A Novel Machine Learning Model for Predicting Orthodontic Treatment Duration
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics
2.2. Study Sample
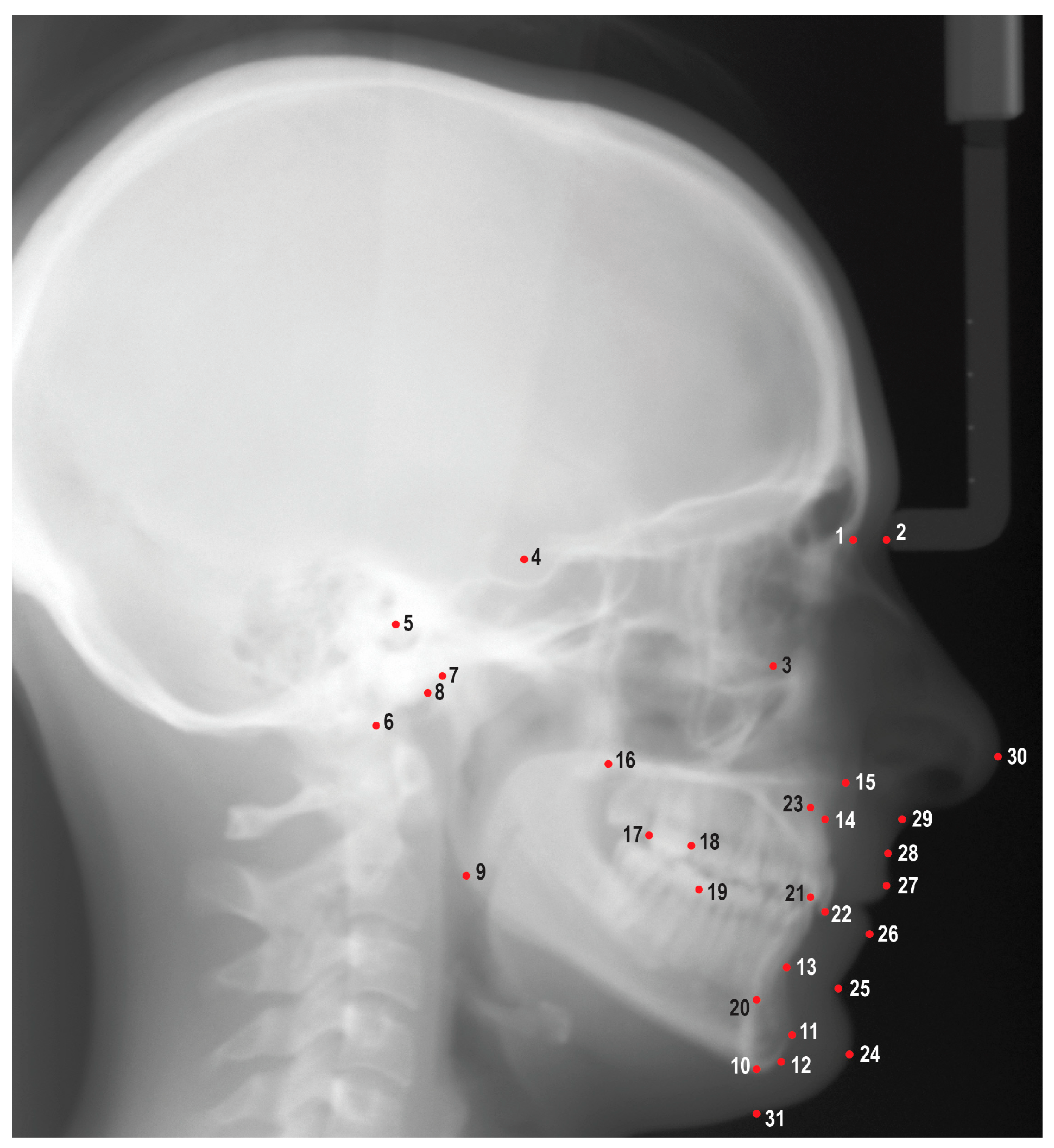
2.3. Data Collection
2.4. Reliability Assessment
2.5. Training and Testing the Models
2.6. Statistical Analysis
3. Results
3.1. Reliability Analysis
3.2. Descriptive Statistics
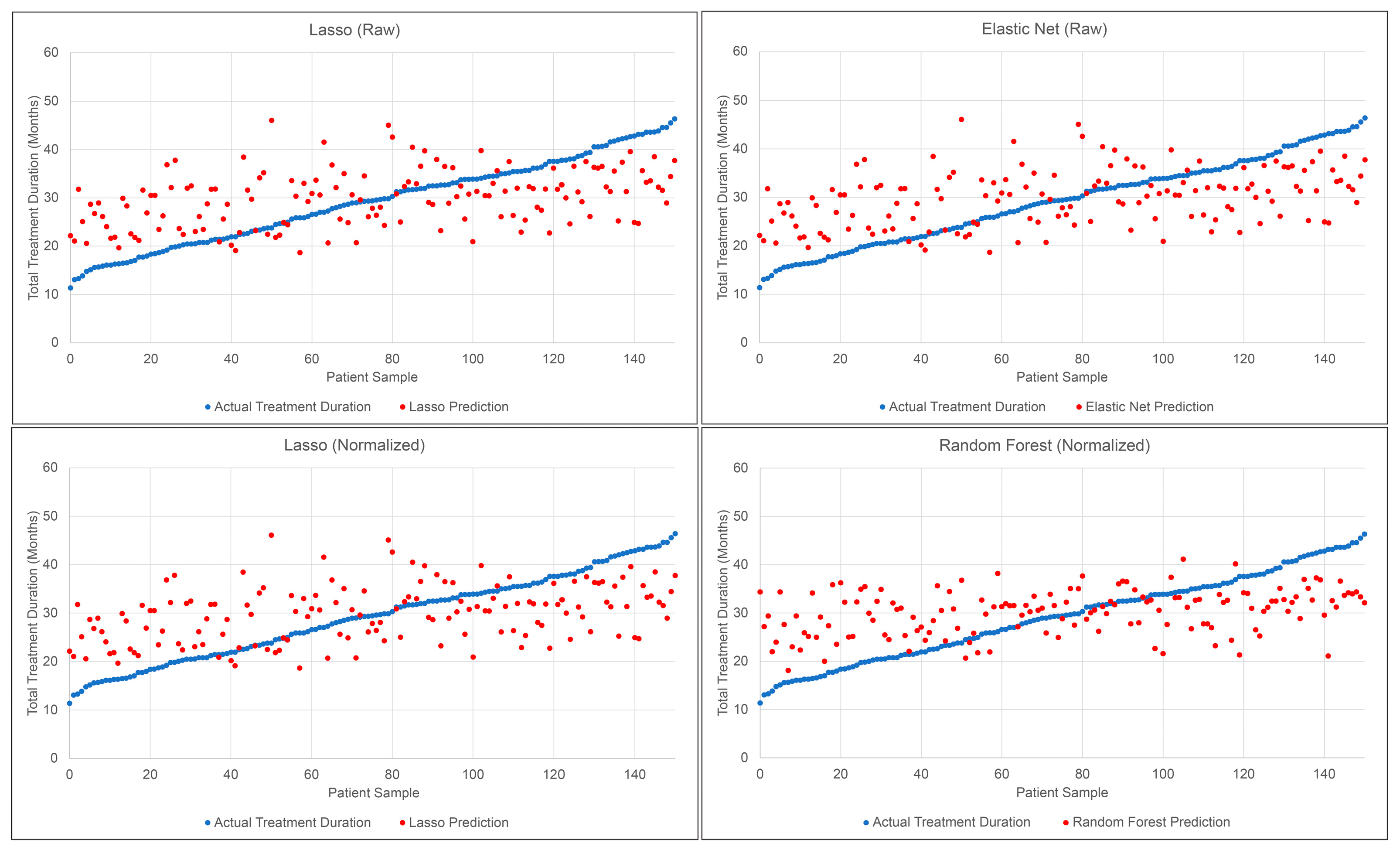
3.3. Performance of ML Models
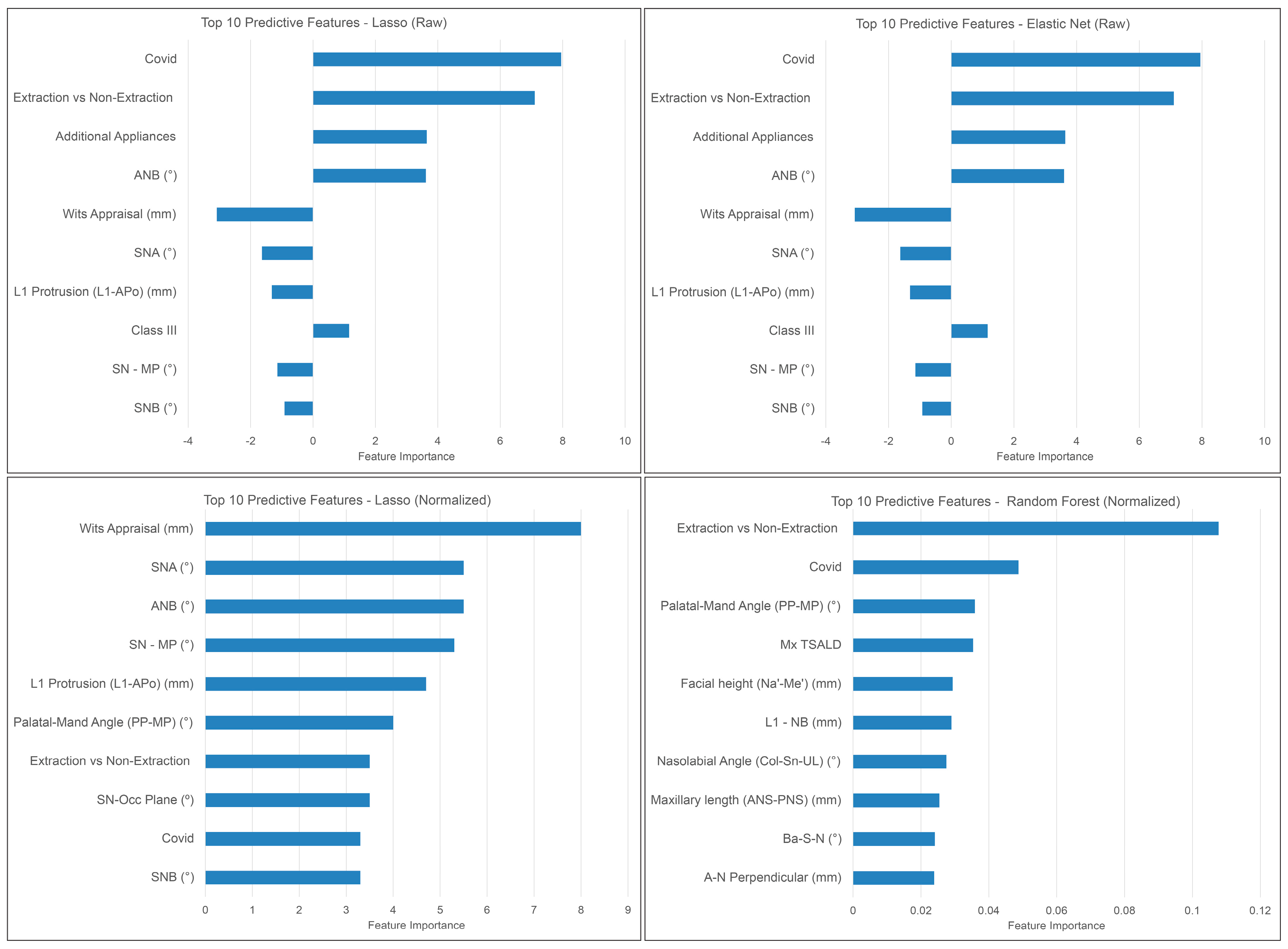
3.4. Predictive Features
3.5. Method Comparison
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Proffit, W.R.; Fields, H.W.; Larson, B.E.; Sarver, D.M. Contemporary Orthodontics; Elsevier: St. Louis, MO, USA, 2019; Volume 6. [Google Scholar]
- Pachêco-Pereira, C.; Pereira, J.R.; Dick, B.D.; Perez, A.; Flores-Mir, C. Factors associated with patient and parent satisfaction after orthodontic treatment: A systematic review. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 652–659. [Google Scholar] [CrossRef] [PubMed]
- Jharwal, V.; Trehan, M.; Rathore, N.; Rathee, P.; Agarwal, D.; Mathur, N. Informed consent for braces. Int. J. Clin. Pediatr. Dent. 2014, 7, 105–108. [Google Scholar] [CrossRef] [PubMed]
- Khanagar, S.B.; Al-Ehaideb, A.; Vishwanathaiah, S.; Maganur, P.C.; Patil, S.; Naik, S.; Baeshen, H.A.; Sarode, S.S. Scope and performance of artificial intelligence technology in orthodontic diagnosis, treatment planning, and clinical decision-making—A systematic review. J. Dent. Sci. 2021, 16, 482–492. [Google Scholar] [CrossRef] [PubMed]
- Rischen, R.J.; Breuning, K.H.; Bronkhorst, E.M.; Kuijpers-Jagtman, A.M. Records needed for orthodontic diagnosis and treatment planning: A systematic review. PLoS ONE 2013, 8, e74186. [Google Scholar] [CrossRef] [PubMed]
- Aljehani, D.; Baeshen, H.A. Effectiveness of the American Board of Orthodontics Discrepancy Index in predicting Treatment Time. J. Contemp. Dent. Pract. 2018, 19, 647–650. [Google Scholar] [PubMed]
- Vu, C.Q.; Roberts, W.E.; Hartsfield, J.K., Jr.; Ofner, S. Treatment complexity index for assessing the relationship of treatment duration and outcomes in a graduate orthodontics clinic. Am. J. Orthod. Dentofacial Orthop. 2008, 133, 9.e1–9.e13. [Google Scholar] [CrossRef] [PubMed]
- Mavreas, D.; Athanasiou, A.E. Factors affecting the duration of orthodontic treatment: A systematic review. Eur. J. Orthod. 2008, 30, 386–395. [Google Scholar] [CrossRef] [PubMed]
- Vig, K.W.; Weyant, R.; Vayda, D.; O’Brien, K.; Bennett, E. Orthodontic process and outcome: Efficacy studies—Strategies for developing process and outcome measures: A new era in orthodontics. Clin. Orthod. Res. 1998, 1, 147–155. [Google Scholar] [CrossRef]
- Chen, Y.W.; Stanley, K.; Att, W. Artificial intelligence in dentistry: Current applications and future perspectives. Quintessence Int. 2020, 51, 248–257. [Google Scholar] [CrossRef]
