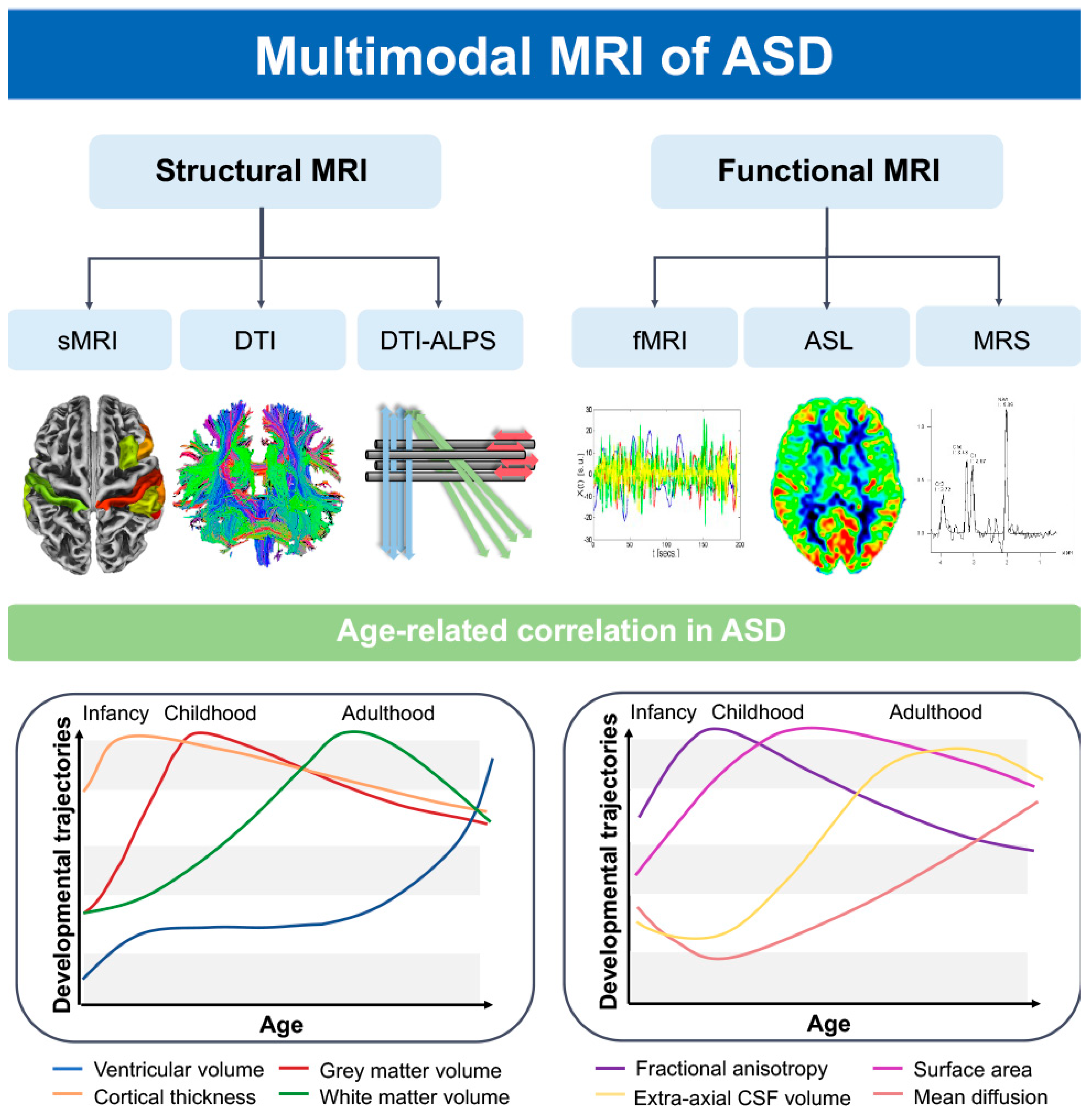
Application of Multimodal MRI in the Early Diagnosis of Autism Spectrum Disorders: A Review
Abstract
1. Introduction
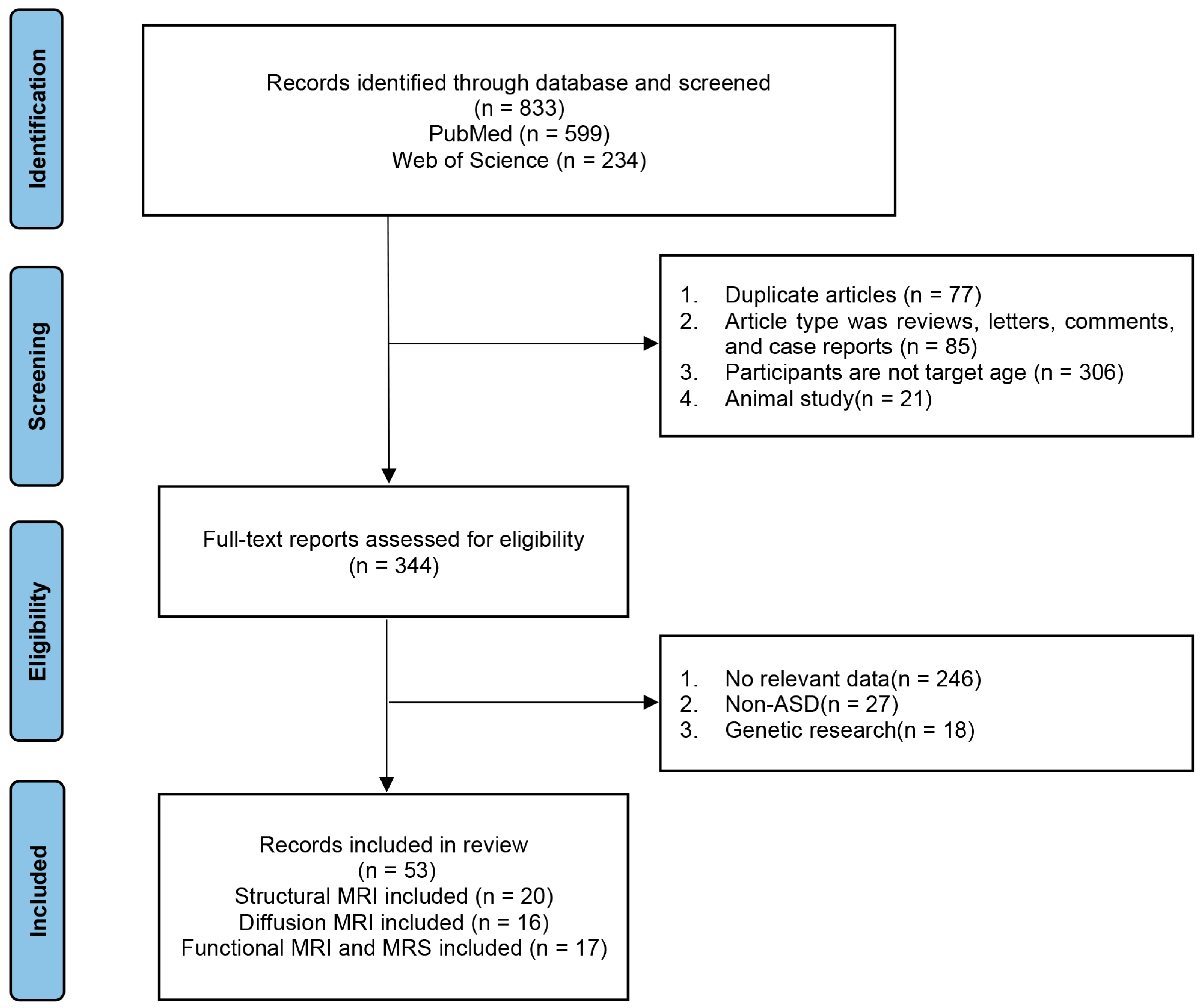
2. Materials and Methods
3. Research Progress of Structural MRI in ASD
4. Studying Brain Network Changes in Children with ASD Using DTI
5. Functional MRI–Based Functional Brain Network Alterations in ASD
6. ASL-Based Alterations in ASD Perfusion
7. Proton Magnetic Resonance Spectroscopy–Based Biochemical Metabolite Alterations in ASD
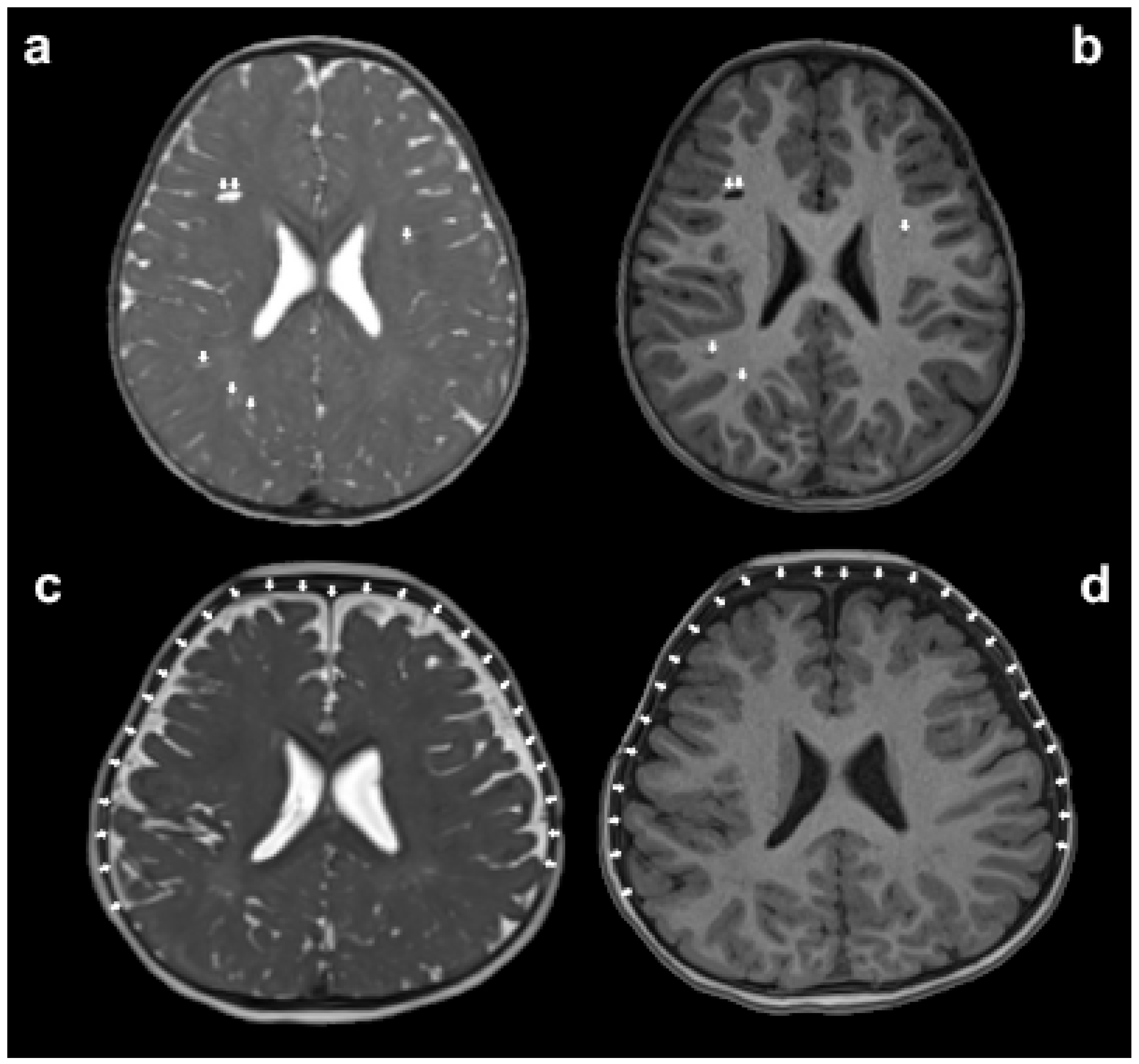
8. Glymphatic System Changes in ASD
9. Conclusions
10. Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rafiee, F.; Rezvani Habibabadi, R.; Motaghi, M.; Yousem, D.M.; Yousem, I.J. Brain MRI in Autism Spectrum Disorder: Narrative Review and Recent Advances. J. Magn. Reson. Imaging 2022, 55, 1613–1624. [Google Scholar] [CrossRef]
- Akhavan Aghdam, M.; Sharifi, A.; Pedram, M.M. Combination of rs-fMRI and sMRI Data to Discriminate Autism Spectrum Disorders in Young Children Using Deep Belief Network. J. Digit. Imaging 2018, 31, 895–903. [Google Scholar] [CrossRef]
- Maenner, M.J.; Warren, Z.; Williams, A.R.; Amoakohene, E.; Bakian, A.V.; Bilder, D.A.; Durkin, M.S.; Fitzgerald, R.T.; Furnier, S.M.; Hughes, M.M.; et al. Prevalence and Characteristics of Autism Spectrum Disorder Among Children Aged 8—Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2020. MMWR Surv. Summ. 2023, 72, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Rogge, N.; Janssen, J. The Economic Costs of Autism Spectrum Disorder: A Literature Review. J. Autism Dev. Disord. 2019, 49, 2873–2900. [Google Scholar] [CrossRef]
- Leigh, J.P.; Du, J. Brief Report: Forecasting the Economic Burden of Autism in 2015 and 2025 in the United States. J. Autism Dev. Disord. 2015, 45, 4135–4139. [Google Scholar] [CrossRef] [PubMed]
- Schumann, C.M.; Bloss, C.S.; Barnes, C.C.; Wideman, G.M.; Carper, R.A.; Akshoomoff, N.; Pierce, K.; Hagler, D.; Schork, N.; Lord, C.; et al. Longitudinal magnetic resonance imaging study of cortical development through early childhood in autism. J. Neurosci. 2010, 30, 4419–4427. [Google Scholar] [CrossRef]
- Tschida, J.E.; Yerys, B.E. A Systematic Review of the Positive Valence System in Autism Spectrum Disorder. Neuropsychol. Rev. 2021, 31, 58–88. [Google Scholar] [CrossRef]
- Weber, C.F.; Lake, E.M.R.; Haider, S.P.; Mozayan, A.; Mukherjee, P.; Scheinost, D.; Bamford, N.S.; Ment, L.; Constable, T.; Payabvash, S. Age-dependent white matter microstructural disintegrity in autism spectrum disorder. Front. Neurosci. 2022, 16, 957018. [Google Scholar] [CrossRef] [PubMed]
- Sharp, T.H.; Elsabbagh, M.; Pickles, A.; Bedford, R. The subcortical correlates of autistic traits in school-age children: A population-based neuroimaging study. Mol. Autism 2023, 14, 6. [Google Scholar] [CrossRef] [PubMed]
- Karunakaran, P.; Hamdan, Y.B. Early Prediction of Autism Spectrum Disorder by Computational Approaches to fMRI Analysis with Early Learning Technique. J. Artif. Intell. Capsul. Netw. 2020, 2, 207–216. [Google Scholar] [CrossRef]
- Xiao, Z.; Qiu, T.; Ke, X.; Xiao, X.; Xiao, T.; Liang, F.; Zou, B.; Huang, H.; Fang, H.; Chu, K.; et al. Autism spectrum disorder as early neurodevelopmental disorder: Evidence from the brain imaging abnormalities in 2–3 years old toddlers. J. Autism Dev. Disord. 2014, 44, 1633–1640. [Google Scholar] [CrossRef]
- Maier, S.; Düppers, A.L.; Runge, K.; Dacko, M.; Lange, T.; Fangmeier, T.; Riedel, A.; Ebert, D.; Endres, D.; Domschke, K.; et al. Increased prefrontal GABA concentrations in adults with autism spectrum disorders. Autism Res. 2022, 15, 1222–1236. [Google Scholar] [CrossRef]
- Wang, H.; Ma, Z.H.; Xu, L.Z.; Yang, L.; Ji, Z.Z.; Tang, X.Z.; Liu, J.R.; Li, X.; Cao, Q.J.; Liu, J. Developmental brain structural atypicalities in autism: A voxel-based morphometry analysis. Child. Adolesc. Psychiatry Ment. Health 2022, 16, 7. [Google Scholar] [CrossRef] [PubMed]
- Nickl-Jockschat, T.; Habel, U.; Michel, T.M.; Manning, J.; Laird, A.R.; Fox, P.T.; Schneider, F.; Eickhoff, S.B. Brain structure anomalies in autism spectrum disorder--a meta-analysis of VBM studies using anatomic likelihood estimation. Hum. Brain Mapp. 2012, 33, 1470–1489. [Google Scholar] [CrossRef] [PubMed]
- Hazlett, H.C.; Gu, H.; Munsell, B.C.; Kim, S.H.; Styner, M.; Wolff, J.J.; Elison, J.T.; Swanson, M.R.; Zhu, H.; Botteron, K.N.; et al. Early brain development in infants at high risk for autism spectrum disorder. Nature 2017, 542, 348–351. [Google Scholar] [CrossRef]
- Courchesne, E.; Pierce, K.; Schumann, C.M.; Redcay, E.; Buckwalter, J.A.; Kennedy, D.P.; Morgan, J. Mapping early brain development in autism. Neuron 2007, 56, 399–413. [Google Scholar] [CrossRef]
- Hazlett, H.C.; Poe, M.D.; Gerig, G.; Styner, M.; Chappell, C.; Smith, R.G.; Vachet, C.; Piven, J. Early brain overgrowth in autism associated with an increase in cortical surface area before age 2 years. Arch. Gen. Psychiatry 2011, 68, 467–476. [Google Scholar] [CrossRef]
- Ohta, H.; Nordahl, C.W.; Iosif, A.M.; Lee, A.; Rogers, S.; Amaral, D.G. Increased Surface Area, but not Cortical Thickness, in a Subset of Young Boys With Autism Spectrum Disorder. Autism Res. 2016, 9, 232–248. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Yao, L.; Zhang, W.; Xiao, Y.; Liu, L.; Gao, X.; Shah, C.; Li, S.; Tao, B.; Gong, Q.; et al. Gray matter abnormalities in pediatric autism spectrum disorder: A meta-analysis with signed differential mapping. Eur. Child. Adolesc. Psychiatry 2017, 26, 933–945. [Google Scholar] [CrossRef]
- Guo, X.; Duan, X.; Suckling, J.; Wang, J.; Kang, X.; Chen, H.; Biswal, B.B.; Cao, J.; He, C.; Xiao, J.; et al. Mapping Progressive Gray Matter Alterations in Early Childhood Autistic Brain. Cereb. Cortex 2021, 31, 1500–1510. [Google Scholar] [CrossRef]
- Bai, C.; Wang, Y.; Zhang, Y.; Wang, X.; Chen, Z.; Yu, W.; Zhang, H.; Li, X.; Zhu, K.; Wang, Y.; et al. Abnormal gray matter volume and functional connectivity patterns in social cognition-related brain regions of young children with autism spectrum disorder. Autism Res. 2023, 16, 1124–1137. [Google Scholar] [CrossRef] [PubMed]
