Diagnostic Value of Four-Dimensional Dynamic Computed Tomography for Primary Hyperparathyroidism in Patients with Low Baseline Parathyroid Hormone Levels
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
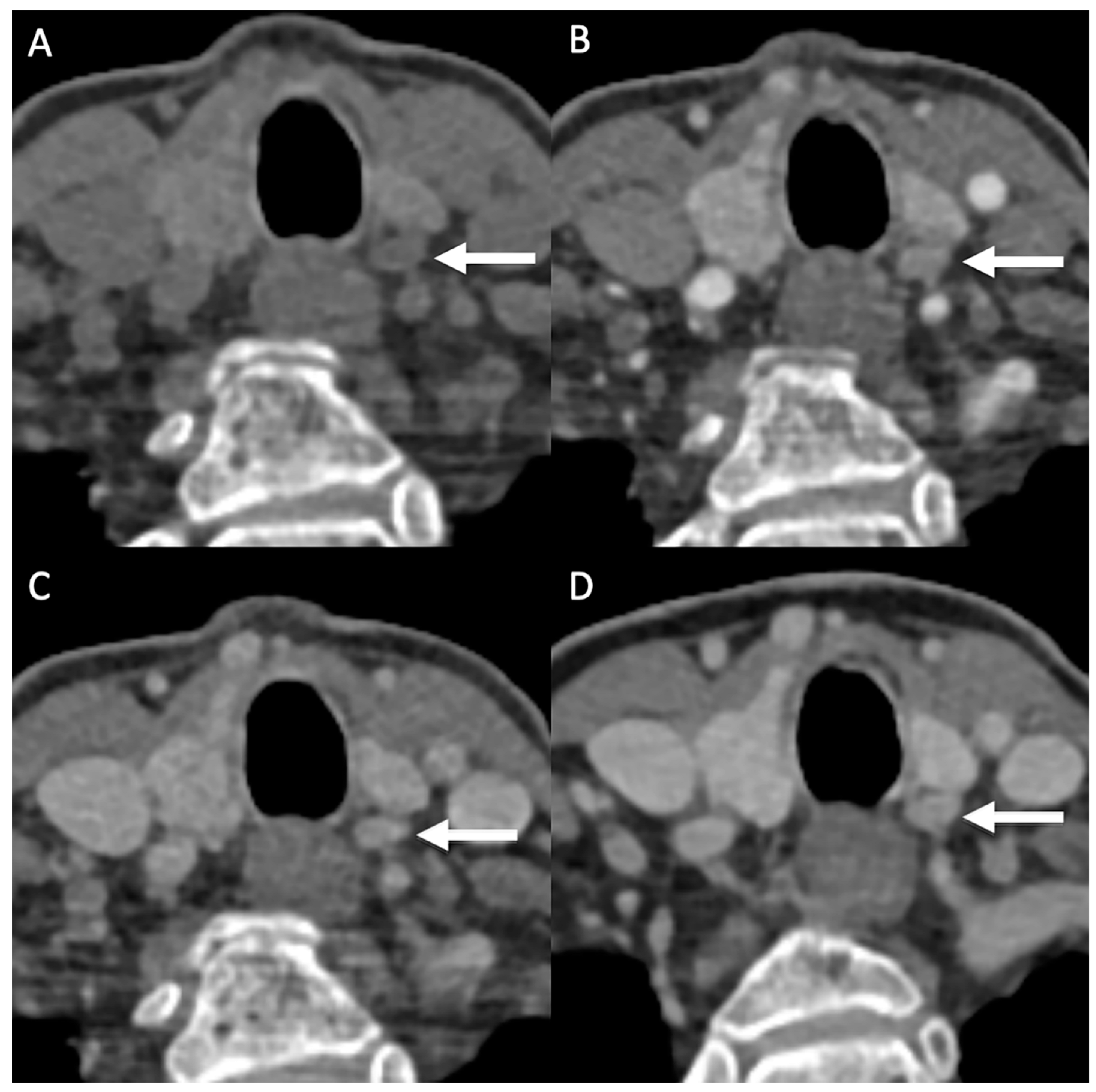
2.2. Imaging Technique
2.3. Surgery
2.4. Statistical Analysis
3. Results
Patient Characteristics
4. Diagnostic Accuracy
5. Discussion
6. Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bilezikian, J.P.; Bandeira, L.; Khan, A.; Cusano, N.E. Hyperparathyroidism. Lancet 2018, 391, 168–178. [Google Scholar] [CrossRef]
- Kandil, E.; Alabbas, H.; Tufaro, A.P.; Carson, K.A.; Tufano, R.P. The impact of baseline intact parathyroid hormone levels on severity of primary hyperparathyroidism and outcomes in patients undergoing surgery. Arch. Otolaryngol. Head Neck Surg. 2010, 136, 147–150. [Google Scholar] [CrossRef]
- Clark, M.J.; Pellitteri, P.K. Assessing the impact of low baseline parathyroid hormone levels on surgical treatment of primary hyperparathyroidism. Laryngoscope 2009, 119, 1100–1105. [Google Scholar] [CrossRef]
- Applewhite, M.K.; Schneider, D.F. Mild primary hyperparathyroidism: A literature review. Oncologist 2014, 19, 919–929. [Google Scholar] [CrossRef]
- Rameau, A.; Eng, S.; Vu, J.; Saket, R.; Jun, P.; Friduss, M. Four-dimensional computed tomography scan utility in parathyroidectomy for primary hyperparathyroidism with low baseline intact parathyroid hormone. Laryngoscope 2017, 127, 1476–1482. [Google Scholar] [CrossRef]
- Miller, B.S.; England, B.G.; Nehs, M.; Burney, R.E.; Doherty, G.M.; Gauger, P.G. Interpretation of intraoperative parathyroid hormone monitoring in patients with baseline parathyroid hormone levels of <100 pg/mL. Surgery 2006, 140, 883–889; discussion 889–890. [Google Scholar] [CrossRef] [PubMed]
- Khorasani, N.; Mohammadi, A. Effective factors on the sensitivity of preoperative sestamibi scanning for primary hyperparathyroidism. Int. J. Clin. Exp. Med. 2014, 7, 2639–2644. [Google Scholar] [PubMed]
- Cron, D.C.; Kapeles, S.R.; Andraska, E.A.; Kwon, S.T.; Kirk, P.S.; McNeish, B.L.; Lee, C.S.; Hughes, D.T. Predictors of operative failure in parathyroidectomy for primary hyperparathyroidism. Am. J. Surg. 2017, 214, 509–514. [Google Scholar] [CrossRef]
- Kluijfhout, W.P.; Pasternak, J.D.; Beninato, T.; Drake, F.T.; Gosnell, J.E.; Shen, W.T.; Duh, Q.-Y.; Allen, I.E.; Vriens, M.R.; de Keizer, B.; et al. Diagnostic performance of computed tomography for parathyroid adenoma localization; a systematic review and meta-analysis. Eur. J. Radiol. 2017, 88, 117–128. [Google Scholar] [CrossRef]
