Anterior Incisura Fibularis Corner Landmarks Can Safely Validate the Optimal Distal Tibiofibular Reduction in Malleolar Fractures—Prospective CT Study
Abstract
1. Introduction
2. Patients and Methods
Operative Technique
- Anatomical fixation of the fracture site
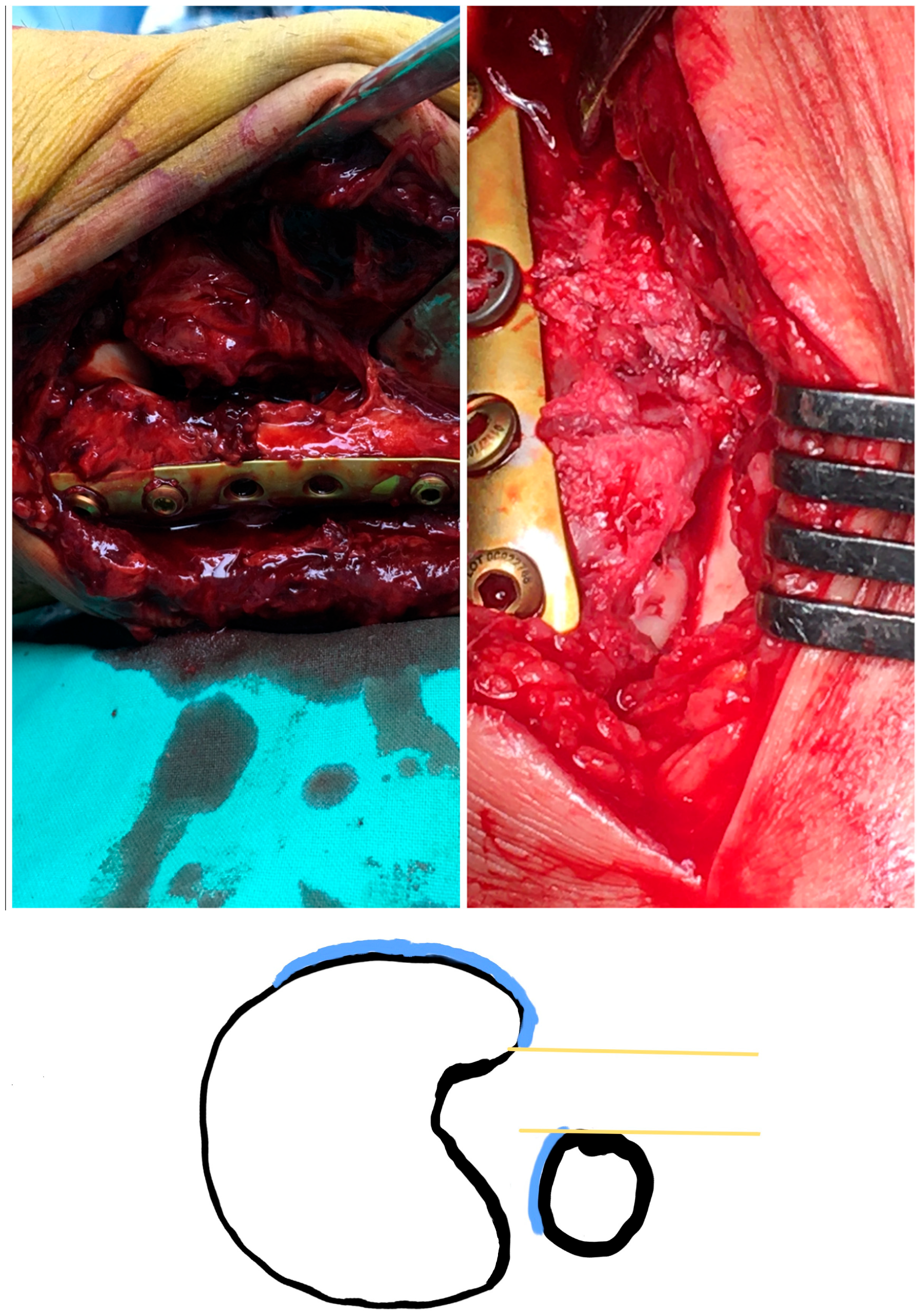
- The superior lateral malleolus cartilage was aligned with the anterolateral tibial plafond cartilage (restoring the fibula length) (Figure 2):
- The lateral malleolus cartilage was put parallel to the lateral talar surface (restoring the fibula rotation)
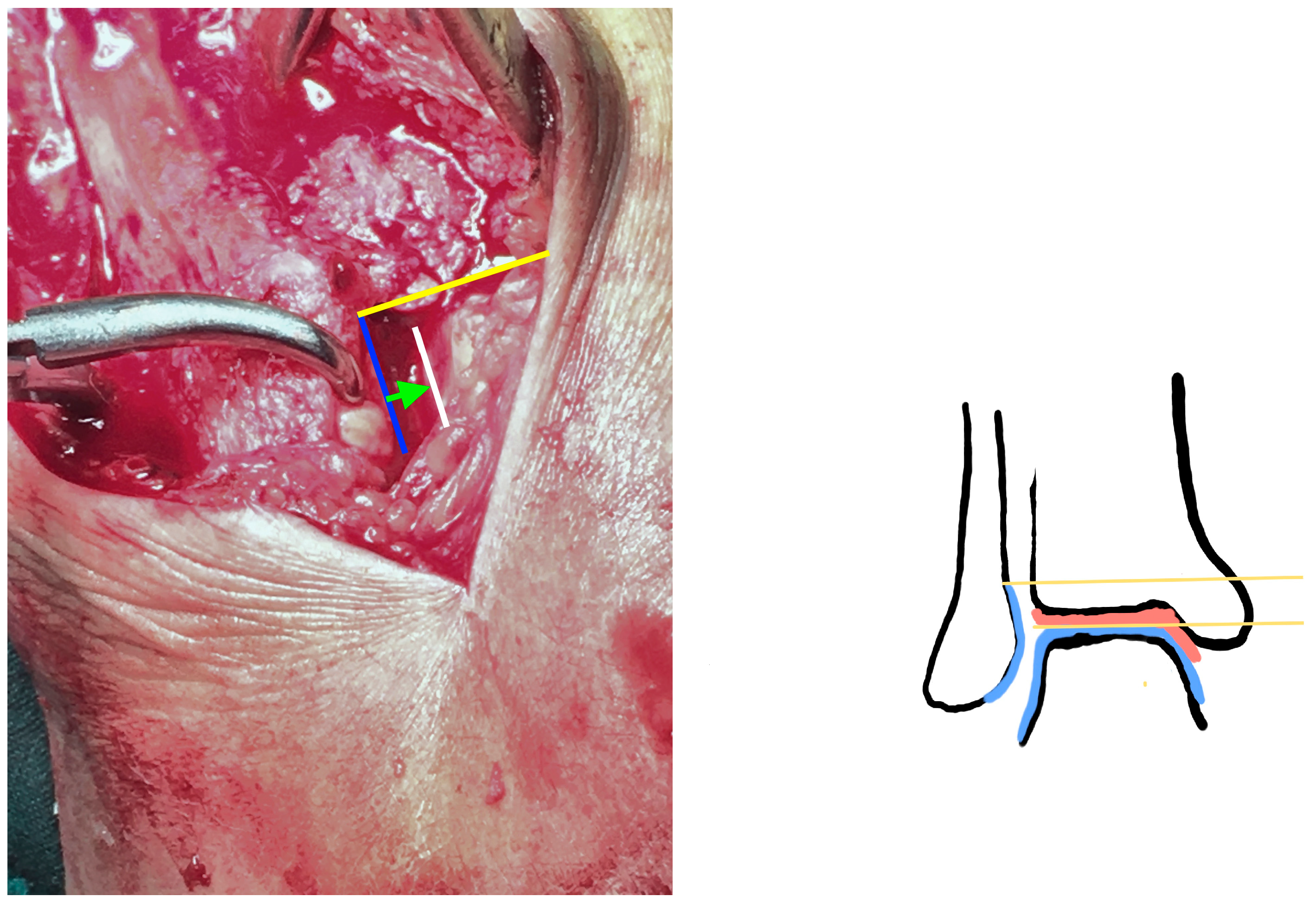
- In the sagittal plane, the lateral malleolus cartilage was fixed as anteriorly as the anterolateral tibial plafond cartilage (restoring the sagittal translation) (Figure 3)
3. Results
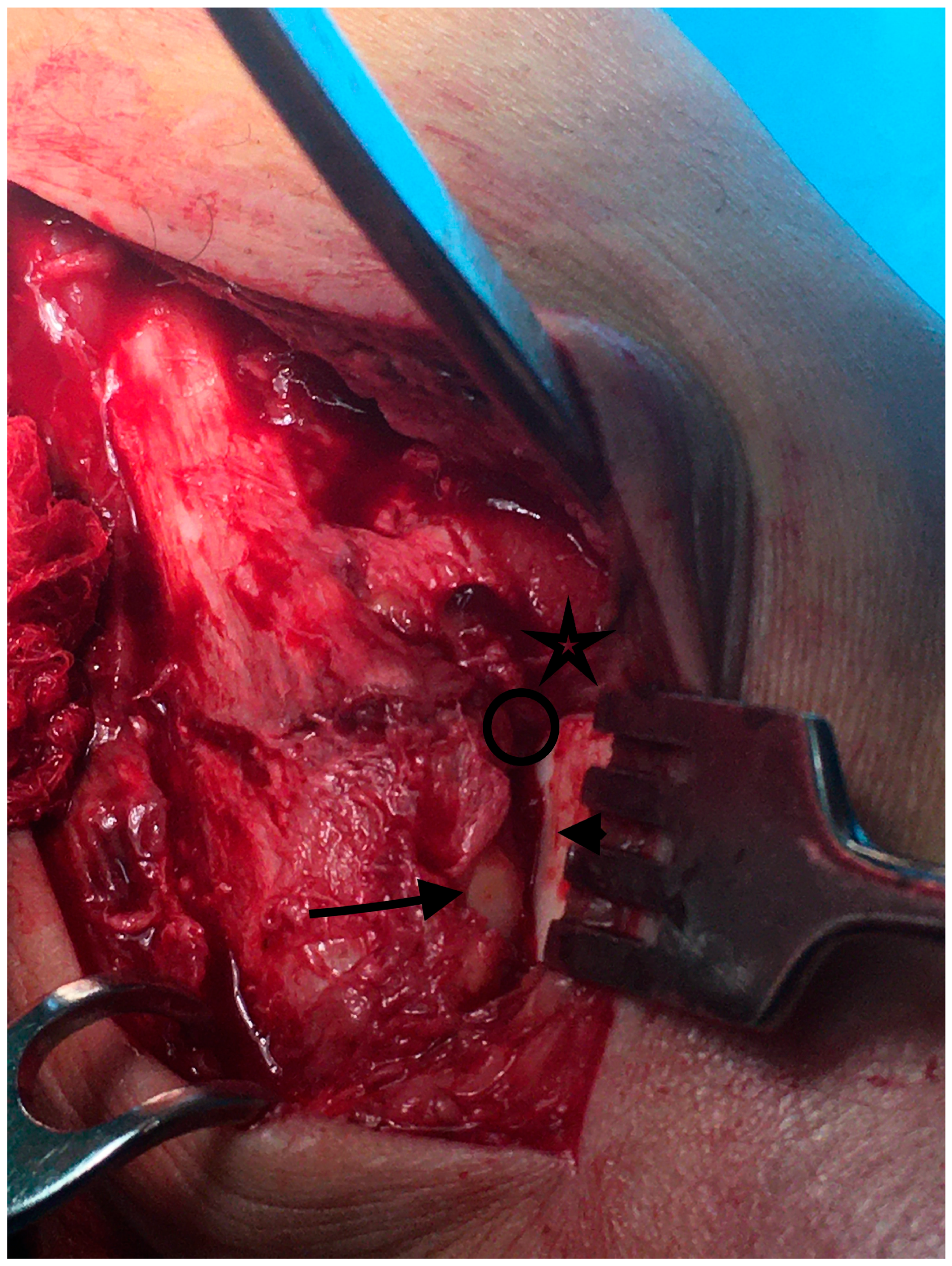
3.1. Intraoperative Findings
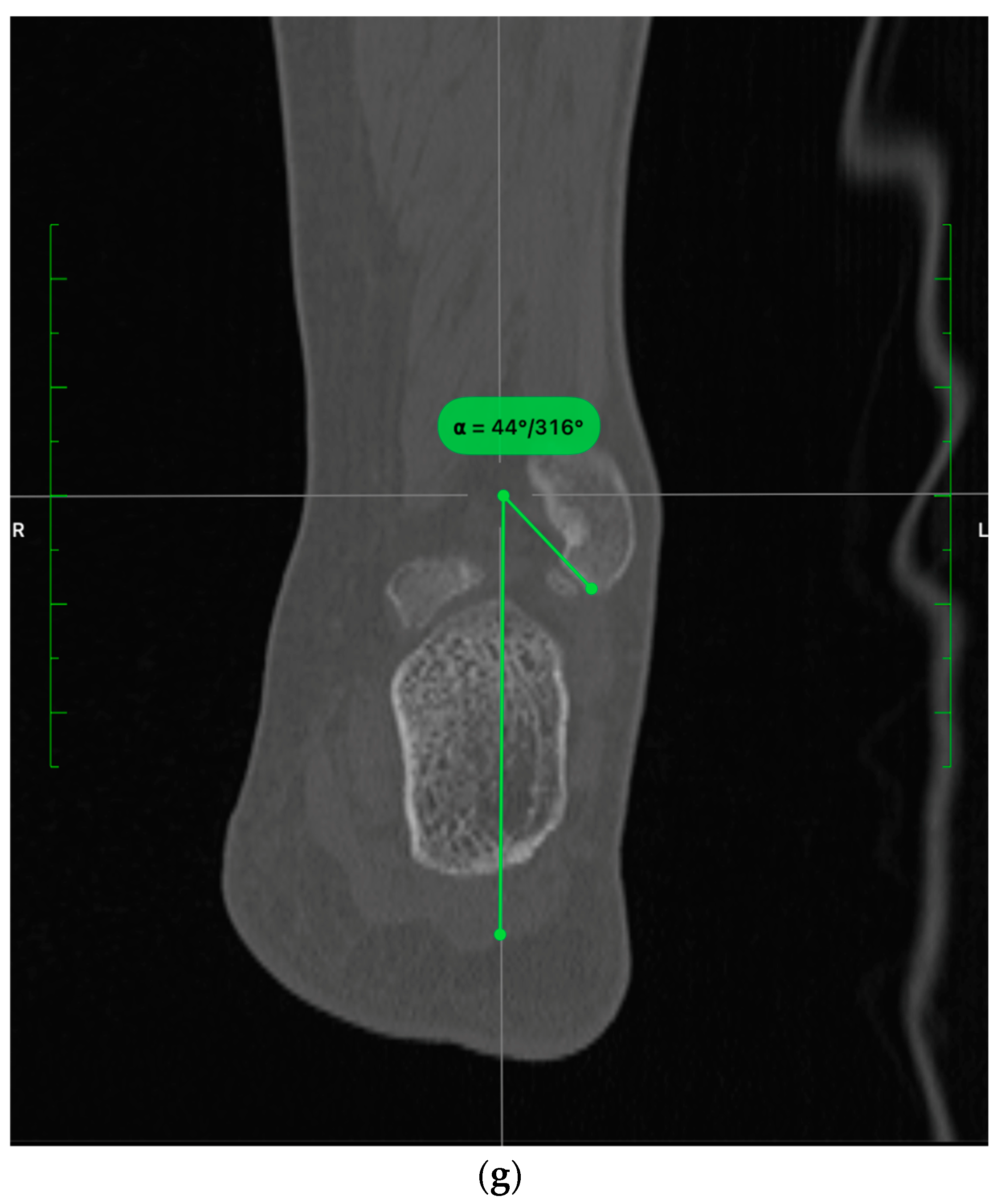
3.2. CT Evaluation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shibuya, N.; Davis, M.L.; Jupiter, D.C. Epidemiology of foot and ankle fractures in the United States: An analysis of the National Trauma Data Bank (2007 to 2011). J. Foot Ankle Surg. 2014, 53, 606–608. [Google Scholar] [CrossRef] [PubMed]
- Horisberger, M.; Valderrabano, V.; Hintermann, B. Posttraumatic ankle osteoarthritis after ankle-related fractures. J. Orthop. Trauma. 2009, 23, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Michelson, J.D.; Wright, M.; Blankstein, M. Syndesmotic Ankle Fractures. J. Orthop. Trauma. 2018, 32, 10–14. [Google Scholar] [CrossRef] [PubMed]
- Lauge-Hansen, N. Fractures of the ankle: II. Combined experimental-surgical and experimental-roentgenologic investigations. Arch. Surg. 1950, 60, 957–985. [Google Scholar] [CrossRef]
