Somatostatin Receptor Targeted PET-CT and Its Role in the Management and Theranostics of Gastroenteropancreatic Neuroendocrine Neoplasms
Abstract
1. Introduction
2. Radiopharmaceuticals for SSTR-PET Imaging
2.1. Somatostatin Receptor Agonists
2.2. Somatostatin Receptor Antagonists
2.3. Appropriate Use Criteria
- (a)
- Appropriate: Initial staging after histologic diagnosis of NET-9; localization of primary tumor in patients with known metastatic NET but unknown primary-9; selection of patients for SSTR targeting PRRT-9; staging NETs before planned surgery-8; evaluation of mass suggestive of NET and not amenable to endoscopic or percutaneous biopsy-8; monitoring of NETs seen predominantly on SSTR PET-8; evaluation of patients with biochemical evidence and symptoms of NET without evidence on conventional imaging (CI) and without prior histological diagnosis of NET-7; restaging at the time of clinical or laboratory progression without progression on CI-7; and new indeterminate lesion on CI with unclear progression-7.
- (b)
- May be appropriate: Restaging of patients with NETs at initial follow up after resection with curative intent-6; selection of patients with non-functional NETs for SSA treatment-6; and monitoring in patients with NETs seen on both CI and SSTR PET with active disease and no clinical evidence of progression-6.
2.4. Clinical Utility of SSTR-PET
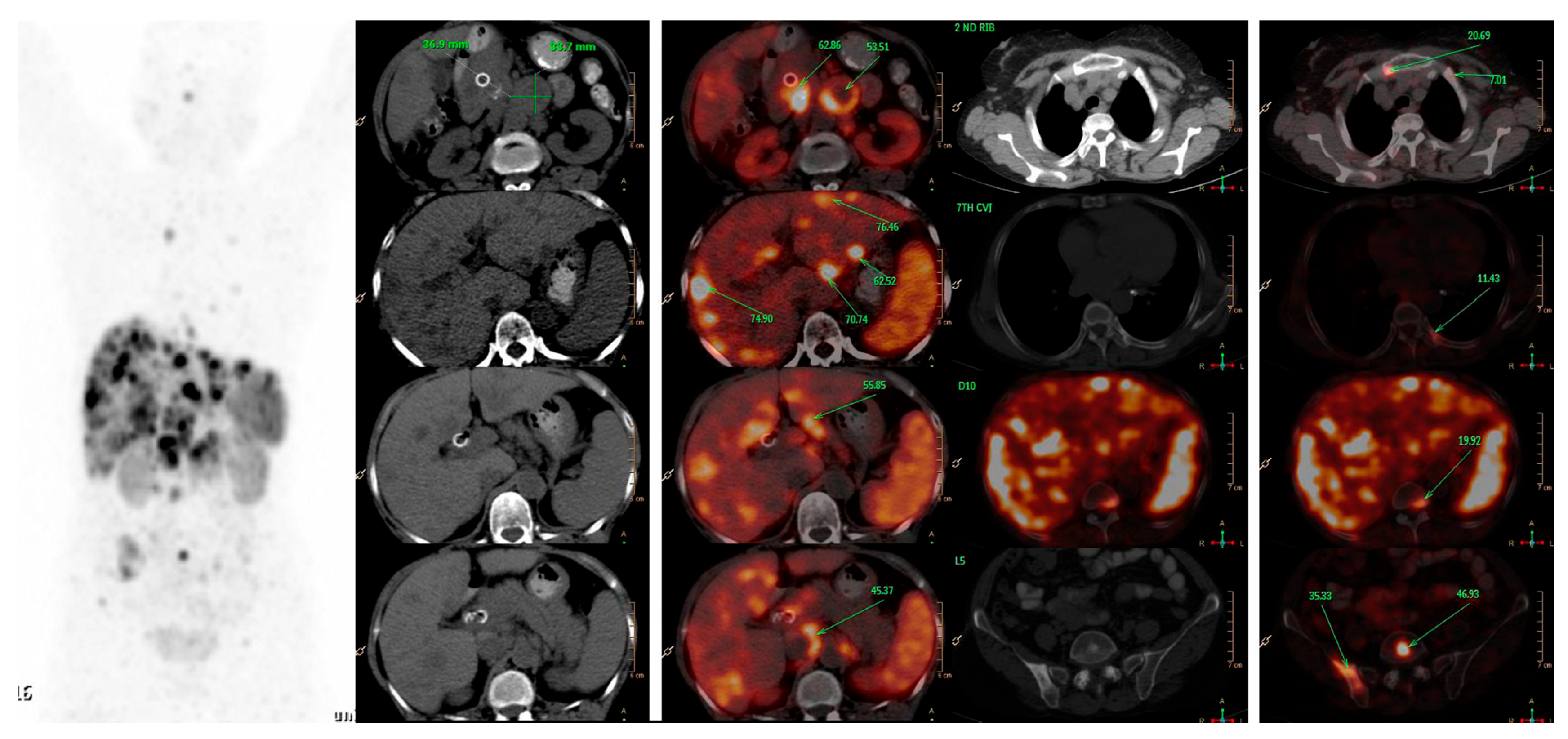
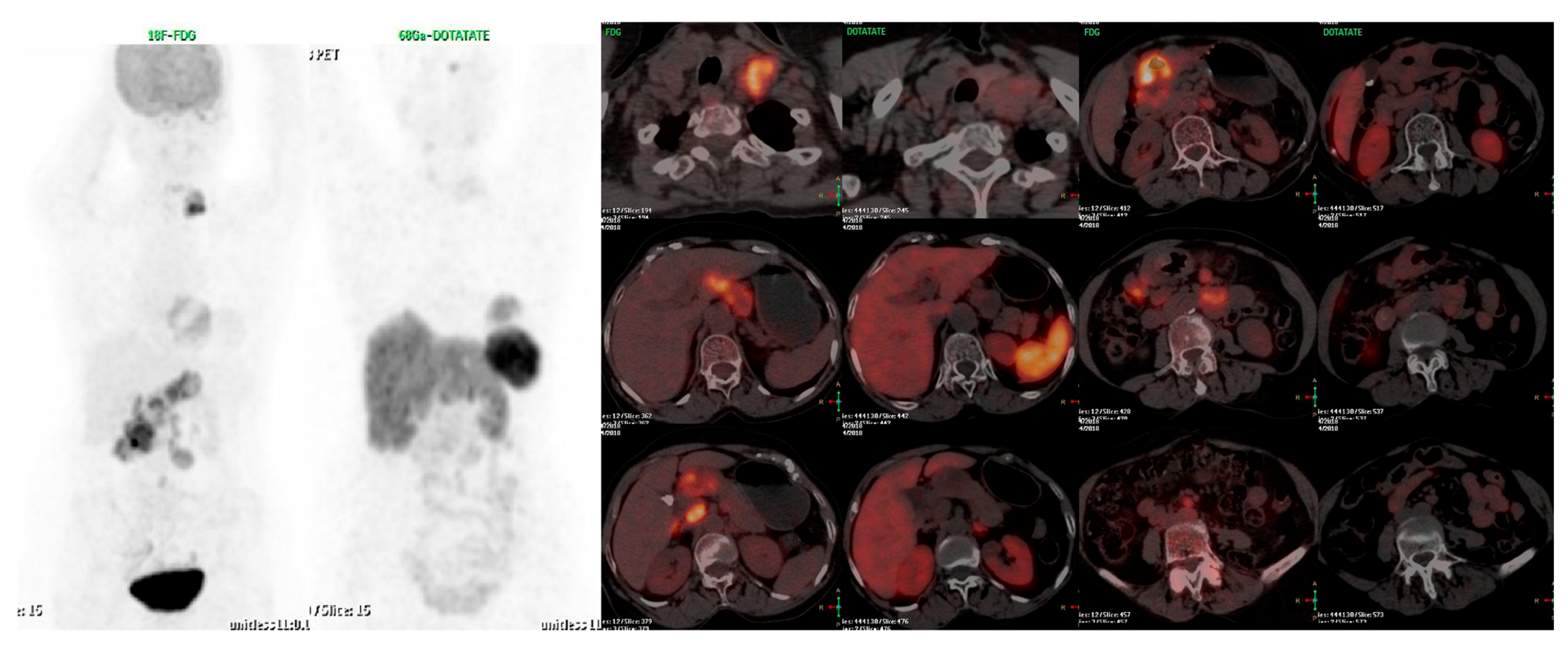
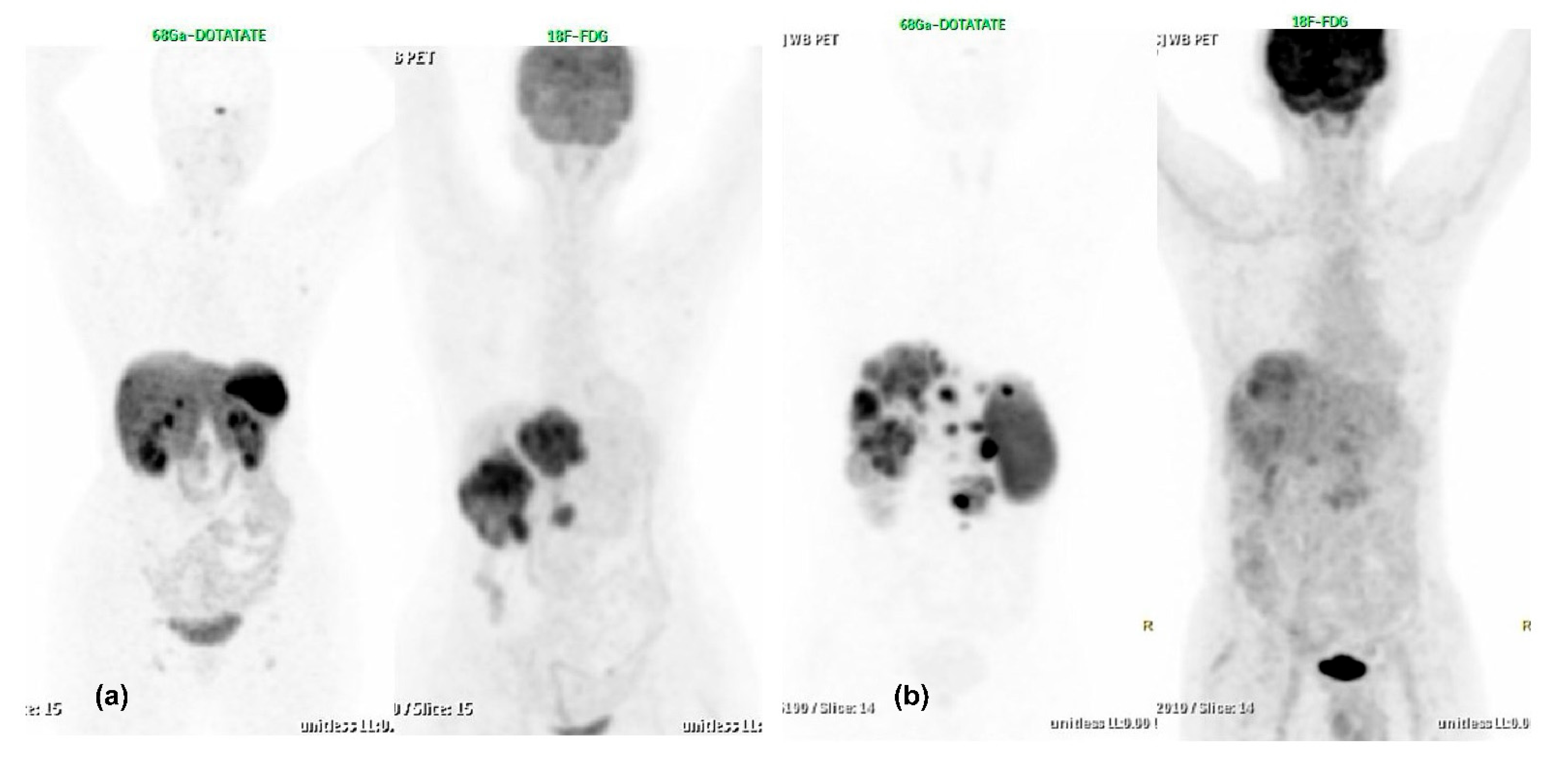
2.5. Dual Tracer PET-CT and Its Critical Role in Neuroendocrine Tumours
2.6. Biodistribution and Incidental Findings on SSTR-Based PET-CT
2.7. Future Directions and Other PET Tracers Used in Neuroendocrine Tumour Imaging
3. Conclusions
Funding
Conflicts of Interest
References
- Hofland, J.; Kaltsas, G.; de Herder, W.W. Advances in the diagnosis and management of well-differentiated neuroendocrine neoplasms. Endocr. Rev. 2019, 41, 371–403. [Google Scholar] [CrossRef]
- Mignon, M. Natural history of neuroendocrine entero-pancreatic tumors. Digestion 2000, 62, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Yao, J.C.; Hassan, M.; Phan, A.; Dagohoy, C.; Leary, C.; Mares, J.E.; Abdalla, E.K.; Fleming, J.B.; Vauthey, J.-N.; Rashid, A.; et al. One hundred years after “carcinoid”: Epidemiology of and prognostic factors for neuroen-docrine tumors in 35, 825 cases in the United States. J. Clin. Oncol. 2008, 26, 3063–3072. [Google Scholar] [CrossRef]
