Neurological and Psychiatric Manifestations of Long COVID-19 and Their [18F]FDG PET Findings: A Review
Abstract
1. Introduction
2. Etiopathogenesis of Neuropsychiatric Manifestations of Long COVID-19
3. Neurological Manifestations of Long COVID-19
4. Psychiatric Manifestations of Long COVID-19
5. PET Findings in the Brain in Patients with Long COVID-19
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alimohamadi, Y.; Sepandi, M.; Taghdir, M.; Hosamirudsari, H. Determine the Most Common Clinical Symptoms in COVID-19 Patients: A Systematic Review and Meta-Analysis. J. Prev. Med. Hyg. 2020, 61, E304–E312. [Google Scholar] [CrossRef]
- Mahase, E. Covid-19: Sore Throat, Fatigue, and Myalgia Are More Common with New UK Variant. BMJ 2021, 372, n288. [Google Scholar] [CrossRef]
- Shah, S.; Danda, D.; Kavadichanda, C.; Das, S.; Adarsh, M.B.; Negi, V.S. Autoimmune and Rheumatic Musculoskeletal Diseases as a Consequence of SARS-CoV-2 Infection and Its Treatment. Rheumatol. Int. 2020, 40, 1539–1554. [Google Scholar] [CrossRef]
- Jain, U. Effect of COVID-19 on the Organs. Cureus 2020, 12, e9540. [Google Scholar] [CrossRef]
- Iadecola, C.; Anrather, J.; Kamel, H. Effects of COVID-19 on the Nervous System. Cell 2020, 183, 16–27.e1. [Google Scholar] [CrossRef]
- Toptan, T.; Aktan, Ç.; Başarı, A.; Bolay, H. Case Series of Headache Characteristics in COVID-19: Headache Can Be an Isolated Symptom. Headache 2020, 60, 1788–1792. [Google Scholar] [CrossRef]
- Mattace-Raso, F.; Polinder-Bos, H.; Oosterwijk, B.; van Bruchem-Visser, R.; Goudzwaard, J.; Oudshoorn, C.; Ziere, G.; Egberts, A. Delirium: A Frequent Manifestation in COVID-19 Older Patients. Clin. Interv. Aging 2020, 15, 2245–2247. [Google Scholar] [CrossRef]
- Banerjee, D.; Viswanath, B. Neuropsychiatric Manifestations of COVID-19 and Possible Pathogenic Mechanisms: Insights from Other Coronaviruses. Asian J. Psychiatr. 2020, 54, 102350. [Google Scholar] [CrossRef] [PubMed]
- Rogers, J.P.; Chesney, E.; Oliver, D.; Pollak, T.A.; McGuire, P.; Fusar-Poli, P.; Zandi, M.S.; Lewis, G.; David, A.S. Psychiatric and Neuropsychiatric Presentations Associated with Severe Coronavirus Infections: A Systematic Review and Meta-Analysis with Comparison to the COVID-19 Pandemic. Lancet Psychiatry 2020, 7, 611–627. [Google Scholar] [CrossRef] [PubMed]
- Selvakumar, J.; Havdal, L.B.; Drevvatne, M.; Brodwall, E.M.; Berven, L.L.; Stiansen-Sonerud, T.; Einvik, G.; Leegaard, T.M.; Tjade, T.; Michelsen, A.E.; et al. Prevalence and Characteristics Associated with Post–COVID-19 Condition Among Nonhospitalized Adolescents and Young Adults. JAMA Netw. Open 2023, 6, e235763. [Google Scholar] [CrossRef] [PubMed]