- Fonseca, L.L.D.; Nunes, I.G.; Nogueira, R.R.; Martins, G.E.V.; Mesencio, A.C.; Kobata, S.I. Reproducibility of the Lauge-Hansen, Danis-Weber, and AO classifications for ankle fractures. Rev. Bras. Ortop. 2018, 53, 101–106. [Google Scholar] [CrossRef]
- Ray, R.; Koohnejad, N.; Clement, N.D.; Keenan, G.F. Ankle fractures with syndesmotic stabilisation are associated with a high rate of secondary osteoarthritis. Foot Ankle Surg. 2019, 25, 180–185. [Google Scholar] [CrossRef]
- Weening, B.; Bhandari, M. Predictors of functional outcome following transsyndesmotic screw fixation of ankle fractures. J. Orthop. Trauma. 2005, 19, 102–108. [Google Scholar] [CrossRef]
- Loizou, C.L.; Sudlow, A.; Collins, R.; Loveday, D.; Smith, G. Radiological assessment of ankle syndesmotic reduction. Foot 2017, 32, 39–43. [Google Scholar] [CrossRef]
- Salameh, M.; Byun, S.E.; Chu, X.; Hadeed, M.; Funk, A.; Stacey, S.; Mauffrey, C.; Parry, J.A. Need for syndesmotic fixation and assessment of reduction during ankle fracture fixation, with and without contralateral fluoroscopic images, has poor interobserver reliability. Eur. J. Orthop. Surg. Traumatol. 2022, 32, 1089–1095. [Google Scholar] [CrossRef]
- Harper, M.C.; Keller, T.S. A radiographic evaluation of the tibiofibular syndesmosis. Foot Ankle 1989, 10, 156–160. [Google Scholar] [CrossRef]
- Manning, B.T.; Bohl, D.D.; Idarraga, A.J.P.; Holmes, G.B.; Lee, S.; Lin, J.L.; Hamid, K.S. Patient Knowledge Regarding Radiation Exposure From Foot and Ankle Imaging. Foot Ankle Spec. 2020, 13, 324–329. [Google Scholar] [CrossRef]
