Diagnostic Performance of the Darth Vader Sign for the Diagnosis of Lumbar Spondylolysis in Routinely Acquired Abdominal CT
Abstract
1. Introduction
2. Materials & Methods
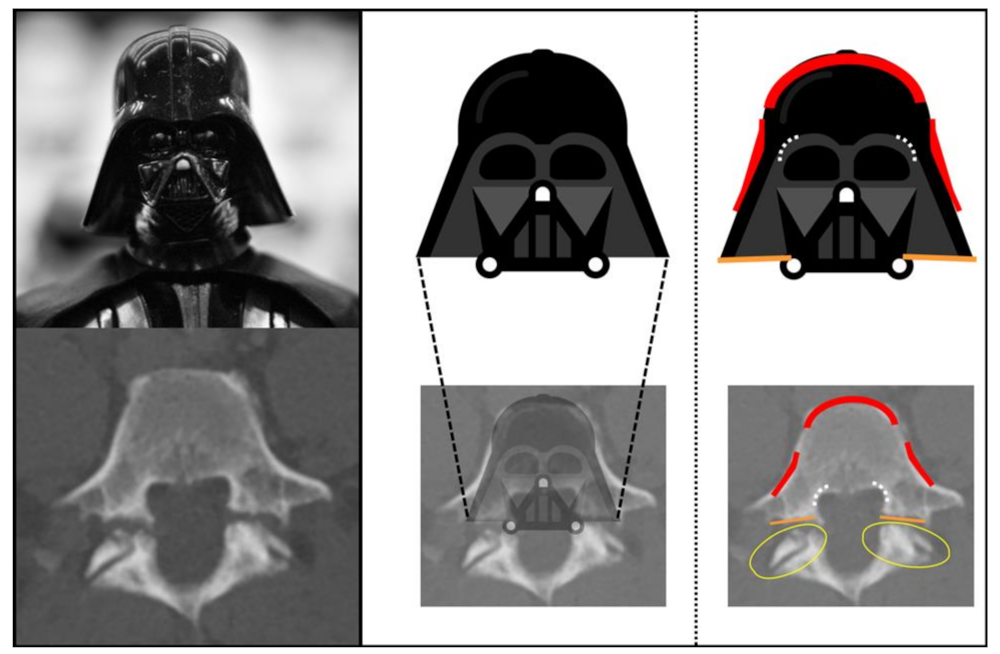
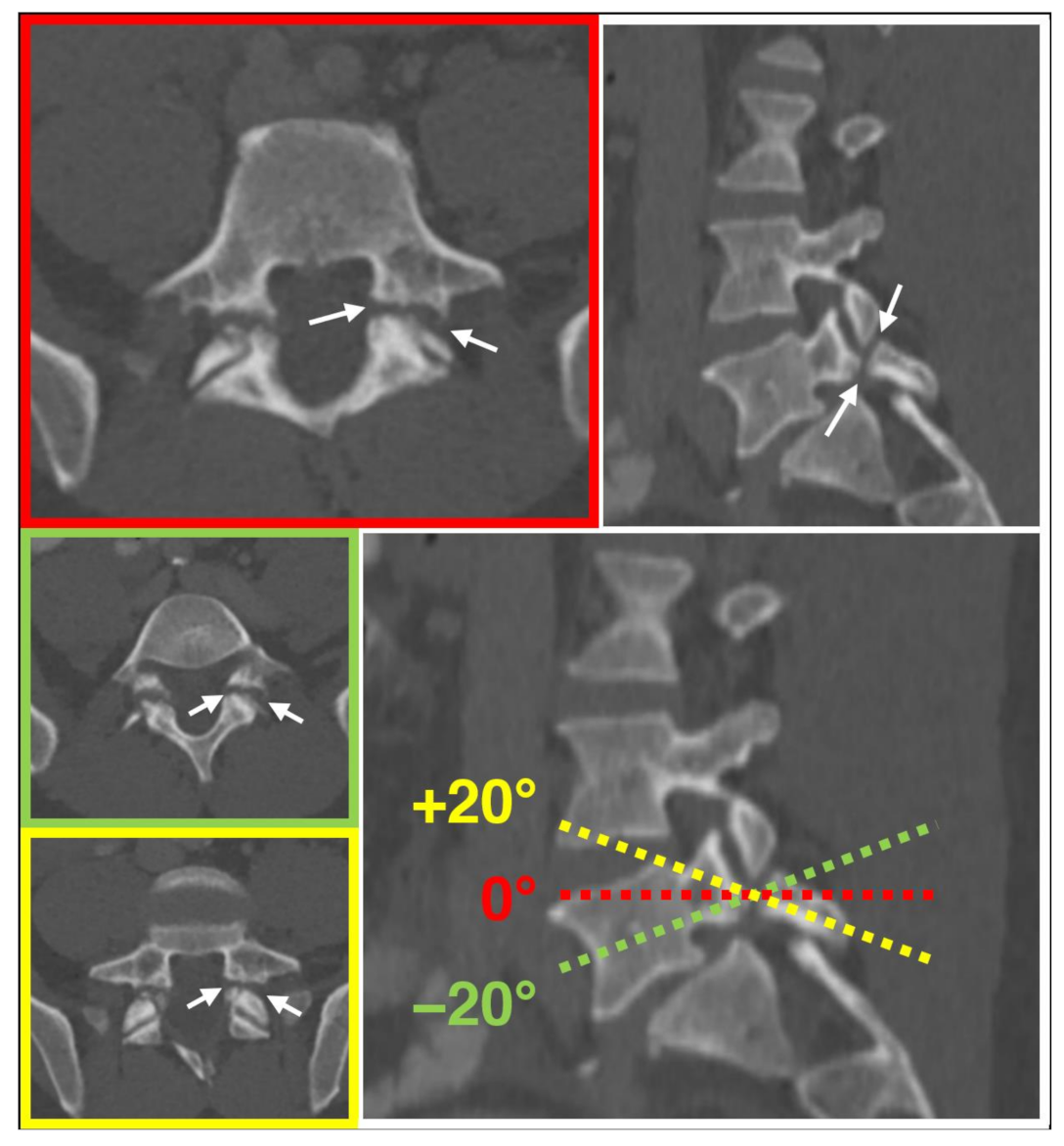
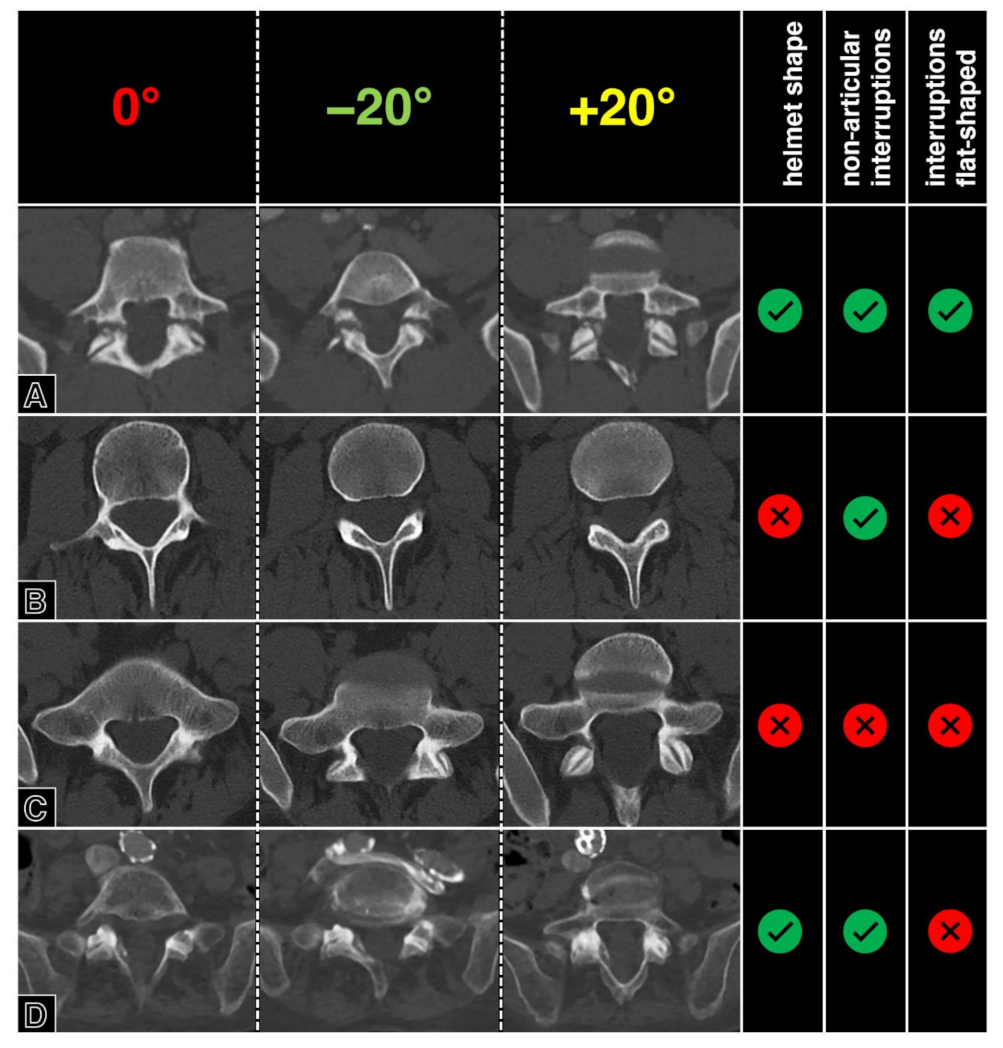
2.1. Definition of the Darth Vader Sign
2.2. Feasibility Testing
2.3. Patient and Image Selection
2.4. Image Readout
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ANOVA | Analysis of variance |
| AUC | Area under the curve |
| CT | Computed tomography |
| PACS | Picture archiving and communication system |
References
- Stock, L.; March, J.; Afram, P.; Dolan, H.; Ganguly, R.; Grange, E. Star Wars: Jedi Battles; DK Children: London, UK, 2014. [Google Scholar]
- Wallace, D.; Anderson, K.J.; Chiarello, M.; Edwards, T.L.; Van Fleet, J. Star Wars: The New Essential Chronology; Del Rey Books: New York, NY, USA, 2005. [Google Scholar]
- Galluccio, A.C. Spondylolisthesis; Further remarks with emphasis on radiologic aspects. Radiology 1946, 46, 356–363. [Google Scholar] [CrossRef] [PubMed]
- Harris, R.I. Spondylolisthesis. Ann. R. Coll. Surg. Engl. 1951, 8, 259–297. [Google Scholar] [PubMed]
- Wiltse, L.L.; Newman, P.H.; Macnab, I. Classification of spondylolisis and spondylolisthesis. Clin. Orthop. Relat. Res. 1976, 117, 23–29. [Google Scholar]
- Marchetti, P.G.; Bartolozzi, P. Classification of Spondylolisthesis as a guideline for treatment. In Textbook of Spinal Surgery; Bridwell, K.H., Dewald, R.L., Hammerberg, K.W., Eds.; Lippincott-Raven: Philadelphia, PA, USA, 1997; pp. 1211–1254. [Google Scholar]
- Mardjetko, S.; Albert, T.; Andersson, G.; Bridwell, K.; DeWald, C.; Gaines, R.; Geck, M.; Hammerberg, K.; Herkowitz, H.; Kwon, B.; et al. Spine/SRS spondylolisthesis summary statement. Spine 2005, 30 (Suppl. S6), S3. [Google Scholar] [CrossRef] [PubMed]
