Refractory Bilateral Tubo-Ovarian Abscesses in a Patient with Iatrogenic Hypogammaglobulinemia
Abstract
:1. Introduction
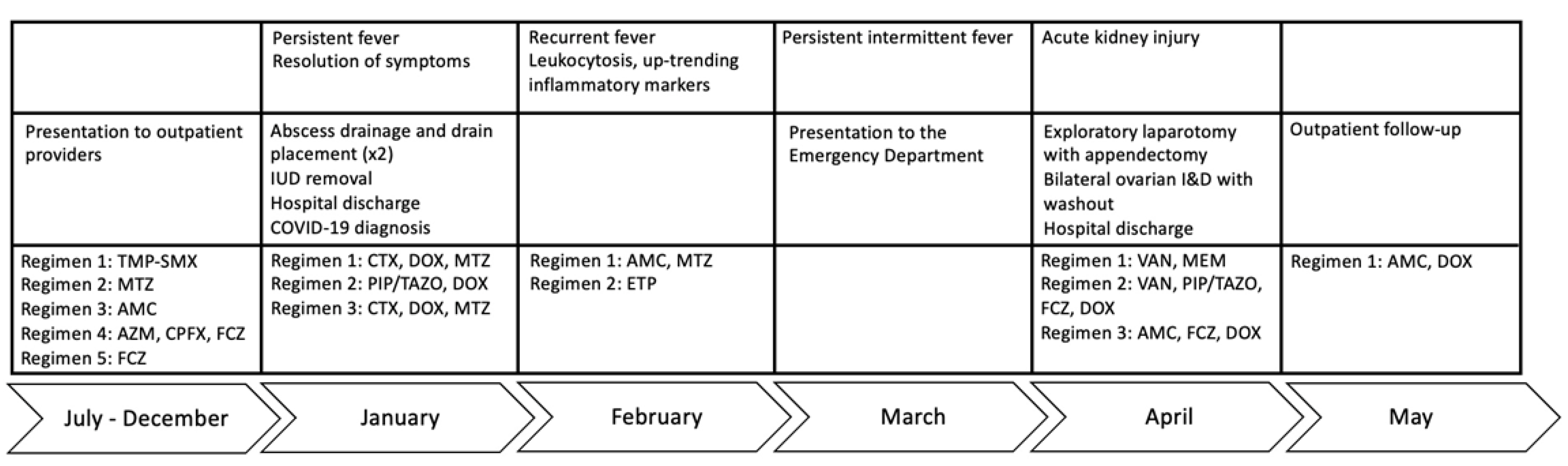
2. Clinical Case Description
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McCormack, W.M.; Almeida, P.C.; Bailey, P.E.; Grady, E.M.; Lee, Y.H. Sexual activity and vaginal colonization with genital mycoplasmas. JAMA 1972, 221, 1375–1377. [Google Scholar] [CrossRef] [PubMed]
- Waites, K.B.; Schelonka, R.L.; Xiao, L.; Grigsby, P.L.; Novy, M.J. Congenital and opportunistic infections: Ureaplasma species and Mycoplasma hominis. Semin. Fetal Neonatal Med. 2009, 14, 190–199. [Google Scholar] [CrossRef] [PubMed]
- Plummer, E.L.; Vodstrcil, L.A.; Bodiyabadu, K.; Murray, G.L.; Doyle, M.; Latimer, R.L.; Fairley, C.K.; Payne, M.; Chow, E.P.F.; Garland, S.M.; et al. Are Mycoplasma hominis, Ureaplasma urealyticum and Ureaplasma parvum Associated With Specific Genital Symptoms and Clinical Signs in Nonpregnant Women? Clin. Infect. Dis. 2021, 73, 659–668. [Google Scholar] [CrossRef] [PubMed]
- Taylor-Robinson, D. Mollicutes in vaginal microbiology: Mycoplasma hominis, Ureaplasma urealyticum, Ureaplasma parvum and Mycoplasma genitalium. Res. Microbiol. 2017, 168, 875–881. [Google Scholar] [CrossRef]
- Kletzel, H.H.; Rotem, R.; Barg, M.; Michaeli, J.; Reichman, O. Ureaplasma urealyticum: The Role as a Pathogen in Women’s Health, a Systematic Review. Curr. Infect. Dis. Rep. 2018, 20, 33. [Google Scholar] [CrossRef] [PubMed]
- Horner, P.; Donders, G.; Cusini, M.; Gomberg, M.; Jensen, J.S.; Unemo, M. Should we be testing for urogenital Mycoplasma hominis, Ureaplasma parvum and Ureaplasma urealyticum in men and women?—A position statement from the European STI Guidelines Editorial Board. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 1845–1851. [Google Scholar] [CrossRef]
- Workowski, K.A.; Bachmann, L.H.; Chan, P.A.; Johnston, C.M.; Muzny, C.A.; Park, I.; Reno, H.; Zenilman, J.M.; Bolan, G.A. Sexually Transmitted Infections Treatment Guidelines, 2021. MMWR Recomm. Rep. 2021, 70, 1–187. [Google Scholar] [CrossRef]
- Diaz Pallares, C.; Griener, T.; Vaughan, S. Ureaplasma urealyticum disseminated multifocal abscesses in an immunocompromised adult patient: A case report. BMC Infect. Dis. 2020, 20, 47. [Google Scholar] [CrossRef]
- Kvalvik, S.A.; Skarstein, I.; Veddeng, A.; Løland von Volkmann, H.; Kvalvik, T.; Torkildsen, Ø.F.G.; Ebbing, C. An immunocompromised woman in her twenties with abdominal pain and vaginal discharge. Tidsskr. Nor. Laegeforen. 2020, 140. [Google Scholar] [CrossRef]