- Bahl, M. Preoperative Parathyroid Imaging: Trends in Utilization and Comparative Accuracy of Sonography, Scintigraphy, and 4-Dimensional Computed Tomography. J. Comput. Assist. Tomogr. 2019, 43, 264–268. [Google Scholar] [CrossRef] [PubMed]
- Roskies, M.; Liu, X.; Hier, M.P.; Payne, R.J.; Mlynarek, A.; Forest, V.; Levental, M.; Forghani, R. 3-phase dual-energy CT scan as a feasible salvage imaging modality for the identification of non-localizing parathyroid adenomas: A prospective study. J. Otolaryngol. Head Neck Surg. 2015, 44, 44. [Google Scholar] [CrossRef] [PubMed]
- Vijayasarathi, A.; Karnezis, S.; Azizyan, A.; Salamon, N.; Sepahdari, A. 4D CT Parathyroid for the General Radiologist: A Pictorial Essay of Illustrative Cases. Curr. Probl. Diagn. Radiol. 2022, 51, 659–665. [Google Scholar] [CrossRef]
- Kattar, N.; Migneron, M.; Debakey, M.S.; Haidari, M.; Pou, A.M.; McCoul, E.D. Advanced Computed Tomographic Localization Techniques for Primary Hyperparathyroidism: A Systematic Review and Meta-analysis. JAMA Otolaryngol. Head Neck Surg. 2022, 148, 448–456. [Google Scholar] [CrossRef] [PubMed]
- Chazen, J.L.; Gupta, A.; Dunning, A.; Phillips, C.D. Diagnostic accuracy of 4D-CT for parathyroid adenomas and hyperplasia. AJNR Am. J. Neuroradiol. 2012, 33, 429–433. [Google Scholar] [CrossRef] [PubMed]
- Minhas, P.; Jadhav, R.; Singh, J.; Virmani, S.; Gupta, K. Diagnostic performance of 4D-CT in cases of Primary hyperparathyroidism with negative SPECT 99mTc Sestamibi scan. J. Nucl. Med. 2020, 61, 1162. [Google Scholar]
- Rodgers, S.E.; Hunter, G.J.; Hamberg, L.M.; Schellingerhout, D.; Doherty, D.B.; Ayers, G.D.; Shapiro, S.E.; Edeiken, B.S.; Truong, M.T.; Evans, D.B.; et al. Improved preoperative planning for directed parathyroidectomy with 4-dimensional computed tomography. Surgery 2006, 140, 932–940; discussion 940–941. [Google Scholar] [CrossRef]
- Starker, L.F.; Mahajan, A.; Björklund, P.; Sze, G.; Udelsman, R.; Carling, T. 4D parathyroid CT as the initial localization study for patients with de novo primary hyperparathyroidism. Ann. Surg. Oncol. 2011, 18, 1723–1728. [Google Scholar] [CrossRef]
- Hinson, A.M.; Lee, D.R.; Hobbs, B.A.; Fitzgerald, R.T.; Bodenner, D.L.; Stack, B.C., Jr. Preoperative 4D CT Localization of Nonlocalizing Parathyroid Adenomas by Ultrasound and SPECT-CT. Otolaryngol. Head Neck Surg. 2015, 153, 775–778. [Google Scholar] [CrossRef]
- Mortenson, M.M.; Evans, D.B.; Lee, J.E.; Hunter, G.J.; Shellingerhout, D.; Vu, T.; Edeiken, B.S.; Feng, L.; Perrier, N.D. Parathyroid exploration in the reoperative neck: Improved preoperative localization with 4D-computed tomography. J. Am. Coll. Surg. 2008, 206, 888–895; discussion 895–886. [Google Scholar] [CrossRef]
