Diagnostic Evaluation of Hypersensitivity Reactions to Antibiotics in a Large Cohort of Mastocytosis Patients
Abstract
:1. Introduction
2. Methods
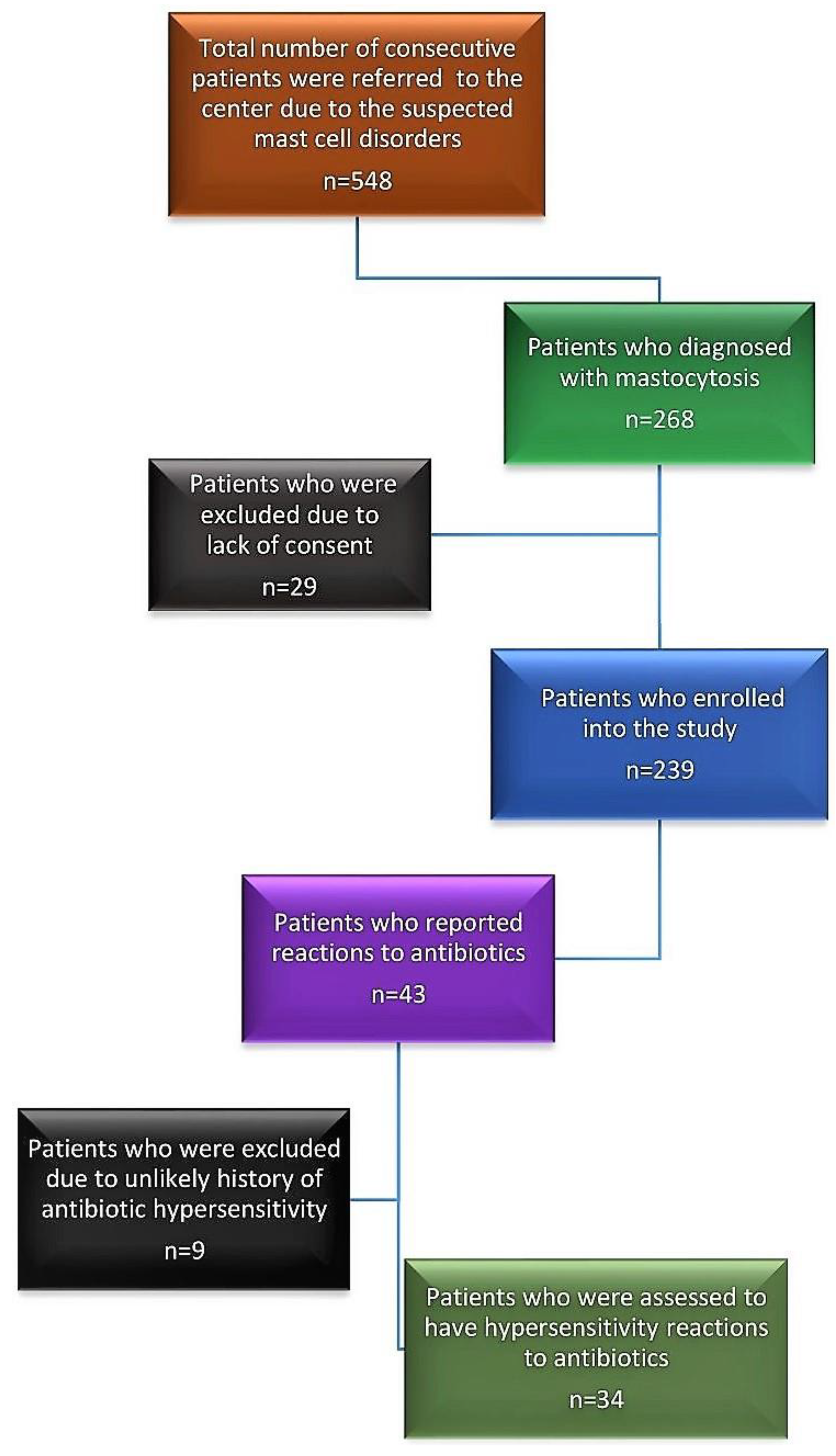
2.1. Study Population, Study Subjects and Study Design
2.2. Diagnosis of Antibiotic Hypersensitivity
2.3. Drug Provocation Test
2.4. Statistics
3. Results
3.1. Patient Characteristics
3.2. Prevalence of Hypersensitivity to Antibiotics
3.3. Clinical Features of the Reactions
3.4. Culprit Antibiotics
3.5. Risk Factors of Antibiotic Hypersensitivity
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shehab, N.; Patel, P.R.; Srinivasan, A.; Budnitz, D.S. Emergency department visits for antibiotic-associated adverse events. Clin. Infect. Dis. 2008, 15, 735–743. [Google Scholar] [CrossRef] [Green Version]
- Brockow, K. Triage strategies for clarifying reported betalactam allergy. J. Allergy Clin. Immunol. Pract. 2019, 7, 1066–1067. [Google Scholar] [CrossRef] [PubMed]
- Macy, E.; Poon, K.-Y.T. Self-reported antibiotic allergy incidence and prevalence: Age and sex effects. Am. J. Med. 2009, 122, e1–e7. [Google Scholar] [CrossRef] [PubMed]
- Gülen, T.; Hagglund, H.; Dahlen, B.; Nilsson, G. Mastocytosis: The puzzling clinical spectrum and challenging diagnostic aspects of an enigmatic disease. J. Intern. Med. 2016, 279, 211–228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valent, P.; Akin, C.; Hartmann, K.; Alvarez-Twose, I.; Brockow, K.; Hermine, O.; Niedoszytko, M.; Schwaab, J.; Lyons, J.J.; Carter, M.C.; et al. Updated Diagnostic Criteria and Classification of Mast Cell Disorders: A Consensus Proposal. Hemasphere 2021, 13, e646. [Google Scholar] [CrossRef]
- Gülen, T.; Akin, C. Anaphylaxis and Mast Cell Disorders. Immunol. Allergy Clin. N. Am. 2022, 42, 45–63. [Google Scholar] [CrossRef]
- Gülen, T.; Hagglund, H.; Dahlen, S.E.; Sander, B.; Dahlen, B.; Nilsson, G. Flushing, fatigue, and recurrent anaphylaxis: A delayed diagnosis of mastocytosis. Lancet 2014, 383, 1608. [Google Scholar] [CrossRef]
- Gülen, T.; Hagglund, H.; Dahlen, B.; Nilsson, G. High prevalence of anaphylaxis in patients with systemic mastocytosis—A single-centre experience. Clin. Exp. Allergy 2014, 44, 121–129. [Google Scholar] [CrossRef]
- Gülen, T.; Ljung, C.; Nilsson, G.; Akin, C. Risk factor analysis of anaphylactic reactions in patients with systemic mastocytosis. J. Allergy Clin. Immunol. Pract. 2017, 5, 1248–1255. [Google Scholar] [CrossRef]