- Stefanou, M.-I.; Palaiodimou, L.; Bakola, E.; Smyrnis, N.; Papadopoulou, M.; Paraskevas, G.P.; Rizos, E.; Boutati, E.; Grigoriadis, N.; Krogias, C.; et al. Neurological Manifestations of Long-COVID Syndrome: A Narrative Review. Ther. Adv. Chronic Dis. 2022, 13, 20406223221076890. [Google Scholar] [CrossRef]
- Kontoangelos, K.; Economou, M.; Papageorgiou, C. Mental Health Effects of COVID-19 Pandemia: A Review of Clinical and Psychological Traits. Psychiatry Investig. 2020, 17, 491–505. [Google Scholar] [CrossRef]
- Soriano, J.B.; Murthy, S.; Marshall, J.C.; Relan, P.; Diaz, J.V. WHO Clinical Case Definition Working Group on Post-COVID-19 Condition A Clinical Case Definition of Post-COVID-19 Condition by a Delphi Consensus. Lancet Infect. Dis. 2022, 22, e102–e107. [Google Scholar] [CrossRef]
- Cascella, M.; Rajnik, M.; Aleem, A.; Dulebohn, S.C.; Di Napoli, R. Features, Evaluation, and Treatment of Coronavirus (COVID-19); StatPearls Publishing: St. Petersburg, FL, USA, 2023. [Google Scholar]
- Chen, R.; Wang, K.; Yu, J.; Howard, D.; French, L.; Chen, Z.; Wen, C.; Xu, Z. The Spatial and Cell-Type Distribution of SARS-CoV-2 Receptor ACE2 in the Human and Mouse Brains. Front. Neurol. 2020, 11, 573095. [Google Scholar] [CrossRef]
- Zubair, A.S.; McAlpine, L.S.; Gardin, T.; Farhadian, S.; Kuruvilla, D.E.; Spudich, S. Neuropathogenesis and Neurologic Manifestations of the Coronaviruses in the Age of Coronavirus Disease 2019: A Review. JAMA Neurol. 2020, 77, 1018–1027. [Google Scholar] [CrossRef] [PubMed]
- Crunfli, F.; Carregari, V.C.; Veras, F.P.; Silva, L.S.; Nogueira, M.H.; Antunes, A.S.L.M.; Vendramini, P.H.; Valença, A.G.F.; Brandão-Teles, C.; Zuccoli, G.d.S.; et al. Morphological, Cellular, and Molecular Basis of Brain Infection in COVID-19 Patients. Proc. Natl. Acad. Sci. USA 2022, 119, e2200960119. [Google Scholar] [CrossRef] [PubMed]
- Steardo, L., Jr.; Steardo, L.; Scuderi, C. Astrocytes and the Psychiatric Sequelae of COVID-19: What We Learned from the Pandemic. Neurochem. Res. 2023, 48, 1015–1025. [Google Scholar] [CrossRef] [PubMed]
- Pathak, D.; Sriram, K. Molecular Mechanisms Underlying Neuroinflammation Elicited by Occupational Injuries and Toxicants. Int. J. Mol. Sci. 2023, 24, 2272. [Google Scholar] [CrossRef]
- Carroll, E.; Neumann, H.; Aguero-Rosenfeld, M.E.; Lighter, J.; Czeisler, B.M.; Melmed, K.; Lewis, A. Post-COVID-19 Inflammatory Syndrome Manifesting as Refractory Status Epilepticus. Epilepsia 2020, 61, e135–e139. [Google Scholar] [CrossRef]
- Emecen, A.N.; Keskin, S.; Turunc, O.; Suner, A.F.; Siyve, N.; Basoglu Sensoy, E.; Dinc, F.; Kilinc, O.; Avkan Oguz, V.; Bayrak, S.; et al. The Presence of Symptoms within 6 Months after COVID-19: A Single-Center Longitudinal Study. Ir. J. Med. Sci. 2022, 192, 741–750. [Google Scholar] [CrossRef]
