Development and Validation of a Nomograph Model for Post-Operative Central Nervous System Infection after Craniocerebral Surgery
Abstract
:1. Introduction
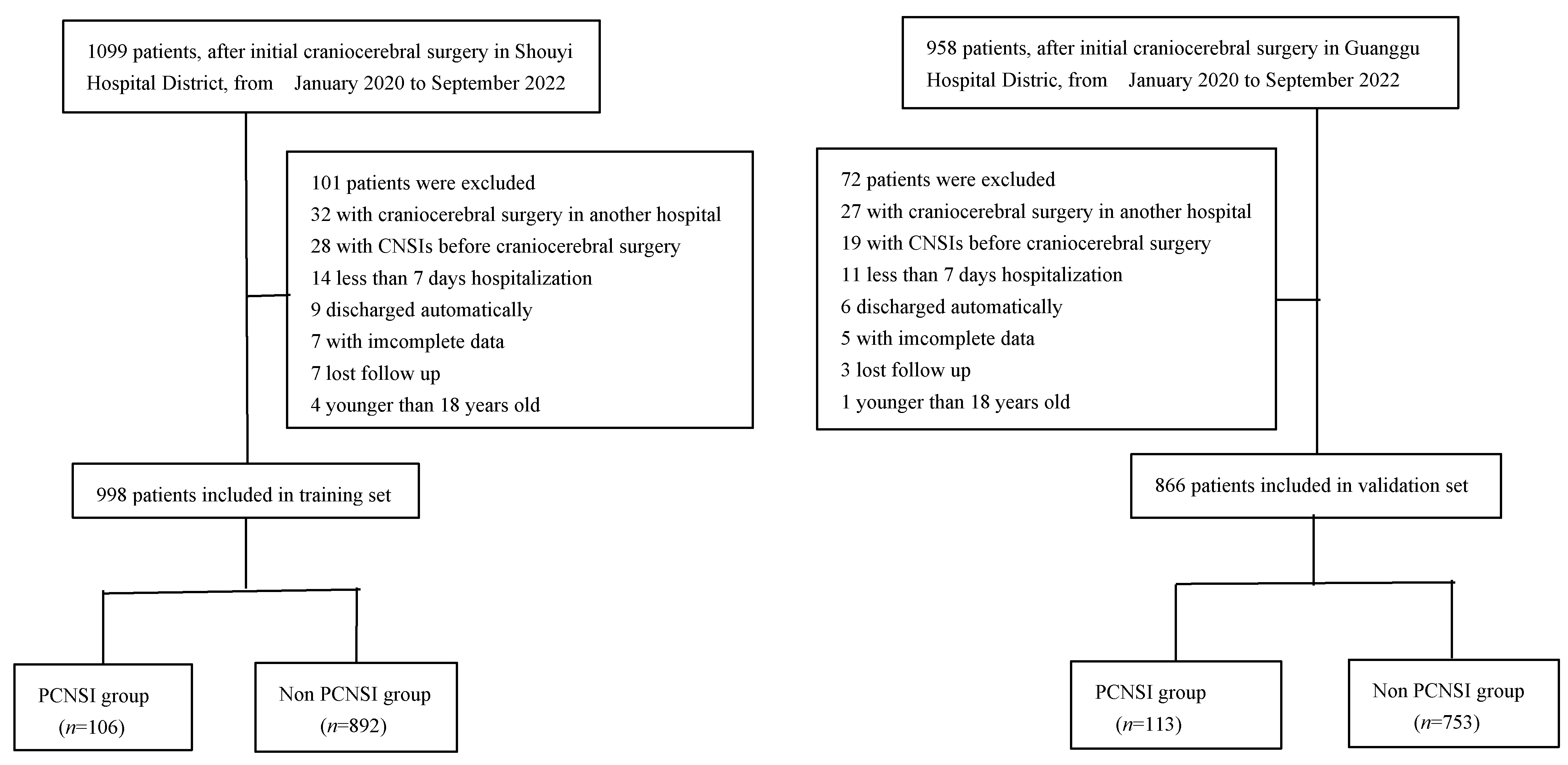
2. Materials and Methods
2.1. General Data
2.1.1. Inclusion Criteria
2.1.2. Exclusion Criteria
2.1.3. Diagnostic Criteria for PCNSI
Clinical Diagnostic Criteria
Etiological Diagnostic Criteria
2.2. Data Collection
2.3. Statistical Methods
3. Results
3.1. Analysis of Baseline Data of Patients
3.2. Lasso and Logistic Regression Analysis
3.3. Establishment of Nomogram Model
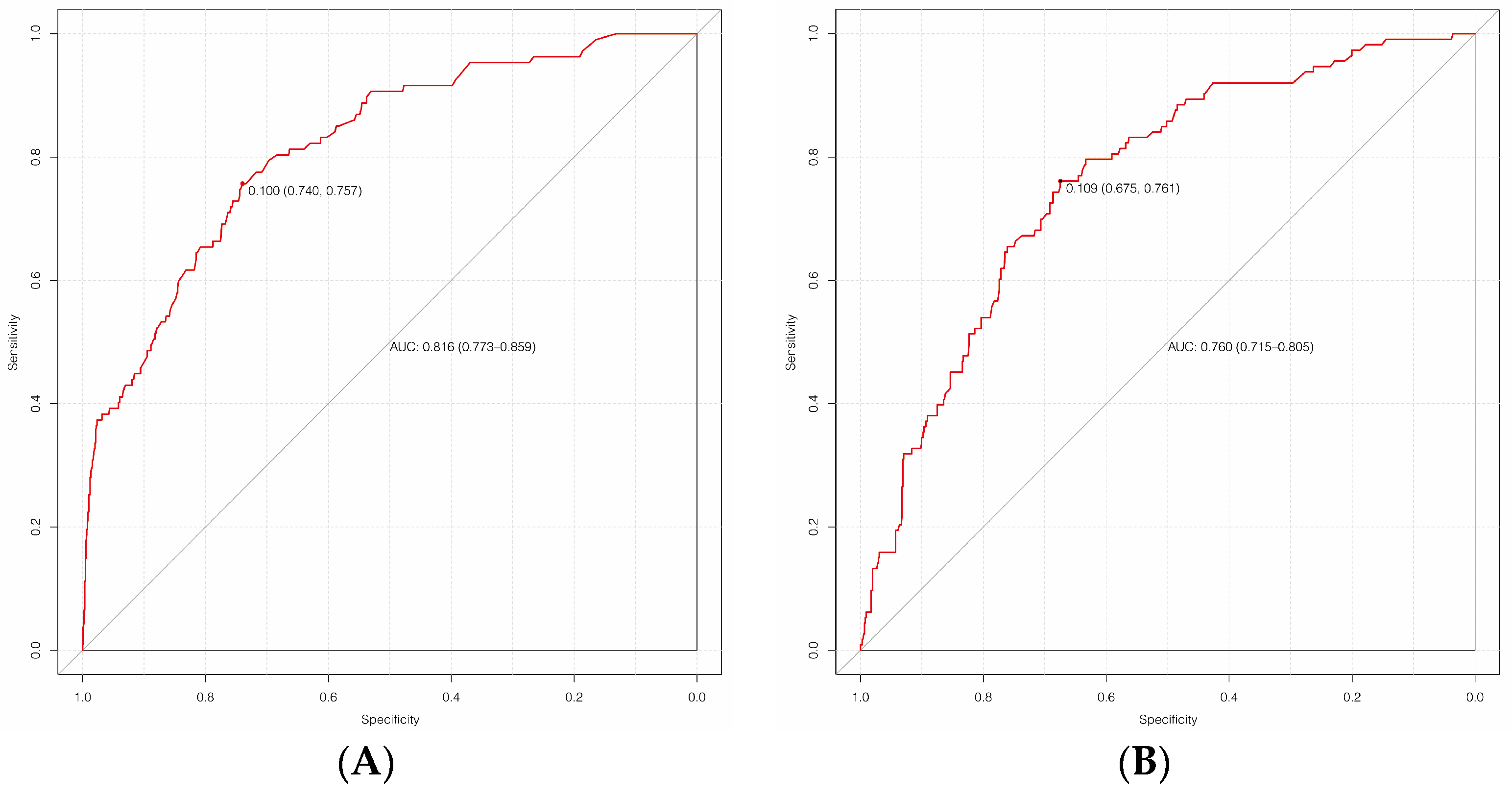
3.4. Internal Validation of the Model
3.5. External Validation of the Model
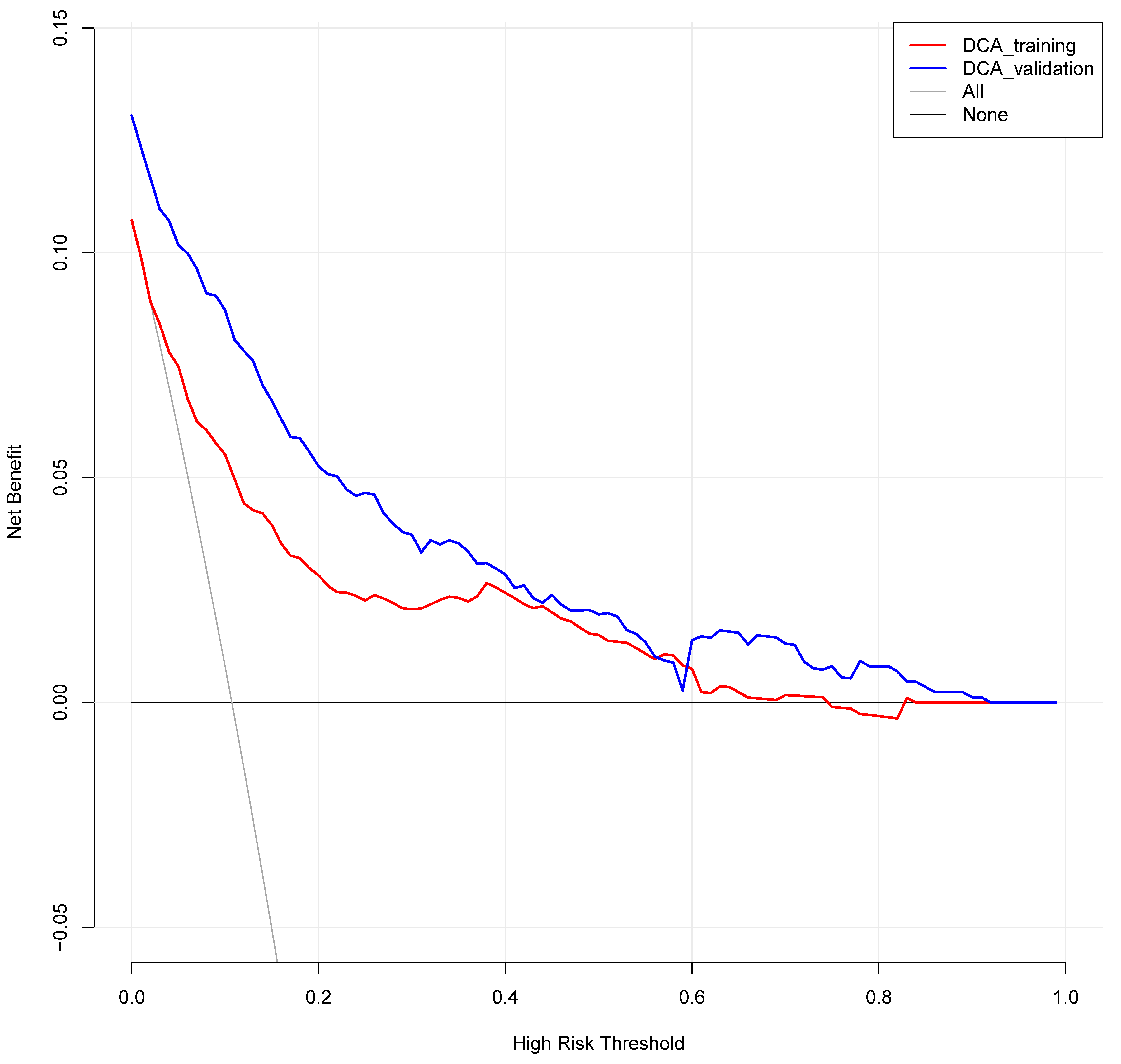
3.6. Clinical Decision Curve Analysis (Figure 6)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wang, L.; Cao, X.; Shi, L.; Ma, Z.; Wang, Y.; Liu, Y. Risk factors for intracranial infection after craniotomy: A case-control study. Brain Behav. 2020, 10, e01658. [Google Scholar] [CrossRef]
- Fang, C.; Zhu, T.; Zhang, P.; Xia, L.; Sun, C. Risk factors of neurosurgical site infection after craniotomy: A systematic review and meta-analysis. Am. J. Infect. Control 2017, 45, e123–e134. [Google Scholar] [CrossRef]
- Ortiz, O.H.H.; García, H.I.G.; Ramírez, F.M.; Flórez, J.S.C.; Gil Valencia, B.A.; Mantilla, S.E.M.; Ochoa, M.J.M.; Ochoa, J.E.S.; Jaimes, F. Development of a prediction rule for diagnosing postoperative meningitis: A cross-sectional study. J. Neurosurg. 2018, 128, 262–271. [Google Scholar] [CrossRef] [Green Version]
- Ma, Y.F.; Wen, L.; Zhu, Y. Prospective study evaluating postoperative central nervous system infections following cranial surgery. Br. J. Neurosurg. 2019, 33, 80–83. [Google Scholar] [CrossRef]