- Ossowska, A.; Kusiak, A.; Świetlik, D. Artificial intelligence in dentistry—Narrative review. Int. J. Environ. Res. Public Health 2022, 19, 3449. [Google Scholar] [CrossRef]
- Alekseeva, V.; Nechyporenko, A.; Frohme, M.; Gargin, V.; Meniailov, I.; Chumachenko, D. Intelligent Decision Support System for Differential Diagnosis of Chronic Odontogenic Rhinosinusitis Based on U-Net Segmentation. Electronics 2023, 12, 1202. [Google Scholar] [CrossRef]
- Jung, S.K.; Kim, T.W. New approach for the diagnosis of extractions with neural network machine learning. Am. J. Orthod. Dentofacial Orthop. 2016, 149, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; Kong, D.; Tang, T.; Su, D.; Yang, P.; Wang, H.; Zhao, Z.; Liu, Y. Orthodontic Treatment Planning based on Artificial Neural Networks. Sci. Rep. 2019, 9, 2037. [Google Scholar] [CrossRef]
- Suhail, Y.; Upadhyay, M.; Chhibber, A.; Kshitiz. Machine Learning for the Diagnosis of Orthodontic Extractions: A Computational Analysis Using Ensemble Learning. Bioengineering 2020, 7, 55. [Google Scholar] [CrossRef]
- Etemad, L.; Wu, T.H.; Heiner, P.; Liu, J.; Lee, S.; Chao, W.L.; Zaytoun, M.L.; Guez, C.; Lin, F.C.; Jackson, C.B.; et al. Machine learning from clinical data sets of a contemporary decision for orthodontic tooth extraction. Orthod. Craniofac. Res. 2021, 24 (Suppl. S2), 193–200. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Ahmad, S.; Frazier, M.; Dundar, M.M.; Turkkahraman, H. A novel machine learning model for class III surgery decision. J. Orofac. Orthop. 2022. [Google Scholar] [CrossRef] [PubMed]
- Ryu, J.; Lee, Y.-S.; Mo, S.-P.; Lim, K.; Jung, S.-K.; Kim, T.-W. Application of deep learning artificial intelligence technique to the classification of clinical orthodontic photos. BMC Oral Health 2022, 22, 454. [Google Scholar] [CrossRef] [PubMed]
- Real, A.D.; Real, O.D.; Sardina, S.; Oyonarte, R. Use of automated artificial intelligence to predict the need for orthodontic extractions. Korean J. Orthod. 2022, 52, 102–111. [Google Scholar] [CrossRef]
- Prasad, J.; Mallikarjunaiah, D.R.; Shetty, A.; Gandedkar, N.; Chikkamuniswamy, A.B.; Shivashankar, P.C. Machine Learning Predictive Model as Clinical Decision Support System in Orthodontic Treatment Planning. Dent. J. 2022, 11, 1. [Google Scholar] [CrossRef]
- Mason, T.; Kelly, K.M.; Eckert, G.; Dean, J.A.; Dundar, M.M.; Turkkahraman, H. A machine learning model for orthodontic extraction/non-extraction decision in a racially and ethnically diverse patient population. Int. Orthod. 2023, 21, 100759. [Google Scholar] [CrossRef]
- Leavitt, L.; Volovic, J.; Steinhauer, L.; Mason, T.; Eckert, G.; Dean, J.A.; Dundar, M.M.; Turkkahraman, H. Can we predict orthodontic extraction patterns by using machine learning? Orthod. Craniofac. Res. 2023. [Google Scholar] [CrossRef] [PubMed]