- Suh, Y.J.; Choi, J.Y.; Kim, S.J.; Chun, I.K.; Yun, T.J.; Lee, K.E.; Kim, J.H.; Cheon, G.J.; Youn, Y.K. Comparison of 4D CT, ultrasonography, and 99mTc sestamibi SPECT/CT in localizing single-gland primary hyperparathyroidism. Otolaryngol. Head Neck Surg. 2015, 152, 438–443. [Google Scholar] [CrossRef]
- Hiebert, J.; Hague, C.; Hou, S.; Wiseman, S.M. Dual energy computed tomography should be a first line preoperative localization imaging test for primary hyperparathyroidism patients. Am. J. Surg. 2018, 215, 788–792. [Google Scholar] [CrossRef] [PubMed]
- Dhillon, V.K.; Pitukcheewanont, P.; Yeh, M.; Maceri, D. Identifying an Ectopic Parathyroid Adenoma Using 4DCT in a Pediatric Patient with Persistent Primary Hyperparathyroidism. Case Rep. Otolaryngol. 2013, 2013, 676039. [Google Scholar] [CrossRef] [PubMed]
- Morris, M.A.; Saboury, B.; Ahlman, M.; Malayeri, A.A.; Jones, E.C.; Chen, C.C.; Millo, C. Parathyroid Imaging: Past, Present, and Future. Front. Endocrinol. 2021, 12, 760419. [Google Scholar] [CrossRef] [PubMed]
- Alhefdhi, A.; Pinchot, S.N.; Davis, R.; Sippel, R.S.; Chen, H. The necessity and reliability of intraoperative parathyroid hormone (PTH) testing in patients with mild hyperparathyroidism and PTH levels in the normal range. World J. Surg. 2011, 35, 2006–2009. [Google Scholar] [CrossRef]
- Carneiro-Pla, D.M.; Solorzano, C.C.; Lew, J.I.; Irvin, G.L., 3rd. Long-term outcome of patients with intraoperative parathyroid level remaining above the normal range during parathyroidectomy. Surgery 2008, 144, 989–993; discussion 993–984. [Google Scholar] [CrossRef]
- Javid, M.; Callender, G.; Quinn, C.; Carling, T.; Donovan, P.; Udelsman, R. Primary hyperparathyroidism with normal baseline intraoperative parathyroid hormone: A challenging population. Surgery 2017, 161, 493–498. [Google Scholar] [CrossRef]
- Kowalski, G.; Buła, G.; Bednarczyk, A.; Gawrychowska, A.; Gawrychowski, J. Multiglandular Parathyroid Disease. Life 2022, 12, 1286. [Google Scholar] [CrossRef]
- Hargitai, L.; Bereuter, C.M.; Dunkler, D.; Geroldinger, A.; Scheuba, C.; Niederle, B.; Riss, P. The value of intraoperative parathyroid hormone monitoring in patients with primary hyperparathyroidism and varying baseline parathyroid hormone levels. BJS Open 2022, 6, zrac118. [Google Scholar] [CrossRef]
- Kebebew, E.; Hwang, J.; Reiff, E.; Duh, Q.-Y.; Clark, O.H. Predictors of Single-Gland vs Multigland Parathyroid Disease in Primary Hyperparathyroidism: A Simple and Accurate Scoring Model. Arch. Surg. 2006, 141, 777–782. [Google Scholar] [CrossRef]