- Liu, J.W.T.W.; Liu, J.W.T.; de Luca, R.D.; Neto, H.O.M.; Barcellos, I. Post-COVID-19 Syndrome? New Daily Persistent Headache in the Aftermath of COVID-19. Arq. Neuro-Psiquiatr. 2020, 78, 753–754. [Google Scholar] [CrossRef]
- Hoffer, E.P. Long COVID: Does It Exist? What Is It? We Can We Do For Sufferers? Am. J. Med. 2021, 134, 1310–1311. [Google Scholar] [CrossRef] [PubMed]
- Del Brutto, O.H.; Wu, S.; Mera, R.M.; Costa, A.F.; Recalde, B.Y.; Issa, N.P. Cognitive Decline among Individuals with History of Mild Symptomatic SARS-CoV-2 Infection: A Longitudinal Prospective Study Nested to a Population Cohort. Eur. J. Neurol. 2021, 28, 3245–3253. [Google Scholar] [CrossRef] [PubMed]
- Kantonen, J.; Mahzabin, S.; Mäyränpää, M.I.; Tynninen, O.; Paetau, A.; Andersson, N.; Sajantila, A.; Vapalahti, O.; Carpén, O.; Kekäläinen, E.; et al. Neuropathologic Features of Four Autopsied COVID-19 Patients. Brain Pathol. 2020, 30, 1012–1016. [Google Scholar] [CrossRef] [PubMed]
- Reichard, R.R.; Kashani, K.B.; Boire, N.A.; Constantopoulos, E.; Guo, Y.; Lucchinetti, C.F. Neuropathology of COVID-19: A Spectrum of Vascular and Acute Disseminated Encephalomyelitis (ADEM)-like Pathology. Acta Neuropathol. 2020, 140, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Halpin, S.J.; McIvor, C.; Whyatt, G.; Adams, A.; Harvey, O.; McLean, L.; Walshaw, C.; Kemp, S.; Corrado, J.; Singh, R.; et al. Postdischarge Symptoms and Rehabilitation Needs in Survivors of COVID-19 Infection: A Cross-Sectional Evaluation. J. Med. Virol. 2021, 93, 1013–1022. [Google Scholar] [CrossRef]
- Hu, Y.; Liang, W.H.; Ou, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar]
- Nazari, S.; Azari Jafari, A.; Mirmoeeni, S.; Sadeghian, S.; Heidari, M.E.; Sadeghian, S.; Assarzadegan, F.; Puormand, S.M.; Ebadi, H.; Fathi, D.; et al. Central Nervous System Manifestations in COVID-19 Patients: A Systematic Review and Meta-Analysis. Brain Behav. 2021, 11, e02025. [Google Scholar] [CrossRef]
- Pinzon, R.T.; Wijaya, V.O.; Jody, A.A.; Nunsio, P.N.; Buana, R.B. Persistent Neurological Manifestations in Long COVID-19 Syndrome: A Systematic Review and Meta-Analysis. J. Infect. Public Health 2022, 15, 856–869. [Google Scholar] [CrossRef]
- Mazza, M.G.; De Lorenzo, R.; Conte, C.; Poletti, S.; Vai, B.; Bollettini, I.; Melloni, E.M.T.; Furlan, R.; Ciceri, F.; Rovere-Querini, P.; et al. Anxiety and Depression in COVID-19 Survivors: Role of Inflammatory and Clinical Predictors. Brain Behav. Immun. 2020, 89, 594–600. [Google Scholar] [CrossRef]
- Czeisler, M.É.; Lane, R.I.; Petrosky, E.; Wiley, J.F.; Christensen, A.; Njai, R.; Weaver, M.D.; Robbins, R.; Facer-Childs, E.R.; Barger, L.K.; et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic—United States, June 24–30, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1049–1057. [Google Scholar] [CrossRef]