- Karaismailoglu, B.; Sahin, E.; Kara, M.; Tutuncu, M.N. Cortices of Fibula and Tibia Can Provide Landmarks for Accurate Syndesmosis Fixation Angle: Computed Tomography Validation of Angle Bisector Method. J. Foot Ankle Surg. 2023, in press. [Google Scholar] [CrossRef] [PubMed]
- Hermans, J.J.; Beumer, A.; de Jong, T.A.; Kleinrensink, G.J. Anatomy of the distal tibiofibular syndesmosis in adults: A pictorial essay with a multimodality approach. J. Anat. 2010, 217, 633–645. [Google Scholar] [CrossRef] [PubMed]
- Tornetta, P., 3rd; Yakavonis, M.; Veltre, D.; Shah, A. Reducing the Syndesmosis Under Direct Vision: Where Should I Look? J. Orthop. Trauma. 2019, 33, 450–454. [Google Scholar] [CrossRef] [PubMed]
- Ingall, E.M.; Kaiser, P.; Ashkani-Esfahani, S.; Zhao, J.; Kwon, J.Y. The Lateral Fibular Stress Test: High Variability of Force Applied by Orthopaedic Surgeons in a Biomechanical Model. Foot Ankle Orthop. 2022, 7, 24730114221106484. [Google Scholar] [CrossRef] [PubMed]
- Boszczyk, A.; Kwapisz, S.; Krummel, M.; Grass, R.; Rammelt, S. Correlation of Incisura Anatomy With Syndesmotic Malreduction. Foot Ankle Int. 2018, 39, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Gardner, M.J.; Demetrakopoulos, D.; Briggs, S.M.; Helfet, D.L.; Lorich, D.G. Malreduction of the tibiofibular syndesmosis in ankle fractures. Foot Ankle Int. 2006, 27, 788–792. [Google Scholar] [CrossRef]
- Gonzalez, T.; Egan, J.; Ghorbanhoseini, M.; Blais, M.; Lechtig, A.; Velasco, B.; Nazarian, A.; Kwon, J.Y. Overtightening of the syndesmosis revisited and the effect of syndesmotic malreduction on ankle dorsiflexion. Injury 2017, 48, 1253–1257. [Google Scholar] [CrossRef]