- Kepler, C.K.; Hilibrand, A.S.; Sayadipour, A.; Koerner, J.D.; Rihn, J.A.; Radcliff, K.E.; Vaccaro, A.R.; Albert, T.J.; Anderson, D.G. Clinical and radiographic degenerative spondylolisthesis (CARDS) classification. Spine J. 2015, 15, 1804–1811. [Google Scholar] [CrossRef] [PubMed]
- Gille, O.; Bouloussa, H.; Mazas, S.; Vergari, C.; Challier, V.; Vital, J.M.; Coudert, P.; Ghailane, S. A new classification system for degenerative spondylolisthesis of the lumbar spine. Eur. Spine J. 2017, 26, 3096–3105. [Google Scholar] [CrossRef] [PubMed]
- Meyerding, H.W. Spondylolisthesis. Surg. Gynecol. Obstet. 1932, 54, 371–377. [Google Scholar]
- Koslosky, E.; Gendelberg, D. Classification in Brief: The Meyerding Classification System of Spondylolisthesis. Clin. Orthop. Relat. Res. 2020, 478, 1125–1130. [Google Scholar]
- Ghogawala, Z.; Dunbar, M.R.; Essa, I. Lumbar spondylolisthesis: Modern registries and the development of artificial intelligence. J. Neurosurg. Spine 2019, 30, 729–735. [Google Scholar] [CrossRef]
- Liao, S.; Zhan, Y.; Dong, Z.; Yan, R.; Gong, L.; Zhou, X.S.; Salganicoff, M.; Fei, J. Automatic Lumbar Spondylolisthesis Measurement in CT Images. IEEE Trans. Med. Imaging 2016, 35, 1658–1669. [Google Scholar] [CrossRef]
- Teplick, J.G.; Laffey, P.A.; Berman, A.; Haskin, M.E. Diagnosis and evaluation of spondylolisthesis and/or spondylolysis on axial CT. Am. J. Neuroradiol. 1986, 7, 479–491. [Google Scholar] [PubMed]
- Nakayama, T.; Ehara, S. Spondylolytic spondylolisthesis: Various imaging features and natural courses. Jpn. J. Radiol. 2015, 33, 3–12. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Leone, A.; Cianfoni, A.; Cerase, A.; Magarelli, N.; Bonomo, L. Lumbar spondylolysis: A review. Skelet. Radiol. 2011, 40, 683–700. [Google Scholar] [CrossRef] [PubMed]
- Campbell, R.S.; Grainger, A.J.; Hide, I.G.; Papastefanou, S.; Greenough, C.G. Juvenile spondylolysis: A comparative analysis of CT, SPECT and MRI. Skelet. Radiol. 2005, 34, 63–73. [Google Scholar] [CrossRef]