- Modlin, I.M.; Oberg, K.; Chung, D.C.; Jensen, R.T.; de Herder, W.W.; Thakker, P.R.V.; Caplin, M.; Fave, P.G.D.; Kaltsas, G.A.; Krenning, P.E.P.; et al. Gastroenteropancreatic neuroendocrine tumours. Lancet Oncol. 2008, 9, 61–72. [Google Scholar] [CrossRef]
- Hallet, J.; Law, C.H.L.; Cukier, M.; Saskin, R.; Liu, N.; Singh, S. Exploring the rising incidence of neuroendocrine tumors: A population-based analysis of epidemiology, metastatic presentation, and outcomes. Cancer 2014, 121, 589–597. [Google Scholar] [CrossRef] [PubMed]
- Sackstein, P.E.; O’Neil, D.S.; Neugut, A.I.; Chabot, J.; Fojo, T. Epidemiologic trends in neuroendocrine tumors: An examination of incidence rates and survival of specific patient subgroups over the past 20 years. Semin. Oncol. 2018, 45, 249–258. [Google Scholar] [CrossRef]
- Rindi, G.; Klimstra, D.S.; Abedi-Ardekani, B.; Asa, S.L.; Bosman, F.T.; Brambilla, E.; Busam, K.J.; de Krijger, R.R.; Dietel, M.; El-Naggar, A.K.; et al. A common classification framework for neuroendocrine neoplasms: An Interna-tional Agency for Research on Cancer (IARC) and World Health Organization (WHO) expert consensus proposal. Mod. Pathol. 2018, 31, 1770–1786. [Google Scholar] [CrossRef]
- Klimstra, D.S.; Klöppel, G.; La Rosa, S.; Rindi, G. Classification of neuroendocrine neoplasms of the digestive system. In WHO Classification of Tumours, 5th ed.; Digestive System Tumours; IARC: Lyon, France, 2019; pp. 16–19. [Google Scholar]
- Patel, Y.C. Somatostatin and Its Receptor Family. Front. Neuroendocr. 1999, 20, 157–198. [Google Scholar] [CrossRef]
- Weckbecker, G.; Lewis, I.; Albert, R.; Schmid, H.A.; Hoyer, D.; Bruns, C. Opportunities in somatostatin research: Biological, chemical and therapeutic aspects. Nat. Rev. Drug Discov. 2003, 2, 999–1017. [Google Scholar] [CrossRef]
- Krenning, E.; Breeman, W.; Kooij, P.; Lameris, J.; Bakker, W.; Koper, J.; Ausema, L.; Reubi, J.; Lamberts, S. Localisation of Endocrine-Related Tumours with Radioiodinated Analogue of Somatostatin. Lancet 1989, 333, 242–244. [Google Scholar] [CrossRef] [PubMed]
- Heiman, M.L.; Murphy, W.A.; Coy, D.H. Differential binding of somatostatin agonists to somatostatin receptors in brain and ade-nohypophysis. Neuroendocrinology 1987, 45, 429–436. [Google Scholar] [CrossRef]
- Eychenne, R.; Bouvry, C.; Bourgeois, M.; Loyer, P.; Benoist, E.; Lepareur, N. Overview of Radiolabeled Somatostatin Analogs for Cancer Imaging and Therapy. Molecules 2020, 25, 4012. [Google Scholar] [CrossRef]
