Coarctation of the Aorta: Diagnosis and Management
Abstract
:1. Introduction
2. History and Anatomical Descriptions
3. Pathophysiology and Genetics
- Extension of ductal tissue into the aorta, causing constriction of the aorta when the ductus arteriosus closes at birth
- Hemodynamic reduction in LV forward flow leading to abnormal development of the aorta, which would be supported by the association of other left-sided obstructive lesions with CoA
- Abnormalities of the migration of neural crest cells which are the origin of parts of the aorta and left ventricular outflow tract and valves [20].
4. Clinical Presentation
5. Diagnosis—Cardiovascular Imaging
6. Fetal Echocardiography
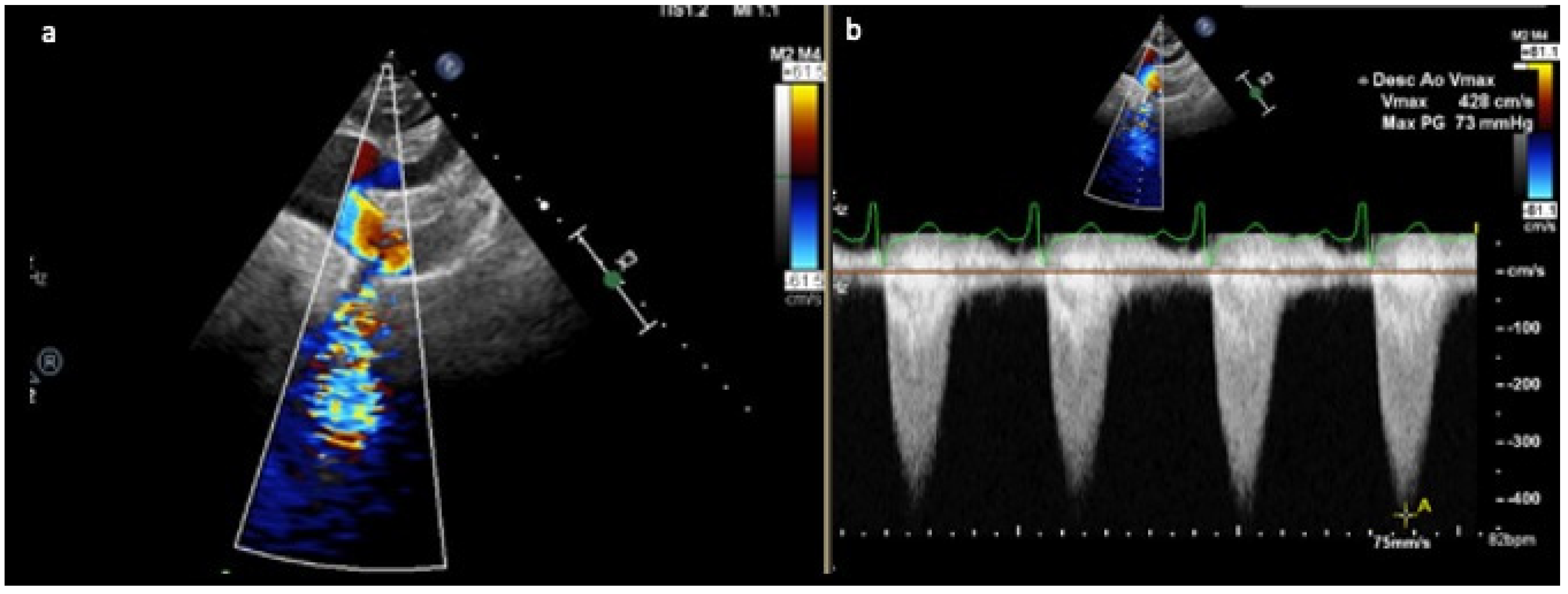
7. Paediatric and Adult Echocardiography
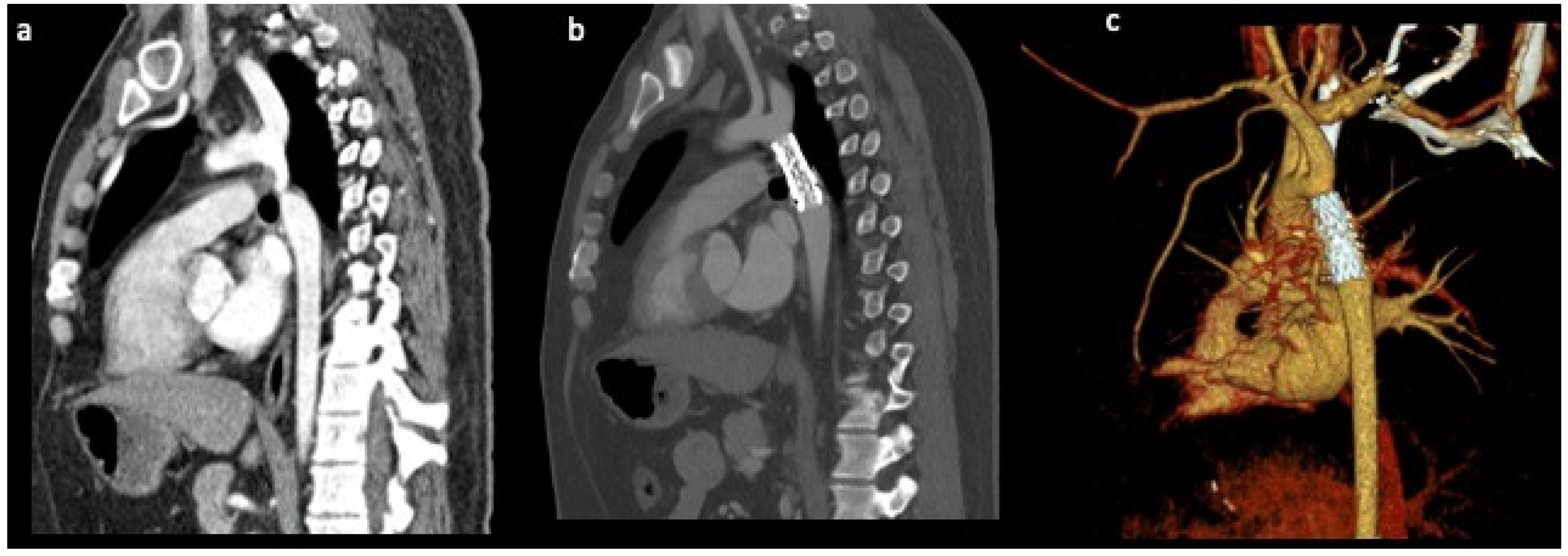
8. Cardiac Computed Tomography
9. Cardiac Magnetic Resonance Imaging
10. Diagnosis—Cardiac Catheterisation
11. Prognosis
12. Treatment
Surgery
13. Transcatheter Interventions
13.1. Balloon Angioplasty
13.2. Stent Implantation
14. Long-Term Complications
14.1. Recoarctation and Reintervention
14.2. Hypertension
14.3. Aortic Aneurysm
14.4. Stroke and Coronary Artery Disease
14.5. LV Remodelling and Failure
15. Pregnancy
16. Conclusions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Roger, V.L.; Go, A.S.; Lloyd-Jones, D.M.; Adams, R.J.; Berry, J.D.; Brown, T.M.; Carnethon, M.R.; Dai, S.; De Simone, G.; Ford, E.S.; et al. Heart Disease and Stroke Statistics—2011 Update. A Report from the American Heart Association. Circulation 2011, 123, e18–e209. [Google Scholar] [CrossRef] [Green Version]
- Reller, M.D.; Strickland, M.J.; Riehle-Colarusso, T.; Mahle, W.T.; Correa, A. Prevalence of Congenital Heart Defects in Metropolitan Atlanta, 1998–2005. J. Pediatr. 2008, 153, 807–813. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crafoord, C.; Nylin, G. Congenital coarctation of the aorta and its surgical treatment. J. Thorac. Surg. 1945, 14, 347–361. [Google Scholar] [CrossRef]
- Hoschtitzky, J.A.; Anderson, R.H.; Elliott, M.J. CHAPTER 46—Aortic Coarctation and Interrupted Aortic Arch. In Paediatric Cardiology, 3rd ed.; Anderson, R.H., Baker, E.J., Penny, D.J., Redington, A.N., Rigby, M.L., Wernovsky, G., Eds.; Churchill Livingstone: Philadelphia, PA, USA, 2010; pp. 945–966. [Google Scholar] [CrossRef]
- Stout, K.K.; Daniels, C.J.; Aboulhosn, J.A.; Bozkurt, B.; Broberg, C.S.; Colman, J.M.; Crumb, S.R.; Dearani, J.A.; Fuller, S.; Gurvitz, M.; et al. 2018 AHA/ACC Guideline for the Management of Adults with Congenital Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 139, e698–e800. [Google Scholar] [CrossRef]
- Baumgartner, H.; De Backer, J.; Babu-Narayan, S.V.; Budts, W.; Chessa, M.; Diller, G.-P.; Lung, B.; Kluin, J.; Lang, I.M.; Meijboom, F.; et al. 2020 ESC Guidelines for the Management of Adult Congenital Heart Disease: The Task Force for the Management of Adult Congenital Heart Disease of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Card. Eur. Heart J. 2021, 42, 563–645. [Google Scholar] [CrossRef]
- Keshavarz-Motamed, Z.; Edelman, E.R.; Motamed, P.K.; Garcia, J.; Dahdah, N.; Kadem, L. The role of aortic compliance in determination of coarctation severity: Lumped parameter modeling, in vitro study and clinical evaluation. J. Biomech. 2015, 48, 4229–4237. [Google Scholar] [CrossRef] [Green Version]
- Teo, L.L.S.; Cannell, T.; Babu-Narayan, S.V.; Hughes, M.; Mohiaddin, R.H. Prevalence of Associated Cardiovascular Abnormalities in 500 Patients with Aortic Coarctation Referred for Cardiovascular Magnetic Resonance Imaging to a Tertiary Center. Pediatr. Cardiol. 2011, 32, 1120–1127. [Google Scholar] [CrossRef]
- Becker, A.E.; Becker, M.J.; Edwards, J.E. Anomalies Associated with Coarctation of Aorta Particular Reference to Infancy. Circulation 1970, 41, 1067–1075. [Google Scholar] [CrossRef] [Green Version]
