Comparison Study between ERCP and PTBD for Recurrent Choledocholithiasis in Patients Following Gastrectomy
Abstract
1. Introduction
2. Materials and Methods
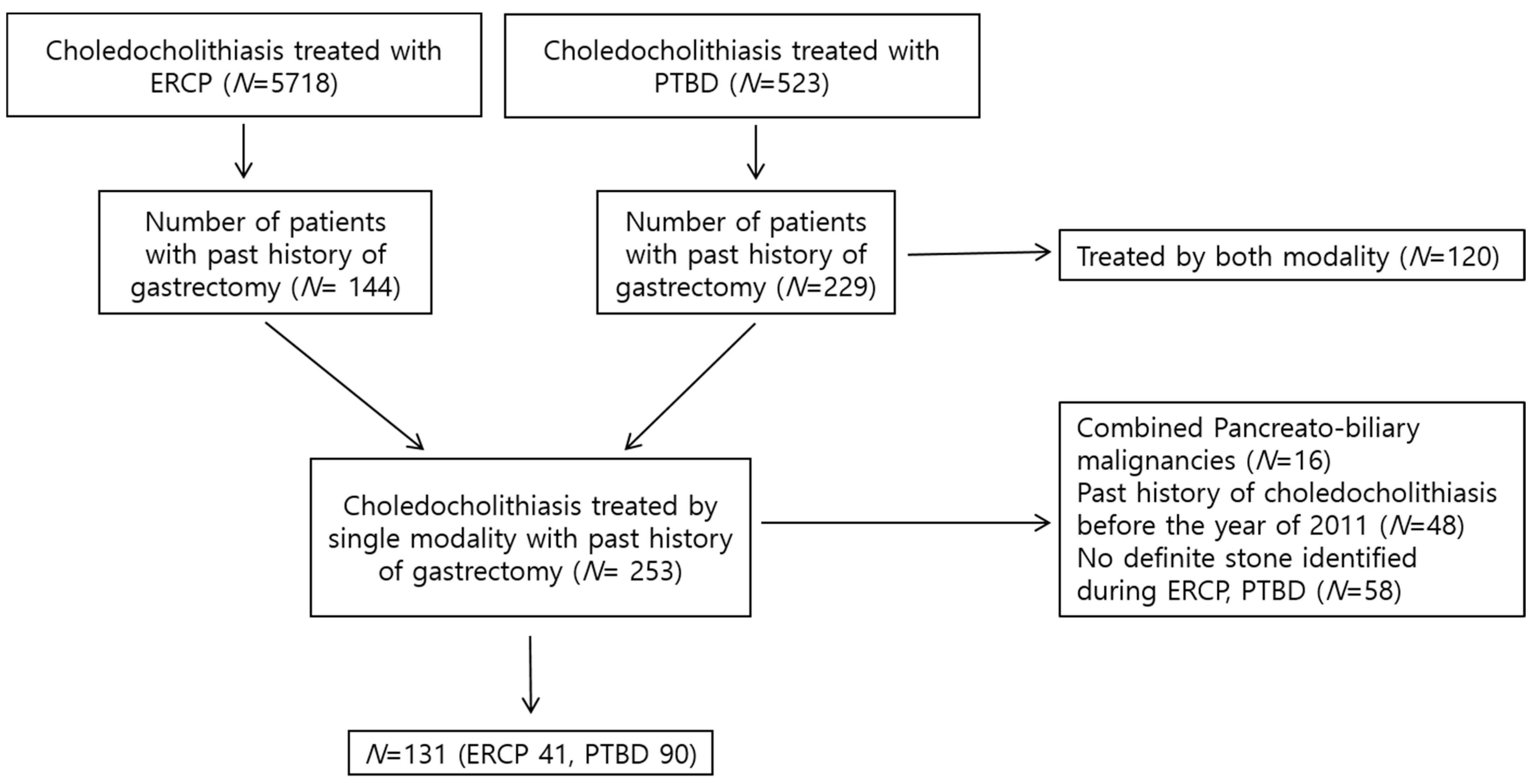
2.1. Patients
2.2. ERCP Method
2.3. PTBD Method
2.4. Follow-Up
2.5. Definition of CBD Stone Recurrence
2.6. Study Outcomes
2.7. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Recurrence Rate
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Figueiredo, J.C.; Haiman, C.; Porcel, J.; Buxbaum, J.; Stram, D.; Tambe, N.; Cozen, W.; Wilkens, L.; Le Marchand, L.; Setiawan, V.W. Sex and ethnic/racial-specific risk factors for gallbladder disease. BMC Gastroenterol. 2017, 17, 153. [Google Scholar] [CrossRef] [PubMed]
- Hedjoudje, A.; Cheurfa, C.; Et Talby, M.; Levy, P.; Prat, F.; Piton, G. Outcomes and predictors of delayed endoscopic biliary drainage for severe acute cholangitis due to choledocholithiasis in an intensive care unit. Dig. Liver Dis. 2023, 55, 763–770. [Google Scholar] [CrossRef] [PubMed]
- Liang, C.-M.; Chiu, Y.-C.; Lu, L.-S.; Wu, C.-K.; Sou, F.-M.; Chiu, S.-M.; Lee, Y.-C.; Huang, P.-Y.; Chuah, S.-K.; Kuo, C.-M. Early and Direct Endoscopic Stone Removal in the Moderate Grade of Acute Cholangitis with Choledocholithiasis Was Safe and Effective: A Prospective Study. Life 2022, 12, 2000. [Google Scholar] [CrossRef]
- Nakamura, K.; Ogoshi, K.; Makuuchi, H. Clinicopathological study of cholelithiasis following gastric cancer surgery. Eur. Surg. Res. 2005, 37, 29–35. [Google Scholar] [CrossRef]
- Kim, S.Y.; Bang, W.J.; Lim, H.; Lim, M.S.; Kim, M.; Choi, H.G. Increased risk of gallstones after gastrectomy: A longitudinal follow-up study using a national sample cohort in Korea. Medicine 2019, 98, e15932. [Google Scholar] [CrossRef] [PubMed]
- Tan, Z.; Xie, P.; Qian, H.; Yao, X. Clinical analysis of prophylactic cholecystectomy during gastrectomy for gastric cancer patients: A retrospective study of 1753 patients. BMC Surg. 2019, 19, 48. [Google Scholar] [CrossRef]
- Bencini, L.; Italian Research Group for Gastric Cancer (GIRCG); Marchet, A.; Alfieri, S.; Rosa, F.; Verlato, G.; Marrelli, D.; Roviello, F.; Pacelli, F.; Cristadoro, L.; et al. The Cholegas trial: Long-term results of prophylactic cholecystectomy during gastrectomy for cancer-a randomized-controlled trial. Gastric Cancer 2019, 22, 632–639. [Google Scholar] [CrossRef]