- Mikołajczak, R.; Maecke, H.R. Radiopharmaceuticals for somatostatin receptor imaging. Nucl. Med. Rev. 2016, 19, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Virgolini, I.; Ambrosini, V.; Bomanji, J.B.; Baum, R.P.; Fanti, S.; Gabriel, M.; Papathanasiou, N.D.; Pepe, G.; Oyen, W.; De Cristoforo, C.; et al. Procedure guidelines for PET/CT tumour imaging with 68Ga-DOTA-conjugated peptides: 68Ga-DOTA-TOC, 68Ga-DOTA-NOC, 68Ga-DOTA-TATE. Eur. J. Nucl. Med. Mol. Imaging 2010, 37, 2004–2010. [Google Scholar] [CrossRef]
- Hofmann, M.; Maecke, H.; Börner, A.; Weckesser, E.; Schöffski, P.; Oei, M.; Schumacher, J.; Henze, M.; Heppeler, A.; Meyer, J.; et al. Biokinetics and imaging with the somatostatin receptor PET radioligand 68Ga-DOTATOC: Preliminary data. Eur. J. Nucl. Med. 2001, 28, 1751–1757. [Google Scholar] [CrossRef] [PubMed]
- Hofman, M.S.; Lau, W.F.; Hicks, R.J. Somatostatin receptor imaging with 68Ga DOTATATE PET/CT: Clinical utility, normal patterns, pearls, and pitfalls in interpretation. Radiographics 2015, 35, 500–516. [Google Scholar] [CrossRef] [PubMed]
- Wild, D.; Mäcke, H.R.; Waser, B.; Reubi, J.C.; Ginj, M.; Rasch, H.; Müller-Brand, J.; Hofmann, M. 68Ga-DOTANOC: A first compound for PET imaging with high affinity for somatostatin receptor subtypes 2 and 5. Eur. J. Nucl. Med. Mol. Imaging 2004, 32, 724. [Google Scholar] [CrossRef]
- Poeppel, T.D.; Binse, I.; Petersenn, S.; Lahner, H.; Schott, M.; Antoch, G.; Brandau, W.; Bockisch, A.; Boy, C. 68Ga-DOTATOC versus 68Ga-DOTATATE PET/CT in functional imaging of neuroendocrine tumors. J. Nucl. Med. 2011, 52, 1864–1870. [Google Scholar] [CrossRef]
- Bodei, L.; Ambrosini, V.; Herrmann, K.; Modlin, I. Current Concepts in (68)Ga-DOTATATE Imaging of Neuroendocrine Neoplasms: Interpretation, Biodistribution, Dosimetry, and Molecular Strategies. J. Nucl. Med. 2017, 58, 1718–1726. [Google Scholar] [CrossRef]
- Bozkurt, M.F.; Virgolini, I.; Balogova, S.; Beheshti, M.; Rubello, D.; Decristoforo, C.; Ambrosini, V.; Kjaer, A.; Delgado-Bolton, R.; Kunikowska, J.; et al. Guideline for PET/CT imaging of neuroendocrine neoplasms with 68Ga-DOTA-conjugated somatostatin receptor targeting peptides and 18F-DOPA. Eur. J. Nucl. Med. Mol. Imaging 2017, 44, 1588–1601. [Google Scholar] [CrossRef]
- Treglia, G.; Sadeghi, R.; Giovinazzo, F.; Galiandro, F.; Annunziata, S.; Muoio, B.; Kroiss, A.S. PET with Different Radiopharmaceuticals in Neuroendocrine Neoplasms: An Umbrella Review of Published Meta-Analyses. Cancers 2021, 13, 5172. [Google Scholar] [CrossRef]
- Graham, M.M.; Gu, X.; Ginader, T.; Breheny, P.; Sunderland, J.J. 68Ga-DOTATOC Imaging of Neuroendocrine Tumors: A Systematic Review and Metaanalysis. J. Nucl. Med. 2017, 58, 1452–1458. [Google Scholar] [CrossRef]