- Grattan, M.; Prince, A.; Rumman, R.K.; Morgan, C.; Petrovic, M.; Hauck, A.; Young, L.; Franco-Cereceda, A.; Loeys, B.; Mohamed, S.A.; et al. Predictors of Bicuspid Aortic Valve–Associated Aortopathy in Childhood. Circ. Cardiovasc. Imaging 2020, 13, e009717. [Google Scholar] [CrossRef] [PubMed]
- Shone, J.D.; Sellers, R.D.; Anderson, R.C.; Adams, P.; Lillehei, C.; Edwards, J.E. The developmental complex of “parachute mitral valve”, supravalvular ring of left atrium, subaortic stenosis, and coarctation of aorta. Am. J. Cardiol. 1963, 11, 714–725. [Google Scholar] [CrossRef]
- Aslam, S.; Khairy, P.; Shohoudi, A.; Mercier, L.-A.; Dore, A.; Marcotte, F.; Miró, J.; Avila-Alonso, P.; Ibrahim, R.; Asgar, A.; et al. Shone Complex: An Under-recognized Congenital Heart Disease with Substantial Morbidity in Adulthood. Can. J. Cardiol. 2017, 33, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Warnes, C.A. Bicuspid aortic valve and coarctation: Two villains part of a diffuse problem. Heart 2003, 89, 965–966. [Google Scholar] [CrossRef] [PubMed]
- Ellesøe, S.G.; Workman, C.T.; Bouvagnet, P.; Loffredo, C.A.; McBride, K.L.; Hinton, R.B.; van Engelen, K.; Gertsen, E.C.; Mulder, B.J.M.; Postma, A.V.; et al. Familial co-occurrence of congenital heart defects follows distinct patterns. Eur. Heart J. 2018, 39, 1015–1022. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parker, L.E.; Landstrom, A.P. Genetic Etiology of Left-Sided Obstructive Heart Lesions: A Story in Development. J. Am. Heart Assoc. 2021, 10, e019006. [Google Scholar] [CrossRef]
- Garg, V.; Muth, A.N.; Ransom, J.F.; Schluterman, M.K.; Barnes, R.; King, I.N.; Grossfeld, P.D.; Srivastava, D. Mutations in NOTCH1 cause aortic valve disease. Nature 2005, 437, 270–274. [Google Scholar] [CrossRef]
- Andelfinger, G.; Tapper, A.R.; Welch, R.C.; Vanoye, C.G.; George, A.L.; Benson, D.W. KCNJ2 Mutation Results in Andersen Syndrome with Sex-Specific Cardiac and Skeletal Muscle Phenotypes. Am. J. Hum. Genet. 2002, 71, 663–668. [Google Scholar] [CrossRef] [Green Version]
- Prandstraller, D.; Mazzanti, L.; Picchio, F.; Magnani, C.; Bergamaschi, R.; Perri, A.; Tsingos, E.; Cacciari, E. Turner’s Syndrome: Cardiologic Profile According to the Different Chromosomal Patterns and Long-Term Clinical Follow-Up of 136 Nonpreselected Patients. Pediatr. Cardiol. 1999, 20, 108–112. [Google Scholar] [CrossRef]
- Krag-Olsen, B.; Nielsen, J.; Sorensen, B.K.E. Prevalence of Cardiovascular Malformations and Association with Karyotypes in Turner’s Syndrome. Arch. Dis. Child. 1994, 71, 433–436. [Google Scholar]
- Yokoyama, U.; Ichikawa, Y.; Minamisawa, S.; Ishikawa, Y. Pathology and molecular mechanisms of coarctation of the aorta and its association with the ductus arteriosus. J. Physiol. Sci. 2017, 67, 259–270. [Google Scholar] [CrossRef]
- Kim, H.S.; Aikawa, M.; Kimura, K.; Kuro-o, M.; Nakahara, K.; Suzuki, T.; Katoh, H.; Okamoto, E.; Yazaki, Y.; Nagai, R. Ductus arteriosus. Advanced differentiation of smooth muscle cells demonstrated by myosin heavy chain isoform expression in rabbits. Circulation 1993, 88, 1804–1810. [Google Scholar] [CrossRef] [Green Version]
- Slomp, J.; Gittenberger-de Groot, A.C.; Glukhova, M.A.; van Munsteren, J.C.; Kockx, M.M.; Schwartz, S.M.; Koteliansky, V.E. Differentiation, Dedifferentiation, and Apoptosis of Smooth Muscle Cells during the Development of the Human Ductus Arteriosus. Arterioscler. Thromb. Vasc. Biol. 1997, 17, 1003–1009. [Google Scholar] [CrossRef]
- Elzenga, N.J.; Groot, A.C.G.-D. Localised coarctation of the aorta. An age dependent spectrum. Br. Heart J. 1983, 49, 317–323. [Google Scholar] [CrossRef] [Green Version]
- Jimenez, M.; Daret, D.; Choussat, A.; Bonnet, J. Immunohistological and ultrastructural analysis of the intimal thickening in coarctation of human aorta. Cardiovasc. Res. 1999, 41, 737–745. [Google Scholar] [CrossRef] [Green Version]
- Anaskovic, I.R.T.; Lic, S.L.I.; Urisic, V.L.J.; Ackovic, M.I.L.; Ilosavljevic, Z.O.M. Histochemical, Immunohisto-chemical and Ultrastructural. Rom. J. Morphol. Embryol. 2019, 60, 1291–1298. [Google Scholar]