- Knops, S.P.; Kohn, M.A.; Hansen, E.N.; Matityahu, A.; Marmor, M. Rotational malreduction of the syndesmosis: Reliability and accuracy of computed tomography measurement methods. Foot Ankle Int. 2013, 34, 1403–1410. [Google Scholar] [CrossRef]
- de Souza, L.J.; Gustilo, R.B.; Meyer, T.J. Results of operative treatment of displaced external rotation-abduction fractures of the ankle. J. Bone Joint Surg. Am. 1985, 67, 1066–1074. [Google Scholar] [CrossRef]
- Pettrone, F.A.; Gail, M.; Pee, D.; Fitzpatrick, T.; Van Herpe, L.B. Quantitative criteria for prediction of the results after displaced fracture of the ankle. J. Bone Joint Surg. Am. 1983, 65, 667–677. [Google Scholar] [CrossRef]
- Pneumaticos, S.G.; Noble, P.C.; Chatziioannou, S.N.; Trevino, S.G. The effects of rotation on radiographic evaluation of the tibiofibular syndesmosis. Foot Ankle Int. 2002, 23, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Miyamoto, W.; Takao, M. Management of chronic disruption of the distal tibiofibular syndesmosis. World J. Orthop. 2011, 2, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Stride, D.; Horner, N.S.; Petrisor, B.; Johal, H.; Khan, M.; Alolabi, B. The Role of Deltoid Ligament Repair in Ankle Fractures With Syndesmotic Instability: A Systematic Review. J. Foot Ankle Surg. 2021, 60, 132–139. [Google Scholar] [CrossRef]
- Mococain, P.; Bejarano-Pineda, L.; Glisson, R.; Kadakia, R.J.; Akoh, C.C.; Chen, J.; Nunley, J.A.; Easley, M.E. Biomechanical Effect on Joint Stability of Including Deltoid Ligament Repair in an Ankle Fracture Soft Tissue Injury Model With Deltoid and Syndesmotic Disruption. Foot Ankle Int. 2020, 41, 1158–1164. [Google Scholar] [CrossRef]