- Panesar, S.; Zhao, A.; Hollensbe, E.; Wong, A.; Bhamidipalli, S.S.; Eckert, G.; Dutra, V.; Turkkahraman, H. Precision and Accuracy Assessment of Cephalometric Analyses Performed by Deep Learning Artificial Intelligence with and without Human Augmentation. Appl. Sci. 2023, 13, 6921. [Google Scholar] [CrossRef]
- Wood, T.; Anigbo, J.O.; Eckert, G.; Stewart, K.T.; Dundar, M.M.; Turkkahraman, H. Prediction of the Post-Pubertal Mandibular Length and Y Axis of Growth by Using Various Machine Learning Techniques: A Retrospective Longitudinal Study. Diagnostics 2023, 13, 1553. [Google Scholar] [CrossRef] [PubMed]
- Ryu, J.; Kim, Y.H.; Kim, T.W.; Jung, S.K. Evaluation of artificial intelligence model for crowding categorization and extraction diagnosis using intraoral photographs. Sci. Rep. 2023, 13, 5177. [Google Scholar] [CrossRef] [PubMed]
- Lindner, C.; Wang, C.W.; Huang, C.T.; Li, C.H.; Chang, S.W.; Cootes, T.F. Fully Automatic System for Accurate Localisation and Analysis of Cephalometric Landmarks in Lateral Cephalograms. Sci. Rep. 2016, 6, 33581. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Kim, I.; Kim, Y.J.; Kim, M.; Cho, J.H.; Hong, M.; Kang, K.H.; Lim, S.H.; Kim, S.J.; Kim, Y.H.; et al. Accuracy of automated identification of lateral cephalometric landmarks using cascade convolutional neural networks on lateral cephalograms from nationwide multi-centres. Orthod. Craniofac. Res. 2021, 24 (Suppl. S2), 59–67. [Google Scholar] [CrossRef] [PubMed]
- Bulatova, G.; Kusnoto, B.; Grace, V.; Tsay, T.P.; Avenetti, D.M.; Sanchez, F.J.C. Assessment of automatic cephalometric landmark identification using artificial intelligence. Orthod. Craniofac. Res. 2021, 24 (Suppl. S2), 37–42. [Google Scholar] [CrossRef]
- Amasya, H.; Yildirim, D.; Aydogan, T.; Kemaloglu, N.; Orhan, K. Cervical vertebral maturation assessment on lateral cephalometric radiographs using artificial intelligence: Comparison of machine learning classifier models. Dentomaxillofac. Radiol. 2020, 49, 20190441. [Google Scholar] [CrossRef]
- Kim, D.W.; Kim, J.; Kim, T.; Kim, T.; Kim, Y.J.; Song, I.S.; Ahn, B.; Choo, J.; Lee, D.Y. Prediction of hand-wrist maturation stages based on cervical vertebrae images using artificial intelligence. Orthod. Craniofac. Res. 2021, 24 (Suppl. S2), 68–75. [Google Scholar] [CrossRef]
- Radwan, M.T.; Sin, Ç.; Akkaya, N.; Vahdettin, L. Artificial intelligence-based algorithm for cervical vertebrae maturation stage assessment. Orthod. Craniofac. Res. 2022, 26, 349–355. [Google Scholar] [CrossRef]
- Li, H.; Chen, Y.; Wang, Q.; Gong, X.; Lei, Y.; Tian, J.; Gao, X. Convolutional neural network-based automatic cervical vertebral maturation classification method. Dentomaxillofac. Radiol. 2022, 51, 20220070. [Google Scholar] [CrossRef] [PubMed]
- Atici, S.F.; Ansari, R.; Allareddy, V.; Suhaym, O.; Cetin, A.E.; Elnagar, M.H. AggregateNet: A deep learning model for automated classification of cervical vertebrae maturation stages. Orthod. Craniofac. Res. 2023. [Google Scholar] [CrossRef] [PubMed]