- Jonas, R.A. Coarctation: Do we need to resect ductal tissue? Ann. Thorac. Surg. 1991, 52, 604–607. [Google Scholar] [CrossRef]
- High, F.A.; Zhang, M.; Proweller, A.; Tu, L.; Parmacek, M.S.; Pear, W.S.; Epstein, J.A. An essential role for Notch in neural crest during cardiovascular development and smooth muscle differentiation. J. Clin. Investig. 2007, 117, 353–363. [Google Scholar] [CrossRef] [Green Version]
- Jain, R.; Engleka, K.A.; Rentschler, S.L.; Manderfield, L.J.; Li, L.; Yuan, L.; Epstein, J.A. Cardiac neural crest orchestrates remodeling and functional maturation of mouse semilunar valves. J. Clin. Investig. 2011, 121, 422–430. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Head, C.E.G.; Jowett, V.C.; Sharland, G.K.; Simpson, J.M. Timing of presentation and postnatal outcome of infants suspected of having coarctation of the aorta during fetal life. Heart 2005, 91, 1070–1074. [Google Scholar] [CrossRef]
- Lee, M.G.Y.; Babu-Narayan, S.V.; Kempny, A.; Uebing, A.; Montanaro, C.; Shore, D.F.; D’udekem, Y.; Gatzoulis, M.A. Long-term mortality and cardiovascular burden for adult survivors of coarctation of the aorta. Heart 2019, 105, 1190–1196. [Google Scholar] [CrossRef] [PubMed]
- Choudhary, P.; Canniffe, C.; Jackson, D.J.; Tanous, D.; Walsh, K.; Celermajer, D.S. Late outcomes in adults with coarctation of the aorta. Heart 2015, 101, 1190–1195. [Google Scholar] [CrossRef] [PubMed]
- Hede, S.V.; DeVore, G.; Satou, G.; Sklansky, M. Neonatal management of prenatally suspected coarctation of the aorta. Prenat. Diagn. 2020, 40, 942–948. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, D.F.; van Poppel, M.P.; Pushparajah, K.; Vigneswaran, T.V.; Zidere, V.; Steinweg, J.; van Amerom, J.F.; Roberts, T.A.; Schulz, A.; Charakida, M.; et al. Analysis of 3-Dimensional Arch Anatomy, Vascular Flow, and Postnatal Outcome in Cases of Suspected Coarctation of the Aorta Using Fetal Cardiac Magnetic Resonance Imaging. Circ. Cardiovasc. Imaging 2021, 14, e012411. [Google Scholar] [CrossRef]
- Gómez-Montes, E.; Herraiz, I.; Mendoza, A.; Escribano, D.; Galindo, A. Prediction of coarctation of the aorta in the second half of pregnancy. Ultrasound Obstet. Gynecol. 2013, 41, 298–305. [Google Scholar] [CrossRef] [PubMed]
- Quaresima, P.; Fesslova, V.; Farina, A.; Kagan, K.O.; Candiani, M.; Morelli, M.; Crispi, F.; Cavoretto, P.I. How to Do a Fetal Cardiac Scan. In Archives of Gynecology and Obstetrics; Springer Science and Business Media: Berlin/Heidelberg, Germany, 2023. [Google Scholar] [CrossRef]
- Quartermain, M.D.; Hill, K.D.; Goldberg, D.J.; Jacobs, J.P.; Jacobs, M.L.; Pasquali, S.K.; Verghese, G.R.; Wallace, A.S.; Ungerleider, R.M. Prenatal Diagnosis Influences Preoperative Status in Neonates with Congenital Heart Disease: An Analysis of the Society of Thoracic Surgeons Congenital Heart Surgery Database. Pediatr. Cardiol. 2019, 40, 489–496. [Google Scholar] [CrossRef] [PubMed]
- Franklin, O.; Burch, M.; Manning, N.; Sleeman, K.; Gould, S.; Archer, N. Prenatal diagnosis of coarctation of the aorta improves survival and reduces morbidity. Heart 2002, 87, 67–69. [Google Scholar] [CrossRef] [Green Version]
- Eapen, R.S.; Rowland, D.G.; Franklin, W.H. Effect of Prenatal Diagnosis of Critical Left Heart Obstruction on Perinatal Morbidity and Mortality. Am. J. Perinatol. 1998, 15, 237–242. [Google Scholar] [CrossRef]
- Langley, S.M.; Sunstrom, R.E.; Reed, R.D.; Rekito, A.J.; Gerrah, R. The Neonatal Hypoplastic Aortic Arch: Decisions and More Decisions. Semin. Thorac. Cardiovasc. Surg. Pediatr. Card. Surg. Annu. 2013, 16, 43–51. [Google Scholar] [CrossRef]
- Goudar, S.P.; Shah, S.S.; Shirali, G.S. Echocardiography of Coarctation of the Aorta, Aortic Arch Hypoplasia, and Arch Interruption: Strategies for Evaluation of the Aortic Arch. Cardiol. Young 2016, 26, 1553–1562. [Google Scholar] [CrossRef]