- Bonadonna, P.; Perbellini, O.; Passalacqua, G.; Caruso, B.; Colarossi, S.; Dal Fior, D.; Castellani, L.; Bonetto, C.; Frattini, F.; Dama, A.; et al. Clonal mast cell disorders in patients with systemic reactions to hymenoptera stings and increased serum tryptase levels. J. Allergy Clin. Immunol. 2009, 123, 680–686. [Google Scholar] [CrossRef]
- Jarkvist, J.; Brockow, K.; Gülen, T. Low Frequency of IgE-Mediated Food Hypersensitivity in Mastocytosis. J. Allergy Clin. Immunol. Pract. 2020, 8, 3093–3101. [Google Scholar] [CrossRef]
- Gülen, T.; Hägglund, H.; Sander, B.; Dahlen, B.; Nilsson, G. The presence of mast cell clonality in patients with unexplained anaphylaxis. Clin. Exp. Allergy 2014, 44, 1179–1187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bonadonna, P.; Pagani, M.; Aberer, W.; Bilò, M.B.; Brockow, K.; Oude Elberink, H.; Garvey, L.; Mosbech, H.; Romano, A.; Zanotti, R.; et al. Drug hypersensitivity in clonal mast cell disorders: ENDA/EAACI position paper. Allergy 2015, 70, 755–763. [Google Scholar] [CrossRef] [PubMed]
- Matito, A.; Morgado, J.M.; Sánchez-López, P.; Álvarez-Twose, I.; Sánchez-Muñoz, L.; Orfao, A.; Escribano, L. Management of anesthesia in adult and pediatric mastocytosis: A study of the Spanish Network on Mastocytosis (REMA) based on 726 anesthetic procedures. Int. Arch. Allergy Immunol. 2015, 167, 47–56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carter, M.C.; Metcalfe, D.D.; Matito, A.; Escribano, L.; Butterfield, J.H.; Schwartz, L.B.; Bonadonna, P.; Zanotti, R.; Triggiani, M.; Castells, M.; et al. Adverse reactions to drugs and biologics in patients with clonal mast cell disorders: A Work Group Report of the Mast Cells Disorder Committee, American Academy of Allergy, Asthma & Immunology. J. Allergy Clin. Immunol. 2019, 143, 880–893. [Google Scholar]
- González de Olano, D.; de la Hoz Caballer, B.; Núñez López, R.; Sánchez Muñoz, L.; Cuevas Agustín, M.; Diéguez, M.C.; Alvarez Twose, I.; Castells, M.C.; Escribano Mora, L. Prevalence of allergy and anaphylactic symptoms in 210 adult and pediatric patients with mastocytosis in Spain: A study of the Spanish network on mastocytosis (REMA). Clin. Exp. Allergy 2007, 37, 1547–1555. [Google Scholar] [CrossRef]
- Brockow, K.; Jofer, C.; Behrendt, H.; Ring, J. Anaphylaxis in patients with mastocytosis: A study on history, clinical features and risk factors in 120 patients. Allergy 2008, 63, 226–232. [Google Scholar] [CrossRef]