- Zakhar, G.; Hazime, S.; Eckert, G.; Wong, A.; Badirli, S.; Turkkahraman, H. Prediction of Pubertal Mandibular Growth in Males with Class II Malocclusion by Utilizing Machine Learning. Diagnostics 2023, 13, 2713. [Google Scholar] [CrossRef]
- Parrish, M.; O’Connell, E.; Eckert, G.; Hughes, J.; Badirli, S.; Turkkahraman, H. Short and Long-term Prediction of the Post-Pubertal Mandibular Length and Y-Axis in Females Utilizing Machine Learning. Diagnostics 2023, 13, 2729. [Google Scholar] [CrossRef]
- Xie, X.; Wang, L.; Wang, A. Artificial neural network modeling for deciding if extractions are necessary prior to orthodontic treatment. Angle Orthod. 2010, 80, 262–266. [Google Scholar] [CrossRef]
- Dharmasena, R.; Nawarathna, L.; Vithanaarachchi, V. Predicting cessation of orthodontic treatments using a classification-based approach. Biom. Biostat. Int. J. 2020, 9, 68–74. [Google Scholar] [CrossRef]
- Elnagar, M.H.; Pan, A.Y.; Handono, A.; Sanchez, F.; Talaat, S.; Bourauel, C.; Kaboudan, A.; Kusnoto, B. Utilization of Machine Learning Methods for Predicting Orthodontic Treatment Length. Oral 2022, 2, 263–273. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Holman, J.K.; Hans, M.G.; Nelson, S.; Powers, M.P. An assessment of extraction versus nonextraction orthodontic treatment using the peer assessment rating (PAR) index. Angle Orthod. 1998, 68, 527–534. [Google Scholar] [CrossRef]
- Morosan, H. Orthodontic treatment in times of COVID-19. J. Med. Life 2021, 14, 205–209. [Google Scholar] [CrossRef]
- Fisher, M.A.; Wenger, R.M.; Hans, M.G. Pretreatment characteristics associated with orthodontic treatment duration. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 178–186. [Google Scholar] [CrossRef]
- Beckwith, F.R.; Ackerman, R.J.; Cobb, C.M.; Tira, D.E. An evaluation of factors affecting duration of orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 1999, 115, 439–447. [Google Scholar] [CrossRef]

| Category | Measurements | Definitions |
|---|---|---|
| Maxilla to Cranial Base | SNA (°) | The angle formed by connecting the sella, nasion, and A point. |
| SN-Palatal Plane (°) | The angle formed from the intersection of the sella-nasion line and a line drawn connecting the anterior nasal spine to the posterior nasal spine. | |
| SN-Occlusal Plane (°) | The angle formed from the sella-nasion and occlusal plane. | |
| A-N Perpendicular (mm) | The linear distance from A point to the nasion perpendicular. | |
| Mandible to Cranial Base | SNB (°) | The angle formed by connecting the sella, nasion, and B point. |
| SNPg (°) | The angle formed by connecting the sella, naison, and pogonion. | |
| FMA: MP-FH (°) | The angle formed from the intersection of the porion-orbitale line and a line drawn connecting the gonion to the gnathion. | |
| SN-MP (°) | The angle formed from the intersection of the sella-nasion line and a line drawn connecting the gonion to the gnathion. | |