- Mao, L.; Jin, H.; Wang, M.; Hu, Y.; Chen, S.; He, Q.; Chang, J.; Hong, C.; Zhou, Y.; Wang, D.; et al. Neurologic Manifestations of Hospitalized Patients with Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol. 2020, 77, 683. [Google Scholar] [CrossRef] [PubMed]
- Cullen, W.; Gulati, G.; Kelly, B.D. Mental Health in the COVID-19 Pandemic. QJM 2020, 113, 311–312. [Google Scholar] [CrossRef] [PubMed]
- van Vuren, E.J.; Steyn, S.F.; Brink, C.B.; Möller, M.; Viljoen, F.P.; Harvey, B.H. The Neuropsychiatric Manifestations of COVID-19: Interactions with Psychiatric Illness and Pharmacological Treatment. Biomed. Pharmacother. 2021, 135, 111200. [Google Scholar] [CrossRef]
- Varatharaj, A.; Thomas, N.; Ellul, M.A.; Davies, N.W.S.; Pollak, T.A.; Tenorio, E.L.; Sultan, M.; Easton, A.; Breen, G.; Zandi, M.; et al. Neurological and Neuropsychiatric Complications of COVID-19 in 153 Patients: A UK-Wide Surveillance Study. Lancet Psychiatry 2020, 7, 875–882. [Google Scholar] [CrossRef] [PubMed]
- Steardo, L., Jr.; Steardo, L.; Verkhratsky, A. Psychiatric Face of COVID-19. Transl. Psychiatry 2020, 10, 261. [Google Scholar] [CrossRef]
- Castanares-Zapatero, D.; Chalon, P.; Kohn, L.; Dauvrin, M.; Detollenaere, J.; Maertens de Noordhout, C.; Primus-de Jong, C.; Cleemput, I.; Van den Heede, K. Pathophysiology and Mechanism of Long COVID: A Comprehensive Review. Ann. Med. 2022, 54, 1473–1487. [Google Scholar] [CrossRef]
- Lindqvist, D.; Janelidze, S.; Hagell, P.; Erhardt, S.; Samuelsson, M.; Minthon, L.; Hansson, O.; Björkqvist, M.; Träskman-Bendz, L.; Brundin, L. Interleukin-6 Is Elevated in the Cerebrospinal Fluid of Suicide Attempters and Related to Symptom Severity. Biol. Psychiatry 2009, 66, 287–292. [Google Scholar] [CrossRef]
- Kern, S.; Skoog, I.; Börjesson-Hanson, A.; Blennow, K.; Zetterberg, H.; Ostling, S.; Kern, J.; Gudmundsson, P.; Marlow, T.; Rosengren, L.; et al. Higher CSF Interleukin-6 and CSF Interleukin-8 in Current Depression in Older Women. Results from a Population-Based Sample. Brain Behav. Immun. 2014, 41, 55–58. [Google Scholar] [CrossRef]
- Uzunova, G.; Pallanti, S.; Hollander, E. Presentation and Management of Anxiety in Individuals with Acute Symptomatic or Asymptomatic COVID-19 Infection, and in the Post-COVID-19 Recovery Phase. Int. J. Psychiatry Clin. Pract. 2021, 25, 115–131. [Google Scholar] [CrossRef]
- Delorme, C.; Paccoud, O.; Kas, A.; Hesters, A.; Bombois, S.; Shambrook, P.; Boullet, A.; Doukhi, D.; Le Guennec, L.; Godefroy, N.; et al. COVID-19-Related Encephalopathy: A Case Series with Brain FDG-Positron-Emission Tomography/Computed Tomography Findings. Eur. J. Neurol. 2020, 27, 2651–2657. [Google Scholar] [CrossRef]