- Retico, A.; Giuliano, A.; Tancredi, R.; Cosenza, A.; Apicella, F.; Narzisi, A.; Biagi, L.; Tosetti, M.; Muratori, F.; Calderoni, S. The effect of gender on the neuroanatomy of children with autism spectrum disorders: A support vector machine case-control study. Mol. Autism 2016, 7, 5. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Chen, M.H.; Li, G.; Wu, D.; Lian, C.; Sun, Q.; Rushmore, R.J.; Wang, L. Volumetric Analysis of Amygdala and Hippocampal Subfields for Infants with Autism. J. Autism Dev. Disord. 2023, 53, 2475–2489. [Google Scholar] [CrossRef]
- Reinhardt, V.P.; Iosif, A.M.; Libero, L.; Heath, B.; Rogers, S.J.; Ferrer, E.; Nordahl, C.; Ghetti, S.; Amaral, D.; Solomon, M. Understanding Hippocampal Development in Young Children With Autism Spectrum Disorder. J. Am. Acad. Child. Adolesc. Psychiatry 2020, 59, 1069–1079. [Google Scholar] [CrossRef] [PubMed]
- Shou, X.J.; Xu, X.J.; Zeng, X.Z.; Liu, Y.; Yuan, H.S.; Xing, Y.; Jia, M.X.; Wei, Q.Y.; Han, S.P.; Zhang, R.; et al. A Volumetric and Functional Connectivity MRI Study of Brain Arginine-Vasopressin Pathways in Autistic Children. Neurosci. Bull. 2017, 33, 130–142. [Google Scholar] [CrossRef]
- Mengotti, P.; D′Agostini, S.; Terlevic, R.; De Colle, C.; Biasizzo, E.; Londero, D.; Ferro, A.; Rambaldelli, G.; Balestrieri, M.; Zanini, S.; et al. Altered white matter integrity and development in children with autism: A combined voxel-based morphometry and diffusion imaging study. Brain Res. Bull. 2011, 84, 189–195. [Google Scholar] [CrossRef]
- Arutiunian, V.; Davydova, E.; Pereverzeva, D.; Sorokin, A.; Tyushkevich, S.; Mamokhina, U.; Danilina, K.; Dragoy, O. Reduced grey matter volume of amygdala and hippocampus is associated with the severity of autistic symptoms and language abilities in school-aged children with Autism Spectrum Disorder: An exploratory study. Brain Struct. Funct. 2023, 228, 1573–1579. [Google Scholar] [CrossRef]
- Sun, F.; Chen, Y.; Gao, Q.; Zhao, Z. Abnormal gray matter structure in children and adolescents with high-functioning autism spectrum disorder. Psychiatry Res. Neuroimaging 2022, 327, 111564. [Google Scholar] [CrossRef]
- Cloarec, R.; Riffault, B.; Dufour, A.; Rabiei, H.; Gouty-Colomer, L.A.; Dumon, C.; Guimond, D.; Bonifazi, P.; Eftekhari, S.; Lozovaya, N.; et al. Pyramidal neuron growth and increased hippocampal volume during labor and birth in autism. Sci. Adv. 2019, 5, eaav0394. [Google Scholar] [CrossRef]
- Becker, E.B.; Stoodley, C.J. Autism spectrum disorder and the cerebellum. Int. Rev. Neurobiol. 2013, 113, 1–34. [Google Scholar] [CrossRef]
- Pote, I.; Wang, S.; Sethna, V.; Blasi, A.; Daly, E.; Kuklisova-Murgasova, M.; Lloyd-Fox, S.; Mercure, E.; Busuulwa, P.; Stoencheva, V.; et al. Familial risk of autism alters subcortical and cerebellar brain anatomy in infants and predicts the emergence of repetitive behaviors in early childhood. Autism Res. 2019, 12, 614–627. [Google Scholar] [CrossRef] [PubMed]
- Yu, K.K.; Cheung, C.; Chua, S.E.; McAlonan, G.M. Can Asperger syndrome be distinguished from autism? An anatomic likelihood meta-analysis of MRI studies. J. Psychiatry Neurosci. 2011, 36, 412–421. [Google Scholar] [CrossRef] [PubMed]
- Cauda, F.; Geda, E.; Sacco, K.; D′Agata, F.; Duca, S.; Geminiani, G.; Keller, R. Grey matter abnormality in autism spectrum disorder: An activation likelihood estimation meta-analysis study. J. Neurol. Neurosurg. Psychiatry 2011, 82, 1304–1313. [Google Scholar] [CrossRef] [PubMed]
- Berretz, G.; Wolf, O.T.; Gunturkun, O.; Ocklenburg, S. Atypical lateralization in neurodevelopmental and psychiatric disorders: What is the role of stress? Cortex 2020, 125, 215–232. [Google Scholar] [CrossRef]
- Cermak, C.A.; Arshinoff, S.; Ribeiro de Oliveira, L.; Tendera, A.; Beal, D.S.; Brian, J.; Anagnostou, E.; Sanjeevan, T. Brain and Language Associations in Autism Spectrum Disorder: A Scoping Review. J. Autism Dev. Disord. 2022, 52, 725–737. [Google Scholar] [CrossRef]
- Braden, B.B.; Riecken, C. Thinning Faster? Age-Related Cortical Thickness Differences in Adults with Autism Spectrum Disorder. Res. Autism Spectr. Disord. 2019, 64, 31–38. [Google Scholar] [CrossRef]
- van Rooij, D.; Anagnostou, E.; Arango, C.; Auzias, G.; Behrmann, M.; Busatto, G.F.; Calderoni, S.; Daly, E.; Deruelle, C.; Di Martino, A.; et al. Cortical and Subcortical Brain Morphometry Differences Between Patients With Autism Spectrum Disorder and Healthy Individuals Across the Lifespan: Results From the ENIGMA ASD Working Group. Am. J. Psychiatry 2018, 175, 359–369. [Google Scholar] [CrossRef]
- Nunes, A.S.; Vakorin, V.A.; Kozhemiako, N.; Peatfield, N.; Ribary, U.; Doesburg, S.M. Atypical age-related changes in cortical thickness in autism spectrum disorder. Sci. Rep. 2020, 10, 11067. [Google Scholar] [CrossRef]
- Zielinski, B.A.; Prigge, M.B.; Nielsen, J.A.; Froehlich, A.L.; Abildskov, T.J.; Anderson, J.S.; Fletcher, P.T.; Zygmunt, K.M.; Travers, B.G.; Lange, N. Longitudinal changes in cortical thickness in autism and typical development. Brain 2014, 137, 1799–1812. [Google Scholar] [CrossRef]
- Doyle-Thomas, K.A.; Duerden, E.G.; Taylor, M.J.; Lerch, J.P.; Soorya, L.V.; Wang, A.T.; Fan, J.; Hollander, E.; Anagnostou, E. Effects of age and symptomatology on cortical thickness in autism spectrum disorders. Res. Autism Spectr. Disord. 2013, 7, 141–150. [Google Scholar] [CrossRef]
- Prigge, M.B.; Bigler, E.D.; Travers, B.G.; Froehlich, A.; Abildskov, T.; Anderson, J.S.; Alexander, A.L.; Lange, N.; Lainhart, J.E.; Zielinski, B.A. Social Responsiveness Scale (SRS) in Relation to Longitudinal Cortical Thickness Changes in Autism Spectrum Disorder. J. Autism Dev. Disord. 2018, 48, 3319–3329. [Google Scholar] [CrossRef] [PubMed]
- Shiohama, T.; Ortug, A.; Warren, J.L.A.; Valli, B.; Levman, J.; Faja, S.K.; Tsujimura, K.; Maunakea, A.K.; Takahashi, E. Small Nucleus Accumbens and Large Cerebral Ventricles in Infants and Toddlers Prior to Receiving Diagnoses of Autism Spectrum Disorder. Cereb. Cortex 2022, 32, 1200–1211. [Google Scholar] [CrossRef] [PubMed]
- Sussman, D.; Leung, R.C.; Vogan, V.M.; Lee, W.; Trelle, S.; Lin, S.; Cassel, D.B.; Chakravarty, M.M.; Lerch, J.P.; Anagnostou, E.; et al. The autism puzzle: Diffuse but not pervasive neuroanatomical abnormalities in children with ASD. Neuroimage Clin. 2015, 8, 170–179. [Google Scholar] [CrossRef] [PubMed]
- Postema, M.C.; van Rooij, D.; Anagnostou, E.; Arango, C.; Auzias, G.; Behrmann, M.; Filho, G.B.; Calderoni, S.; Calvo, R.; Daly, E.; et al. Altered structural brain asymmetry in autism spectrum disorder in a study of 54 datasets. Nat. Commun. 2019, 10, 4958. [Google Scholar] [CrossRef]
