, 71, 1544–1550. [Google Scholar] [CrossRef]

| Variable | All Group | The Day-Hours Group | The Night-Hours Group | p Value | 95% CI | OR |
|---|---|---|---|---|---|---|
| Sex, Male/Female | 480/272 | 375/214 | 105/57 | <0.79 | ||
| Age, median (IQR) | 62 (50–74) | 62 (50–75) | 61.5 (50–72) | <0.38 | ||
| Duration time of the gastroscopy, minutes, median (IQR) | 18 (10–29) | 17 (10–28) | 21 (11–34) | <0.01 | 1.00–1.02 | 1.01 |
| Variceal etiology of the bleeding, n (%) | 174 (23.1%) | 127 (21.79%) | 47 (28.13%) | <0.09 | ||
| Esophageal varices, n (%) | 147 (19.6%) | 108 (18.41%) | 39 (23.75%) | <0.13 | ||
| Gastric varices, n (%) | 47 (6.2%) | 85 (14.53%) | 18 (10.63%) | <0.55 | ||
Non-variceal etiology of bleeding, n (%):
| 332 (44.2%) 133 (17.7%) 78 (10.4%) 23 (3.1%) 18 (2.4%) 13 (1.7%) 12 (1.6%) 10 (1.3%) 9 (1.2%) 9 (1.2%) 8 (1%) 8 (1%) 3 (0.4%) | 267 (45.10%) 109 (18.44%) 60 (10.15%) 15 (2.55%) 15 (2.53%) 12 (2.03%) 8 (1.68%) 5 (1.05%) 5 (1.06%) 4 (0.84%) 5 (1.06%) 4 (0.84%) 2 (0.34%) | 65 (40.625%) 24 (15%) 18 (11.32%) 8 (4.91%) 3 (1.88%) 1 (0.63%) 4 (1.43%) 5 (1.80%) 4 (1.43%) 5 (1.80%) 3 (1.08%) 4 (1.44%) 1 (0.62%) | <0.31 <0.32 <0.67 <0.13 <0.85 <0.39 <0.33 <0.03 <0.10 <0.01 <0.28 <0.05 <0.62 | ||
| Glasgow–Blatchford score, median (IQR) | 10 (6–12) | 10 (6–11) | 10 (6–13) | <0.48 | ||
| ‘Pre-Endoscopy’ Rockall score, median (IQR) | 3 (1–4) | 3 (1–5) | 2.5 (1–4) | <0.50 | ||