- Şişli, E.; Kalın, S.; Tuncer, O.N.; Ayık, M.F.; Alper, H.; Levent, R.E.; Şahin, H.; Atay, Y. Comparison Between Nomograms Used to Define Pediatric Aortic Arch Hypoplasia: Retrospective Evaluation among Patients Less Than 1 Year Old with Coarctation of the Aorta. Pediatr. Cardiol. 2019, 40, 1190–1198. [Google Scholar] [CrossRef]
- Pettersen, M.D.; Du, W.; Skeens, M.E.; Humes, R.A. Regression Equations for Calculation of Z Scores of Cardiac Structures in a Large Cohort of Healthy Infants, Children, and Adolescents: An Echocardiographic Study. J. Am. Soc. Echocardiogr. 2008, 21, 922–934. [Google Scholar] [CrossRef]
- Bruse, J.L.; Khushnood, A.; McLeod, K.; Biglino, G.; Sermesant, M.; Pennec, X.; Taylor, A.M.; Hsia, T.-Y.; Schievano, S.; Khambadkone, S.; et al. How successful is successful? Aortic arch shape after successful aortic coarctation repair correlates with left ventricular function. J. Thorac. Cardiovasc. Surg. 2017, 153, 418–427. [Google Scholar] [CrossRef] [Green Version]
- Van Ooij, P.; Farag, E.S.; Blanken, C.P.S.; Nederveen, A.J.; Groenink, M.; Planken, R.N.; Boekholdt, S.M. Fully quantitative mapping of abnormal aortic velocity and wall shear stress direction in patients with bicuspid aortic valves and repaired coarctation using 4D flow cardiovascular magnetic resonance. J. Cardiovasc. Magn. Reson. 2021, 23, 9. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, R.; Thomas, N.; Ullah, A.H.; Eichholz, B.; Estevadeordal, J.; Suzen, Y.B. Experimental and computational study of pulsatile flow characteristics in Romanesque and gothic aortic arch models. Med. Eng. Phys. 2022, 102, 103784. [Google Scholar] [CrossRef] [PubMed]
- Ou, P.; Bonnet, D.; Auriacombe, L.; Pedroni, E.; Balleux, F.; Sidi, D.; Mousseaux, E. Late systemic hypertension and aortic arch geometry after successful repair of coarctation of the aorta. Eur. Heart J. 2004, 25, 1853–1859. [Google Scholar] [CrossRef]
- Donazzan, L.; Crepaz, R.; Stuefer, J.; Stellin, G. Abnormalities of Aortic Arch Shape, Central Aortic Flow Dynamics, and Distensibility Predispose to Hypertension after Successful Repair of Aortic Coarctation. World J. Pediatr. Congenit. Heart Surg. 2014, 5, 546–553. [Google Scholar] [CrossRef] [PubMed]
- Ou, P.; Celermajer, D.S.; Mousseaux, E.; Giron, A.; Aggoun, Y.; Szezepanski, I.; Sidi, D.; Bonnet, D. Vascular Remodeling after “Successful” Repair of Coarctation. J. Am. Coll. Cardiol. 2007, 49, 883–890. [Google Scholar] [CrossRef]
- Sophocleous, F.; Biffi, B.; Milano, E.G.; Bruse, J.; Caputo, M.; Rajakaruna, C.; Schievano, S.; Emanueli, C.; Bucciarelli-Ducci, C.; Biglino, G. Aortic morphological variability in patients with bicuspid aortic valve and aortic coarctation. Eur. J. Cardio-Thoracic Surg. 2019, 55, 704–713. [Google Scholar] [CrossRef]
- Goodarzi Ardakani, V.; Goordoyal, H.; Ordonez, M.V.; Sophocleous, F.; Curtis, S.; Bedair, R.; Caputo, M.; Gambaruto, A.; Biglino, G. Isolating the Effect of Arch Architecture on Aortic Hemodynamics Late after Coarctation Repair: A Computational Study. Front. Cardiovasc. Med. 2022, 9, 1599. [Google Scholar] [CrossRef]
- Abbott, M.E. Coarctation of the aorta of the adult type: II. A statistical study and historical retrospect of 200 recorded cases with autopsy, of stenosis or obliteration of the descending arch in subjects above the age of two years. Am. Heart J. 1928, 3, 574–618. [Google Scholar] [CrossRef]
- Tulzer, A.; Mair, R.; Kreuzer, M.; Tulzer, G. Outcome of aortic arch reconstruction in infants with coarctation: Importance of operative approach. J. Thorac. Cardiovasc. Surg. 2016, 152, 1506–1513.e1. [Google Scholar] [CrossRef] [Green Version]
- Walhout, R.J.; Lekkerkerker, J.C.; Oron, G.H.; Hitchcock, F.J.; Meijboom, E.J.; Bennink, G.B. Comparison of polytetrafluoroethylene patch aortoplasty and end-to-end anastomosis for coarctation of the aorta. J. Thorac. Cardiovasc. Surg. 2003, 126, 521–528. [Google Scholar] [CrossRef] [Green Version]