- Yang, M.J.; Kim, J.H.; Hwang, J.C.; Yoo, B.M.; Park, S.W.; Kwon, C.I.; Jeong, S. Mechanistic loop resolution strategy for short-type single-balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography in patients with Roux-en-Y reconstruction after gastrectomy (with video). Surg. Endosc. 2022, 36, 8690–8696. [Google Scholar] [CrossRef]
- Kobayashi, T.; Hisanaga, M.; Kanehiro, H.; Yamada, Y.; Ko, S.; Nakajima, Y. Analysis of risk factors for the development of gallstones after gastrectomy. Br. J. Surg. 2005, 92, 1399–1403. [Google Scholar] [CrossRef]
- Zhang, M.; Zhang, J.; Sun, X.; Xu, J.; Zhu, J.; Yuan, W.; Yan, Q. Clinical analysis of treatment strategies to cholecystocholedocholithiasis patients with previous subtotal or total gastrectomy: A retrospective cohort study. BMC Surg. 2018, 18, 54. [Google Scholar] [CrossRef] [PubMed]
- Everhart, J.E.; Khare, M.; Hill, M.; Maurer, K.R. Prevalence and ethnic differences in gallbladder disease in the United States. Gastroenterology 1999, 117, 632–639. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Q.; He, Y.; Qiang, D.C.; Wu, L.X. Prevalence and epidemiological pattern of gallstones in urban residents in China. Eur. J. Gastroenterol. Hepatol. 2012, 24, 1459–1460. [Google Scholar] [CrossRef] [PubMed]
- Paik, K.-H.; Lee, J.-C.; Kim, H.W.; Kang, J.; Lee, Y.S.; Hwang, J.-H.; Ahn, S.H.; Park, D.J.; Kim, H.-H.; Kim, J. Risk Factors for Gallstone Formation in Resected Gastric Cancer Patients. Medicine 2016, 95, e3157. [Google Scholar] [CrossRef]
- Kato, S.; Chinen, K.; Shinoura, S.; Kikuchi, K. Predictors for bile duct stone recurrence after endoscopic extraction for naive major duodenal papilla: A cohort study. PLoS ONE 2017, 12, e0180536. [Google Scholar] [CrossRef]
- Keizman, D.; Shalom, M.I.; Konikoff, F.M. An angulated common bile duct predisposes to recurrent symptomatic bile duct stones after endoscopic stone extraction. Surg. Endosc. 2006, 20, 1594–1599. [Google Scholar] [CrossRef]
- Costamagna, G.; Tringali, A.; Shah, S.K.; Mutignani, M.; Zuccala, G.; Perri, V. Long-term follow-up of patients after endoscopic sphincterotomy for choledocholithiasis, and risk factors for recurrence. Endoscopy 2002, 34, 273–279. [Google Scholar] [CrossRef]