- Rahman, O.; Younas, Z.; Agard, A.; Kruer, R.; Ho, T.; Daly, A.; Khan, H.; Craft, M.; Patel, D.; Jamshaid, F.; et al. Disseminated ureaplasma urealyticum infection and life-threatening hyperammonemia with rituximab use. Crit. Care Med. 2023, 51, 193. [Google Scholar] [CrossRef]
- Schwartz, D.J.; Elward, A.; Storch, G.A.; Rosen, D.A. Ureaplasma urealyticum pyelonephritis presenting with progressive dysuria, renal failure, and neurologic symptoms in an immunocompromised patient. Transpl. Infect. Dis. 2019, 21, e13032. [Google Scholar] [CrossRef]
- Nowbakht, C.; Edwards, A.R.; Rodriguez-Buritica, D.F.; Luce, A.M.; Doshi, P.B.; De Golovine, A.; Bynon, J.S.; Nigo, M. Two Cases of Fatal Hyperammonemia Syndrome due to Mycoplasma hominis and Ureaplasma urealyticum in Immunocompromised Patients Outside Lung Transplant Recipients. Open Forum Infect. Dis. 2019, 6, ofz033. [Google Scholar] [CrossRef] [PubMed]
- Jhaveri, V.V.; Lasalvia, M.T. Invasive Ureaplasma Infection in Patients Receiving Rituximab and Other Humoral Immunodeficiencies-A Case Report and Review of the Literature. Open Forum Infect. Dis. 2019, 6, ofz399. [Google Scholar] [CrossRef] [PubMed]
- Meygret, A.; Le Roy, C.; Renaudin, H.; Bébéar, C.; Pereyre, S. Tetracycline and fluoroquinolone resistance in clinical Ureaplasma spp. and Mycoplasma hominis isolates in France between 2010 and 2015. J. Antimicrob. Chemother. 2018, 73, 2696–2703. [Google Scholar] [CrossRef]
- Robertson, J.A.; Stemke, G.W.; Davis, J.W.; Harasawa, R.; Thirkell, D.; Kong, F.; Shepard, M.C.; Ford, D.K. Proposal of Ureaplasma parvum sp. nov. and emended description of Ureaplasma urealyticum (Shepard et al. 1974) Robertson et al. 2001. Int. J. Syst. Evol. Microbiol. 2002, 52, 587–597. [Google Scholar] [CrossRef]
- Tantengco, O.A.G.; Yanagihara, I. Current understanding and treatment of intra-amniotic infection with Ureaplasma spp. J. Obstet. Gynaecol. Res. 2019, 45, 1796–1808. [Google Scholar] [CrossRef] [PubMed]
- Li, G.Z.; Tio, M.C.; Pak, L.M.; Krier, J.; Seifter, J.L.; Tullius, S.G.; Riella, L.V.; Malek, S.K.; Stergachis, A.B. Noncirrhotic hyperammonemia after deceased donor kidney transplantation: A case report. Am. J. Transplant. 2019, 19, 3197–3201. [Google Scholar] [CrossRef]
- Roberts, S.C.; Malik, W.; Ison, M.G. Hyperammonemia syndrome in immunosuppressed individuals. Curr. Opin. Infect. Dis. 2022, 35, 262–268. [Google Scholar] [CrossRef]
- Seethapathy, H.; Fenves, A.Z. Pathophysiology and Management of Hyperammonemia in Organ Transplant Patients. Am. J. Kidney Dis. 2019, 74, 390–398. [Google Scholar] [CrossRef]