- Pan, S.; Huang, X.; Wang, Y.; Li, L.; Zhao, C.; Yao, Z.; Cui, W.; Zhang, G. Efficacy of intravenous plus intrathecal/intracerebral ventricle injection of polymyxin B for post-neurosurgical intracranial infections due to MDR/XDR Acinectobacter baumannii: A retrospective cohort study. Antimicrob. Resist. Infect. Control 2018, 7, 8. [Google Scholar] [CrossRef] [Green Version]
- Zhong, L.; Shi, X.-Z.; Su, L.; Liu, Z.-F. Sequential intraventricular injection of tigecycline and polymyxin B in the treatment of intracranial Acinetobacter baumannii infection after trauma: A case report and review of the literature. Mil. Med. Res. 2020, 7, 23. [Google Scholar] [CrossRef]
- Zheng, G.; Shi, Y.; Cao, Y.; Qian, L.; Lv, H.; Zhang, L.; Zhang, G. Clinical Feature, Therapy, Antimicrobial Resistance Gene Distribution, and Outcome of Nosocomial Meningitis Induced by Multidrug-Resistant Enterobacteriaceae—A Longitudinal Cohort Study From Two Neurosurgical Centers in Northern China. Front. Cell Infect. Microbiol. 2022, 12, 839257. [Google Scholar] [CrossRef]
- The Neurocritical Care Expert Committee of the Neurosurgeon Branch of the Chinese Medical Association; The Neurosurgery Critical Care Group of the Neurosurgery Branch of the Beijing Medical Association. Chinese expert consensus on the diagnosis and treatment of central nervous system infection in neurosurgery. Chin. J. Neurosurg. 2021, 37, 2–15. [Google Scholar] [CrossRef]
- Brouwer, M.C.; Van de Beek, D. Management of bacterial central nervous system infection. Handb. Clin. Neurol. 2017, 140, 349–364. [Google Scholar] [CrossRef]
- Neurosurgery Branch of Chinese Medical Association; China Neurosurgery Critical Care Management Cooperation Group. Expert consensus on the diagnosis and treatment of infection in severe neurosurgery patients in China. Natl. Med. J. China 2017, 97, 1607–1614. [Google Scholar]
- Wang, Y.C.; Shi, C.Q.; Li, W.Y.; Liu, S.Y.; Liu, Z.H.; Yu, X.H. Establishment of a nomogram model for risk of pulmonary infection after craniocerebral injury and preliminary assessment of its effectiveness. Chin. J. Neuromed. 2019, 18, 1209–1214. [Google Scholar] [CrossRef]