- Nielsen, J.A.; Zielinski, B.A.; Fletcher, P.T.; Alexander, A.L.; Lange, N.; Bigler, E.D.; Lainhart, J.E.; Anderson, J.S. Abnormal lateralization of functional connectivity between language and default mode regions in autism. Mol. Autism 2014, 5, 8. [Google Scholar] [CrossRef]
- Ni, H.C.; Lin, H.Y.; Chen, Y.C.; Tseng, W.I.; Gau, S.S. Boys with autism spectrum disorder have distinct cortical folding patterns underpinning impaired self-regulation: A surface-based morphometry study. Brain Imaging Behav. 2020, 14, 2464–2476. [Google Scholar] [CrossRef]
- Ecker, C.; Bookheimer, S.Y.; Murphy, D.G. Neuroimaging in autism spectrum disorder: Brain structure and function across the lifespan. Lancet Neurol. 2015, 14, 1121–1134. [Google Scholar] [CrossRef]
- Kohli, J.S.; Kinnear, M.K.; Fong, C.H.; Fishman, I.; Carper, R.A.; Muller, R.A. Local Cortical Gyrification is Increased in Children With Autism Spectrum Disorders, but Decreases Rapidly in Adolescents. Cereb. Cortex 2019, 29, 2412–2423. [Google Scholar] [CrossRef]
- Yang, D.Y.; Beam, D.; Pelphrey, K.A.; Abdullahi, S.; Jou, R.J. Cortical morphological markers in children with autism: A structural magnetic resonance imaging study of thickness, area, volume, and gyrification. Mol. Autism 2016, 7, 11. [Google Scholar] [CrossRef]
- Libero, L.E.; DeRamus, T.P.; Deshpande, H.D.; Kana, R.K. Surface-based morphometry of the cortical architecture of autism spectrum disorders: Volume, thickness, area, and gyrification. Neuropsychologia 2014, 62, 1–10. [Google Scholar] [CrossRef]
- Ning, M.; Li, C.; Gao, L.; Fan, J. Core-Symptom-Defined Cortical Gyrification Differences in Autism Spectrum Disorder. Front. Psychiatry 2021, 12, 619367. [Google Scholar] [CrossRef] [PubMed]
- Alemany, S.; Blok, E.; Jansen, P.R.; Muetzel, R.L.; White, T. Brain morphology, autistic traits, and polygenic risk for autism: A population-based neuroimaging study. Autism Res. 2021, 14, 2085–2099. [Google Scholar] [CrossRef]
- Zoltowski, A.R.; Lyu, I.; Failla, M.; Mash, L.E.; Dunham, K.; Feldman, J.I.; Woynaroski, T.G.; Wallace, M.T.; Barquero, L.A.; Nguyen, T.Q.; et al. Cortical Morphology in Autism: Findings from a Cortical Shape-Adaptive Approach to Local Gyrification Indexing. Cereb. Cortex 2021, 31, 5188–5205. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Chen, M.; Li, Y.; Gao, Y.; Li, Y.; Cai, S.; Wang, J. Multisite Autism Spectrum Disorder Classification Using Convolutional Neural Network Classifier and Individual Morphological Brain Networks. Front. Neurosci. 2020, 14, 629630. [Google Scholar] [CrossRef] [PubMed]
- ElNakieb, Y.; Ali, M.T.; Elnakib, A.; Shalaby, A.; Soliman, A.; Mahmoud, A.; Ghazal, M.; Barnes, G.N.; El-Baz, A. The Role of Diffusion Tensor MR Imaging (DTI) of the Brain in Diagnosing Autism Spectrum Disorder: Promising Results. Sensors 2021, 21, 8171. [Google Scholar] [CrossRef]
- Solso, S.; Xu, R.; Proudfoot, J.; Hagler, D.J., Jr.; Campbell, K.; Venkatraman, V.; Carter Barnes, C.; Ahrens-Barbeau, C.; Pierce, K.; Dale, A.; et al. Diffusion Tensor Imaging Provides Evidence of Possible Axonal Overconnectivity in Frontal Lobes in Autism Spectrum Disorder Toddlers. Biol. Psychiatry 2016, 79, 676–684. [Google Scholar] [CrossRef]
- Ouyang, M.; Cheng, H.; Mishra, V.; Gong, G.; Mosconi, M.W.; Sweeney, J.; Peng, Y.; Huang, H. Atypical age-dependent effects of autism on white matter microstructure in children of 2–7 years. Hum. Brain Mapp. 2016, 37, 819–832. [Google Scholar] [CrossRef]
- Andrews, D.S.; Lee, J.K.; Harvey, D.J.; Waizbard-Bartov, E.; Solomon, M.; Rogers, S.J.; Nordahl, C.W.; Amaral, D.G. A Longitudinal Study of White Matter Development in Relation to Changes in Autism Severity Across Early Childhood. Biol. Psychiatry 2021, 89, 424–432. [Google Scholar] [CrossRef]
- Andrews, D.S.; Lee, J.K.; Solomon, M.; Rogers, S.J.; Amaral, D.G.; Nordahl, C.W. A diffusion-weighted imaging tract-based spatial statistics study of autism spectrum disorder in preschool-aged children. J. Neurodev. Disord. 2019, 11, 32. [Google Scholar] [CrossRef]
- Chen, B.; Linke, A.; Olson, L.; Kohli, J.; Kinnear, M.; Sereno, M.; Muller, R.A.; Carper, R.; Fishman, I. Cortical myelination in toddlers and preschoolers with autism spectrum disorder. Dev. Neurobiol. 2022, 82, 261–274. [Google Scholar] [CrossRef]
- Travers, B.G.; Adluru, N.; Ennis, C.; Tromp, D.P.; Destiche, D.; Doran, S.; Bigler, E.D.; Lange, N.; Lainhart, J.E.; Alexander, A.L. Diffusion tensor imaging in autism spectrum disorder: A review. Autism Res. 2012, 5, 289–313. [Google Scholar] [CrossRef] [PubMed]
- Fu, L.; Li, C.; Li, Y.; Cheng, X.; Cui, X.; Jiang, J.; Ding, N.; Fang, H.; Tang, T.; Ke, X. Heritability of abnormalities in limbic networks of autism spectrum disorder children: Evidence from an autism spectrum disorder twin study. Autism Res. 2022, 15, 628–640. [Google Scholar] [CrossRef] [PubMed]
- Hanaie, R.; Mohri, I.; Kagitani-Shimono, K.; Tachibana, M.; Azuma, J.; Matsuzaki, J.; Watanabe, Y.; Fujita, N.; Taniike, M. Altered microstructural connectivity of the superior cerebellar peduncle is related to motor dysfunction in children with autistic spectrum disorders. Cerebellum 2013, 12, 645–656. [Google Scholar] [CrossRef] [PubMed]
- Hrdlicka, M.; Sanda, J.; Urbanek, T.; Kudr, M.; Dudova, I.; Kickova, S.; Pospisilova, L.; Mohaplova, M.; Maulisova, A.; Krsek, P.; et al. Diffusion Tensor Imaging And Tractography In Autistic, Dysphasic, And Healthy Control Children. Neuropsychiatr. Dis. Treat. 2019, 15, 2843–2852. [Google Scholar] [CrossRef]
- Lei, J.; Lecarie, E.; Jurayj, J.; Boland, S.; Sukhodolsky, D.G.; Ventola, P.; Pelphrey, K.A.; Jou, R.J. Altered Neural Connectivity in Females, But Not Males with Autism: Preliminary Evidence for the Female Protective Effect from a Quality-Controlled Diffusion Tensor Imaging Study. Autism Res. 2019, 12, 1472–1483. [Google Scholar] [CrossRef]
- Weinstein, M.; Ben-Sira, L.; Levy, Y.; Zachor, D.A.; Ben Itzhak, E.; Artzi, M.; Tarrasch, R.; Eksteine, P.M.; Hendler, T.; Ben Bashat, D. Abnormal white matter integrity in young children with autism. Hum. Brain Mapp. 2011, 32, 534–543. [Google Scholar] [CrossRef] [PubMed]
- Fingher, N.; Dinstein, I.; Ben-Shachar, M.; Haar, S.; Dale, A.M.; Eyler, L.; Pierce, K.; Courchesne, E. Toddlers later diagnosed with autism exhibit multiple structural abnormalities in temporal corpus callosum fibers. Cortex 2017, 97, 291–305. [Google Scholar] [CrossRef]