- Fleming, D.; Cunningham, S.A.; Patel, R. Contribution of Uremia to Ureaplasma-Induced Hyperammonemia. Microbiol. Spectr. 2022, 10, e0194221. [Google Scholar] [CrossRef]
- Spooner, R.K.; Russell, W.C.; Thirkell, D. Characterization of the immunoglobulin A protease of Ureaplasma urealyticum. Infect. Immun. 1992, 60, 2544–2546. [Google Scholar] [CrossRef] [PubMed]
- Beeton, M.L.; Spiller, O.B. Antibiotic resistance among Ureaplasma spp. isolates: Cause for concern? J. Antimicrob. Chemother. 2017, 72, 330–337. [Google Scholar] [CrossRef]
- Furr, P.M.; Taylor-Robinson, D.; Webster, A.D. Mycoplasmas and ureaplasmas in patients with hypogammaglobulinaemia and their role in arthritis: Microbiological observations over twenty years. Ann. Rheum. Dis. 1994, 53, 183–187. [Google Scholar] [CrossRef]
- Kothari, A.; Morgan, M.; Haake, D.A. Emerging technologies for rapid identification of bloodstream pathogens. Clin. Infect. Dis. 2014, 59, 272–278. [Google Scholar] [CrossRef]
- Schreckenberger, P.C.; McAdam, A.J. Point-Counterpoint: Large Multiplex PCR Panels Should Be First-Line Tests for Detection of Respiratory and Intestinal Pathogens. J. Clin. Microbiol. 2015, 53, 3110–3115. [Google Scholar] [CrossRef]
- Ramanan, P.; Bryson, A.L.; Binnicker, M.J.; Pritt, B.S.; Patel, R. Syndromic Panel-Based Testing in Clinical Microbiology. Clin. Microbiol. Rev. 2017, 31, e00024-17. [Google Scholar] [CrossRef]
- Blauwkamp, T.A.; Thair, S.; Rosen, M.J.; Blair, L.; Lindner, M.S.; Vilfan, I.D.; Kawli, T.; Christians, F.C.; Venkatasubrahmanyam, S.; Wall, G.D.; et al. Analytical and clinical validation of a microbial cell-free DNA sequencing test for infectious disease. Nat. Microbiol. 2019, 4, 663–674. [Google Scholar] [CrossRef] [PubMed]
- Simner, P.J.; Miller, S.; Carroll, K.C. Understanding the Promises and Hurdles of Metagenomic Next-Generation Sequencing as a Diagnostic Tool for Infectious Diseases. Clin. Infect. Dis. 2018, 66, 778–788. [Google Scholar] [CrossRef] [PubMed]
- Greninger, A.L.; Messacar, K.; Dunnebacke, T.; Naccache, S.N.; Federman, S.; Bouquet, J.; Mirsky, D.; Nomura, Y.; Yagi, S.; Glaser, C.; et al. Clinical metagenomic identification of Balamuthia mandrillaris encephalitis and assembly of the draft genome: The continuing case for reference genome sequencing. Genome Med. 2015, 7, 113. [Google Scholar] [CrossRef]
- Wilson, M.R.; Naccache, S.N.; Samayoa, E.; Biagtan, M.; Bashir, H.; Yu, G.; Salamat, S.M.; Somasekar, S.; Federman, S.; Miller, S.; et al. Actionable diagnosis of neuroleptospirosis by next-generation sequencing. N. Engl. J. Med. 2014, 370, 2408–2417. [Google Scholar] [CrossRef]