| Mandibular Plane to Occlusal Plane (°) | The angle formed by the mandibular plane and the occlusal plane. | |
| B-N Perpendicular (mm) | The linear distance from the B point to the nasion perpendicular. | |
| Pog-N Perpendicular (mm) | The linear distance from the pogonion to the nasion perpendicular. | |
| Y-Axis: SGn-SN (°) | The angle formed by connecting the nasion, sella, and gnathion. | |
| Maxilla to Mandible | ANB (°) | The difference between SNA and SNB. |
| Palatal-Mandibular Angle (PP-MP) (°) | The angle formed from the palatal plane and the mandibular plane. | |
| Wits Appraisal (mm) | The distance between A point to the occlusal plane and B point to the occlusal plane. | |
| Maxillary Length: ANS-PNS (mm) | The linear measurement between the anterior nasal spine and the posterior nasal spine. | |
| Mandibular Length: Co-Gn (mm) | The linear measurement between the condylion and the gnathion. | |
| Cranial Base | Cranial Base Flexure Angle: Ba-S-N (°) | The angle formed by connecting the basion, sella, and nasion. |
| Upper Incisors to Maxilla | U1-SN (°) | The angle formed by a line connecting the sella and the nasion and a line connecting the upper incisor incisal tip to the root apex. |
| U1-NA (°) | The angle formed by a line connecting the nasion to the A point and a line connecting the upper incisor incisal tip to the root apex. | |
| U1-NA (mm) | The linear measurement from the labial surface of the upper incisor to the line connecting the nasion to the A point. | |
| U1-Palatal Plane (°) | The angle formed by the position of the maxillary incisor to the palatal plane. | |
| U1 Protrusion (U1-APo) (mm) | The distance from the maxillary incisor to the A point-pogonion reference line. | |
| Lower Incisors to Mandible | L1-MP (°) | The angle formed by a line connecting the lower incisor incisal tip to the root apex and a line connecting the gonion to the gnathion. |
| L1-NB (°) | The angle formed by a line connecting the lower incisor incisal tip to the root apex and a line connecting the nasion to the B point. | |
| L1-NB (mm) | The linear measurement from the labial surface of the lower incisor incisal to the line connecting the nasion to the B point. | |
| L1 Protrusion (L1-Apo) (mm) | The distance from the mandibular incisor to the A point-pogonion reference line. | |
| Incisors to Each Other | Interincisal Angle (°) | The angle formed by a line connecting the lower incisor incisal tip to the apex and a line connecting the upper incisor incisal tip to the root apex. |
| Overjet (mm) | The horizontal distance from maxillary incisor tip to mandibular incisor tip. | |
| Overbite (mm) | The vertical distance from the maxillary incisor tip to the mandibular incisor tip. | |
| Soft Tissue | Upper Lip to E-Plane (mm) | The linear distance from the upper lip to a line connecting the soft tissue pogonion and pronasale. |