- Gabriel, M.; Decristoforo, C.; Kendler, D.; Dobrozemsky, G.; Heute, D.; Uprimny, C.; Kovacs, P.; Von Guggenberg, E.; Bale, R.; Virgolini, I.J. 68Ga-DOTA-Tyr3-Octreotide PET in Neuroendocrine Tumors: Comparison with Somatostatin Receptor Scintigraphy and CT. J. Nucl. Med. 2007, 48, 508–518. [Google Scholar] [CrossRef]
- Putzer, D.; Gabriel, M.; Henninger, B.; Kendler, D.; Uprimny, C.; Dobrozemsky, G.; Decristoforo, C.; Bale, R.J.; Jaschke, W.; Virgolini, I.J. Bone Metastases in Patients with Neuroendocrine Tumor: 68Ga-DOTA-Tyr3-Octreotide PET in Comparison to CT and Bone Scintigraphy. J. Nucl. Med. 2009, 50, 1214–1221. [Google Scholar] [CrossRef]
- Hou, J.; Long, T.; He, Z.; Zhou, M.; Yang, N.; Chen, D.; Zeng, S.; Hu, S. Evaluation of (18)F-AlF-NOTA octreotide for imaging neuro-endocrine neoplasms: Comparison with (68)Ga-DOTATATE PET/CT. EJNMMI Res. 2021, 11, 55. [Google Scholar] [CrossRef]
- Long, T.; Yang, N.; Zhou, M.; Chen, D.; Li, Y.; Li, J.; Tang, Y.; Liu, Z.; Li, Z.; Hu, S. Clinical Application of 18F-AlF-NOTA-Octreotide PET/CT in Combination With 18F-FDG PET/CT for Imaging Neuroendocrine Neoplasms. Clin. Nucl. Med. 2019, 44, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Waldmann, C.M.; Stuparu, A.D.; van Dam, R.M.; Slavik, R. The Search for an Alternative to [68Ga]Ga-DOTA-TATE in Neuroendocrine Tumor Theranostics: Current State of 18F-labeled Somatostatin Analog Development. Theranostics 2019, 9, 1336–1347. [Google Scholar] [CrossRef]
- Laverman, P.; McBride, W.J.; Sharkey, R.M.; Eek, A.; Joosten, L.; Oyen, W.J.; Goldenberg, D.M.; Boerman, O.C. A Novel Facile Method of Labeling Octreotide with 18F-Fluorine. J. Nucl. Med. 2010, 51, 454–461. [Google Scholar] [CrossRef] [PubMed]
- Laverman, P.; D’souza, C.A.; Eek, A.; McBride, W.J.; Sharkey, R.M.; Oyen, W.J.G.; Goldenberg, D.M.; Boerman, O.C. Optimized labeling of NOTA-conjugated octreotide with F-18. Tumor Biol. 2011, 33, 427–434. [Google Scholar] [CrossRef] [PubMed]
- Leyton, J.; Iddon, L.; Perumal, M.; Indrevoll, B.; Glaser, M.; Robins, E.; George, A.J.T.; Cuthbertson, A.; Luthra, S.K.; Aboagye, E.O. Targeting somatostatin receptors: Preclinical evaluation of novel 18F fluoroethyltria-zole-Tyr3-octreotate analogs for PET. J. Nucl. Med. 2011, 52, 1441–1448. [Google Scholar] [CrossRef]
- Delpassand, E.S.; Ranganathan, D.; Wagh, N.; Shafie, A.; Gaber, A.; Abbasi, A.; Kjaer, A.; Tworowska, I.; Núñez, R. 64Cu-DOTATATE PET/CT for Imaging Patients with Known or Suspected Somatostatin Receptor-Positive Neuroendocrine Tumors: Results of the First U.S. Prospective, Reader-Masked Clinical Trial. J. Nucl. Med. 2020, 61, 890–896. [Google Scholar] [CrossRef] [PubMed]