- Collins, G.S.; Reitsma, J.B.; Altman, D.G.; Moons, K.G. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): The TRIPOD statement. Ann. Intern Med. 2015, 162, 55–63. [Google Scholar] [CrossRef] [Green Version]
- Chidambaram, S.; Nair, M.N.; Krishnan, S.S.; Cai, L.; Gu, W.; Vasudevan, M.C. Postoperative central nervous system infection after neurosurgery in a Modernized, Resource-Limited Tertiary Neurosurgical Center in South Asia. World Neurosurg. 2015, 84, 1668–1673. [Google Scholar] [CrossRef]
- Chang, J.; Wu, H.; Wang, H.; Ma, B.-T.; Wang, R.-Z.; Wei, J.-J. Prevalence and antibiotic resistance of bacteria isolated from the cerebrospinal fluid of neurosurgical patients at Peking Union Medical College Hospital. Antimicrob. Resist. Infect. Control 2018, 7, 41. [Google Scholar] [CrossRef] [Green Version]
- Li, J.F.; Cui, K.; Dong, Y.L. Clinical analysis of related factors of intracranial infection in patients with acute craniocerebral injury after operation. Mod. Med. J. China 2014, 24, 87–89. [Google Scholar]
- Ma, Y.F.; Chen, L.; Hou, W.L.; Gao, L.N.; Hou, Y.H. Investigation on the related factors of intracranial infection after craniotomy. Chin. J. Nosocomiol. 2016, 26, 2485–2487. [Google Scholar]
- Shen, H.U.; Yang, J.Y.; Wei, X.Z.; Fu, W.X.; Yue, Y.D. Analysis of risk factors of affecting intracranial infection complicating brain injury operation. Chin. J. Neuromed. 2006, 5, 498–502. [Google Scholar]
- Ren, X.H.; Zhang, Y.; Gao, Z.X.; Ji, L.; Zhang, J.T.; Zhang, L.W. Influencing factors of intracranial infection and risk prediction analysis after neurosurgical operation. Chin. J. Neurosurg. 2015, 31, 992–996. [Google Scholar]
- Yang, X.F.; Wang, H. Emphasizing prevention and treatment of intracranial bacterial infection in patients with critical neurological diseases. Chin. J. Trauma 2019, 35, 6–9. [Google Scholar] [CrossRef]