- Grass, R.; Rammelt, S.; Biewener, A.; Zwipp, H. Peroneus longus ligamentoplasty for chronic instability of the distal tibiofibular syndesmosis. Foot Ankle Int. 2003, 24, 392–397. [Google Scholar] [CrossRef]
- Close, J.R. Some applications of the functional anatomy of the ankle joint. J. Bone Joint Surg. Am. 1956, 38, 761–781. [Google Scholar] [CrossRef] [PubMed]
- Tornetta, P., 3rd; Spoo, J.E.; Reynolds, F.A.; Lee, C. Overtightening of the ankle syndesmosis: Is it really possible? J. Bone Joint Surg. Am. 2001, 83, 489–492. [Google Scholar] [CrossRef]
- Baumbach, S.F.; Synek, A.; Spindler, F.T.; Bauer, L.; Bocker, W.; Polzer, H. Safe drilling zones for anteriorly, central, and posteriorly angulated syndesmotic stabilization devices. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 2199–2207. [Google Scholar] [CrossRef] [PubMed]
- Ovaska, M.T.; Makinen, T.J.; Madanat, R.; Kiljunen, V.; Lindahl, J. A comprehensive analysis of patients with malreduced ankle fractures undergoing re-operation. Int. Orthop. 2014, 38, 83–88. [Google Scholar] [CrossRef]
- Weber, D.; Friederich, N.F.; Muller, W. Lengthening osteotomy of the fibula for post-traumatic malunion. Indications, technique and results. Int. Orthop. 1998, 22, 149–152. [Google Scholar] [CrossRef][Green Version]
- Curtis, M.J.; Michelson, J.D.; Urquhart, M.W.; Byank, R.P.; Jinnah, R.H. Tibiotalar contact and fibular malunion in ankle fractures. A cadaver study. Acta Orthop. Scand. 1992, 63, 326–329. [Google Scholar] [CrossRef]