- Sadowski, S.M.; Millo, C.; Neychev, V.; Aufforth, R.; Keutgen, X.; Glanville, J.; Alimchandani, M.; Nilubol, N.; Herscovitch, P.; Quezado, M.; et al. Feasibility of radio-guided surgery with 68gallium DOTATATE in patients with gas-tro-entero-pancreatic neuroendocrine tumors. Ann. Surg. Oncol. 2015, 22, 676–682. [Google Scholar] [CrossRef] [PubMed]
- Wild, D.; Fani, M.; Fischer, R.; Del Pozzo, L.; Kaul, F.; Krebs, S.; Fischer, R.; Rivier, J.E.F.; Reubi, J.C.; Maecke, H.R.; et al. Comparison of Somatostatin Receptor Agonist and Antagonist for Peptide Receptor Radionuclide Therapy: A Pilot Study. J. Nucl. Med. 2014, 55, 1248–1252. [Google Scholar] [CrossRef] [PubMed]
- Wild, D.; Fani, M.; Behe, M.; Brink, I.; Rivier, J.E.; Reubi, J.C.; Maecke, H.R.; Weber, W.A. First Clinical Evidence That Imaging with Somatostatin Receptor Antagonists Is Feasible. J. Nucl. Med. 2011, 52, 1412–1417. [Google Scholar] [CrossRef]
- Fani, M.; Nicolas, G.P.; Wild, D. Somatostatin Receptor Antagonists for Imaging and Therapy. J. Nucl. Med. 2017, 58 (Suppl. 2), 61S–66S. [Google Scholar] [CrossRef]
- Nicolas, G.P.; Schreiter, N.; Kaul, F.; Uiters, J.; Bouterfa, H.; Kaufmann, J.; Erlanger, T.E.; Cathomas, R.; Christ, E.; Fani, M.; et al. Sensitivity Comparison of Ga OPS202 and Ga-DOTATOC PET/CT in Patients with Gastroenteropancreatic Neuroendocrine Tumors: A Prospective Phase II Imaging Study. J. Nucl. Med. 2018, 59, 915–921. [Google Scholar] [CrossRef]
- Nicolas, G.P.; Beykan, S.; Bouterfa, H.; Kaufmann, J.; Bauman, A.; Lassmann, M.; Reubi, J.C.; Rivier, J.E.F.; Maecke, H.R.; Fani, M.; et al. Safety, Biodistribution, and Radiation Dosimetry of Ga-OPS202 in Patients with Gastroenteropancreatic Neuroendocrine Tumors: A Prospective Phase I Imaging Study. J. Nucl. Med. 2018, 59, 909–914. [Google Scholar] [CrossRef]
- Hope, T.A.; Bergsland, E.K.; Bozkurt, M.F.; Graham, M.; Heaney, A.P.; Herrmann, K.; Howe, J.; Kulke, M.H.; Kunz, P.L.; Mailman, J.; et al. Appropriate Use Criteria for Somatostatin Receptor PET Imaging in Neuroendocrine Tumors. J. Nucl. Med. 2017, 59, 66–74. [Google Scholar] [CrossRef]
- Hendel, R.C.; Patel, M.R.; Allen, J.M.; Min, J.K.; Shaw, L.J.; Wolk, M.J.; Douglas, P.S.; Kramer, C.M.; Stainback, R.F.; Bailey, S.R.; et al. Appropriate use of cardiovascular technology: 2013 ACCF appropriate use criteria methodology update: A report of the American College of Cardiology Foundation appropriate use criteria task force. J. Am. Coll. Cardiol. 2013, 61, 1305–1317. [Google Scholar] [CrossRef]