- Xu, L.; Chen, R. Risk factors and protective strategies of postoperative intracranial infection in aged patients with severe craniocerebral injury. IMHGN 2020, 26, 3415–3417. [Google Scholar] [CrossRef]
- Huang, X.; Zhang, X.; Zhou, J.; Li, G.; Zheng, G.; Peng, L.; Yan, Z.; Chen, S. Analysis of risk factors and preventive strategies for intracranial infection after neuroendoscopic transnasal pituitary adenoma resection. BMC Neurosci. 2022, 23, 1. [Google Scholar] [CrossRef]
- Zhang, Y.; Zeng, Q.; Fang, Y.; Wang, W.; Chen, Y. Risk Prediction of Central Nervous System Infection Secondary to Intraventricular Drainage in Patients with Intracerebral Hemorrhage: Development and Evaluation of a New Predictive Model Nomogram. Ther. Innov. Regul. Sci. 2022, 56, 651–658. [Google Scholar] [CrossRef]
- Korinek, A.M. Risk factors for neurosurgical site infections after craniotomy: A prospective multicenter study of 2944 patients. The French Study Group of Neurosurgical Infections, the SEHP, and the C-CLIN Paris-Nord. Service Epidémiologie Hygiène et Prévention. Neurosurgery 1997, 41, 1073–1079. [Google Scholar] [CrossRef]
- Witteveen, E.; Wieske, L.; Sommers, J. Early Prediction of Intensive Care Unit-Acquired Weakness: A Multicenter External Validation Study. J. Intensive Care Med. 2020, 35, 595–605. [Google Scholar] [CrossRef] [Green Version]
- Zhao, T.; Xu, X.-L.; Nie, J.-M.; Chen, X.-H.; Jiang, Z.-S.; Liu, S.-Q.; Yang, T.-T.; Yang, X.; Sun, F.; Lu, Y.-Q.; et al. Establishment of a novel scoring model for mortality risk prediction in HIV-infected patients with cryptococcal meningitis. BMC Infect. Dis. 2021, 21, 786. [Google Scholar] [CrossRef]
- Van de Beek, D.; Cabellos, C.; Dzupova, O.; Esposito, S.; Klein, M.; Kloek, A.; Leib, S.; Mourvillier, B.; Ostergaard, C.; Pagliano, P.; et al. ESCMID guideline: Diagnosis and treatment of acute bacterial meningitis. Clin. Microbiol. Infect. 2016, 22 (Suppl. S3), S37–S62. [Google Scholar] [CrossRef] [Green Version]