- Darwich, A.; Adam, J.; Dally, F.J.; Hetjens, S.; Jawhar, A. Correction to: Incidence of concomitant chondral/osteochondral lesions in acute ankle fractures and their effect on clinical outcome: A systematic review and meta-analysis. Arch. Orthop. Trauma. Surg. 2021, 141, 1437–1438. [Google Scholar] [CrossRef] [PubMed]
- Martijn, H.A.; Lambers, K.T.A.; Dahmen, J.; Stufkens, S.A.S.; Kerkhoffs, G. High incidence of (osteo)chondral lesions in ankle fractures. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 1523–1534. [Google Scholar] [CrossRef] [PubMed]
- Williamson, E.R.C.; Shimozono, Y.; Toale, J.; Dankert, J.; Hurley, E.T.; Egol, K.A.; Kennedy, J.G. Incidence of Chondral and Osteochondral Lesions in Ankle Fracture Patients Identified With Ankle Arthroscopy Following Rotational Ankle Fracture: A Systematic Review. J. Foot Ankle Surg. 2022, 61, 668–673. [Google Scholar] [CrossRef] [PubMed]
- van Dijk, C.N.; Verhagen, R.A.; Tol, J.L. Arthroscopy for problems after ankle fracture. J. Bone Joint Surg. Br. 1997, 79, 280–284. [Google Scholar] [CrossRef]
- Chen, Y.; Qiang, M.; Zhang, K.; Li, H.; Dai, H. A reliable radiographic measurement for evaluation of normal distal tibiofibular syndesmosis: A multi-detector computed tomography study in adults. J. Foot Ankle Res. 2015, 8, 32. [Google Scholar] [CrossRef]


| 113 |
|
| 62 |
|
| 42 |
|
| Gender | 23M/16F |
|---|---|
| Mean Age | 41.6 years [Range: 19–71] |
| Injury Mechanism | SER: 73.68% PER: 26.32% |
| Torn AITFL | 42/42 (100%) |
|---|---|
| Midsubstance rupture | 37/42 (88%) |
| Tibial insertion | 4/42 (9%) |
| Fibular insertion | 1/42 (3%) |
| Gross proximal fragment instability | 13/42 (30.9%) |
| SER | 2/13 |
| PER | 11/13 |
| IA loose bodies | 9/42 (21.4%) |