- Barrio, M.; Czernin, J.; Fanti, S.; Ambrosini, V.; Binse, I.; Du, L.; Eiber, M.; Herrmann, K.; Fendler, W.P. The Impact of Somatostatin Receptor–Directed PET/CT on the Management of Patients with Neuroendocrine Tumor: A Systematic Review and Meta-Analysis. J. Nucl. Med. 2017, 58, 756–761. [Google Scholar] [CrossRef]
- Bauckneht, M.; Albano, D.; Annunziata, S.; Santo, G.; Guglielmo, P.; Frantellizzi, V.; Branca, A.; Ferrari, C.; Vento, A.; Mirabile, A.; et al. Somatostatin Receptor PET/CT Imaging for the Detection and Staging of Pancreatic NET: A Systematic Review and Meta-Analysis. Diagnostics 2020, 10, 598. [Google Scholar] [CrossRef] [PubMed]
- Geijer, H.; Breimer, L.H. Somatostatin receptor PET/CT in neuroendocrine tumours: Update on systematic review and me-ta-analysis. Eur. J. Nucl. Med. Mol. Imaging 2013, 40, 1770–1780. [Google Scholar] [CrossRef]
- Kazmierczak, P.M.; Rominger, A.; Wenter, V.; Spitzweg, C.; Auernhammer, C.; Angele, M.K.; Rist, C.; Cyran, C.C. The added value of 68Ga-DOTA-TATE-PET to contrast-enhanced CT for primary site detection in CUP of neuroendocrine origin. Eur. Radiol. 2016, 27, 1676–1684. [Google Scholar] [CrossRef] [PubMed]
- Mayerhoefer, M.E.; Schuetz, M.; Magnaldi, S.; Weber, M.; Trattnig, S.; Karanikas, G. Are contrast media required for (68)Ga-DOTATOC PET/CT in patients with neuroendocrine tumours of the abdomen? Eur. Radiol. 2012, 22, 938–946. [Google Scholar] [CrossRef]
- Oien, K.A. Pathologic Evaluation of Unknown Primary Cancer. Semin. Oncol. 2009, 36, 8–37. [Google Scholar] [CrossRef] [PubMed]
- Pavel, M.; O’Toole, D.; Costa, F.; Capdevila, J.; Gross, D.; Kianmanesh, R.; Krenning, E.; Knigge, U.; Salazar, R.; Pape, U.-F.; et al. ENETS Consensus Guidelines Update for the Management of Distant Metastatic Disease of Intestinal, Pancreatic, Bronchial Neuroendocrine Neoplasms (NEN) and NEN of Unknown Primary Site. Neuroendocrinology 2016, 103, 172–185. [Google Scholar] [CrossRef]
- Alexandraki, K.; Angelousi, A.; Boutzios, G.; Kyriakopoulos, G.; Rontogianni, D.; Kaltsas, G. Management of neuroendocrine tumors of unknown primary. Rev. Endocr. Metab. Disord. 2017, 18, 423–431. [Google Scholar] [CrossRef]
- Ma, H.; Kan, Y.; Yang, J.-G. Clinical value of 68Ga-DOTA-SSTR PET/CT in the diagnosis and detection of neuroendocrine tumors of unknown primary origin: A systematic review and meta-analysis. Acta Radiol. 2020, 62, 1217–1228. [Google Scholar] [CrossRef]
- Sampathirao, N.; Basu, S. MIB-1 Index–Stratified Assessment of Dual-Tracer PET/CT with 68Ga-DOTATATE and 18F-FDG and Multimodality Anatomic Imaging in Metastatic Neuroendocrine Tumors of Unknown Primary in a PRRT Workup Setting. J. Nucl. Med. Technol. 2017, 45, 34–41. [Google Scholar] [CrossRef]