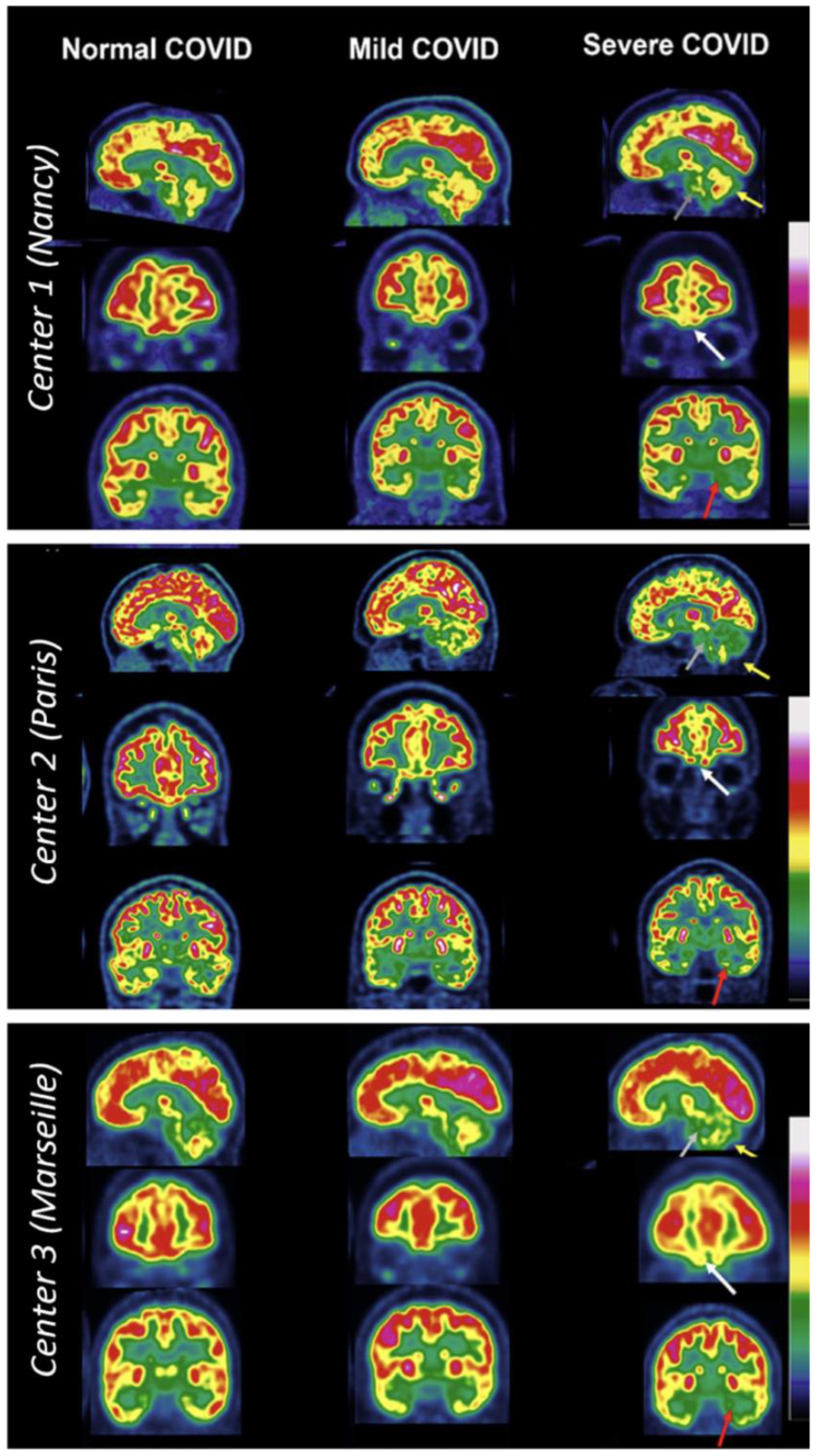
- Verger, A.; Kas, A.; Dudouet, P.; Goehringer, F.; Salmon-Ceron, D.; Guedj, E. Visual Interpretation of Brain Hypometabolism Related to Neurological Long COVID: A French Multicentric Experience. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 3197–3202. [Google Scholar] [CrossRef]
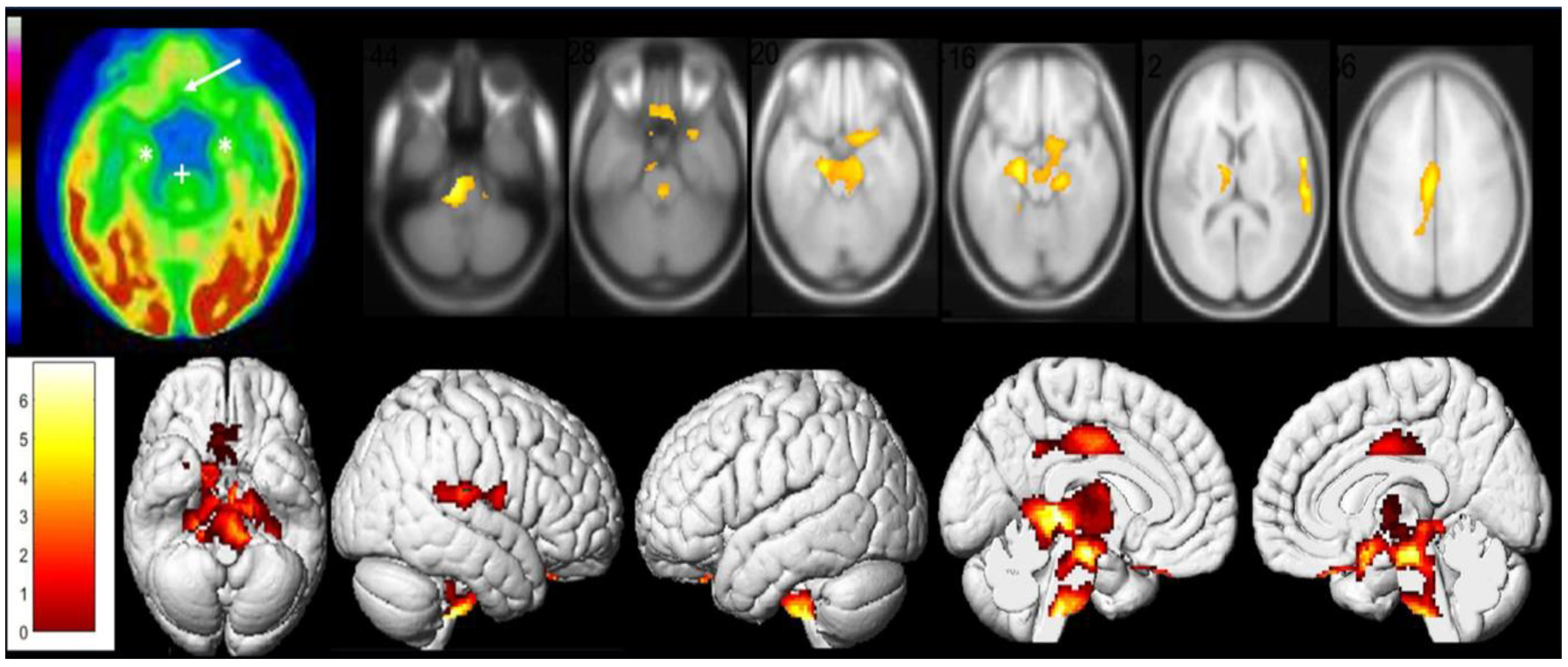
- Guedj, E.; Campion, J.Y.; Dudouet, P.; Kaphan, E.; Bregeon, F.; Tissot-Dupont, H.; Guis, S.; Barthelemy, F.; Habert, P.; Ceccaldi, M.; et al. 18F-FDG Brain PET Hypometabolism in Patients with Long COVID. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 2823–2833. [Google Scholar] [CrossRef]
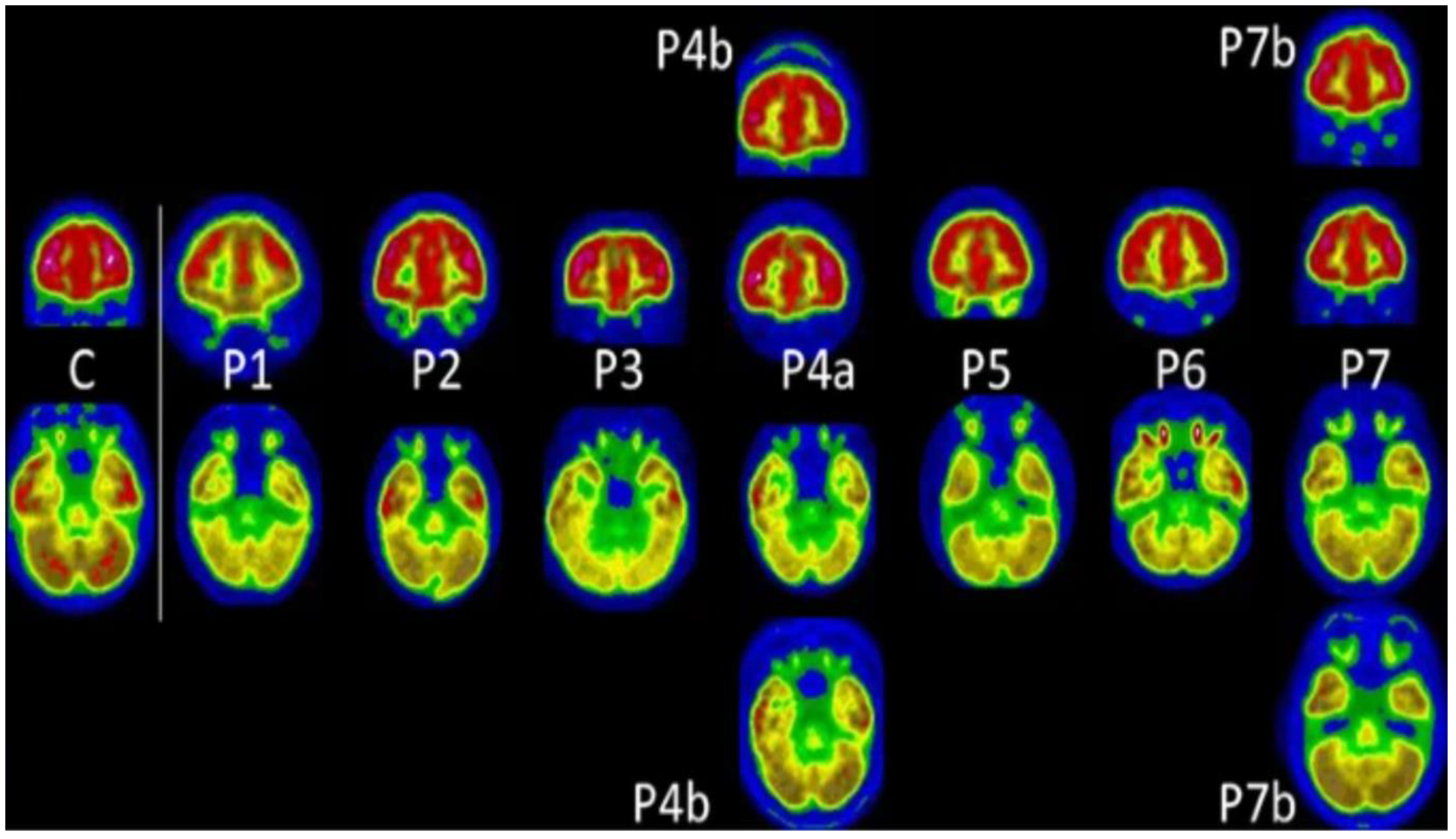
- Guedj, E.; Million, M.; Dudouet, P.; Tissot-Dupont, H.; Bregeon, F.; Cammilleri, S.; Raoult, D. 18F-FDG Brain PET Hypometabolism in Post-SARS-CoV-2 Infection: Substrate for Persistent/Delayed Disorders? Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 592–595. [Google Scholar] [CrossRef] [PubMed]
- Sollini, M.; Morbelli, S.; Ciccarelli, M.; Cecconi, M.; Aghemo, A.; Morelli, P.; Chiola, S.; Gelardi, F.; Chiti, A. Long COVID Hallmarks on [18F]FDG-PET/CT: A Case-Control Study. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 3187–3197. [Google Scholar] [CrossRef]
- Donegani, M.I.; Miceli, A.; Pardini, M.; Bauckneht, M.; Chiola, S.; Pennone, M.; Marini, C.; Massa, F.; Raffa, S.; Ferrarazzo, G.; et al. Brain Metabolic Correlates of Persistent Olfactory Dysfunction after SARS-Cov2 Infection. Biomedicines 2021, 9, 287. [Google Scholar] [CrossRef] [PubMed]
- Morand, A.; Campion, J.-Y.; Lepine, A.; Bosdure, E.; Luciani, L.; Cammilleri, S.; Chabrol, B.; Guedj, E. Similar Patterns of [18F]-FDG Brain PET Hypometabolism in Paediatric and Adult Patients with Long COVID: A Paediatric Case Series. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 913–920. [Google Scholar] [CrossRef] [PubMed]
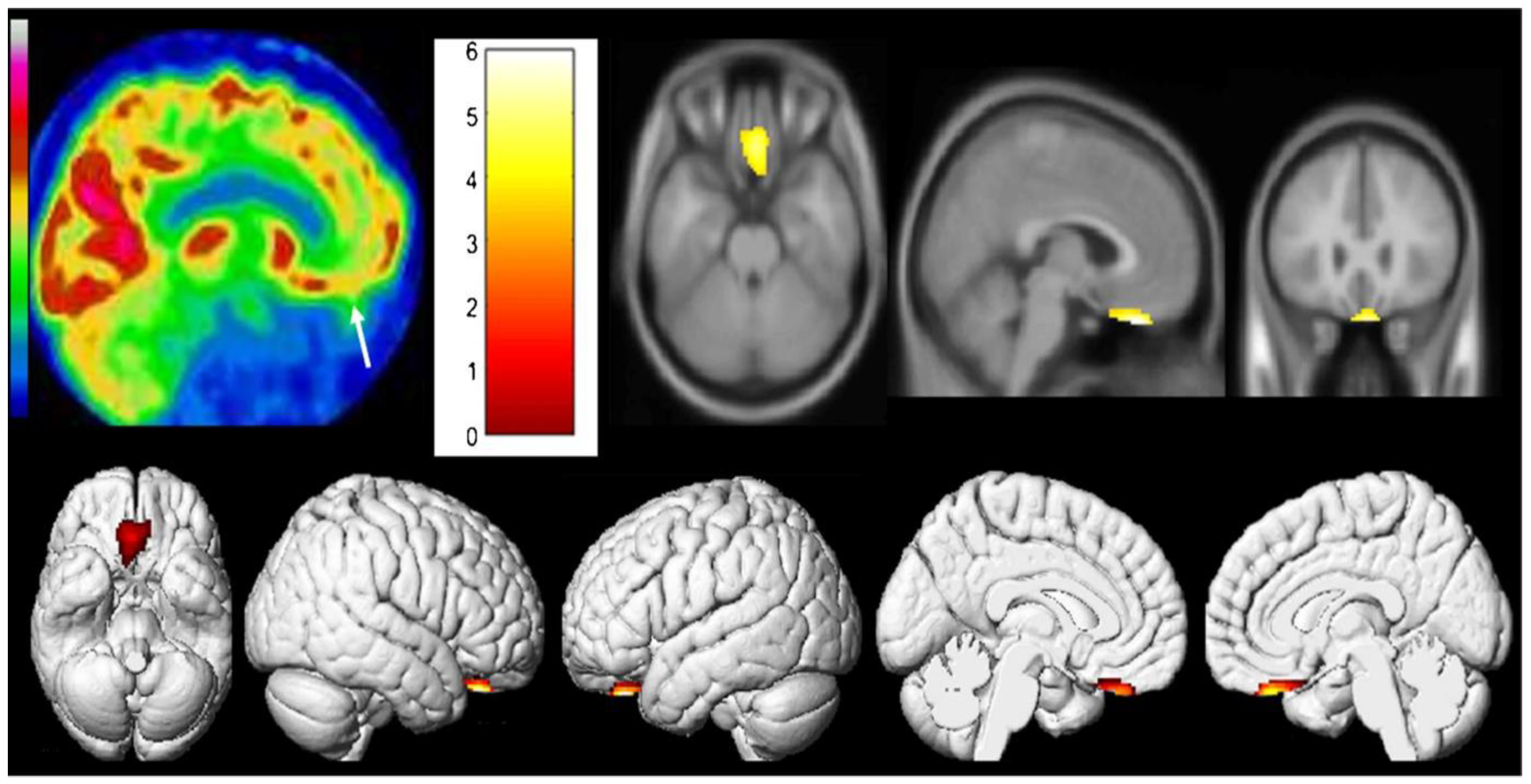
- Cocciolillo, F.; Di Giuda, D.; Morello, R.; De Rose, C.; Valentini, P.; Buonsenso, D. Orbito-Frontal Cortex Hypometabolism in Children with Post-COVID Condition (Long COVID): A Preliminary Experience. Pediatr. Infect. Dis. J. 2022, 41, 663–665. [Google Scholar] [CrossRef]
- Kiatkittikul, P.; Promteangtrong, C.; Kunawudhi, A.; Siripongsatian, D.; Siripongboonsitti, T.; Ruckpanich, P.; Thongdonpua, S.; Jantarato, A.; Piboonvorawong, C.; Fonghoi, N.; et al. Abnormality Pattern of F-18 FDG PET Whole Body with Functional MRI Brain in Post-Acute COVID-19. Nucl. Med. Mol. Imaging 2022, 56, 29–41. [Google Scholar] [CrossRef]
- Hugon, J.; Queneau, M.; Sanchez Ortiz, M.; Msika, E.F.; Farid, K.; Paquet, C. Cognitive Decline and Brainstem Hypometabolism in Long COVID: A Case Series. Brain Behav. 2022, 12, e2513. [Google Scholar] [CrossRef]