- Mery, C.M.; Guzmán-Pruneda, F.A.; Trost, J.G., Jr.; McLaughlin, E.; Smith, B.M.; Parekh, D.R.; Adachi, I.; Heinle, J.S.; McKenzie, E.D.; Fraser, C.D., Jr. Contemporary Results of Aortic Coarctation Repair Through Left Thoracotomy. Ann. Thorac. Surg. 2015, 100, 1039–1046. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, M.L.; Burkhart, H.M.; Connolly, H.M.; Dearani, J.A.; Cetta, F.; Li, Z.; Oliver, W.C.; Warnes, C.A.; Schaff, H.V. Coarctation of the Aorta: Lifelong Surveillance Is Mandatory Following Surgical Repair. J. Am. Coll. Cardiol. 2013, 62, 1020–1025. [Google Scholar] [CrossRef] [Green Version]
- Jahangiri, M.; Shinebourne, E.A.; Zurakowski, D.; Rigby, M.L.; Redington, A.N.; Lincoln, C. Subclavian flap angioplasty: Does the arch look after itself? J. Thorac. Cardiovasc. Surg. 2000, 120, 224–229. [Google Scholar] [CrossRef] [Green Version]
- Forbes, T.J.; Kim, D.W.; Du, W.; Turner, D.R.; Holzer, R.; Amin, Z.; Hijazi, Z.; Ghasemi, A.; Rome, J.J.; Nykanen, D.; et al. Comparison of Surgical, Stent, and Balloon Angioplasty Treatment of Native Coarctation of the Aorta: An Observational Study by the CCISC (Congenital Cardiovascular Interventional Study Consortium). J. Am. Coll. Cardiol. 2011, 58, 2664–2674. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salcher, M.; Naci, H.; Law, T.J.; Kuehne, T.; Schubert, S.; Kelm, M.; Morley-Fletcher, E.; Hennemuth, A.; Manset, D.; Mcguire, A.; et al. Balloon Dilatation and Stenting for Aortic Coarctation. Circ. Cardiovasc. Interv. 2016, 9, e003153. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Butera, G.; Manica, J.L.L.; Marini, D.; Piazza, L.; Chessa, M.; Filho, R.I.R.; Leite, R.E.S.; Carminati, M. From Bare to Covered. Catheter. Cardiovasc. Interv. 2014, 83, 953–963. [Google Scholar] [CrossRef]
- Holzer, R.J.; Gauvreau, K.; McEnaney, K.; Watanabe, H.; Ringel, R. Long-Term Outcomes of the Coarctation of the Aorta Stent Trials. Circ. Cardiovasc. Interv. 2021, 14, e010308. [Google Scholar] [CrossRef] [PubMed]
- Meadows, J.; Minahan, M.; McElhinney, D.B.; McEnaney, K.; Ringel, R. Intermediate Outcomes in the Prospective, Multicenter Coarctation of the Aorta Stent Trial (COAST). Circulation 2015, 131, 1656–1664. [Google Scholar] [CrossRef] [Green Version]
- Taggart, N.W.; Minahan, M.; Cabalka, A.K.; Cetta, F.; Usmani, K.; Ringel, R.E. Immediate Outcomes of Covered Stent Placement for Treatment or Prevention of Aortic Wall Injury Associated with Coarctation of the Aorta (COAST II). JACC Cardiovasc. Interv. 2016, 9, 484–493. [Google Scholar] [CrossRef]
- Boe, B.A.; Armstrong, A.K.; Janse, S.A.; Loccoh, E.C.; Stockmaster, K.; Holzer, R.J.; Cheatham, S.L.; Cheatham, J.P.; Berman, D.P. Percutaneous Implantation of Adult Sized Stents for Coarctation of the Aorta in Children ≤20 kg. Circ. Cardiovasc. Interv. 2021, 14, e009399. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.-L.; Tometzki, A.; Taliotis, D.; Martin, R. Stent Therapy for Aortic Coarctation in Children <30 Kg: Use of the Low Profile Valeo Stent. Pediatr. Cardiol. 2017, 38, 1441–1449. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.S.M.; Dimopoulos, K.; Alonso-Gonzalez, R.; Liodakis, E.; Teijeira-Fernandez, E.; Alvarez-Barredo, M.; Kempny, A.; Diller, G.; Uebing, A.; Shore, D.; et al. Prevalence and prognostic implication of restenosis or dilatation at the aortic coarctation repair site assessed by cardiovascular MRI in adult patients late after coarctation repair. Int. J. Cardiol. 2014, 173, 209–215. [Google Scholar] [CrossRef]
- Canniffe, C.; Ou, P.; Walsh, K.; Bonnet, D.; Celermajer, D. Hypertension after repair of aortic coarctation—A systematic review. Int. J. Cardiol. 2013, 167, 2456–2461. [Google Scholar] [CrossRef]
- Martins, J.D.; Zachariah, J.; Selamet Tierney, E.S.; Truong, U.; Morris, S.A.; Kutty, S.; de Ferranti, S.D.; Guarino, M.; Thomas, B.; Oliveira, D.; et al. Impact of Treatment Modality on Vascular Function in Coarctation of the Aorta: The LOVE-COARCT Study. J. Am. Heart Assoc. 2019, 8, e011536. [Google Scholar] [CrossRef] [Green Version]