- Oberg, K.; Knigge, U.; Kwekkeboom, D.; Perren, A. ESMO Guidelines Working Group. Neuroendocrine gastro-entero-pancreatic tumors: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2012, 23 (Suppl. 7), vii124–vii130. [Google Scholar] [CrossRef]
- Kumar, R.; Sharma, P.; Garg, P.; Karunanithi, S.; Naswa, N.; Sharma, R.; Thulkar, S.; Lata, S.; Malhotra, A. Role of 68Ga-DOTATOC PET-CT in the diagnosis and staging of pancreatic neuroendocrine tumours. Eur. Radiol. 2011, 21, 2408–2416. [Google Scholar] [CrossRef]
- Treglia, G.; Castaldi, P.; Rindi, G.; Giordano, A.; Rufini, V. Diagnostic performance of Gallium-68 somatostatin receptor PET and PET/CT in patients with thoracic and gastroenteropancreatic neuroendocrine tumours: A meta-analysis. Endocrine 2012, 42, 80–87. [Google Scholar] [CrossRef]
- Miederer, M.; Seidl, S.; Buck, A.; Scheidhauer, K.; Wester, H.-J.; Schwaiger, M.; Perren, A. Correlation of immunohistopathological expression of somatostatin receptor 2 with stand-ardised uptake values in 68Ga-DOTATOC PET/CT. Eur. J. Nucl. Med. Mol. Imaging 2009, 36, 48–52. [Google Scholar] [CrossRef]
- Sorbye, H.; Strosberg, J.; Baudin, E.; Klimstra, D.S.; Yao, J.C. Gastroenteropancreatic high-grade neuroendocrine carcinoma. Cancer 2014, 120, 2814–2823. [Google Scholar] [CrossRef] [PubMed]
- Alexandraki, K.I.; Kaltsas, G. Gastroenteropancreatic neuroendocrine tumors: New insights in the diagnosis and therapy. Endocrine 2011, 41, 40–52. [Google Scholar] [CrossRef]
- Fine, R.L.; Gulati, A.P.; Krantz, B.A.; Moss, R.A.; Schreibman, S.; Tsushima, D.A.; Mowatt, K.B.; Dinnen, R.D.; Mao, Y.; Stevens, P.D.; et al. Capecitabine and temozolomide (CAPTEM) for metastatic, well-differentiated neuroen-docrine cancers: The Pancreas Center at Columbia University experience. Cancer Chemother. Pharmacol. 2013, 71, 663–670. [Google Scholar] [CrossRef] [PubMed]
- Squires, M.H.; Adsay, V.; Schuster, D.; Russell, M.C.; Cardona, K.; Delman, K.A.; Winer, J.H.; Altinel, D.; Sarmiento, J.M.; El-Rayes, B.; et al. Octreoscan Versus FDG-PET for Neuroendocrine Tumor Staging: A Biological Approach. Ann. Surg. Oncol. 2015, 22, 2295–2301. [Google Scholar] [CrossRef] [PubMed]