- Fletcher, P.T.; Whitaker, R.T.; Tao, R.; DuBray, M.B.; Froehlich, A.; Ravichandran, C.; Alexander, A.L.; Bigler, E.D.; Lange, N.; Lainhart, J.E. Microstructural connectivity of the arcuate fasciculus in adolescents with high-functioning autism. Neuroimage 2010, 51, 1117–1125. [Google Scholar] [CrossRef]
- Peterson, D.; Mahajan, R.; Crocetti, D.; Mejia, A.; Mostofsky, S. Left-hemispheric microstructural abnormalities in children with high-functioning autism spectrum disorder. Autism Res. 2015, 8, 61–72. [Google Scholar] [CrossRef]
- Walker, L.; Gozzi, M.; Lenroot, R.; Thurm, A.; Behseta, B.; Swedo, S.; Pierpaoli, C. Diffusion tensor imaging in young children with autism: Biological effects and potential confounds. Biol. Psychiatry 2012, 72, 1043–1051. [Google Scholar] [CrossRef]
- Conti, E.; Calderoni, S.; Gaglianese, A.; Pannek, K.; Mazzotti, S.; Rose, S.; Scelfo, D.; Tosetti, M.; Muratori, F.; Cioni, G.; et al. Lateralization of Brain Networks and Clinical Severity in Toddlers with Autism Spectrum Disorder: A HARDI Diffusion MRI Study. Autism Res. 2016, 9, 382–392. [Google Scholar] [CrossRef] [PubMed]
- Fu, L.; Wang, Y.; Fang, H.; Xiao, X.; Xiao, T.; Li, Y.; Li, C.; Wu, Q.; Chu, K.; Xiao, C.; et al. Longitudinal Study of Brain Asymmetries in Autism and Developmental Delays Aged 2–5 years. Neuroscience 2020, 432, 137–149. [Google Scholar] [CrossRef] [PubMed]
- Qin, B.; Wang, L.; Zhang, Y.; Cai, J.; Chen, J.; Li, T. Enhanced Topological Network Efficiency in Preschool Autism Spectrum Disorder: A Diffusion Tensor Imaging Study. Front. Psychiatry 2018, 9, 278. [Google Scholar] [CrossRef]
- Li, S.J.; Wang, Y.; Qian, L.; Liu, G.; Liu, S.F.; Zou, L.P.; Zhang, J.S.; Hu, N.; Chen, X.Q.; Yu, S.Y.; et al. Alterations of White Matter Connectivity in Preschool Children with Autism Spectrum Disorder. Radiology 2018, 288, 209–217. [Google Scholar] [CrossRef]
- Qian, L.; Li, Y.; Wang, Y.; Wang, Y.; Cheng, X.; Li, C.; Cui, X.; Jiao, G.; Ke, X. Shared and Distinct Topologically Structural Connectivity Patterns in Autism Spectrum Disorder and Attention-Deficit/Hyperactivity Disorder. Front. Neurosci. 2021, 15, 664363. [Google Scholar] [CrossRef] [PubMed]
- Cai, Y.; Zhao, J.; Wang, L.; Xie, Y.; Fan, X. Altered topological properties of white matter structural network in adults with autism spectrum disorder. Asian J. Psychiatry 2022, 75, 103211. [Google Scholar] [CrossRef]
- Qian, L.; Wang, Y.; Chu, K.; Li, Y.; Xiao, C.; Xiao, T.; Xiao, X.; Qiu, T.; Xiao, Y.; Fang, H.; et al. Alterations in hub organization in the white matter structural network in toddlers with autism spectrum disorder: A 2-year follow-up study. Autism Res. 2018, 11, 1218–1228. [Google Scholar] [CrossRef]
- Li, C.; Li, Y.; Fu, L.; Wang, Y.; Cheng, X.; Cui, X.; Jiang, J.; Xiao, T.; Ke, X.; Fang, H. The relationships between the topological properties of the whole-brain white matter network and the severity of autism spectrum disorder: A study from monozygotic twins. Neuroscience 2021, 465, 60–70. [Google Scholar] [CrossRef]
- Kim, J.I.; Bang, S.; Yang, J.J.; Kwon, H.; Jang, S.; Roh, S.; Kim, S.H.; Kim, M.J.; Lee, H.J.; Lee, J.M.; et al. Classification of Preschoolers with Low-Functioning Autism Spectrum Disorder Using Multimodal MRI Data. J. Autism Dev. Disord. 2023, 53, 25–37. [Google Scholar] [CrossRef]
- Helmy, E.; Elnakib, A.; ElNakieb, Y.; Khudri, M.; Abdelrahim, M.; Yousaf, J.; Ghazal, M.; Contractor, S.; Barnes, G.N.; El-Baz, A. Role of Artificial Intelligence for Autism Diagnosis Using DTI and fMRI: A Survey. Biomedicines 2023, 11, 1858. [Google Scholar] [CrossRef]
- Yan, W.; Rangaprakash, D.; Deshpande, G. Aberrant hemodynamic responses in autism: Implications for resting state fMRI functional connectivity studies. NeuroImage Clin. 2018, 19, 320–330. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Zhang, K.; He, X.; Zhou, J.; Jin, C.; Shen, L.; Gao, Y.; Tian, M.; Zhang, H. Structural, Functional, and Molecular Imaging of Autism Spectrum Disorder. Neurosci. Bull. 2021, 37, 1051–1071. [Google Scholar] [CrossRef] [PubMed]
- Holiga, Š.; Hipp, J.F.; Chatham, C.H.; Garces, P.; Spooren, W.; D′Ardhuy, X.L.; Bertolino, A.; Bouquet, C.; Buitelaar, J.K.; Bours, C.; et al. Patients with autism spectrum disorders display reproducible functional connectivity alterations. Sci. Transl. Med. 2019, 11, eaat9223. [Google Scholar] [CrossRef] [PubMed]
- Buckner, R.L.; Andrews-Hanna, J.R.; Schacter, D.L. The brain′s default network: Anatomy, function, and relevance to disease. Ann. N. Y. Acad. Sci. 2008, 1124, 1–38. [Google Scholar] [CrossRef]
- Menon, V.; Uddin, L.Q. Saliency, switching, attention and control: A network model of insula function. Brain Struct. Funct. 2010, 214, 655–667. [Google Scholar] [CrossRef]
- Seeley, W.W. The Salience Network: A Neural System for Perceiving and Responding to Homeostatic Demands. J. Neurosci. 2019, 39, 9878–9882. [Google Scholar] [CrossRef]
- Seeley, W.W.; Menon, V.; Schatzberg, A.F.; Keller, J.; Glover, G.H.; Kenna, H.; Reiss, A.L.; Greicius, M.D. Dissociable intrinsic connectivity networks for salience processing and executive control. J. Neurosci. 2007, 27, 2349–2356. [Google Scholar] [CrossRef]
- Spreng, R.N.; Sepulcre, J.; Turner, G.R.; Stevens, W.D.; Schacter, D.L. Intrinsic architecture underlying the relations among the default, dorsal attention, and frontoparietal control networks of the human brain. J. Cogn. Neurosci. 2013, 25, 74–86. [Google Scholar] [CrossRef]
- Burrows, C.A.; Laird, A.R.; Uddin, L.Q. Functional connectivity of brain regions for self- and other-evaluation in children, adolescents and adults with autism. Dev. Sci. 2016, 19, 564–580. [Google Scholar] [CrossRef]
- Haghighat, H.; Mirzarezaee, M.; Araabi, B.N.; Khadem, A. Functional Networks Abnormalities in Autism Spectrum Disorder: Age-Related Hypo and Hyper Connectivity. Brain Topogr. 2021, 34, 306–322. [Google Scholar] [CrossRef]
- Xiao, Y.; Wen, T.H.; Kupis, L.; Eyler, L.T.; Taluja, V.; Troxel, J.; Goel, D.; Lombardo, M.V.; Pierce, K.; Courchesne, E. Atypical functional connectivity of temporal cortex with precuneus and visual regions may be an early-age signature of ASD. Mol. Autism 2023, 14, 11. [Google Scholar] [CrossRef] [PubMed]