- Oh, C.H.; Dong, S.H. Recent Advances in the Management of Recurrent Bile Duct Stones. Korean J. Gastroenterol. 2015, 66, 251–254. [Google Scholar] [CrossRef]
- Nzenza, T.C.; Al-Habbal, Y.; Guerra, G.R.; Manolas, S.; Yong, T.; McQuillan, T. Recurrent common bile duct stones as a late complication of endoscopic sphincterotomy. BMC Gastroenterol. 2018, 18, 39. [Google Scholar] [CrossRef]
- Tsai, T.J.; Lin, C.K.; Lai, K.H.; Chan, H.H.; Wang, E.M.; Tsai, W.L.; Cheng, J.S.; Yu, H.C.; Chen, W.C.; Hsu, P.I. Does preserved sphincter of Oddi function prevent common bile duct stones recurrence in patients after endoscopic papillary balloon dilation? J. Chin. Med. Assoc. 2018, 81, 311–315. [Google Scholar] [CrossRef] [PubMed]
- Hatjidakis, A.A.; Karampekios, S.; Prassopoulos, P.; Xynos, E.; Raissaki, M.; Vasilakis, S.I.; Gourtsoyiannis, N.C. Maturation of the tract after percutaneous cholecystostomy with regard to the access route. Cardiovasc. Intervent. Radiol. 1998, 21, 36–40. [Google Scholar] [CrossRef]
- Park, T.Y.; Kang, J.S.; Song, T.J.; Lee, S.S.; Lee, H.; Choi, J.S.; Kim, H.J.; Jang, J.W. Outcomes of ERCP in Billroth II gastrectomy patients. Gastrointest. Endosc. 2016, 83, 1193–1201. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Patients Who Underwent CBD Stone Removal Following Gastrectomy (N = 131) |
|---|---|
| Sex, male, n (%) | 100 (76.3) |
| Age, mean ± SD (years) | 72.0 ± 9.4 |
| Charlson comorbidity index score, mean ± SD, (points) | 3.4 ± 1.9 |
| Gastrectomy type, n (%) | |
| Subtotal gastrectomy with Billroth I | 24 (18.3) |
| Subtotal gastrectomy with Billroth II | 59 (45.0) |
| Total gastrectomy with Roux-en-Y | 48 (36.6) |
| Treatment modality for CBD stones | |
| ERCP, n (%) | 41 (31.3) |
| PTBD, n (%) | 90 (68.7) |
| Duration between gastrectomy and CBD stone removal, mean ± SD (days) | 183.7 ± 133.3 |
| CBD stone, numbers, mean ± SD | 1.7 ± 1.5 |
| CBD stone size, mean ± SD (mm) | 9.5 ± 4.4 |
| CBD stone type, n (%) | |
| Brown | 28 (21.4) |
| Black | 3 (2.3) |
| Sludge | 1 (0.8) |
| Unknown | 99 (75.6) |
| Follow-up duration, mean ± SD (months) | 31.5 ± 28.5 |
| Recurrent Group (N = 19) | Non-Recurrent Group (N = 112) | p-Value | |
|---|---|---|---|
| Sex, male, n (%) | 15 (78.9) | 85 (75.9) | 0.772 |
| Age (years) | 73.0 ± 9.2 | 71.8 ± 9.5 | 0.616 |
| ERCP stone removal, n (%) | 10 (52.6) | 31 (27.7) | 0.030 |
| Balloon sphincteroplasty, n (%) | 8 (42.1) | 84 (75.0) | 0.004 |