| Incisura Depth (mm) | Incisura Rotation (deg) | Fibular Engagement (mm) | Fibula Anterior Translation | Fibula Length (deg) | Relative Torsion (deg) | Torsion (deg) | |
|---|---|---|---|---|---|---|---|
| Healthy side | 4.08 | −3.26 | 0.81 | 8.8 | 50.6 | 9.35 | −2.58 |
| Injured side | 3.6 | −3.33 | 0.59 | 9.33 | 49.2 | 12.8 | 0.5 |
| Side to side mean Difference | 0.48 | 0.06 | 0.22 | −0.52 | 1.3 | −3.4 | −3.1 |
| p | >0.05 | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rozis, M.; Zachariou, D.; Vavourakis, M.; Vasiliadis, E.; Vlamis, J. Anterior Incisura Fibularis Corner Landmarks Can Safely Validate the Optimal Distal Tibiofibular Reduction in Malleolar Fractures—Prospective CT Study. Diagnostics 2023, 13, 2615. https://doi.org/10.3390/diagnostics13152615
Rozis M, Zachariou D, Vavourakis M, Vasiliadis E, Vlamis J. Anterior Incisura Fibularis Corner Landmarks Can Safely Validate the Optimal Distal Tibiofibular Reduction in Malleolar Fractures—Prospective CT Study. Diagnostics. 2023; 13(15):2615. https://doi.org/10.3390/diagnostics13152615
Chicago/Turabian StyleRozis, Meletis, Dimitrios Zachariou, Michalis Vavourakis, Elias Vasiliadis, and John Vlamis. 2023. "Anterior Incisura Fibularis Corner Landmarks Can Safely Validate the Optimal Distal Tibiofibular Reduction in Malleolar Fractures—Prospective CT Study" Diagnostics 13, no. 15: 2615. https://doi.org/10.3390/diagnostics13152615
APA StyleRozis, M., Zachariou, D., Vavourakis, M., Vasiliadis, E., & Vlamis, J. (2023). Anterior Incisura Fibularis Corner Landmarks Can Safely Validate the Optimal Distal Tibiofibular Reduction in Malleolar Fractures—Prospective CT Study. Diagnostics, 13(15), 2615. https://doi.org/10.3390/diagnostics13152615