- Bilò, M.B.; Frontini, F.; Massaccesi, C.; Cinti, B.; Antonicelli, L. Mast cell diseases and the severity and course of intraoperative anaphylaxis. Ann. Allergy Asthma Immunol. 2009, 103, 175–176. [Google Scholar] [CrossRef]
- Shaker, M.S.; Wallace, D.V.; Golden, D.B.K.; Oppenheimer, J.; Bernstein, J.A.; Campbell, R.L.; Dinakar, C.; Ellis, A.; Greenhawt, M.; Khan, D.A.; et al. Anaphylaxis—A 2020 practice parameter update, systematic review, and Grading of Recommendations, Assessment, Development and Evaluation (GRADE) analysis. J. Allergy Clin. Immunol. 2020, 145, 1082–1123. [Google Scholar] [CrossRef] [Green Version]
- Muraro, A.; Worm, M.; Alviani, C.; Cardona, V.; DunnGalvin, A.; Garvey, L.H.; Riggioni, C.; de Silva, D.; Angier, E.; Arasi, S.; et al. EAACI guideline: Anaphylaxis (2021 update). Allergy 2022, 77, 357–377. [Google Scholar] [CrossRef]
- Albin, S.; Agarwal, S. Prevalence and characteristics of reported penicillin allergy in an urban outpatient adult population. Allergy Asthma Proc. 2014, 35, 489–494. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Dhopeshwarkar, N.; Blumenthal, K.G.; Goss, F.; Topaz, M.; Slight, S.P.; Bates, D.W. Drug allergies documented in electronic health records of a large healthcare system. Allergy 2016, 71, 1305–1313. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kowalik, A.; de Monestrol, I.; Sorjonen, K.; Brockow, K.; Gülen, T. Antibiotic hypersensitivity in cystic fibrosis—Low frequency of anaphylaxis over 16000 courses. Br. J. Clin. Pharmacol. 2022, 88, 4845–4853. [Google Scholar] [CrossRef] [PubMed]
- Dhopeshwarkar, N.; Sheikh, A.; Doan, R.; Topaz, M.; Bates, D.W.; Blumenthal, K.G.; Zhou, L. Drug-Induced Anaphylaxis Documented in Electronic Health Records. J. Allergy Clin. Immunol. Pract. 2019, 7, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Bonadonna, P.; Olivieri, F.; Jarkvist, J.; Nalin, F.; Zanotti, R.; Maclachlan, L.; Gülen, T. Non-steroidal anti-inflammatory drug-induced anaphylaxis infrequent in 388 patients with mastocytosis: A two-center retrospective cohort study. Front. Allergy 2022, 5, 1071807. [Google Scholar] [CrossRef]
- Rama, T.A.; Morgado, J.M.; Henriques, A.; Escribano, L.; Alvarez-Twose, I.; Sanchez-Muñoz, L.; Moreira, A.; Romão, J.; Órfão, A.; Matito, A. Mastocytosis presenting with mast cell-mediator release-associated symptoms elicited by cyclooxygenase inhibitors: Prevalence, clinical, and laboratory features. Clin. Transl. Allergy 2022, 12, e12132. [Google Scholar] [CrossRef]