| Balloons larger than 12 mm, n (%) | 4 (21.1) | 60 (53.6) | 0.009 |
| Cholecystectomy, n (%) | 5 (26.3) | 28 (25.0) | 1.000 |
| GB stone/sludge, n (%) | 11 (57.9) | 67 (59.8) | 0.874 |
| Distal CBD angulation ≤ 135°, n (%) | 14 (73.7) | 88 (78.6) | 0.765 |
| CBD stricture, n (%) | 4 (21.1) | 8 (7.1) | 0.074 |
| CBD diameter, mean ± SD (mm) | 13.5 ± 3.9 | 11.9 ± 3.6 | 0.089 |
| Periampullary diverticulum, n (%) | 5/11 (45.5) | 5/36 (13.9) | 0.039 |
| ERCP (N = 41) | PTBD (N = 90) | p-Value | |
|---|---|---|---|
| Sex, male, n (%) | 31 (75.6) | 69 (76.7) | 0.895 |
| Age (years) | 71.7 ± 9.7 | 72.1 ± 9.4 | 0.801 |
| Charlson comorbidity index score, mean ± SD (points) | 3.5 ± 2.0 | 3.3 ± 1.8 | 0.736 |
| Gastrectomy type, n (%) | <0.001 | ||
| Subtotal gastrectomy with Billroth I | 20 (48.8) | 4 (4.4) | |
| Subtotal gastrectomy with Billroth II | 21 (51.2) | 38 (42.2) | |
| Total gastrectomy with Roux-en-Y | 48 (53.3) | ||
| CBD stone recurrence, n (%) | 10 (24.4) | 9 (10.0) | 0.030 |
| Balloon sphincteroplasty, larger than 12 mm, n (%) | 11 (26.8) | 53 (58.9) | 0.001 |
| Balloon sphincteroplasty, n (%) | 24 (58.5) | 68 (75.6) | 0.048 |
| Variable | HR | 95% CI | p-Value |
|---|---|---|---|
| PTBD | 0.278 | 0.078–0.791 | 0.016 |
| CBD stricture | 3.823 | 1.118–13.080 | 0.033 |
| Balloon sphincteroplasty | 0.207 | 0.072–0.599 | 0.004 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kweon, O.S.; Heo, J.; Jung, M.K. Comparison Study between ERCP and PTBD for Recurrent Choledocholithiasis in Patients Following Gastrectomy. Diagnostics 2023, 13, 2651. https://doi.org/10.3390/diagnostics13162651
Kweon OS, Heo J, Jung MK. Comparison Study between ERCP and PTBD for Recurrent Choledocholithiasis in Patients Following Gastrectomy. Diagnostics. 2023; 13(16):2651. https://doi.org/10.3390/diagnostics13162651
Chicago/Turabian StyleKweon, O Seong, Jun Heo, and Min Kyu Jung. 2023. "Comparison Study between ERCP and PTBD for Recurrent Choledocholithiasis in Patients Following Gastrectomy" Diagnostics 13, no. 16: 2651. https://doi.org/10.3390/diagnostics13162651
APA StyleKweon, O. S., Heo, J., & Jung, M. K. (2023). Comparison Study between ERCP and PTBD for Recurrent Choledocholithiasis in Patients Following Gastrectomy. Diagnostics, 13(16), 2651. https://doi.org/10.3390/diagnostics13162651