- Goehringer, F.; Bruyere, A.; Doyen, M.; Bevilacqua, S.; Charmillon, A.; Heyer, S.; Verger, A. Brain 18F-FDG PET Imaging in Outpatients with Post-COVID-19 Conditions: Findings and Associations with Clinical Characteristics. Eur. J. Nucl. Med. Mol. Imaging 2023, 50, 1084–1089. [Google Scholar] [CrossRef] [PubMed]
- Yu, A.T.; Absar, N.M. Long-Term Neuropsychiatric Complications and 18F-FDG-PET Hypometabolism in the Brain from Prolonged Infection of COVID-19. Alzheimer Dis. Assoc. Disord. 2022, 36, 173–175. [Google Scholar] [CrossRef] [PubMed]
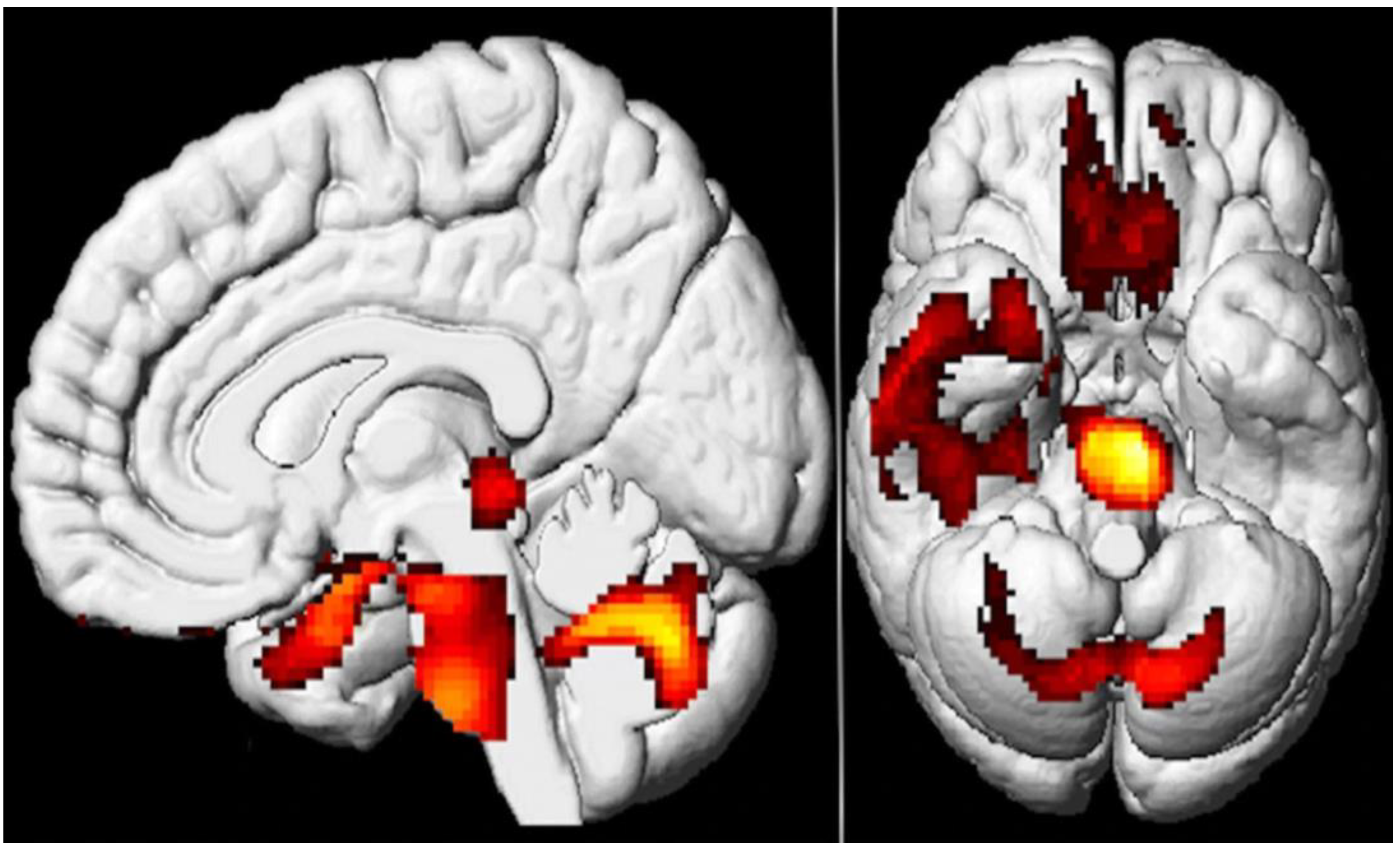
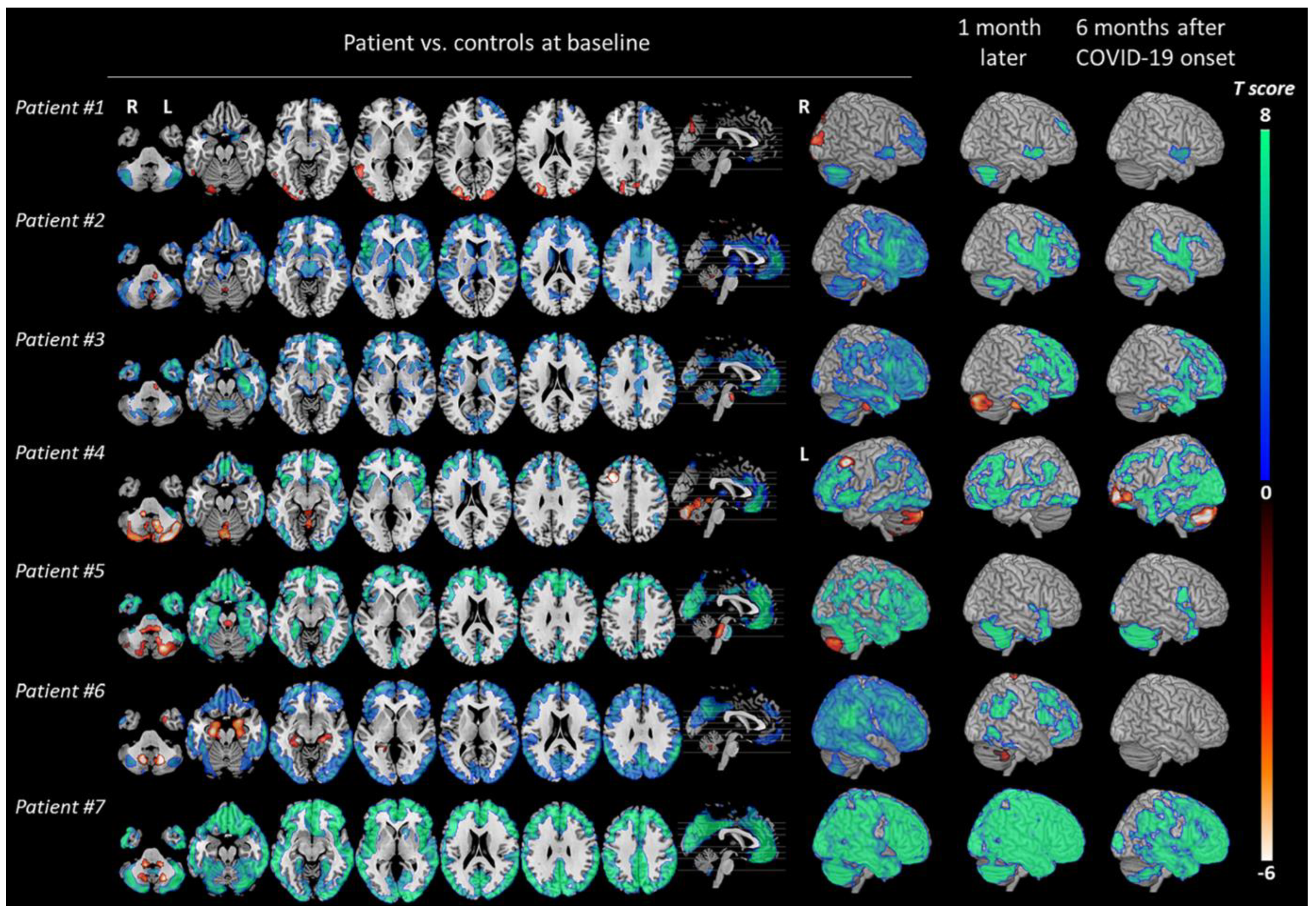
- Kas, A.; Soret, M.; Pyatigoskaya, N.; Habert, M.-O.; Hesters, A.; Le Guennec, L.; Paccoud, O.; Bombois, S.; Delorme, C. The Cerebral Network of COVID-19-Related Encephalopathy: A Longitudinal Voxel-Based 18F-FDG-PET Study. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 2543–2557. [Google Scholar] [CrossRef] [PubMed]
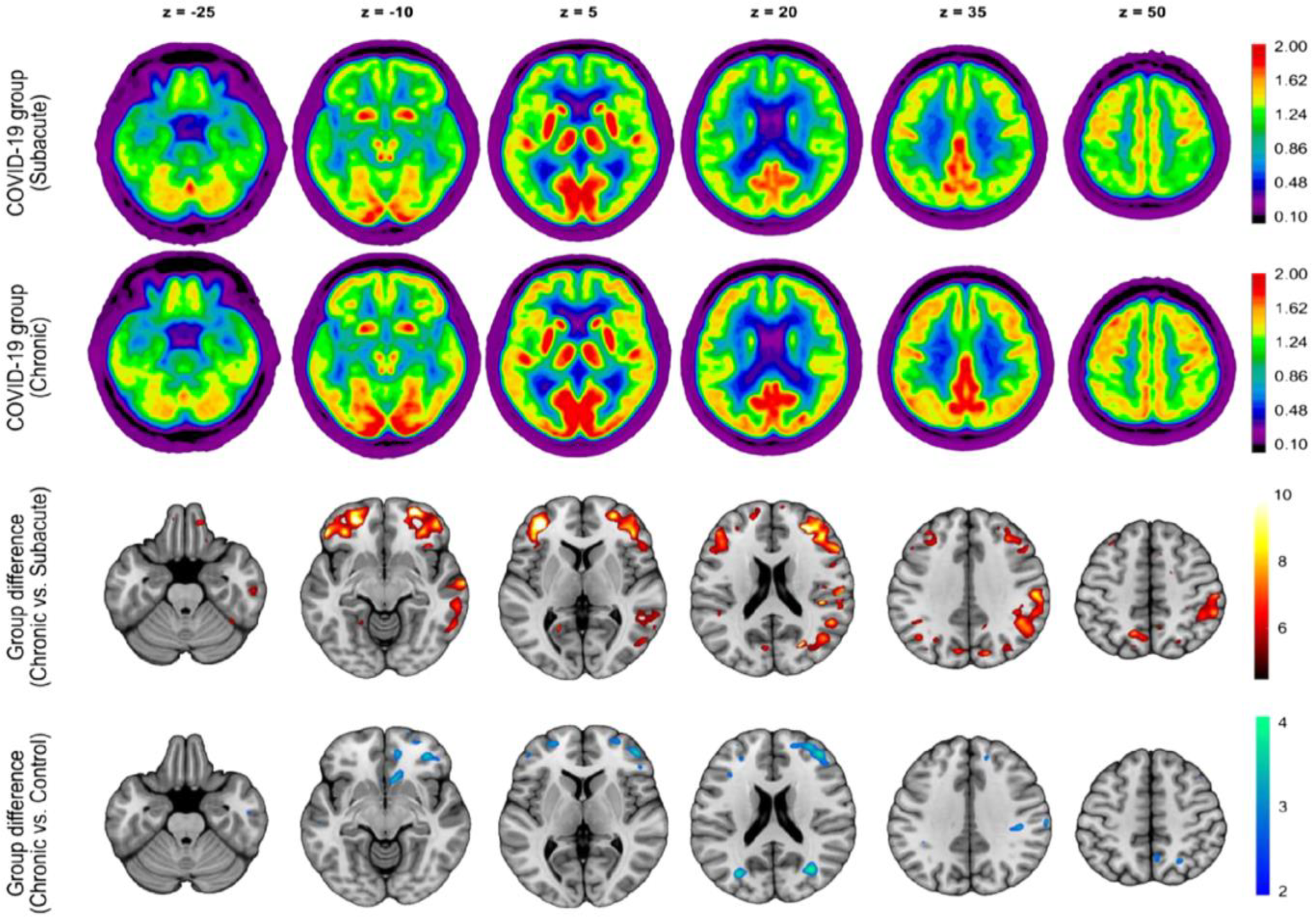
- Blazhenets, G.; Schröter, N.; Bormann, T.; Thurow, J.; Wagner, D.; Frings, L.; Weiller, C.; Meyer, P.T.; Dressing, A.; Hosp, J.A. Slow but Evident Recovery from Neocortical Dysfunction and Cognitive Impairment in a Series of Chronic COVID-19 Patients. J. Nucl. Med. 2021, 62, 910–915. [Google Scholar] [CrossRef] [PubMed]
- Dressing, A.; Bormann, T.; Blazhenets, G.; Schroeter, N.; Walter, L.I.; Thurow, J.; August, D.; Hilger, H.; Stete, K.; Gerstacker, K.; et al. Neuropsychologic Profiles and Cerebral Glucose Metabolism in Neurocognitive Long COVID Syndrome. J. Nucl. Med. 2022, 63, 1058–1063. [Google Scholar] [CrossRef]
| Variant | Year and Country of Origin Reported |
|---|---|
| Alpha (B.1.1.7) | December 2020 (UK) |
| Beta (B.1.351) | December 2020 (South Africa) |
| Gamma (P.1) | January 2021 (Brazil) |
| Delta (B.1.617.2) | December 2020 (India) |
| Omicron (B1.1.529) | November 2021 (South Africa) |
| Study | PET Findings ([18F]FDG PET Hypometabolism): Main Structures Affected | Correlated Neuropsychiatric Clinical Findings | Days Post-COVID | Study Method/Sample Size |
|---|---|---|---|---|
| Verger et al. [43] | Fronto-orbital and olfactory regions, limbic and paralimbic regions (amygdalae, hippocampal, and parahippocampal regions), brainstem, and cerebellum | Cognitive impairment, dysexecutive symptoms, memory difficulties, dizziness, limb paraesthesia, and memory/concentration impairment | 10.9 months (approximately) | Retrospective, multicenter descriptive study/143 subjects (98 females and 45 males) |