- Macy, E.; Ho, N.J. Multiple drug intolerance syndrome: Prevalence, clinical characteristics, and management. Ann. Allergy Asthma Immunol. 2012, 108, 88–93. [Google Scholar] [CrossRef]
- Gomes, E.; Cardoso, M.F.; Praca, F.; Gomes, L.; Marino, E.; Demoly, P. Self-reported drug allergy in a general adult Portuguese population. Clin. Exp. Allergy 2004, 34, 1597–1601. [Google Scholar] [CrossRef] [Green Version]
- Romano, A.; Atanaskovic-Markovic, M.; Barbaud, A.; Bircher, A.J.; Brockow, K.; Caubet, J.C.; Celik, G.; Cernadas, J.; Chiriac, A.M.; Demoly, P.; et al. Towards a more precise diagnosis of hypersensitivity to beta-lactams—An EAACI position paper. Allergy 2020, 75, 1300–1315. [Google Scholar] [CrossRef] [Green Version]
- Zopf, Y.; Rabe, C.; Neubert, A.; Gassmann, K.G.; Rascher, W.; Hahn, E.G.; Brune, K.; Dormann, H. Women encounter ADRs more often than do men. Eur. J. Clin. Pharmacol. 2008, 64, 999–1004. [Google Scholar] [CrossRef]
- Barranco, P.; Lopez-Serrano, M.C. General and epidemiological aspects of allergic drug reactions. Clin. Exp. Allergy 1998, 28, S61–S62. [Google Scholar]
- Cornejo-Garcia, J.A.; Gueant-Rodriguez, R.M.; Torres, M.J.; Blanca-Lopez, N.; Tramoy, D.; Romano, A.; Blanca, M.; Gueant, J.L. Biological and genetic determinants of atopy are predictors of immediate-type allergy to beta-lactams, in Spain. Allergy 2012, 67, 1181–1185. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | Total (n = 239) | SM (n = 176) | MIS (n = 18) | MMAS (n = 45) |
|---|---|---|---|---|
| Male gender, n (%) | 112 (46.9) | 81 (46) | 7 (38.9) | 24 (53.3) |
| Age at diagnosis, median (range) | 52 (18–84) | 53 (18–84) | 39 (18–76) | 51 (28–74) |
| Presence of mast cell aggregates, n (%) | 97 (46.4) 30 n/a | 97 (56.7) 5 n/a | Not conducted | 0 (0) 12 n/a |
| Presence of atypical morphology, n (%) | 169 (81.3) 31 n/a | 162 (95.3) 6 n/a | Not conducted | 7 (21.2) 12 n/a |
| Presence of CD25, n (%) | 200 (96.6) 32 n/a | 169 (100) 7 n/a | Not conducted | 29 (87.9) 12 n/a |
| Presence of D816V mutation, n (%) | 164 (74.5) 1 9 n/a | 135 (84.4) 16 n/a | 9 (60) 3 n/a | 20 (44.4) |
| Baseline tryptase (ng/mL), median (range) | 22 (2.8–650) | 30 (3.2–650) | 11.5 (2.8–160) | 10 (3.1–31) |
| Presence of atopy, n (%) | 68 (28.8) 3 n/a | 46 (26,3) 1 n/a | 5 (29.4) 1 n/a | 17 (38.6) 1 n/a |
| Presence of UP, n (%) | 125 (52.3) | 107 (60.8) | 18 (100) | 0 (0) |
| Total IgE (kU/L), median (range) | 16 (1–1600) | 14 (1–1 600) | 13 (2.3–310) | 47 (5.8–1 100) |