- Sepahdari, A.R.; Bahl, M.; Harari, A.; Kim, H.J.; Yeh, M.W.; Hoang, J.K. Predictors of Multigland Disease in Primary Hyperparathyroidism: A Scoring System with 4D-CT Imaging and Biochemical Markers. Am. J. Neuroradiol. 2015, 36, 987–992. [Google Scholar] [CrossRef]
- Mahajan, A.; Starker, L.F.; Ghita, M.; Udelsman, R.; Brink, J.A.; Carling, T. Parathyroid four-dimensional computed tomography: Evaluation of radiation dose exposure during preoperative localization of parathyroid tumors in primary hyperparathyroidism. World J. Surg. 2012, 36, 1335–1339. [Google Scholar] [CrossRef]
- Bunch, P.M.; Randolph, G.W.; Brooks, J.A.; George, V.; Cannon, J.; Kelly, H.R. Parathyroid 4D CT: What the Surgeon Wants to Know. Radiographics 2020, 40, 1383–1394. [Google Scholar] [CrossRef]
- Campbell, M.J.; Sicuro, P.; Alseidi, A.; Blackmore, C.C.; Ryan, J.A. Two-phase (low-dose) computed tomography is as effective as 4D-CT for identifying enlarged parathyroid glands. Int. J. Surg. 2015, 14, 80–84. [Google Scholar] [CrossRef] [PubMed]
- Kutler, D.I.; Moquete, R.; Kazam, E.; Kuhel, W.I. Parathyroid localization with modified 4D-computed tomography and ultrasonography for patients with primary hyperparathyroidism. Laryngoscope 2011, 121, 1219–1224. [Google Scholar] [CrossRef] [PubMed]
- Brown, S.J.; Lee, J.C.; Christie, J.; Maher, R.; Sidhu, S.B.; Sywak, M.S.; Delbridge, L.W. Four-dimensional computed tomography for parathyroid localization: A new imaging modality. ANZ J. Surg. 2015, 85, 483–487. [Google Scholar] [CrossRef]
- Nael, K.; Hur, J.; Bauer, A.; Khan, R.; Sepahdari, A.; Inampudi, R.; Guerrero, M. Dynamic 4D MRI for Characterization of Parathyroid Adenomas: Multiparametric Analysis. Am. J. Neuroradiol. 2015, 36, 2147–2152. [Google Scholar] [CrossRef]
- Leiva-Salinas, C.; Flors, L.; Durst, C.R.; Hou, Q.; Patrie, J.T.; Wintermark, M.; Mukherjee, S. Detection of parathyroid adenomas using a monophasic dual-energy computed tomography acquisition: Diagnostic performance and potential radiation dose reduction. Neuroradiology 2016, 58, 1135–1141. [Google Scholar] [CrossRef] [PubMed]
- Maraia, D.; Hemmerdinger, S.; Chiarolanzio, P.; Mehta, H.; Ali, S.; Gomes, W.; Schefflein, J.; High, M.; Gulko, E. Dual-layer spectral CT virtual-non-contrast images aid in parathyroid adenoma analysis and radiation dose reduction: Confirmation of findings from dual-energy CT. Clin. Imaging 2022, 84, 113–117. [Google Scholar] [CrossRef]