- Pieper, T.; Latus, H.; Schranz, D.; Kreuder, J.; Reich, B.; Gummel, K.; Hudel, H.; Voges, I. Aortic elasticity after aortic coarctation relief: Comparison of surgical and interventional therapy by cardiovascular magnetic resonance imaging. BMC Cardiovasc. Disord. 2019, 19, 286. [Google Scholar] [CrossRef]
- De Divitiis, M.; Pilla, C.; Kattenhorn, M.; Zadinello, M.; Donald, A.; Leeson, P.; Wallace, S.; Redington, A.; Deanfield, J.E. Vascular Dysfunction after Repair of Coarctation of the Aorta. Circulation 2001, 104 (Suppl. S1), I-165–I-170. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gardiner, H.M.; Celermajer, D.S.; Sorensen, K.; Georgakopoulos, D.; Robinson, J.; Thomas, O.; Deanfield, J.E. Arterial reactivity is significantly impaired in normotensive young adults after successful repair of aortic coarctation in childhood. Circulation 1994, 89, 1745–1750. [Google Scholar] [CrossRef] [Green Version]
- Heger, M.; Willfort, A.; Neunteufl, T.; Rosenhek, R.; Gabriel, H.; Wollenek, G.; Wimmer, M.; Maurer, G.; Baumgartner, H. Vascular dysfunction after coarctation repair is related to the age at surgery. Int. J. Cardiol. 2005, 99, 295–299. [Google Scholar] [CrossRef]
- Egbe, A.C.; Miranda, W.R.; Connolly, H.M.; Kullo, I.J. Ambulatory blood pressure data is the best approximation of central aortic pressure in coarctation of aorta. Int. J. Cardiol. Congenit. Heart Dis. 2021, 4, 100142. [Google Scholar] [CrossRef]
- Egbe, A.C.; Miranda, W.R.; Jain, C.C.; Borlaug, B.A.; Connolly, H.M. Prognostic Implications of Exercise-Induced Hypertension in Adults with Repaired Coarctation of Aorta. Hypertension 2022, 79, 2796–2805. [Google Scholar] [CrossRef]
- Somers, T.; Nies, H.M.J.M.; van Kimmenade, R.R.J.; Bosboom, D.G.H.; Geuzebroek, G.S.C.; Morshuis, W.J. Necessity of life-long follow-up after surgery for coarctation of the aorta: A case series of very late false aneurysm formation. Eur. Heart J. Case Rep. 2022, 6, ytac073. [Google Scholar] [CrossRef]
- Von Kodolitsch, Y.; Aydin, M.A.; Koschyk, D.H.; Loose, R.; Schalwat, I.; Karck, M.; Cremer, J.; Haverich, A.; Berger, J.; Meinertz, T.; et al. Predictors of aneurysmal formation after surgical correction of aortic coarctation. J. Am. Coll. Cardiol. 2002, 39, 617–624. [Google Scholar] [CrossRef] [Green Version]
- Lim, M.S.; Cordina, R.; Kotchetkova, I.; Celermajer, D.S. Late complication rates after aortic coarctation repair in patients with or without a bicuspid aortic valve. Heart 2022, 108, 855–859. [Google Scholar] [CrossRef] [PubMed]
- Pickard, S.S.; Gauvreau, K.; Gurvitz, M.; Gagne, J.J.; Opotowsky, A.R.; Jenkins, K.J.; Prakash, A. Stroke in Adults with Coarctation of the Aorta: A National Population-Based Study. J. Am. Heart Assoc. 2023, 7, e009072. [Google Scholar] [CrossRef] [Green Version]
- Giang, K.W.; Fedchenko, M.; Dellborg, M.; Eriksson, P.; Mandalenakis, Z. Burden of Ischemic Stroke in Patients with Congenital Heart Disease: A Nationwide, Case-Control Study. J. Am. Heart Assoc. 2021, 10, e020939. [Google Scholar] [CrossRef]
- Giang, K.W.; Mandalenakis, Z.; Dellborg, M.; Lappas, G.; Eriksson, P.; Hansson, P.-O.; Rosengren, A. Long-Term Risk of Hemorrhagic Stroke in Young Patients with Congenital Heart Disease. Stroke 2018, 49, 1155–1162. [Google Scholar] [CrossRef] [PubMed]
- Curtis, S.; Bradley, M.; Wilde, P.; Aw, J.; Chakrabarti, S.; Hamilton, M.; Martin, R.; Turner, M.; Stuart, A.G. Results of Screening for Intracranial Aneurysms in Patients with Coarctation of the Aorta. Am. J. Neuroradiol. 2012, 33, 1182–1186. [Google Scholar] [CrossRef] [Green Version]
- Meijs, T.A.; van Tuijl, R.J.; van den Brink, H.; Weaver, N.A.; Siero, J.C.W.; van der Worp, H.B.; Braun, K.P.J.; Leiner, T.; de Jong, P.A.; Zwanenburg, J.J.M.; et al. Assessment of aortic and cerebral haemodynamics and vascular brain injury with 3 and 7 T magnetic resonance imaging in patients with aortic coarctation. Eur. Heart J. Open 2023, 3, oead001. [Google Scholar] [CrossRef]