| Lower Lip to E-Plane (mm) | The linear distance from the lower lip to a line connecting the soft tissue pogonion and pronasale. | |
| ILG (HP) (mm) | The vertical distance from stomion superius to stomion inferius. | |
| Nasolabial Angle (Pn-Sn-UL) (°) | The angle formed by the pronasale, subnasale, and upper lip. | |
| H-Angle (Pg’UL-Pg’Na’) (°) | The angle formed by soft tissue pogonion-upper lip to soft tissue pogonion-soft tissue nasion. | |
| Facial Height (Na’-Me’) (mm) | The linear measurement from soft tissue nasion and soft tissue menton. | |
| Soft Tissue Upper Face Height: G’-Sn’ (mm) | The linear measurement between soft tissue glabella and soft tissue subnasale. | |
| Soft Tissue Lower Face Height: Sn’-Me’ (mm) | The linear measurement between soft tissue subnasale and soft tissue pogonion. | |
| Hard Tissue Upper Face Height: N-ANS (mm) | The linear measurement between the nasion and anterior nasal spine. | |
| Hard Tissue Lower Face Height: ANS-Me (mm) | The linear measurement between the anterior nasal spine and menton. | |
| UFH (N-ANS/(N-ANS + ANS-Me)) (%) | The ratio of the upper face height to facial height. | |
| LFH (ANS-Me/(N-ANS + ANS-Me)) (%) | The ratio of lower face height to facial height. | |
| Posterior Face Height: Ar-Go (mm) | The linear measurement between articulare and gonion. | |
| PFH:AFH (Co-Go:N-Me) (%) | The ratio of posterior facial height to anterior facial height. | |
| Profile | Convexity: NA-APo (°) | The angle formed by connecting the nasion, A point, and pogonion. |
| Facial Angle: FH-NPo (°) | The angle formed by a line connecting the porion to the orbitale and a line connecting the nasion to the pogonion. |
| Threshold | Agreement | Quantity | Percent | |
|---|---|---|---|---|
| 0 < ICCs < 0.50 | Poor | 3 | 6% | |
| Intra-examiner repeatability | 0.50 < ICCs < 0.75 | Moderate | 7 | 14% |
| 0.75 < ICCs < 0.90 | Good | 14 | 28% | |
| ICCs > 0.9 | Excellent | 26 | 52% | |
| 0 < ICCs < 0.50 | Poor | 1 | 2% | |
| Inter-examiner agreement | 0.50 < ICCs < 0.75 | Moderate | 6 | 12% |
| 0.75 < ICCs < 0.90 | Good | 27 | 54% | |
| ICCs > 0.9 | Excellent | 16 | 32% |
| Variable | Mean | SD | Min | Max |
|---|---|---|---|---|
| Treatment Time (Months) | 30.12 | 9.32 | 11.37 | 51.80 |
| Age (Years) | 16.00 | 5.61 | 9.00 | 50.00 |
| SNA (°) | 82.55 | 4.14 | 71.00 | 94.90 |
| SN-Palatal Plane (°) | 7.52 | 3.71 | −2.80 | 19.20 |
| SN-Occlusal Plane (°) | 15.62 | 4.85 | −1.50 | 29.00 |
| A-N Perpendicular (mm) | 0.49 | 3.72 | −9.60 | 12.00 |
| SNB (°) | 79.25 | 4.14 | 67.40 | 92.90 |
| SNPg (°) | 79.78 | 4.18 | 66.50 | 93.00 |
| FMA (MP-FH) (°) | 27.28 | 5.54 | 11.00 | 45.50 |
| SN—MP (°) | 32.66 | 5.98 | 14.80 | 51.70 |
| Mandibular Plane to Occlusal Plane (°) | 18.25 | 4.52 | 4.80 | 35.10 |
| B-N Perpendicular (mm) | −4.36 | 6.09 | −22.10 | 13.20 |
| Pog-N Perpendicular (mm) | −4.09 | 7.01 | −24.80 | 15.70 |