- Trout, A.T.; Sharp, S.E.; Anton, C.G.; Gelfand, M.J.; Mehlman, C.T. Spondylolysis and Beyond: Value of SPECT/CT in Evaluation of Low Back Pain in Children and Young Adults. Radiographics 2015, 35, 819–834. [Google Scholar] [CrossRef]
- Chung, C.C.; Shimer, A.L. Lumbosacral Spondylolysis and Spondylolisthesis. Clin. Sports Med. 2021, 40, 471–490. [Google Scholar] [CrossRef]
- Ulmer, J.L.; Mathews, V.P.; Elster, A.D.; Mark, L.P.; Daniels, D.L.; Mueller, W. MR imaging of lumbar spondylolysis: The importance of ancillary observations. AJR Am. J. Roentgenol. 1997, 169, 233–239. [Google Scholar] [CrossRef]
- Jinkins, J.R.; Matthes, J.C.; Sener, R.N.; Venkatappan, S.; Rauch, R. Spondylolysis, spondylolisthesis, and associated nerve root entrapment in the lumbosacral spine: MR evaluation. AJR Am. J. Roentgenol. 1992, 159, 799–803. [Google Scholar] [CrossRef]
- Kreiner, D.S.; Baisden, J.; Mazanec, D.J.; Patel, R.D.; Bess, R.S.; Burton, D.; Chutkan, N.B.; Cohen, B.A.; Crawford, C.H.; Ghiselli, G.; et al. Guideline summary review: An evidence-based clinical guideline for the diagnosis and treatment of adult isthmic spondylolisthesis. Spine J. 2016, 16, 1478–1485. [Google Scholar] [CrossRef]
- Daghighi, M.H.; Poureisa, M.; Arablou, F.; Fouladi, D.F. Supine spinal magnetic resonance imaging with straightened lower extremities in spondylolisthesis: A comparison with the conventional technique. Eur. J. Radiol. 2015, 84, 921–926. [Google Scholar] [CrossRef]
- Wang, D.; Yuan, H.; Liu, A.; Li, C.; Yang, K.; Zheng, S.; Wang, L.; Wang, J.C.; Buser, Z. Analysis of the relationship between the facet fluid sign and lumbar spine motion of degenerative spondylolytic segment using Kinematic MRI. Eur. J. Radiol. 2017, 94, 6–12. [Google Scholar]
- McAfee, P.C.; Yuan, H.A. Computed tomography in spondylolisthesis. Clin. Orthop. Relat. Res. 1982, 166, 62–71. [Google Scholar] [CrossRef]