| Guedj et al. [45] | Olfactory/rectal gyrus (bilateral), medial temporal lobe, brainstem, right pre-/post-central gyrus, the right superior temporal gyrus, bilateral thalamus, hypothalamus, and cerebellum | (Case 1) memory impairment. (Case 2) sensitive lower leg crushing sensation alternating in right/left toes | Not specified | Case reports/2 subjects (both were males and had history of hospitalization) |
| Sollini et al. [46] | Parahippocampal gyri (Brodmann areas 27 and 36) and orbitofrontal cortex (gyrus rectus, BA 11) on both hemispheres, right parahippocampal gyrus (Brodmann area 30), the brainstem (substantia nigra), and the thalamus of both hemispheres | Anosmia/ageusia and persistent fatigue | 132 ± 31 days after diagnosis | Prospective observational case–control/13 subjects (8 males and 5 females) |
| Blazhenets et al. [55] | Frontoparietal and temporal regions | Mild cognitive impairment (assessed using MoCA) | 6 months (approximately) | Prospective cohort/8 subjects (6 males and 2 females) |
| Kiatkittikul et al. [50] | Parietal lobe, temporal lobe, frontal lobe, occipital lobe, and thalamus | Fatigue/myalgia, negative mood, depression, anxiety, mild cognitive impairment, and loss of taste and smell | >28 days | Retrospective descriptive/13 subjects (6 males and 7 females: 2 had severe COVID-19, presumably hospitalized) |
| Dressing et al. [56] | None | Impaired attention, memory, and multitasking abilities, word-finding difficulties, and fatigue | 197.9 ± 61.1 days | Prospective cohort/31 subjects (11 males and 20 females) |
| Hugon et al. [51] | Brainstem, particularly the pons (all cases). The left parietal, precuneus and medial temporal lobe (case 2). Anterior and posterior cingulate cortex, and the medial part of the orbitofrontal cortex (case 3) | Brain fog with memory impairments and abnormal executive functioning (all cases), language deficits (case 2), instability with gait (case 3) | Specific not given | Case series/3 subjects (2 males and 1 female; 1 of them had history of hospitalization) |
| Yu et al. [53] | Left temporal lobe, in particular, superior temporal gyrus, and mild hypometabolism in the adjacent left frontal and parietal regions with mildly asymmetric decreased tracer activity in the left basal ganglia and thalamus (case 1) and parietal and mesial temporal lobe (case 2) | Difficulty in word retrieval, word finding, memory impairments, “brain fog”, poor attention, and impaired executive functioning | 5 months and 10 months | Case report/2 subjects (both females; only one of them had history of hospitalization) |
| Donegani et al. [47] | Relative hypometabolism was demonstrated in bilateral parahippocampal and fusiform gyri and in left insula | Hyposmia | 4 and 12 weeks | Prospective cohort/14 subjects (7 males and 7 females) |