- McKinnon, C.J.; Eggebrecht, A.T.; Todorov, A.; Wolff, J.J.; Elison, J.T.; Adams, C.M.; Snyder, A.Z.; Estes, A.M.; Zwaigenbaum, L.; Botteron, K.N.; et al. Restricted and Repetitive Behavior and Brain Functional Connectivity in Infants at Risk for Developing Autism Spectrum Disorder. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 2019, 4, 50–61. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.; Linke, A.; Olson, L.; Ibarra, C.; Reynolds, S.; Müller, R.A.; Kinnear, M.; Fishman, I. Greater functional connectivity between sensory networks is related to symptom severity in toddlers with autism spectrum disorder. J. Child. Psychol. Psychiatry 2021, 62, 160–170. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Wang, J.; Uddin, L.Q.; Wang, X.; Guo, X.; Lu, F.; Duan, X.; Wu, L.; Chen, H. Aberrant functional connectivity of neural circuits associated with social and sensorimotor deficits in young children with autism spectrum disorder. Autism Res. 2018, 11, 1643–1652. [Google Scholar] [CrossRef] [PubMed]
- Uddin, L.Q.; Supekar, K.; Menon, V. Reconceptualizing functional brain connectivity in autism from a developmental perspective. Front. Hum. Neurosci. 2013, 7, 458. [Google Scholar] [CrossRef] [PubMed]
- Nomi, J.S.; Uddin, L.Q. Developmental changes in large-scale network connectivity in autism. Neuroimage Clin. 2015, 7, 732–741. [Google Scholar] [CrossRef]
- Farrant, K.; Uddin, L.Q. Atypical developmental of dorsal and ventral attention networks in autism. Dev. Sci. 2016, 19, 550–563. [Google Scholar] [CrossRef]
- Nunes, A.S.; Peatfield, N.; Vakorin, V.; Doesburg, S.M. Idiosyncratic organization of cortical networks in autism spectrum disorder. Neuroimage 2019, 190, 182–190. [Google Scholar] [CrossRef]
- Yerys, B.E.; Gordon, E.M.; Abrams, D.N.; Satterthwaite, T.D.; Weinblatt, R.; Jankowski, K.F.; Strang, J.; Kenworthy, L.; Gaillard, W.D.; Vaidya, C.J. Default mode network segregation and social deficits in autism spectrum disorder: Evidence from non-medicated children. Neuroimage Clin. 2015, 9, 223–232. [Google Scholar] [CrossRef]
- Yerys, B.E.; Herrington, J.D.; Satterthwaite, T.D.; Guy, L.; Schultz, R.T.; Bassett, D.S. Globally weaker and topologically different: Resting-state connectivity in youth with autism. Mol. Autism 2017, 8, 39. [Google Scholar] [CrossRef]
- Morgan, B.R.; Ibrahim, G.M.; Vogan, V.M.; Leung, R.C.; Lee, W.; Taylor, M.J. Characterization of Autism Spectrum Disorder across the Age Span by Intrinsic Network Patterns. Brain Topogr. 2019, 32, 461–471. [Google Scholar] [CrossRef] [PubMed]
- Ilioska, I.; Oldehinkel, M.; Llera, A.; Chopra, S.; Looden, T.; Chauvin, R.; Van Rooij, D.; Floris, D.L.; Tillmann, J.; Moessnang, C.; et al. Connectome-wide Mega-analysis Reveals Robust Patterns of Atypical Functional Connectivity in Autism. Biol. Psychiatry 2023, 94, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Abbott, A.E.; Nair, A.; Keown, C.L.; Datko, M.; Jahedi, A.; Fishman, I.; Muller, R.A. Patterns of Atypical Functional Connectivity and Behavioral Links in Autism Differ Between Default, Salience, and Executive Networks. Cereb. Cortex 2016, 26, 4034–4045. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Huang, H. Alterations of functional connectivities associated with autism spectrum disorder symptom severity: A multi-site study using multivariate pattern analysis. Sci. Rep. 2020, 10, 4330. [Google Scholar] [CrossRef]
- Monk, C.S.; Peltier, S.J.; Wiggins, J.L.; Weng, S.J.; Carrasco, M.; Risi, S.; Lord, C. Abnormalities of intrinsic functional connectivity in autism spectrum disorders. Neuroimage 2009, 47, 764–772. [Google Scholar] [CrossRef]
- von dem Hagen, E.A.; Stoyanova, R.S.; Baron-Cohen, S.; Calder, A.J. Reduced functional connectivity within and between ′social′ resting state networks in autism spectrum conditions. Soc. Cogn. Affect. Neurosci. 2013, 8, 694–701. [Google Scholar] [CrossRef]
- Dickie, E.W.; Ameis, S.H.; Shahab, S.; Calarco, N.; Smith, D.E.; Miranda, D.; Viviano, J.D.; Voineskos, A.N. Personalized Intrinsic Network Topography Mapping and Functional Connectivity Deficits in Autism Spectrum Disorder. Biol. Psychiatry 2018, 84, 278–286. [Google Scholar] [CrossRef]
- Lorenzini, L.; van Wingen, G.; Cerliani, L. Atypically high influence of subcortical activity on primary sensory regions in autism. Neuroimage Clin. 2021, 32, 102839. [Google Scholar] [CrossRef]
- Oldehinkel, M.; Mennes, M.; Marquand, A.; Charman, T.; Tillmann, J.; Ecker, C.; Dell′Acqua, F.; Brandeis, D.; Banaschewski, T.; Baumeister, S.; et al. Altered Connectivity Between Cerebellum, Visual, and Sensory-Motor Networks in Autism Spectrum Disorder: Results from the EU-AIMS Longitudinal European Autism Project. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 2019, 4, 260–270. [Google Scholar] [CrossRef]
- Sha, Z.; van Rooij, D.; Anagnostou, E.; Arango, C.; Auzias, G.; Behrmann, M.; Bernhardt, B.; Bolte, S.; Busatto, G.F.; Calderoni, S.; et al. Subtly altered topological asymmetry of brain structural covariance networks in autism spectrum disorder across 43 datasets from the ENIGMA consortium. Mol. Psychiatry 2022, 27, 2114–2125. [Google Scholar] [CrossRef]
- Floris, D.L.; Barber, A.D.; Nebel, M.B.; Martinelli, M.; Lai, M.C.; Crocetti, D.; Baron-Cohen, S.; Suckling, J.; Pekar, J.J.; Mostofsky, S.H. Atypical lateralization of motor circuit functional connectivity in children with autism is associated with motor deficits. Mol. Autism 2016, 7, 35. [Google Scholar] [CrossRef]
- Sylvester, C.M.; Kaplan, S.; Myers, M.J.; Gordon, E.M.; Schwarzlose, R.F.; Alexopoulos, D.; Nielsen, A.N.; Kenley, J.K.; Meyer, D.; Yu, Q. Network-specific selectivity of functional connections in the neonatal brain. Cereb. Cortex 2023, 33, 2200–2214. [Google Scholar] [CrossRef] [PubMed]
- Du, Y.; He, X.; Kochunov, P.; Pearlson, G.; Hong, L.E.; van Erp, T.G.M.; Belger, A.; Calhoun, V.D. A new multimodality fusion classification approach to explore the uniqueness of schizophrenia and autism spectrum disorder. Hum. Brain Mapp. 2022, 43, 3887–3903. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.; Liu, X.; Ran, Q.; Nie, L.; Wu, L.; Pan, Z.; He, L. Application of Three-Dimensional Pseudocontinuous Arterial Spin Labeling Perfusion Imaging in the Brains of Children With Autism. Front. Neurol. 2022, 13, 851430. [Google Scholar] [CrossRef]