| Y-Axis (SGn-SN) (°) | 67.84 | 4.27 | 56.20 | 83.90 |
| ANB (°) | 3.29 | 2.06 | −3.70 | 11.10 |
| Palatal-Mandibular Plane Angle (PP-MP) (°) | 26.35 | 6.08 | 2.10 | 43.10 |
| Wits Appraisal (mm) | −0.15 | 3.06 | −9.50 | 8.90 |
| Maxillary length (ANS-PNS) (mm) | 49.47 | 3.85 | 38.20 | 65.40 |
| Mandibular length (Co-Gn) (mm) | 113.10 | 8.20 | 93.40 | 158.40 |
| Ba-S-N (°) | 130.91 | 5.71 | 114.30 | 153.90 |
| U1—SN (°) | 107.44 | 9.60 | 67.30 | 134.50 |
| U1—NA (°) | 24.89 | 8.80 | −14.10 | 51.50 |
| U1—NA (mm) | 5.55 | 3.22 | −7.50 | 17.70 |
| U1—Palatal Plane (°) | 114.96 | 8.82 | 80.40 | 140.50 |
| U1 Protrusion (U1-APo) (mm) | 7.74 | 3.74 | −2.40 | 20.90 |
| L1—MP (°) | 92.19 | 7.70 | 65.50 | 112.80 |
| L1—NB (°) | 26.70 | 8.35 | 4.80 | 51.30 |
| L1—NB (mm) | 5.60 | 3.21 | −1.30 | 17.10 |
| L1 Protrusion (L1-APo) (mm) | 3.35 | 3.41 | −5.20 | 13.60 |
| Interincisal Angle (U1-L1) (°) | 125.12 | 14.53 | 89.50 | 171.60 |
| Upper Lip to E-Plane (mm) | −1.60 | 3.12 | −12.90 | 8.50 |
| Lower Lip to E-Plane (mm) | 0.37 | 3.64 | −9.80 | 13.80 |
| Interlabial gap (HP) (mm) | 1.19 | 1.40 | −1.10 | 8.80 |
| Nasolabial Angle (Col-Sn-UL) (°) | 106.58 | 11.27 | 68.00 | 132.60 |
| Holdaway Angle (Pg’UL-Pg’Na’) (°) | 17.34 | 4.91 | 0.60 | 36.70 |
| Facial height (Na’-Me’) (mm) | 112.97 | 7.60 | 79.90 | 137.20 |
| Soft tissue Upper Facial Height (G’-Sn’) (mm) | 63.96 | 4.82 | 49.60 | 76.80 |
| Soft tissue Lower Facial Height (Sn’-Me’) (mm) | 69.64 | 6.18 | 53.60 | 87.10 |
| Upper Face Height (N-ANS) (mm) | 49.13 | 3.41 | 38.50 | 59.60 |
| Lower Face Height (ANS-Me) (mm) | 63.37 | 6.34 | 44.90 | 94.20 |
| UFH (N-ANS/(N-ANS + ANS-Me)) (%) | 43.75 | 2.56 | 36.40 | 50.10 |
| LFH (ANS-Me/(N-ANS + ANS-Me)) (%) | 56.25 | 2.56 | 49.90 | 63.60 |
| Posterior Face Height (Ar-Go) (mm) | 42.89 | 5.24 | 29.70 | 62.70 |
| PFH:AFH (Co-Go: N-Me) (%) | 51.74 | 4.84 | 37.40 | 67.30 |
| Convexity (NA-APo) (°) | 5.65 | 5.30 | −8.20 | 26.30 |
| Facial Angle (FH-NPo) (°) | 87.76 | 3.83 | 75.30 | 98.20 |
| Overjet (mm) | 4.48 | 2.33 | −2.30 | 18.20 |
| Overbite (mm) | 2.17 | 2.19 | −6.30 | 10.20 |
| Raw Data | Normalized Data | |||||||
|---|---|---|---|---|---|---|---|---|
| MAE | RMSE | ME | ICC | MAE | RMSE | ME | ICC | |
| XGBoost | 8.70 | 10.56 | −0.29 | 0.97 | 8.43 | 10.40 | −0.45 | 0.97 |
| Random Forest | 7.75 | 9.63 | −0.65 | 0.97 | 7.27 | 8.79 | −0.46 | 0.96 |
| Lasso | 7.27 | 8.73 | −0.13 | 0.96 | 7.27 | 8.73 | −0.13 | 0.96 |
| Ridge | 7.30 | 8.76 | −0.29 | 0.96 | 7.29 | 8.73 | −0.16 | 0.96 |
| Linear Regression | 7.30 | 8.76 | −0.29 | 0.96 | 7.31 | 8.77 | −0.36 | 0.96 |
| Elastic Net | 7.27 | 8.73 | −0.13 | 0.96 | 7.27 | 8.73 | −0.13 | 0.96 |
| Gaussian Process | 29.77 | 31.27 | 29.77 | 0.99 | 8.62 | 11.02 | 3.42 | 0.98 |
| Support Vector | 7.66 | 9.13 | 1.18 | 0.96 | 10.24 | 12.47 | 0.07 | 0.98 |
| MLP Regressor | 13.04 | 15.69 | 12.63 | 0.99 | 8.52 | 10.57 | −3.20 | 0.97 |