| Morand et al. [48] | Bilateral medial temporal lobes, brainstem and cerebellum, and also the right olfactory gyrus | Fatigue and cognitive impairment such as memory and concentration difficulties | Approximately 5 months | Retrospective/7 pediatric subjects (1 male and 6 females) |
| Cocciolillo et al. [49] | Left orbitofrontal region | Chronic olfactory dysfunction (1 of 3 cases), short-term memory problems, difficulty in concentrating and headaches (2 of 3 cases) | Approximately 3 months | Observational–case series/3 subjects (1 male and 2 females; all 3 non-hospitalized) |
| Guedj et al. [44] | Bilateral rectal/orbital gyrus, including the olfactory gyrus; the right temporal lobe, including the amygdala and the hippocampus, extending to the right thalamus; the bilateral pons/medulla brainstem; the bilateral cerebellum | Shortness of breath, chest pain, muscular pain, memory cognitive complaints, insomnia, hyposmia/anosmia, dysgeusia/ageusia | Approximately 97 days | Retrospective/35 subjects (15 males and 20 females; 12 had history of hospitalization in the ICU) |
| Kas et al. [54] | Prefrontal, insular and subcortical | Cognitive and emotional disorders of varying severity remained with attention/executive disabilities and anxio-depressive symptoms | Approximately 6 months | Observational- prospective/7 subjects (4 males and 3 females; 2 had history of hospitalization) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hameed, R.; Bahadur, A.R.; Singh, S.B.; Sher, J.; Todua, M.; Moradi, L.; Bastakoti, S.; Arslan, M.; Ajmal, H.; Lee, G.Y.; et al. Neurological and Psychiatric Manifestations of Long COVID-19 and Their [18F]FDG PET Findings: A Review. Diagnostics 2023, 13, 2353. https://doi.org/10.3390/diagnostics13142353
Hameed R, Bahadur AR, Singh SB, Sher J, Todua M, Moradi L, Bastakoti S, Arslan M, Ajmal H, Lee GY, et al. Neurological and Psychiatric Manifestations of Long COVID-19 and Their [18F]FDG PET Findings: A Review. Diagnostics. 2023; 13(14):2353. https://doi.org/10.3390/diagnostics13142353
Chicago/Turabian StyleHameed, Rizwanullah, Anuradha Rosario Bahadur, Shashi Bhushan Singh, Juwairah Sher, Maia Todua, Leah (Mahsa) Moradi, Sanjiv Bastakoti, Maeen Arslan, Hanfa Ajmal, Gha Young Lee, and et al. 2023. "Neurological and Psychiatric Manifestations of Long COVID-19 and Their [18F]FDG PET Findings: A Review" Diagnostics 13, no. 14: 2353. https://doi.org/10.3390/diagnostics13142353
APA StyleHameed, R., Bahadur, A. R., Singh, S. B., Sher, J., Todua, M., Moradi, L., Bastakoti, S., Arslan, M., Ajmal, H., Lee, G. Y., Ayubcha, C., Werner, T. J., Alavi, A., & Revheim, M.-E. (2023). Neurological and Psychiatric Manifestations of Long COVID-19 and Their [18F]FDG PET Findings: A Review. Diagnostics, 13(14), 2353. https://doi.org/10.3390/diagnostics13142353