- Becker, J.L.; Patel, V.; Johnson, K.J.; Guerrero, M.; Klein, R.R.; Ranvier, G.F.; Owen, R.P.; Pawha, P.; Nael, K. 4D-Dynamic Contrast-Enhanced MRI for Preoperative Localization in Patients with Primary Hyperparathyroidism. AJNR Am. J. Neuroradiol. 2020, 41, 522–528. [Google Scholar] [CrossRef]
- Broos, W.A.M.; van der Zant, F.M.; Knol, R.J.J.; Wondergem, M. Choline PET/CT in parathyroid imaging: A systematic review. Nucl. Med. Commun. 2019, 40, 96–105. [Google Scholar] [CrossRef]
- Cakir, B.; Cuhaci Seyrek, F.N.; Topaloglu, O.; Ozdemir, D.; Dirikoc, A.; Aydin, C.; Polat, S.B.; Ogmen, B.E.; Tam, A.A.; Baser, H.; et al. Ultrasound elastography score and strain index in different parathyroid lesions. Endocr. Connect. 2019, 8, 1579–1590. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.-W.; Shim, S.R.; Jeong, S.Y.; Kim, S.-J. Direct Comparison of Preoperative Imaging Modalities for Localization of Primary Hyperparathyroidism: A Systematic Review and Network Meta-analysis. JAMA Otolaryngol.–Head Neck Surg. 2021, 147, 692–706. [Google Scholar] [CrossRef] [PubMed]
- Ozturk, M.; Polat, A.V.; Celenk, C.; Elmali, M.; Kir, S.; Polat, C. The diagnostic value of 4D MRI at 3T for the localization of parathyroid adenomas. Eur. J. Radiol. 2019, 112, 207–213. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Low PTH (n = 28) | High PTH (n = 32) | p-Value |
|---|---|---|---|
| Female | 23 (82.1%) | 23 (71.9%) | 0.42 |
| Age | 61.1 (9.3) | 61.7 (12.3) | 0.74 |
| BMI | 26.5 (4.4) | 26.6 (5.7) | 0.6 |
| Baseline PTH | 73.8 pg/mL (SD 17.9) | 247.0 pg/mL (241.7) | <0.001 |
| Baseline Calcium | 10.7 mg/dL (0.5) | 11.2 mg/dL (0.8) | 0.03 |
| SGD | 92.9% (26/28) | 87.5% (28/32) | - |
| MGD | 7.1% (2/28) | 18.8% (6/32) | 0.19 |
| Double adenoma | 2 | 5 | |
| Triple | 0 | 1 | - |
| Weight | 0.77 g (SD 0.69) | 1.4 g (SD 1.6) | 0.25 |
| Max diameter | 15.9 mm (8.6) | 19.5 mm (10.9) | 0.23 |
| Lesion not found during surgery | 5 (17.9%) | 1 (3.1%) | 0.058 |
| BNE | 1 | 5 | 0.12 |
| Parameter | Low PTH | High PTH | p-Value |
|---|---|---|---|
| Correct localization (N) | 22 | 36 | - |
| Total glands (N) | 25 | 38 | - |
| Lesion-based sensitivity | 88.0% (22/25) | 94.7% (36/38) | 0.33 |
| Parameter | Low PTH | High PTH | p-Value |
|---|---|---|---|
| Correct localization (N) | 20 | 29 | - |
| Total glands (N) | 28 | 32 | - |
| Successful image-guided surgical resection rate | 71.4% (20/28) | 90.6% (29/32) | 0.056 |
| No. | 4D-CT Finding | Previous Neck Surgery | Thyroid Comorbidity | Preoperative PTH (pg/mL) | Preoperative Calcium (mg/dL) | Adenoma Weight (grams) | Surgery/Histopathology | Cure |
|---|---|---|---|---|---|---|---|---|