| Characteristic | Training Set (n = 998) | Validation Set (n = 866) | Z/χ2 Value | p-Value |
|---|---|---|---|---|
| Male/female (cases) | 530/468 | 464/402 | 0.042 | 0.838 |
| Age [n(%)] | ||||
| 18~40 years | 260 (26.1) | 216 (24.9) | 0.300 | 0.584 |
| 40~50 years | 128 (12.8) | 129 (14.9) | 1.672 | 0.196 |
| 50~60 years | 252 (25.3) | 241 (27.8) | 1.276 | 0.259 |
| 60~70 years | 150 (15.0) | 129 (14.9) | 0.007 | 0.936 |
| >70 years | 208 (20.8) | 151 (17.4) | 3.457 | 0.063 |
| Comorbidities [n(%)] | ||||
| Hypertension | 206 (20.6) | 199 (23.0) | 1.490 | 0.222 |
| Diabetes | 96 (9.6) | 90 (10.4) | 0.309 | 0.578 |
| Infection in other parts | 38 (3.8) | 43 (5.0) | 1.598 | 0.206 |
| Autoimmune disease | 26 (2.6) | 12 (1.4) | 3.453 | 0.063 |
| Pathogenies [n(%)] | ||||
| Open craniocerebral injury | 177 (17.7) | 128 (14.8) | 2.958 | 0.085 |
| Closed craniocerebral injury | 65 (6.5) | 77 (8.9) | 3.727 | 0.054 |
| Hemorrhagic stroke | 356 (35.7) | 287 (33.1) | 1.314 | 0.252 |
| Ischemic stroke | 61 (6.1) | 45 (5.2) | 6.338 | 0.012 |
| Intracranial tumor | 290 (29.1) | 285 (32.9) | 3.225 | 0.073 |
| Others | 49 (4.9) | 44 (5.1) | 0.014 | 0.905 |
| Type of infections [n(%)] | ||||
| Epidural abscess | 11 (9.7) | 0 (0.0) | - | <0.001 a |
| Subdural empyema | 7 (6.2) | 0 (0.0) | - | <0.001 a |
| Meningitis | 41 (36.3) | 0 (0.0) | - | <0.001 a |
| Ventriculitis | 22 (19.5) | 0 (0.0) | - | <0.001 a |
| Brain abscess | 32 (28.3) | 0 (0.0) | - | <0.001 a |
| Pathogen types [n(%)] | ||||
| G+ | 31 (27.4) | 0 (0.0) | - | <0.001 a |
| G− | 35 (31.0) | 0 (0.0) | - | <0.001 a |
| Fungus | 9 (8.0) | 0 (0.0) | - | <0.001 a |
| Type of surgeries [n(%)] | 3.609 | 0.057 | ||
| Emergency surgery | 361 (36.2) | 277 (32.0) | - | - |
| Elective surgery | 637 (63.8) | 589 (68.0) | - | - |
| Operation mode [n(%)] | ||||
| Craniotomy | 35 (31.0) | 259 (34.4) | 0.513 | 0.474 |
| Cranial burr-hole | 47 (41.6) | 296 (39.3) | 0.214 | 0.644 |