- Miao, Q.; Ma, Y.; Wang, Q.; Pan, J.; Zhang, Y.; Jin, W.; Yao, Y.; Su, Y.; Huang, Y.; Wang, M.; et al. Microbiological Diagnostic Performance of Metagenomic Next-generation Sequencing When Applied to Clinical Practice. Clin. Infect. Dis. 2018, 67, S231–S240. [Google Scholar] [CrossRef]
- Abril, M.K.; Barnett, A.S.; Wegermann, K.; Fountain, E.; Strand, A.; Heyman, B.M.; Blough, B.A.; Swaminathan, A.C.; Sharma-Kuinkel, B.; Ruffin, F.; et al. Diagnosis of Capnocytophaga canimorsus Sepsis by Whole-Genome Next-Generation Sequencing. Open Forum Infect. Dis. 2016, 3, ofw144. [Google Scholar] [CrossRef] [PubMed]
- Hong, D.K.; Blauwkamp, T.A.; Kertesz, M.; Bercovici, S.; Truong, C.; Banaei, N. Liquid biopsy for infectious diseases: Sequencing of cell-free plasma to detect pathogen DNA in patients with invasive fungal disease. Diagn. Microbiol. Infect. Dis. 2018, 92, 210–213. [Google Scholar] [CrossRef] [PubMed]
- Taur, Y.; Pamer, E.G. The intestinal microbiota and susceptibility to infection in immunocompromised patients. Curr. Opin. Infect. Dis. 2013, 26, 332–337. [Google Scholar] [CrossRef]
- Taur, Y.; Xavier, J.B.; Lipuma, L.; Ubeda, C.; Goldberg, J.; Gobourne, A.; Lee, Y.J.; Dubin, K.A.; Socci, N.D.; Viale, A.; et al. Intestinal domination and the risk of bacteremia in patients undergoing allogeneic hematopoietic stem cell transplantation. Clin. Infect. Dis. 2012, 55, 905–914. [Google Scholar] [CrossRef]
- Benamu, E.; Gajurel, K.; Anderson, J.N.; Lieb, T.; Gomez, C.A.; Seng, H.; Aquino, R.; Hollemon, D.; Hong, D.K.; Blauwkamp, T.A.; et al. Plasma Microbial Cell-free DNA Next-generation Sequencing in the Diagnosis and Management of Febrile Neutropenia. Clin. Infect. Dis. 2022, 74, 1659–1668. [Google Scholar] [CrossRef]
- Païssé, S.; Valle, C.; Servant, F.; Courtney, M.; Burcelin, R.; Amar, J.; Lelouvier, B. Comprehensive description of blood microbiome from healthy donors assessed by 16S targeted metagenomic sequencing. Transfusion 2016, 56, 1138–1147. [Google Scholar] [CrossRef] [PubMed]
- Gosiewski, T.; Flis, A.; Sroka, A.; Kędzierska, A.; Pietrzyk, A.; Kędzierska, J.; Drwiła, R.; Bulanda, M. Comparison of nested, multiplex, qPCR; FISH; SeptiFast and blood culture methods in detection and identification of bacteria and fungi in blood of patients with sepsis. BMC Microbiol. 2014, 14, 313. [Google Scholar] [CrossRef]
- Schulz, E.; Grumaz, S.; Hatzl, S.; Gornicec, M.; Valentin, T.; Huber-Kraßnitzer, B.; Kriegl, L.; Uhl, B.; Deutsch, A.; Greinix, H.; et al. Pathogen Detection by Metagenomic Next-Generation Sequencing During Neutropenic Fever in Patients With Hematological Malignancies. Open Forum Infect. Dis. 2022, 9, ofac393. [Google Scholar] [CrossRef]