- Ye, F.; Du, L.; Liu, B.; Gao, X.; Yang, A.; Liu, D.; Chen, Y.; Lv, K.; Xu, P.; Chen, Y.; et al. Application of pseudocontinuous arterial spin labeling perfusion imaging in children with autism spectrum disorders. Front. Neurosci. 2022, 16, 1045585. [Google Scholar] [CrossRef] [PubMed]
- Mori, T.; Ito, H.; Harada, M.; Hisaoka, S.; Matsumoto, Y.; Goji, A.; Toda, Y.; Mori, K.; Kagami, S. Multi-delay arterial spin labeling brain magnetic resonance imaging study for pediatric autism. Brain Dev. 2020, 42, 315–321. [Google Scholar] [CrossRef]
- Tang, S.L.; Nie, L.S.; Liu, X.F.; Chen, Z.; Zhou, Y.; Pan, Z.X.; He, L. Application of Quantitative Magnetic Resonance Imaging in the Diagnosis of Autism in Children. Front. Med. 2022, 9, 12. [Google Scholar] [CrossRef] [PubMed]
- Mori, K.; Toda, Y.; Ito, H.; Mori, T.; Goji, A.; Fujii, E.; Miyazaki, M.; Harada, M.; Kagami, S. A proton magnetic resonance spectroscopic study in autism spectrum disorders: Amygdala and orbito-frontal cortex. Brain Dev. 2013, 35, 139–145. [Google Scholar] [CrossRef]
- Goji, A.; Ito, H.; Mori, K.; Harada, M.; Hisaoka, S.; Toda, Y.; Mori, T.; Abe, Y.; Miyazaki, M.; Kagami, S. Assessment of Anterior Cingulate Cortex (ACC) and Left Cerebellar Metabolism in Asperger′s Syndrome with Proton Magnetic Resonance Spectroscopy (MRS). PLoS ONE 2017, 12, e0169288. [Google Scholar] [CrossRef]
- Margari, L.; De Giacomo, A.; Craig, F.; Palumbi, R.; Peschechera, A.; Margari, M.; Picardi, F.; Caldarola, M.; Maghenzani, M.A.; Dicuonzo, F. Frontal lobe metabolic alterations in autism spectrum disorder: A (1)H-magnetic resonance spectroscopy study. Neuropsychiatr. Dis. Treat. 2018, 14, 1871–1876. [Google Scholar] [CrossRef]
- DeMayo, M.M.; Harris, A.D.; Song, Y.J.C.; Pokorski, I.; Thapa, R.; Patel, S.; Ambarchi, Z.; Thomas, E.E.; Hickie, I.B.; Guastella, A.J. Age-related parietal GABA alterations in children with autism spectrum disorder. Autism Res. 2021, 14, 859–872. [Google Scholar] [CrossRef] [PubMed]
- Ito, H.; Mori, K.; Harada, M.; Hisaoka, S.; Toda, Y.; Mori, T.; Goji, A.; Abe, Y.; Miyazaki, M.; Kagami, S. A Proton Magnetic Resonance Spectroscopic Study in Autism Spectrum Disorder Using a 3-Tesla Clinical Magnetic Resonance Imaging (MRI) System: The Anterior Cingulate Cortex and the Left Cerebellum. J. Child. Neurol. 2017, 32, 731–739. [Google Scholar] [CrossRef]
- Yerys, B.E.; Herrington, J.D.; Bartley, G.K.; Liu, H.S.; Detre, J.A.; Schultz, R.T. Arterial spin labeling provides a reliable neurobiological marker of autism spectrum disorder. J. Neurodev. Disord. 2018, 10, 32. [Google Scholar] [CrossRef] [PubMed]
- Jann, K.; Hernandez, L.M.; Beck-Pancer, D.; McCarron, R.; Smith, R.X.; Dapretto, M.; Wang, D.J. Altered resting perfusion and functional connectivity of default mode network in youth with autism spectrum disorder. Brain Behav. 2015, 5, e00358. [Google Scholar] [CrossRef] [PubMed]
- Peterson, B.S.; Zargarian, A.; Peterson, J.B.; Goh, S.; Sawardekar, S.; Williams, S.C.R.; Lythgoe, D.J.; Zelaya, F.O.; Bansal, R. Hyperperfusion of Frontal White and Subcortical Gray Matter in Autism Spectrum Disorder. Biol. Psychiatry 2019, 85, 584–595. [Google Scholar] [CrossRef]
- Liang, X.; Zou, Q.; He, Y.; Yang, Y. Coupling of functional connectivity and regional cerebral blood flow reveals a physiological basis for network hubs of the human brain. Proc. Natl. Acad. Sci. USA 2013, 110, 1929–1934. [Google Scholar] [CrossRef]
- Du, Y.; Chen, L.; Yan, M.C.; Wang, Y.L.; Zhong, X.L.; Xv, C.X.; Li, Y.B.; Cheng, Y. Neurometabolite levels in the brains of patients with autism spectrum disorders: A meta-analysis of proton magnetic resonance spectroscopy studies (N = 1501). Mol. Psychiatry, 2023; online ahead of print. [Google Scholar] [CrossRef]
- Kang, Q.Q.; Li, X.; Tong, G.L.; Fan, Y.L.; Shi, L. Magnetic resonance spectroscopy features of the thalamus and the cerebellum and their association with clinical features in children with autism spectrum disorder: A prospective study. Zhongguo Dang Dai Er Ke Za Zhi 2021, 23, 1250–1255. [Google Scholar] [CrossRef]
- Mori, K.; Toda, Y.; Ito, H.; Mori, T.; Mori, K.; Goji, A.; Hashimoto, H.; Tani, H.; Miyazaki, M.; Harada, M.; et al. Neuroimaging in autism spectrum disorders- 1H-MRS and NIRS study. J. Med. Investig. 2015, 62, 29–36. [Google Scholar] [CrossRef][Green Version]
- Hegarty, J.P., II; Gu, M.; Spielman, D.M.; Cleveland, S.C.; Hallmayer, J.F.; Lazzeroni, L.C.; Raman, M.M.; Frazier, T.W.; Phillips, J.M.; Reiss, A.L.; et al. A proton MR spectroscopy study of the thalamus in twins with autism spectrum disorder. Prog. Neuropsychopharmacol. Biol. Psychiatry 2018, 81, 153–160. [Google Scholar] [CrossRef]
- Jimenez-Espinoza, C.; Marcano Serrano, F.; Gonzalez-Mora, J.L. N-Acetylaspartyl-Glutamate Metabolism in the Cingulated Cortices as a Biomarker of the Etiology in ASD: A (1)H-MRS Model. Molecules 2021, 26, 675. [Google Scholar] [CrossRef]
- Ford, T.C.; Crewther, D.P. A Comprehensive Review of the (1)H-MRS Metabolite Spectrum in Autism Spectrum Disorder. Front. Mol. Neurosci. 2016, 9, 14. [Google Scholar] [CrossRef] [PubMed]
- Hardan, A.Y.; Fung, L.K.; Frazier, T.; Berquist, S.W.; Minshew, N.J.; Keshavan, M.S.; Stanley, J.A. A proton spectroscopy study of white matter in children with autism. Prog. Neuropsychopharmacol. Biol. Psychiatry 2016, 66, 48–53. [Google Scholar] [CrossRef]
- Puts, N.A.J.; Wodka, E.L.; Harris, A.D.; Crocetti, D.; Tommerdahl, M.; Mostofsky, S.H.; Edden, R.A.E. Reduced GABA and altered somatosensory function in children with autism spectrum disorder. Autism Res. 2017, 10, 608–619. [Google Scholar] [CrossRef] [PubMed]
- Brix, M.K.; Ersland, L.; Hugdahl, K.; Gruner, R.; Posserud, M.B.; Hammar, A.; Craven, A.R.; Noeske, R.; Evans, C.J.; Walker, H.B.; et al. Brain MR spectroscopy in autism spectrum disorder-the GABA excitatory/inhibitory imbalance theory revisited. Front. Hum. Neurosci. 2015, 9, 365. [Google Scholar] [CrossRef] [PubMed]
- Ajram, L.A.; Pereira, A.C.; Durieux, A.M.S.; Velthius, H.E.; Petrinovic, M.M.; McAlonan, G.M. The contribution of [1H] magnetic resonance spectroscopy to the study of excitation-inhibition in autism. Prog. Neuropsychopharmacol. Biol. Psychiatry 2019, 89, 236–244. [Google Scholar] [CrossRef]
- Hwang, B.J.; Mohamed, M.A.; Brasic, J.R. Molecular imaging of autism spectrum disorder. Int. Rev. Psychiatry 2017, 29, 530–554. [Google Scholar] [CrossRef]