| Neuroendoscope | 31 (27.4) | 198 (26.3) | 0.066 | 0.798 |
| Operation time [n(%)] | 1.877 | 0.171 | ||
| ≥4 h | 222 (22.2) | 216 (24.9) | - | - |
| <4 h | 776 (77.8) | 650 (75.1) | - | - |
| Intraoperative bleeding [n(%)] | 1.297 | 0.255 | ||
| ≥400 mL | 161 (16.1) | 155 (18.1) | - | - |
| <400 mL | 837 (83.9) | 700 (81.9) | - | - |
| CSF leak [n(%)] | 39 (3.9) | 42 (4.8) | 0.990 | 0.320 |
| Intracranial drainage tube [n(%)] | ||||
| ≥72 h | 334 (33.5) | 312 (36.0) | 1.343 | 0.247 |
| <72 h | 328 (32.9) | 304 (35.1) | 1.036 | 0.309 |
| Lumbar cistern drainage [n(%)] | ||||
| ≥72 h | 272 (27.3) | 258 (29.8) | 1.467 | 0.226 |
| <72 h | 216 (21.6) | 158 (18.2) | 3.339 | 0.068 |
| After CPCR [n(%)] | 50 (5.0) | 52 (6.0) | 0.887 | 0.346 |
| Complicated with Shock [n(%)] | 136 (13.6) | 132 (15.2) | 0.983 | 0.322 |
| Mechanical ventilation time [n(%)] | ||||
| ≥48 h | 149 (15.1) | 152 (17.6) | 2.072 | 0.150 |
| <48 h | 200 (20.0) | 156 (18.0) | 1.232 | 0.267 |
| Total parenteral nutrition ≥ 5 d [n(%)] | 139 (13.9) | 146 (16.9) | 3.076 | 0.079 |
| ALB ≤ 30 g/L [n(%)] | 420 (42.1) | 354 (40.9) | 0.278 | 0.598 |
| The duration of ICU [days,M(QL, QU)] | 4.0 (3.0,5.0) | 5.0 (4.0,6.0) | −8.393 | <0.001 |
| APACHE II score [points,M(QL, QU)] | 13.0 (10.0,16.0) | 13.0 (10.0,17.0) | −3.599 | <0.001 |
| GCS score [points,M(QL, QU)] | 14.0 (8.0,15.0) | 12.0 (6.0,15.0) | −4.116 | <0.001 |
| Variable | Β | SE | Wald | p | OR | 95%CI |
|---|---|---|---|---|---|---|
| Age > 70 y | 1.171 | 0.261 | 20.179 | <0.001 | 3.225 | 1.935–5.375 |
| History of diabetes | 1.253 | 0.310 | 16.355 | <0.001 | 3.502 | 1.908–6.429 |
| APACHE II score | −0.002 | 0.027 | 0.007 | 0.931 | 0.998 | 0.946–1.053 |
| GCS score | 0.002 | 0.028 | 0.008 | 0.930 | 1.002 | 0.948–1.060 |
| Emergency surgery | 1.033 | 0.240 | 18.462 | <0.001 | 2.808 | 1.753–4.498 |
| Operation time ≥ 4 h | −0.610 | 0.295 | 4.284 | 0.038 | 0.543 | 0.305–0.968 |