| Methods | Estimate | Standard Error | p-Value |
|---|---|---|---|
| Elastic Net < Gaussian | −1.35 | 0.47 | <0.01 |
| Elastic Net and Lasso | 0.00 | 0.47 | 1.00 |
| Elastic Net and Linear | −0.03 | 0.47 | 0.94 |
| Elastic Net < MLP | −1.25 | 0.47 | 0.01 |
| Elastic Net and Random Forest | 0.00 | 0.47 | 1.00 |
| Elastic Net and Ridge | −0.01 | 0.47 | 0.97 |
| Elastic Net < SVR | −2.96 | 0.47 | <0.01 |
| Elastic Net < XGBoost | −1.16 | 0.47 | 0.01 |
| Gaussian > Lasso | 1.35 | 0.47 | <0.01 |
| Gaussian > Linear | 1.31 | 0.47 | 0.01 |
| Gaussian and MLP | 0.10 | 0.47 | 0.83 |
| Gaussian > Random Forest | 1.35 | 0.47 | <0.01 |
| Gaussian > Ridge | 1.33 | 0.47 | <0.01 |
| Gaussian < SVR | −1.62 | 0.47 | <0.01 |
| Gaussian and XGBoost | 0.19 | 0.47 | 0.68 |
| Lasso and Linear | −0.03 | 0.47 | 0.94 |
| Lasso < MLP | −1.25 | 0.47 | 0.01 |
| Lasso and Random Forest | 0.00 | 0.47 | 1.00 |
| Lasso and Ridge | −0.01 | 0.47 | 0.97 |
| Lasso < SVR | −2.96 | 0.47 | <0.01 |
| Lasso < XGBoost | −1.16 | 0.47 | 0.01 |
| Linear < MLP | −1.21 | 0.47 | 0.01 |
| Linear and Random Forest | 0.03 | 0.47 | 0.94 |
| Linear and Ridge | 0.02 | 0.47 | 0.97 |
| Linear < SVR | −2.93 | 0.47 | <0.01 |
| Linear < XGBoost | −1.12 | 0.47 | 0.02 |
| MLP > Random Forest | 1.25 | 0.47 | 0.01 |
| MLP > Ridge | 1.23 | 0.47 | 0.01 |
| MLP < SVR | −1.72 | 0.47 | <0.01 |
| MLP and XGBoost | 0.09 | 0.47 | 0.85 |
| Random Forest and Ridge | −0.01 | 0.47 | 0.97 |
| Random Forest < SVR | −2.96 | 0.47 | <0.01 |
| Random Forest < XGBoost | −1.16 | 0.47 | 0.01 |
| Ridge < SVR | −2.95 | 0.47 | <0.01 |
| Ridge < XGBoost | −1.14 | 0.47 | 0.01 |
| SVR > XGBoost | 1.81 | 0.47 | <0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Volovic, J.; Badirli, S.; Ahmad, S.; Leavitt, L.; Mason, T.; Bhamidipalli, S.S.; Eckert, G.; Albright, D.; Turkkahraman, H. A Novel Machine Learning Model for Predicting Orthodontic Treatment Duration. Diagnostics 2023, 13, 2740. https://doi.org/10.3390/diagnostics13172740
Volovic J, Badirli S, Ahmad S, Leavitt L, Mason T, Bhamidipalli SS, Eckert G, Albright D, Turkkahraman H. A Novel Machine Learning Model for Predicting Orthodontic Treatment Duration. Diagnostics. 2023; 13(17):2740. https://doi.org/10.3390/diagnostics13172740
Chicago/Turabian StyleVolovic, James, Sarkhan Badirli, Sunna Ahmad, Landon Leavitt, Taylor Mason, Surya Sruthi Bhamidipalli, George Eckert, David Albright, and Hakan Turkkahraman. 2023. "A Novel Machine Learning Model for Predicting Orthodontic Treatment Duration" Diagnostics 13, no. 17: 2740. https://doi.org/10.3390/diagnostics13172740
APA StyleVolovic, J., Badirli, S., Ahmad, S., Leavitt, L., Mason, T., Bhamidipalli, S. S., Eckert, G., Albright, D., & Turkkahraman, H. (2023). A Novel Machine Learning Model for Predicting Orthodontic Treatment Duration. Diagnostics, 13(17), 2740. https://doi.org/10.3390/diagnostics13172740