- Park, G.; Jeon, S.J.; Ko, I.O.; Park, J.H.; Lee, K.C.; Kim, M.S.; Shin, C.Y.; Kim, H.; Lee, Y.S. Decreased in vivo glutamate/GABA ratio correlates with the social behavior deficit in a mouse model of autism spectrum disorder. Mol. Brain 2022, 15, 19. [Google Scholar] [CrossRef]
- Drenthen, G.S.; Barendse, E.M.; Aldenkamp, A.P.; van Veenendaal, T.M.; Puts, N.A.; Edden, R.A.; Zinger, S.; Thoonen, G.; Hendriks, M.P.; Kessels, R.P.; et al. Altered neurotransmitter metabolism in adolescents with high-functioning autism. Psychiatry Res. Neuroimaging 2016, 256, 44–49. [Google Scholar] [CrossRef]
- Bernardino, I.; Dionisio, A.; Violante, I.R.; Monteiro, R.; Castelo-Branco, M. Motor Cortex Excitation/Inhibition Imbalance in Young Adults With Autism Spectrum Disorder: A MRS-TMS Approach. Front. Psychiatry 2022, 13, 860448. [Google Scholar] [CrossRef]
- Klostranec, J.M.; Vucevic, D.; Bhatia, K.D.; Kortman, H.G.J.; Krings, T.; Murphy, K.P.; terBrugge, K.G.; Mikulis, D.J. Current Concepts in Intracranial Interstitial Fluid Transport and the Glymphatic System: Part I-Anatomy and Physiology. Radiology 2021, 301, 502–514. [Google Scholar] [CrossRef]
- Shen, M.D.; Nordahl, C.W.; Li, D.D.; Lee, A.; Angkustsiri, K.; Emerson, R.W.; Rogers, S.J.; Ozonoff, S.; Amaral, D.G. Extra-axial cerebrospinal fluid in high-risk and normal-risk children with autism aged 2–4 years: A case-control study. Lancet Psychiatry 2018, 5, 895–904. [Google Scholar] [CrossRef] [PubMed]
- Taber, K.H.; Shaw, J.B.; Loveland, K.A.; Pearson, D.A.; Lane, D.M.; Hayman, L.A. Accentuated Virchow-Robin spaces in the centrum semiovale in children with autistic disorder. Comput. Assist. Tomogr. 2004, 28, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Ruan, C.; Zibrila, A.I.; Musa, M.; Wu, Y.; Zhang, Z.; Liu, H.; Salimeen, M. Children with autism spectrum disorder present glymphatic system dysfunction evidenced by diffusion tensor imaging along the perivascular space. Medicine 2022, 101, e32061. [Google Scholar] [CrossRef] [PubMed]
- Shen, M.D.; Kim, S.H.; McKinstry, R.C.; Gu, H.; Hazlett, H.C.; Nordahl, C.W.; Emerson, R.W.; Shaw, D.; Elison, J.T.; Swanson, M.R.; et al. Increased Extra-axial Cerebrospinal Fluid in High-Risk Infants Who Later Develop Autism. Biol. Psychiatry 2017, 82, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Lehtinen, M.K. Cerebrospinal Fluid Magnetic Resonance Imaging: Improving Early Diagnosis of Autism and Other Neurodevelopmental Conditions. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 2020, 5, 635–637. [Google Scholar] [CrossRef]
- Peterson, M.; Prigge, M.B.D.; Bigler, E.D.; Zielinski, B.; King, J.B.; Lange, N.; Alexander, A.; Lainhart, J.E.; Nielsen, J.A. Evidence for normal extra-axial cerebrospinal fluid volume in autistic males from middle childhood to adulthood. Neuroimage 2021, 240, 118387. [Google Scholar] [CrossRef]
- Diem, A.K.; Carare, R.O.; Weller, R.O.; Bressloff, N.W. A control mechanism for intra-mural peri-arterial drainage via astrocytes: How neuronal activity could improve waste clearance from the brain. PLoS ONE 2018, 13, e0205276. [Google Scholar] [CrossRef]
| Reference | Age Range (Mean) | Brain Regions | Main Findings in the ASD Group |
|---|---|---|---|
| Schumann et al. [6] | Longitudinal, 1.5–5 (2.5) years | Cerebral | ↑ GMV and WMV in the cerebrum; notably in frontal, temporal, and cingulate cortices |
| Hazlett et al. [15] | (Longitudinal, prospective), 6–7, 12–13, 24–25 months | Cortical surface area | ↑ Cortical surface area (6–12 month); ↑ TBV (12–24 month) |
| Hazlett et al. [17] | Longitudinal, 18–35 (32) month | Cerebral; CT | ↑ Cerebral cortical (2 and 4–5 years); ↑ surface area in temporal, frontal, and parietal–occipital; no differences in cortical thickness |
| Ohta et al. [18] | Longitudinal, 2.5–3.5 (3) years | Cerebral cortical grey matter; surface area; cortical thickness | ↑ Cortical surface; no difference in cortical thickness |
| Guo et al. [20] | 2–7 (5) years | Cerebral; cerebellum | ↑ GMV in fusiform face area and cerebellum/vermis |
| Bai et al. [21] | 2–7 (5) years | Cerebral | ↑ GMV in right medial superior frontal gyrus and left fusiform gyrus |
| Retico et al. [22] | 2–7 (4.4) years | Cerebral | ↑ GMV in bilateral superior frontal gyrus, precuneus, superior temporal gyrus; ↓ GMV in right inferior temporal gyrus |
| Li et al. [23] | 6–24 months | Amygdala; hippocampus | ↑ TBV in amygdala and hippocampus |
| Reinhardt et al. [24] | 25–80 (38.2) month | Hippocampus | ↑ TBV in hippocampus |
| Shou et al. [25] | 2.9–5 (4.1) years | Amygdala; hippocampus | ↑ TBV in left amygdala and left hippocampus |
| Mengotti et al. [26] | 4–14 (7) years | Cerebral | ↑ WMV in right inferior frontal gyrus, right fusiform gyrus, left precentral, supplementary motor area, and left hippocampus |
| Pote et al. [31] | 4–6 (4.8) month | Cerebral | ↑ TBV in cerebellar and subcortical |
| van Rooij et al. [37] | 2–64 (15.4) years | Cerebral; CT | ↓ Subcortical volumes of the pallidum, putamen, amygdala, and nucleus accumbens; ↑ CT in the frontal cortex; ↓ CT in the temporal cortex |
| Zielinski et al. [39] | 3–36 (16.8) years | CT | ↑ Thinning rate of CT in early childhood; ↓ thinning rate of CT in later childhood, adolescence, and early adulthood |
| Prigge et al. [41] | Longitudinal, 3.4–36 (16.4) years | CT | ↑ CT in right frontal and temporal poles, and left superior frontal; ↓ CT in left inferior temporal and bank of the superior temporal sulcus, and right caudal anterior and posterior cingulate |
| Shiohama et al. [42] | 10–35 (7.3) months | CT | ↑ CT in right medial orbitofrontal cortex; ↓ CT in caudal anterior cingulate |
| Sussman et al. [43] | 4–18 years | CT | ↓ CT in left orbitofrontal cortex and left posterior cingulate gyrus |
| Postema et al. [44] | 1.8–64 years | Cortical thickness asymmetries | ↓ Cortical thickness asymmetries in medial frontal, orbitofrontal, inferior temporal, and cingulate regions |
| Yang et al. [49] | 4–12 (8.4) years | Cerebral; cortical folding; CT; SA | ↑ GI in right inferior parietal, inferior temporal, and the left isthmus cingulate gyri; ↑ CT and TBV in right middle temporal gyrus and the posterior superior temporal sulcus |
| Zoltowski et al. [53] | 5–54 (15) years | Cortical folding; CT; | ↑ lGI in right middle frontal gyrus, right inferior temporal gyrus, and right middle occipital; ↓ lGI in left posterior insula and right precuneus; ↑ CT in right anterior cingulate, right planum temporale/superior temporal gyrus |