| Prescence of asthma/rhinitis, n (%) | 59 (24.9) 2 n/a | 40 (22.9) 1 n/a | 3 (16.7) | 16 (36.4) 1 n/a |
| History of any anaphylaxis, n (%) | 123 (51.5) | 89 (50.6) | 0 (0) | 34 (75.6) |
| Prevalence | Total Cohort (n = 239) | Mastocytosis (n = 194) | MMAS (n = 45) |
|---|---|---|---|
| Drug hypersensitivity to antibiotics, n (%) | 34 (14.2) | 29 (14.9) | 5 (11.1) |
| Antibiotic-induced anaphylaxis, n (%) | 2 (0.8) | 2 (1) | None |
| Characteristics | Mastocytosis without Antibiotics Reaction (n = 167) | Mastocytosis with Antibiotics Reaction (n = 29) | p-Value | MMAS without Antibiotics Reaction (n = 40) | MMAS with Antibiotics Reaction (n = 5) | p-Value |
|---|---|---|---|---|---|---|
| Male gender, n (%) | 78 (46.7) | 10 (34.4) | 0.12 * | 24 (60) | 0 (0) | 0.017 * |
| Age at diagnosis, median (range) | 53 (18–84) | 46 (18–81) | 0.259 † | 51 (28–74) | 54 (28–61) | 0.820 † |
| Presence of atopy, n (%) | 43 (25.8) | 9 (31) | 0.825 * | 15 (37.5) | 2 (40) | 1.00 * |
| Presence of UP, n (%) | 103 (62.2) | 21 (72) | 0.540 * | n/a | n/a | ND |
| Prescence of asthma/rhinitis, n (%) | 35 (20.9) | 9 (31) | 0.349 * | 13 (32.5) | 3 (60) | 0.336 * |
| Total IgE (kU/L), median (range) | 13 (1–1600) | 23 (1–250) | 0.048 † | 64 (5.8–1100) | 22 (6.2–180) | 0.234 † |
| Baseline tryptase (ng/mL), median (range) | 29 (2.8–650) | 28 (6.9–150) | 0.474 † | 10 (3.1–31) | 10 (3.9–15) | 0.636 † |
| History of any anaphylaxis, n (%) | 73 (43.7) | 16 (55) | 0.557 * | 32 (80) | 2 (40) | 0.085 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jarkvist, J.; Gülen, T. Diagnostic Evaluation of Hypersensitivity Reactions to Antibiotics in a Large Cohort of Mastocytosis Patients. Diagnostics 2023, 13, 2241. https://doi.org/10.3390/diagnostics13132241
Jarkvist J, Gülen T. Diagnostic Evaluation of Hypersensitivity Reactions to Antibiotics in a Large Cohort of Mastocytosis Patients. Diagnostics. 2023; 13(13):2241. https://doi.org/10.3390/diagnostics13132241
Chicago/Turabian StyleJarkvist, Jesper, and Theo Gülen. 2023. "Diagnostic Evaluation of Hypersensitivity Reactions to Antibiotics in a Large Cohort of Mastocytosis Patients" Diagnostics 13, no. 13: 2241. https://doi.org/10.3390/diagnostics13132241
APA StyleJarkvist, J., & Gülen, T. (2023). Diagnostic Evaluation of Hypersensitivity Reactions to Antibiotics in a Large Cohort of Mastocytosis Patients. Diagnostics, 13(13), 2241. https://doi.org/10.3390/diagnostics13132241