- Cokkinos, D.V.; Leachman, R.D.; Cooley, D.A. Increased mortality rate from coronary artery disease following operation for coarctation of the aorta at a late age. J. Thorac. Cardiovasc. Surg. 1979, 77, 315–318. [Google Scholar] [CrossRef] [PubMed]
- Toro-Salazar, O.H.; Steinberger, J.; Thomas, W.; Rocchini, A.P.; Carpenter, B.; Moller, J.H. Long-term follow-up of patients after coarctation of the aorta repair. Am. J. Cardiol. 2002, 89, 541–547. [Google Scholar] [CrossRef]
- Roifman, I.; Therrien, J.; Ionescu-Ittu, R.; Pilote, L.; Guo, L.; Kotowycz, M.A.; Martucci, G.; Marelli, A.J. Coarctation of the Aorta and Coronary Artery Disease. Circulation 2012, 126, 16–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Egbe, A.C.; Rihal, C.S.; Thomas, A.; Boler, A.; Mehra, N.; Andersen, K.; Kothapalli, S.; Taggart, N.W.; Connolly, H.M. Coronary Artery Disease in Adults with Coarctation of Aorta: Incidence, Risk Factors, and Outcomes. J. Am. Heart Assoc. 2019, 8, e012056. [Google Scholar] [CrossRef] [PubMed]
- Moskowitz, W.B.; Schieken, R.M.; Mosteller, M.; Bossano, R. Altered systolic and diastolic function in children after “successful” repair of coarctation of the aorta. Am. Heart J. 1990, 120, 103–109. [Google Scholar] [CrossRef]
- Egbe, A.C.; Miranda, W.R.; Connolly, H.M. Increased prevalence of left ventricular diastolic dysfunction in adults with repaired coarctation of aorta. IJC Heart Vasc. 2020, 28, 100530. [Google Scholar] [CrossRef]
- Menting, M.E.; van Grootel, R.W.J.; van den Bosch, A.E.; Eindhoven, J.A.; McGhie, J.S.; Cuypers, J.A.A.E.; Witsenburg, M.; Helbing, W.A.; Roos-Hesselink, J.W. Quantitative assessment of systolic left ventricular function with speckle-tracking echocardiography in adult patients with repaired aortic coarctation. Int. J. Cardiovasc. Imaging 2016, 32, 777–787. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Egbe, A.C.; Miranda, W.R.; Jain, C.C.; Connolly, H.M. Right Heart Dysfunction in Adults with Coarctation of Aorta: Prevalence and Prognostic Implications. Circ. Cardiovasc. Imaging 2021, 14, 1100–1108. [Google Scholar] [CrossRef]
- Regitz-Zagrosek, V.; Roos-Hesselink, J.W.; Bauersachs, J.; Blomström-Lundqvist, C.; Cífková, R.; De Bonis, M.; Iung, B.; Johnson, M.R.; Kintscher, U.; Kranke, P.; et al. 2018 ESC Guidelines for the Management of Cardiovascular Diseases during Pregnancy: The Task Force for the Management of Cardiovascular Diseases during Pregnancy of the European Society of Cardiology (ESC). Eur. Heart. J. 2018, 39, 3165–3241. [Google Scholar] [CrossRef]
- Van Hagen, I.M.; Roos-Hesselink, J.W. Pregnancy in congenital heart disease: Risk prediction and counselling. Heart 2020, 106, 1853–1861. [Google Scholar] [CrossRef]
- Vriend, J.W.J.; Drenthen, W.; Pieper, P.G.; Roos-Hesselink, J.W.; Zwinderman, A.H.; van Veldhuisen, D.J.; Mulder, B.J.M.; on behalf of the ZAHARA Investigators. Outcome of Pregnancy in Patients after Repair of Aortic Coarctation. Eur. Heart J. 2005, 26, 2173–2178. [Google Scholar] [CrossRef]
- Krieger, E.V.; Landzberg, M.J.; Economy, K.E.; Webb, G.D.; Opotowsky, A.R. Comparison of Risk of Hypertensive Complications of Pregnancy among Women with versus without Coarctation of the Aorta. Am. J. Cardiol. 2011, 107, 1529–1534. [Google Scholar] [CrossRef]
- Beauchesne, L.M.; Connolly, H.M.; Ammash, N.M.; Warnes, C.A. Coarctation of the aorta: Outcome of pregnancy. J. Am. Coll. Cardiol. 2001, 38, 1728–1733. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Plunkett, M.D.; Bond, L.M.; Geiss, D.M. Staged repair of acute Type I aortic dissection and coarctation in pregnancy. Ann. Thorac. Surg. 2000, 69, 1945–1947. [Google Scholar] [CrossRef] [PubMed]
- Siegmund, A.S.; Kampman, M.A.M.; Bilardo, C.M.; Balci, A.; van Dijk, A.P.J.; Oudijk, M.A.; Mulder, B.J.M.; Roos-Hesselink, J.W.; Sieswerda, G.T.; Koenen, S.V.; et al. Pregnancy in women with corrected aortic coarctation: Uteroplacental Doppler flow and pregnancy outcome. Int. J. Cardiol. 2017, 249, 145–150. [Google Scholar] [CrossRef]