| Reference | Age Range (Mean) | Brain Regions | Main Findings in the ASD Group |
|---|---|---|---|
| Solso et al. [56] | 12–48 (30.2) months | Frontal tracts | ↑ FA and volume in forceps minor, inferior frontal superior frontal tract, uncinate, frontal projection of the superior corticostriatal tract |
| Ouyang et al. [57] | 2–7 (4.1) years | Global main fiber tracts | ↑ FA in most major white-matter tracts (before 4 years) |
| Andrews et al. [58] | Longitudinal, 2.5–7 years | Global main fiber tracts | ↑ FA in middle and inferior cerebellar peduncles, superior longitudinal fasciculus, internal capsule, and splenium of the corpus callosum (young children); ↓ FA in sagittal stratum, cingulum, uncinate fasciculus, and internal capsule (63.6 months) |
| Andrews et al. [59] | 25.9–49.6 (38.8) months | Global main fiber tracts | ↑ FA in genu, body, and splenium of the corpus callosum, inferior frontal–occipital fasciculi, inferior and superior longitudinal fasciculi, middle and superior cerebellar peduncles, and corticospinal tract |
| Xiao et al. [11] | 2–3 (2.5) years | Global main fiber tracts | ↑ FA in corpus callosum, posterior cingulate cortex, and limbic lobes; ↓ MD in corpus callosum, posterior cingulate, limbic lobes, and insular cortex |
| Fu et al. [62] | 2–9 years | Global main fiber tracts | ↓ FA and ↑ MD in bilateral fornix, uncinate fasciculus |
| Hanaie et al. [63] | 5–14 (9.8) years | Global main fiber tracts | ↓ FA in bilateral superior cerebellar peduncle |
| Hrdlicka et al. [64] | 5–13.2 (8.0) years | Global main fiber tracts | ↓ FA in left arcuate fasciculus and inferior frontal occipital fasciculus |
| Lei et al. [65] | 4–21 (9.3) years | Association fibers; projection fibers | ↓ FA in association fibers (cingulum, inferior fronto–occipital fasciculus, inferior longitudinal fasiculus, superior longitudinal fasiculus, uncinate fasciculus), projection fibers (anterior thalamic radiation, corticospinal tract) |
| Weinstein et al. [66] | 1.5–5.8 (2.9) years | Global main fiber tracts | ↑ FA in genu of corpus callosum, and left superior longitudinal fasciculus |
| Fingher et al. [67] | 13–51 (31) months | Global main fiber tracts | ↑ FA in temporal corpus callosum segment |
| Walker et al. [70] | 2–8 (4.7) years | Global main fiber tracts | ↑ MD in posterior brain regions |
| Qin et al. [73] | 2–6 (2.9) years | Topological network | ↑ Nodal efficiency in left precuneus, thalamus, and bilateral superior parietal cortex |
| Li et al. [74] | 3–6 (4.6) years | Topological network | ↑ Nodal efficiency in left pallidum, right caudate nucleus; ↑ global efficiency and clustering coefficient; ↓ shortest path length |
| Qian et al. [75] | 6–16 (9) years | Amygdala | ↓ Nodal efficiency in right amygdala |
| Li et al. [78] | 2–9 (3.9) years | Topological network | ↓ Global efficiency; ↑ shortest path length |
| Reference | Age Range (Mean) | Brain Regions | Main Findings in the ASD Group |
|---|---|---|---|
| Haghighat et al. [90] | 5–10 (7.3), 11–17 (13.7), 18–39 (25.9) years | Whole brain | ↑ Connectivity in cingulate cortex, anterior insula, central opercular cortex, temporal pole, right anterior superior temporal gyrus, planum polare, middle frontal gyrus, right inferior frontal gyrus, cerebellum, and brainstem (children) |
| Xiao et al. [91] | 1–4 (2.3) years | Temporal cortex | ↑ Connectivity in temporal–cuneus, and temporal–precuneus |
| McKinnon et al. [92] | 11–27 months | Whole brain | ↑ Connectivity in DMN and control networks, DMN and DAN |
| Chen et al. [93] | 17–45 (30) months | Whole brain | ↑ Connectivity in visual and sensorimotor networks |
| Chen et al. [94] | 3.5–7.9 (5) years | Whole brain | ↑ Connectivity in sensory-motor and visual brain regions; ↓ connectivity in social cognition brain regions |
| Yerys et al. [100] | 6–17 (12.4) years | Networks: VAN | ↑ Connectivity in VAN and retrosplenial–temporal systems; ↓ connectivity in VAN and somatomotor-mouth systems |
| LLioska et al. [102] | 5–58 (16) years | Networks: DMN; subcortical areas | ↑ Connectivity in DMN and subcortex, ↓ connectivity in primary sensory and attention networks |
| Sha et al. [110] | 2–64 (15.7) years | Whole brain | ↓ Leftward asymmetry in rostral middle frontal, cuneus, medial orbitofrontal, and postcentral regions |
| Tang et al. [114] | 2–18 years | Cerebral | ↓ CBF in frontal lobe, hippocampus, temporal lobe, and caudate nucleus |
| Ye et al. [115] | 3–8 (4) years | Cerebral | ↓ CBF in left frontal lobe, the bilateral parietal lobes, and the bilateral temporal lobes |
| Mori et al. [116] | 2–14 (7.3) years | Cerebral | ↓ CBF in insula, superior parietal lobule, superior temporal gyrus, and inferior frontal gyrus |
| Tang et al. [117] | 2–3 (2.7 years) | Cerebral | ↓ CBF in frontal lobe, temporal lobe, hippocampus, caudate nucleus, substantia nigra, and red nucleus |
| Mori et al. [118] | 3–6 (4) years | Amygdala and orbito-frontal cortex | ↓ NAA in left amygdala and bilateral orbito-frontal cortex |
| Goji et al. [119] | 2–12 (5) years | Anterior cingulate | ↓ NAA, Cr, Cho, and mI in anterior cingulate cortex |
| Margari et al. [120] | 1.7–14 (1.9) years | Frontal lobe | ↓ NAA/Cr in frontal lobe white matter |
| DeMayo et al. [121] | 4–12 (8.9) years | Parietal lobe | ↓ GABA in left parietal lobe, ↑ GABA with age |
| Ito et al. [122] | 2–15 (6.7) years | Anterior cingulate | ↓ GABA/Cr in anterior cingulate cortex and left cerebellum, ↑ Glu/Cr in left cerebellum |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, M.; Xu, D.; Zhang, L.; Jiang, H. Application of Multimodal MRI in the Early Diagnosis of Autism Spectrum Disorders: A Review. Diagnostics 2023, 13, 3027. https://doi.org/10.3390/diagnostics13193027
Wang M, Xu D, Zhang L, Jiang H. Application of Multimodal MRI in the Early Diagnosis of Autism Spectrum Disorders: A Review. Diagnostics. 2023; 13(19):3027. https://doi.org/10.3390/diagnostics13193027
Chicago/Turabian StyleWang, Miaoyan, Dandan Xu, Lili Zhang, and Haoxiang Jiang. 2023. "Application of Multimodal MRI in the Early Diagnosis of Autism Spectrum Disorders: A Review" Diagnostics 13, no. 19: 3027. https://doi.org/10.3390/diagnostics13193027
APA StyleWang, M., Xu, D., Zhang, L., & Jiang, H. (2023). Application of Multimodal MRI in the Early Diagnosis of Autism Spectrum Disorders: A Review. Diagnostics, 13(19), 3027. https://doi.org/10.3390/diagnostics13193027