| Endoscopically achieved hemostasis rate/‘success rate’ | 425/509 (83.5) | 334/391 (85) | 91/118 (77) | <0.03 | 0.90–2.32 | 1.44 |
| Second-look endoscopy, n (%) | 178 (23.8%) | 130 (22.24%) | 48 (29.75%) | <0.26 | ||
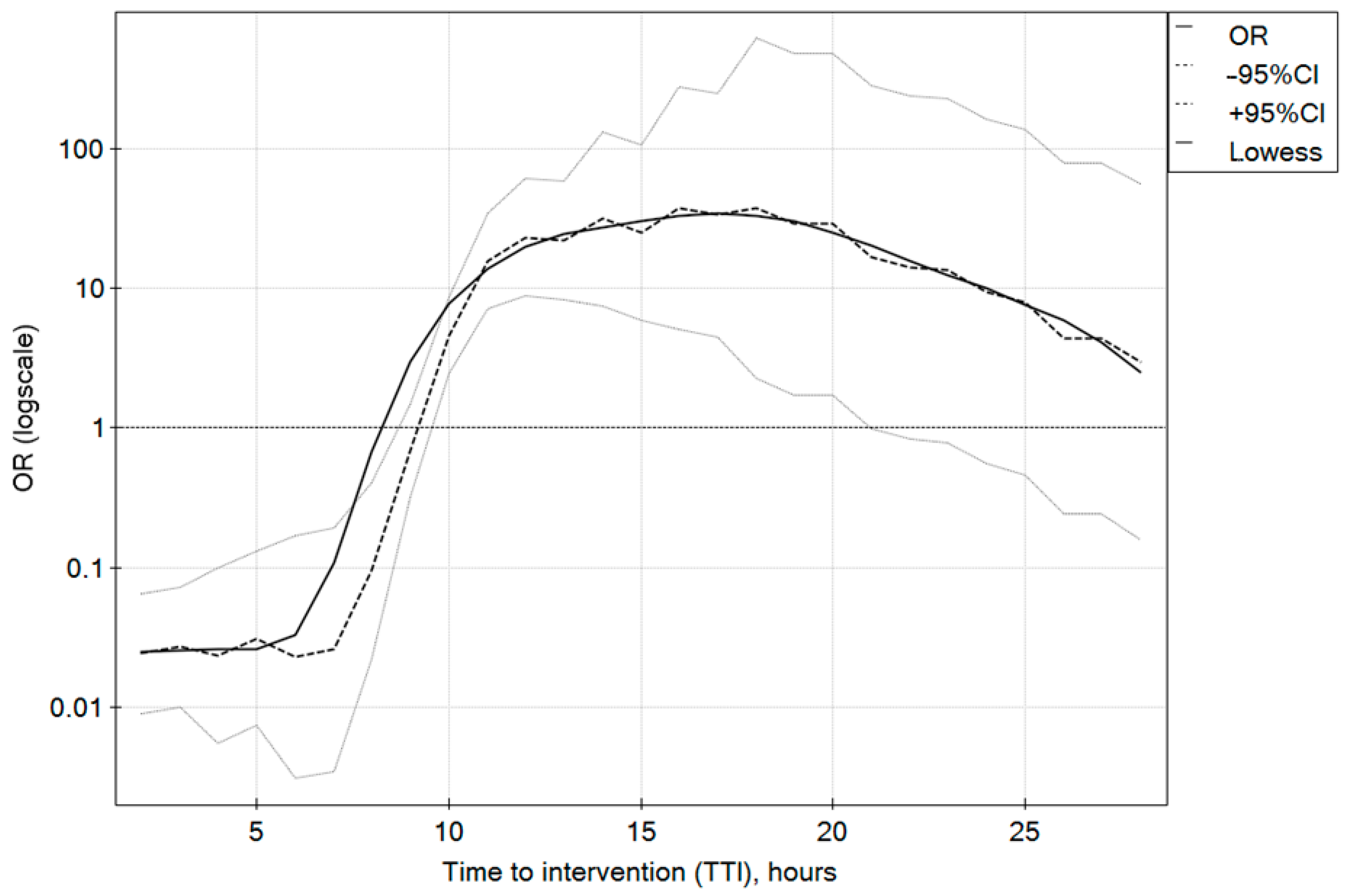
| Time to intervention (TTI), hours (IQR) | 9 (5–15) | 10 (6–15) | 6 (4–16) | <0.001 | 1.01–1.10 | 1.10 |
| Time of hospital stay, days (IQR) | 10 (5–26) | 10 (4–24) | 12.5 (5–27) | <0.33 | ||
| Mean TTI in ‘successful hemostasis group’, hours (IQR) | 10 (7–13) | 10 (8–13) * | 8 (5–14) ** | <0.06 | 0.97–1.12 | 1.04 |
| Mean TTI for ‘failed hemostasis group’, hours (IQR) | 4 (4–5) | 4 (4–5) * | 4 (3–4) ** | <0.01 | 0.99–2.49 | 1.57 |
| Re-bleeding, n (%) | 131 (17.4%) | 98 (16.72%) | 33 (20%) | <0.44 | ||
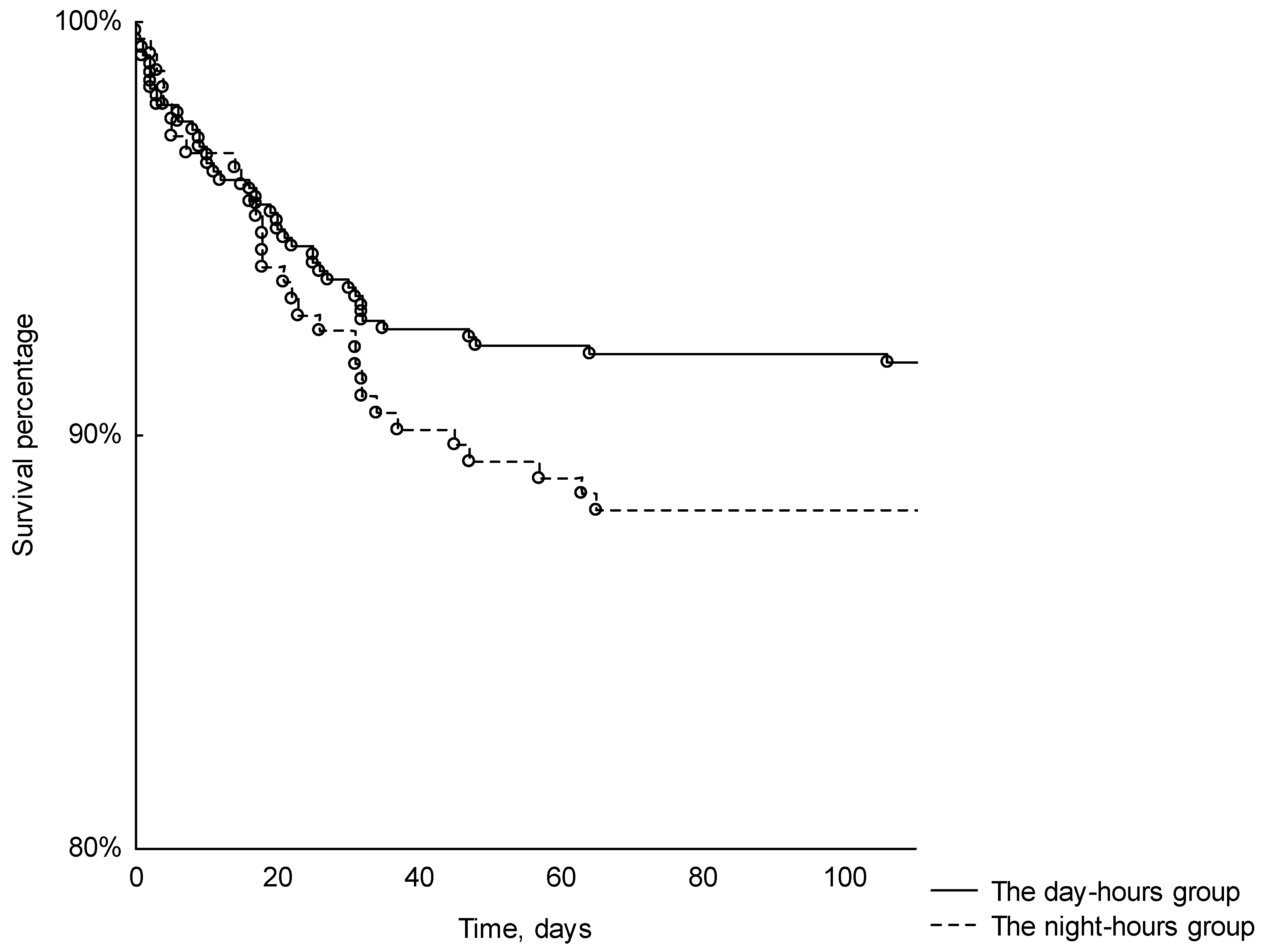
| 120-day all-cause mortality, n (%) | 72 (10.6%) | 41 (8.65%) | 31 (11.15%) | <0.26 |
| All | The Day-Hours Group | The Night-Hours Group | p Value | |
|---|---|---|---|---|
| Endoscopically Confirmed Bleeding (ECB), n/N (%), | 509/752 (68) | 390/590 (66) | 119/162 (74) | <0.76 |
| ECB ≥ 3 points in Rockall score, n/N (%),where n is ECB and N is number of pts with Rockall score ≥ 3 | 146/216 (68) | 120/183 (66) | 26/33 (79) | <0.14 |
| ECB < 3 points in Rockall score, n/N (%), where n is ECB and N is number of pts with Rockall score < 3 | 109/167 (65) | 84/134 (63) | 25/33 (76) | <0.16 |