| Laboratory Test | Value at Admission | Value at Discharge | Reference Range and Units |
|---|---|---|---|
| Chemistry, Serum | |||
| Blood urea nitrogen | 15 mg/dL | 10 mg/dL | 6–24 mg/dL |
| Creatinine | 2.57 mg/dL | 0.96 mg/dL | 0.44–1.03 mg/dL |
| ALT 1 | 15 IU/L | 27 IU/L | 6–45 IU/L |
| AST 2 | 14 IU/L | 22 IU/L | 10–42 IU/L |
| Alkaline phosphatase | 199 IU/L | 152 IU/L | 34–104 IU/L |
| Total bilirubin | 0.7 g/dL | 0.4 g/dL | 0.2–1.3 mg/dL |
| Albumin | 2.4 g/dL | 3.3 g/dL | 3.5–5.0 g/dL |
| Total protein | 4.8 g/dL | 6.5 g/dL | 6.0–8.0 g/dL |
| Ammonia | 42 μmol/L | ND 3 | 2–50 μmol/L |
| Microbiological Tests | |||
| Ureaplasma parvum, urine PCR | Not detected | Not detected | |
| Ureaplasma urealyticum, urine PCR | Detected | Not detected | |
| Mycoplasma hominis, urine PCR | Not detected | Not detected | |
| Mycoplasma genitalium, urine PCR | Not detected | Not detected | |
| Bacterial detection via PCR with reflex to 16S NGS in blood | Ureaplasma urealyticum 4256 DNA MPM | <10 DNA MPM | |
| Legionella urine antigen | Negative | Negative | |
| C. difficile toxin, PCR | Not detected | Not detected | |
| Other Tests | |||
| CRP 4 | 237.33 mg/L | 34.78 mg/L | 0.00–10.00 mg/L |
| ESR 5 | 76 mm/h | ND | 0–20 mm/h |
| Urine pregnancy | Negative | ND | Negative |
| IgG | 321 mg/dL | ND | 552–1631 mg/dL |
| IgG1 | 160 mg/dL | ND | 240–1118 mg/dL |
| IgG2 | 99 mg/dL | ND | 124–549 mg/dL |
| IgG3 | 12 mg/dL | ND | 21–134 mg/dL |
| IgG4 | 7 mg/dL | ND | 1–123 mg/dL |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Klein, E.J.; Almaghlouth, N.K.; Weigel, G.; Farmakiotis, D.; Hardy, E. Refractory Bilateral Tubo-Ovarian Abscesses in a Patient with Iatrogenic Hypogammaglobulinemia. Diagnostics 2023, 13, 3478. https://doi.org/10.3390/diagnostics13223478
Klein EJ, Almaghlouth NK, Weigel G, Farmakiotis D, Hardy E. Refractory Bilateral Tubo-Ovarian Abscesses in a Patient with Iatrogenic Hypogammaglobulinemia. Diagnostics. 2023; 13(22):3478. https://doi.org/10.3390/diagnostics13223478
Chicago/Turabian StyleKlein, Elizabeth J., Nouf K. Almaghlouth, Gabriela Weigel, Dimitrios Farmakiotis, and Erica Hardy. 2023. "Refractory Bilateral Tubo-Ovarian Abscesses in a Patient with Iatrogenic Hypogammaglobulinemia" Diagnostics 13, no. 22: 3478. https://doi.org/10.3390/diagnostics13223478
APA StyleKlein, E. J., Almaghlouth, N. K., Weigel, G., Farmakiotis, D., & Hardy, E. (2023). Refractory Bilateral Tubo-Ovarian Abscesses in a Patient with Iatrogenic Hypogammaglobulinemia. Diagnostics, 13(22), 3478. https://doi.org/10.3390/diagnostics13223478