- Aoki, Y.; Takahashi, H.; Nakajima, A.; Kubota, G.; Watanabe, A.; Nakajima, T.; Eguchi, Y.; Orita, S.; Fukuchi, H.; Yanagawa, N.; et al. Prevalence of lumbar spondylolysis and spondylolisthesis in patients with degenerative spinal disease. Sci. Rep. 2020, 10, 6739. [Google Scholar] [CrossRef]
- Foreman, P.; Griessenauer, C.J.; Watanabe, K.; Conklin, M.; Shoja, M.M.; Rozzelle, C.J.; Loukas, M.; Tubbs, R.S. L5 spondylolysis/spondylolisthesis: A comprehensive review with an anatomic focus. Childs Nerv. Syst. 2013, 29, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Floman, Y. Progression of lumbosacral isthmic spondylolisthesis in adults. Spine 2000, 25, 342–347. [Google Scholar]
- Libson, E.; Bloom, R.A.; Dinari, G. Symptomatic and asymptomatic spondylolysis and spondylolisthesis in young adults. Int. Orthop. 1983, 6, 259–261. [Google Scholar]
- Zack, O.; Barak, Y.; Finestone, A.S.; Krakov, A.; Slodownik, D.; Alperovitch-Najenson, D.; Moshe, S. Occupational influences on Spondylolysis and Spondylolisthesis in a cohort of 18-year-old male military conscripts. BMC Musculoskelet. Disord. 2020, 21, 720. [Google Scholar]
- Steinberg, E.L.; Luger, E.; Arbel, R.; Menachem, A.; Dekel, S. A comparative roentgenographic analysis of the lumbar spine in male army recruits with and without lower back pain. Clin. Radiol. 2003, 58, 985–989. [Google Scholar] [CrossRef] [PubMed]
- Donald, J.J.; Barnard, S.A. Common patterns in 558 diagnostic radiology errors. J. Med. Imaging Radiat. Oncol. 2012, 56, 173–178. [Google Scholar] [CrossRef]
- Siewert, B.; Sosna, J.; McNamara, A.; Raptopoulos, V.; Kruskal, J.B. Missed lesions at abdominal oncologic CT: Lessons learned from quality assurance. Radiographics 2008, 28, 623–638. [Google Scholar] [CrossRef]
- Horton, K.M.; Johnson, P.T.; Fishman, E.K. MDCT of the abdomen: Common misdiagnoses at a busy academic center. AJR Am. J. Roentgenol. 2010, 194, 660–667. [Google Scholar] [PubMed]
- Elster, A.D.; Jensen, K.M. Importance of sagittally reformatted images in CT evaluation of spondylolisthesis. Am. J. Neuroradiol. 1986, 7, 1102–1103. [Google Scholar] [PubMed]