| Lumbar cistern drainage ≥ 72 h | 1.739 | 0.304 | 32.710 | <0.001 | 5.689 | 3.135–10.323 |
| Intracranial drainage tube ≥ 72 h | 0.949 | 0.241 | 15.513 | <0.001 | 2.583 | 1.611–4.143 |
| CSF leak | 0.503 | 0.516 | 0.591 | 0.329 | 1.654 | 0.602–4.545 |
| Intraoperative bleeding ≥ 400 mL | 0.923 | 0.282 | 10.725 | 0.001 | 2.516 | 1.448–4.370 |
| Complicated with Shock | 1.080 | 0.296 | 13.328 | <0.001 | 2.945 | 1.649–5.258 |
| Total parenteral nutrition ≥ 5 d | 0.324 | 0.330 | 0.964 | 0.326 | 1.383 | 0.724–2.641 |
| ALB ≤ 30 g/L | 0.769 | 0.238 | 10.421 | 0.001 | 2.158 | 1.353–3.442 |
| The duration of ICU ≥ 3 d | 0.199 | 0.047 | 17.839 | <0.001 | 1.220 | 1.112–1.337 |
| Constant | −5.637 | 0.698 | 65.226 | 0.000 | 0.004 | -- |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheng, L.; Bai, W.; Song, P.; Zhou, L.; Li, Z.; Gao, L.; Zhou, C.; Cai, Q. Development and Validation of a Nomograph Model for Post-Operative Central Nervous System Infection after Craniocerebral Surgery. Diagnostics 2023, 13, 2207. https://doi.org/10.3390/diagnostics13132207
Cheng L, Bai W, Song P, Zhou L, Li Z, Gao L, Zhou C, Cai Q. Development and Validation of a Nomograph Model for Post-Operative Central Nervous System Infection after Craniocerebral Surgery. Diagnostics. 2023; 13(13):2207. https://doi.org/10.3390/diagnostics13132207
Chicago/Turabian StyleCheng, Li, Wenhui Bai, Ping Song, Long Zhou, Zhiyang Li, Lun Gao, Chenliang Zhou, and Qiang Cai. 2023. "Development and Validation of a Nomograph Model for Post-Operative Central Nervous System Infection after Craniocerebral Surgery" Diagnostics 13, no. 13: 2207. https://doi.org/10.3390/diagnostics13132207
APA StyleCheng, L., Bai, W., Song, P., Zhou, L., Li, Z., Gao, L., Zhou, C., & Cai, Q. (2023). Development and Validation of a Nomograph Model for Post-Operative Central Nervous System Infection after Craniocerebral Surgery. Diagnostics, 13(13), 2207. https://doi.org/10.3390/diagnostics13132207