| 1 | 1 lesion identified: right side | no | no | 99.02 | 10.40 | - | No lesion found during surgery | no |
| 2 | 1 lesion identified: intrathyroidal right side | Yes: previous parathyroidectomy | no | 41.49 | 10.36 | - | No lesion found during surgery | no |
| 3 | 1 lesion identified: left side | no | no | 68.84 | 10.88 | - | No lesion found during surgery | no |
| 4 | 1 lesion identified: right side | no | no | 84.87 | 10.96 | - | No lesion found during surgery | no |
| 5 | No lesion identified | no | no | 99.02 | 10.36 | 0.40 | 1 parathyroid adenoma left side | yes |
| 6 | No lesion identified | no | no | 96.19 | 10.32 | 0.32 | 1 parathyroid adenoma left side | yes |
| 7 | No lesion identified | no | no | 36.78 | 10.24 | 0.40 | 1 parathyroid adenoma right side | yes |
| 8 | 1 lesion identified: left side | no | no | 139.56 | 12.72 | 6.5 and 0.48 | 2 parathyroid adenomas: left side and right side. | yes |
| 9 | No lesion identified | no | no | 68.84 | 11.00 | No lesion found during surgery | no | |
| 10 | 1 lesion identified: mediastinal | no | no | 207.46 | 22.00 | No lesion found during surgery | no | |
| 11 | No lesion identified | no | no | 809.09 | 12.52 | 3 | 1 parathyroid adenoma found in thymus | yes |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Difaie, Z.; Scheepers, M.H.M.C.; Engelen, S.M.E.; Havekes, B.; Bouvy, N.D.; Postma, A.A. Diagnostic Value of Four-Dimensional Dynamic Computed Tomography for Primary Hyperparathyroidism in Patients with Low Baseline Parathyroid Hormone Levels. Diagnostics 2023, 13, 2621. https://doi.org/10.3390/diagnostics13162621
Al-Difaie Z, Scheepers MHMC, Engelen SME, Havekes B, Bouvy ND, Postma AA. Diagnostic Value of Four-Dimensional Dynamic Computed Tomography for Primary Hyperparathyroidism in Patients with Low Baseline Parathyroid Hormone Levels. Diagnostics. 2023; 13(16):2621. https://doi.org/10.3390/diagnostics13162621
Chicago/Turabian StyleAl-Difaie, Zaid, Max H. M. C. Scheepers, Sanne M. E. Engelen, Bastiaan Havekes, Nicole D. Bouvy, and Alida A. Postma. 2023. "Diagnostic Value of Four-Dimensional Dynamic Computed Tomography for Primary Hyperparathyroidism in Patients with Low Baseline Parathyroid Hormone Levels" Diagnostics 13, no. 16: 2621. https://doi.org/10.3390/diagnostics13162621
APA StyleAl-Difaie, Z., Scheepers, M. H. M. C., Engelen, S. M. E., Havekes, B., Bouvy, N. D., & Postma, A. A. (2023). Diagnostic Value of Four-Dimensional Dynamic Computed Tomography for Primary Hyperparathyroidism in Patients with Low Baseline Parathyroid Hormone Levels. Diagnostics, 13(16), 2621. https://doi.org/10.3390/diagnostics13162621