- Fortin, J. An algorithm for understanding spine imaging. Pain Physician 2002, 5, 102–109. [Google Scholar] [CrossRef]
- Bartalena, T.; Giannelli, G.; Rinaldi, M.F.; Rimondi, E.; Rinaldi, G.; Sverzellati, N.; Gavelli, G. Prevalence of thoracolumbar vertebral fractures on multidetector CT: Underreporting by radiologists. Eur. J. Radiol. 2009, 69, 555–559. [Google Scholar] [CrossRef] [PubMed]
- Hosmer, D.W.; Lemeshow, S.; Sturdivant, R.X. Applied Logistic Regression, 3rd ed.; John Wiley & Sons, Inc.: New York, NY, USA, 2013. [Google Scholar]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar]
- Millard, L. The Scotty dog and his collar. J. Ark. Med. Soc. 1976, 72, 339–340. [Google Scholar]
- Talangbayan, L.E. The inverted Napoleon’s hat sign. Radiology 2007, 243, 603–604. [Google Scholar] [CrossRef]
- Lantsman, C.D.; Barash, Y.; Klang, E.; Guranda, L.; Konen, E.; Tau, N. Trend in radiologist workload compared to number of admissions in the emergency department. Eur. J. Radiol. 2022, 149, 110195. [Google Scholar] [CrossRef]
- Peng, Y.C.; Lee, W.J.; Chang, Y.C.; Chan, W.P.; Chen, S.J. Radiologist burnout: Trends in medical imaging utilization under the national health insurance system with the universal code bundling strategy in an academic tertiary medical centre. Eur. J. Radiol. 2022, 157, 110596. [Google Scholar] [CrossRef]
- Cheung, K.K.; Dhawan, R.T.; Wilson, L.F.; Peirce, N.S.; Rajeswaran, G. Pars interarticularis injury in elite athletes—The role of imaging in diagnosis and management. Eur. J. Radiol. 2018, 108, 28–42. [Google Scholar]
- Ulmer, J.L.; Elster, A.D.; Mathews, V.P.; King, J.C. Distinction between degenerative and isthmic spondylolisthesis on sagittal MR images: Importance of increased anteroposterior diameter of the spinal canal (“wide canal sign”). Am. J. Roentgenol. 1994, 163, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Huber, F.A.; Guggenberger, R. AI MSK clinical applications: Spine imaging. Skelet. Radiol. 2021, 51, 279–291. [Google Scholar] [CrossRef] [PubMed]