| ECB ≥ 6 points in Glasgow–Blatchford score, n/N (%), where n is ECB and N is number of pts with GBS ≥ 6 | 70/103 (68) | 56/87 (64) | 14/16 (88) | <0.13 |
| ECB < 6 points in Glasgow–Blatchford score, n/N (%), where n is ECB and N is number of pts with GBS < 6 | 13/21 (62) | 11/18 (61) | 2/3 (67) | <0.65 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mackiewicz-Pracka, A.; Nehring, P.; Przybyłkowski, A. Emergency Endoscopic Interventions in Acute Upper Gastrointestinal Bleeding: A Cohort Study. Diagnostics 2023, 13, 3584. https://doi.org/10.3390/diagnostics13233584
Mackiewicz-Pracka A, Nehring P, Przybyłkowski A. Emergency Endoscopic Interventions in Acute Upper Gastrointestinal Bleeding: A Cohort Study. Diagnostics. 2023; 13(23):3584. https://doi.org/10.3390/diagnostics13233584
Chicago/Turabian StyleMackiewicz-Pracka, Anna, Piotr Nehring, and Adam Przybyłkowski. 2023. "Emergency Endoscopic Interventions in Acute Upper Gastrointestinal Bleeding: A Cohort Study" Diagnostics 13, no. 23: 3584. https://doi.org/10.3390/diagnostics13233584
APA StyleMackiewicz-Pracka, A., Nehring, P., & Przybyłkowski, A. (2023). Emergency Endoscopic Interventions in Acute Upper Gastrointestinal Bleeding: A Cohort Study. Diagnostics, 13(23), 3584. https://doi.org/10.3390/diagnostics13233584