- Saidi, A.; Bezold, L.; Altman, C.; Ayres, N.; Bricker, J.T. Outcome of pregnancy following intervention for coarctation of the aorta. Am. J. Cardiol. 1998, 82, 786–788. [Google Scholar] [CrossRef]
- Ramlakhan, K.P.; Tobler, D.; Greutmann, M.; Schwerzmann, M.; Baris, L.; Yetman, A.T.; Nihoyannopoulos, P.; Manga, P.; Boersma, E.; Maggioni, A.P.; et al. Pregnancy outcomes in women with aortic coarctation. Heart 2021, 107, 290–298. [Google Scholar] [CrossRef] [PubMed]



| Age Group | Clinical Symptoms | Examination and Investigation Findings |
|---|---|---|
| Neonates—early presentation | Often asymptomatic prior to ductal closure Tachypnoea Difficulty feeding/failure to thrive | Pulse oximetry-based screening may reveal reduced saturations in the lower limbs compared to the upper limbs, due to left to right shunting through the patent ductus arteriosus Diminished femoral pulses Oliguria, renal failure Left ventricular failure and cardiogenic shock Echo: narrowed aortic segment with pressure gradient across it, ductal patency with left to right shunt Signs of any associated congenital heart lesions, e.g., VSD or aortic stenosis. |
| Neonates— late presentation | Tachypnoea Difficult feeding/failure to thrive | Diminished femoral pulses Intrascapular systolic murmur Echo: Left ventricular hypertrophy and left ventricular failure in addition to CoA ECG reveals left ventricular hypertrophy. CXR may show cardiomegaly and signs of interstitial pulmonary oedema |
| Children–Adults | Often asymptomatic Headaches, epistaxis Lower limb claudication Reduced exercise capacity May more rarely present with symptoms related to complications due to long-term undiagnosed hypertension including coronary artery disease and heart failure | Uncontrolled hypertension Upper and lower limb BP discrepancy Continuous murmur due to collaterals Echo: left ventricular hypertrophy, left ventricular failure, May more rarely present with catastrophic sequelae such as aortic dissection or intracranial haemorrhage |
| Indications for Treatment |
|---|
| Surgical or catheter-based treatment indicated in hypertensive patients with an increased non-invasive gradient between upper and lower limbs confirmed with invasive measurement (peak to peak > 20 mmHg) with preference for catheter treatment (stenting) |
| Catheter treatment should be considered in hypertensive patients with >50% narrowing relative to the aortic diameter at the diaphragm, even if the invasive peak-to-peak gradient is <20 mmHg |
| Catheter treatment should be considered in normotensive patients with an increased non-invasive gradient confirmed with invasive measurement (peak-to-peak > 20 mmhg) |
| Catheter treatment may be considered in normotensive patients with >50% narrowing relative to the aortic diameter at the diaphragm, even if the invasive peak-to-peak gradient is <20 mmHg |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raza, S.; Aggarwal, S.; Jenkins, P.; Kharabish, A.; Anwer, S.; Cullington, D.; Jones, J.; Dua, J.; Papaioannou, V.; Ashrafi, R.; et al. Coarctation of the Aorta: Diagnosis and Management. Diagnostics 2023, 13, 2189. https://doi.org/10.3390/diagnostics13132189
Raza S, Aggarwal S, Jenkins P, Kharabish A, Anwer S, Cullington D, Jones J, Dua J, Papaioannou V, Ashrafi R, et al. Coarctation of the Aorta: Diagnosis and Management. Diagnostics. 2023; 13(13):2189. https://doi.org/10.3390/diagnostics13132189
Chicago/Turabian StyleRaza, Sadaf, Suneil Aggarwal, Petra Jenkins, Ahmed Kharabish, Shehab Anwer, Damien Cullington, Julia Jones, Jaspal Dua, Vasileios Papaioannou, Reza Ashrafi, and et al. 2023. "Coarctation of the Aorta: Diagnosis and Management" Diagnostics 13, no. 13: 2189. https://doi.org/10.3390/diagnostics13132189
APA StyleRaza, S., Aggarwal, S., Jenkins, P., Kharabish, A., Anwer, S., Cullington, D., Jones, J., Dua, J., Papaioannou, V., Ashrafi, R., & Moharem-Elgamal, S. (2023). Coarctation of the Aorta: Diagnosis and Management. Diagnostics, 13(13), 2189. https://doi.org/10.3390/diagnostics13132189