| Group | Spondylolysis | Degenerative Spondylolisthesis | Controls |
|---|---|---|---|
| Cases (N = 59) | 40 (68%) | 13 (22%) | 6 (10%) |
| Age (mean ± SD) | 55.5 ± 15.7 | 73.5 ± 11.1 * | 54.8 ± 15.7 |
| Sex (%) | 14 (35%) Female | 8 (62%) Female | 2 (33%) Female |
| Meyerding Grade (0/1/2/3/4) | 9/13/13/5/- | -/11/2/-/- | - |
| Spondylolysis | Degenerative Spondylolisthesis | ||
|---|---|---|---|
| L 3 | 2 | L 3/4 | 1 |
| L 4 | 4 | L 4/5 | 5 |
| L 5 | 34 (6 unilateral) | L 5/S 1 | 7 |
| Overall | 40 (6 unilateral) | Overall | 13 |
| All Spondylolysis Cases | Bilateral Spondylolysis Cases | |||
|---|---|---|---|---|
| Reader | R3 | R4 | R3 | R4 |
| Sensitivity (%) | 65 | 80 | 76.5 | 88.2 |
| Specificity (%) | 99 | 98 | 99 | 96.2 |
| AUC | 0.820 | 0.890 | 0.878 | 0.922 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huber, F.A.; Schmidt, C.S.; Alkadhi, H. Diagnostic Performance of the Darth Vader Sign for the Diagnosis of Lumbar Spondylolysis in Routinely Acquired Abdominal CT. Diagnostics 2023, 13, 2616. https://doi.org/10.3390/diagnostics13152616
Huber FA, Schmidt CS, Alkadhi H. Diagnostic Performance of the Darth Vader Sign for the Diagnosis of Lumbar Spondylolysis in Routinely Acquired Abdominal CT. Diagnostics. 2023; 13(15):2616. https://doi.org/10.3390/diagnostics13152616
Chicago/Turabian StyleHuber, Florian A., Cynthia S. Schmidt, and Hatem Alkadhi. 2023. "Diagnostic Performance of the Darth Vader Sign for the Diagnosis of Lumbar Spondylolysis in Routinely Acquired Abdominal CT" Diagnostics 13, no. 15: 2616. https://doi.org/10.3390/diagnostics13152616
APA StyleHuber, F. A., Schmidt, C. S., & Alkadhi, H. (2023). Diagnostic Performance of the Darth Vader Sign for the Diagnosis of Lumbar Spondylolysis in Routinely Acquired Abdominal CT. Diagnostics, 13(15), 2616. https://doi.org/10.3390/diagnostics13152616