- Moertel, C.G.; Kvols, L.K.; O’Connell, M.J.; Rubin, J. Treatment of neuroendocrine carcinomas with combined etoposide and cisplatin: Evidence of major therapeutic activity in the anaplastic variants of these neoplasms. Cancer 1991, 68, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Kwekkeboom, D.J.; de Herder, W.W.; Kam, B.L.; van Eijck, C.H.; van Essen, M.; Kooij, P.P.; Feelders, R.A.; van Aken, M.O.; Krenning, E.P. Treatment with the radiolabeled somato- statin analog [177 Lu-DOTA 0, Tyr3]octreotate: Toxicity, efficacy, and survival. J. Clin. Oncol. 2008, 26, 2124–2130. [Google Scholar] [CrossRef]
- Kim, H.S.; Lee, H.S.; Kim, W.H. Clinical significance of protein expression of cyclooxygenase-2 and somatostatin receptors in gas-troenteropancreatic neuroendocrine tumors. Cancer Res. Treat. 2011, 43, 181–188. [Google Scholar] [CrossRef]
- Asnacios, A.; Courbon, F.; Rochaix, P.; Bauvin, E.; Cances-Lauwers, V.; Susini, C.; Schulz, S.; Boneu, A.; Guimbaud, R.; Buscail, L. Indium-111-pentetreotide scintigraphy and somato- statin receptor subtype 2 ex-pression: New prognostic factors for malignant well-differentiated endocrine tumors. J. Clin. Oncol. 2008, 26, 963–970. [Google Scholar] [CrossRef] [PubMed]
- Strosberg, J.R.; Wolin, E.M.; Chasen, B.; Kulke, M.H.; Bushnell, D.L.; Caplin, M.E.; Baum, R.P.; Kunz, P.L.; Hobday, T.J.; Hendifar, A.E.; et al. NETTER-1 phase III: Progression-free survival, radiographic response, and preliminary overall survival results in patients with midgut neuroendocrine tumors treated with 177-Lu-Dotatate. J. Clin. Oncol. 2016, 34, 194. [Google Scholar] [CrossRef]
- Kunikowska, J.; Królicki, L.; Hubalewska-Dydejczyk, A.; Mikołajczak, R.; Sowa-Staszczak, A.; Pawlak, D. Clinical results of radionuclide therapy of neuroendocrine tumours with 90Y-DOTATATE and tan- dem 90Y/177Lu-DOTATATE: Which is a better therapy option? Eur. J. Nucl. Med. Mol. Imaging 2011, 38, 1788–1797. [Google Scholar] [CrossRef]
- Refardt, J.; Zandee, W.T.; Brabander, T.; Feelders, R.A.; Franssen, G.J.H.; Hofland, L.J.; Christ, E.; De Herder, W.W.; Hofland, J. Inferior outcome of neuroendocrine tumor patients negative on somatostatin receptor imaging. Endocr. Relat. Cancer 2020, 27, 615–624. [Google Scholar] [CrossRef]
- Hou, J.; Yang, Y.; Chen, N.; Chen, D.; Hu, S. Prognostic Value of Volume-Based Parameters Measured by SSTR PET/CT in Neuro-endocrine Tumors: A Systematic Review and Meta-Analysis. Front. Med. 2021, 8, 771912. [Google Scholar] [CrossRef]
- Nagtegaal, I.D.; Odze, R.D.; Klimstra, D.; Paradis, V.; Rugge, M.; Schirmacher, P.; Washington, K.M.; Carneiro, F.; Cree, I.A.; The WHO Classification of Tumours Editorial Board. The 2019 WHO classification of tumours of the digestive system. Histopathology 2020, 76, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Botling, J.; Lamarca, A.; Bajic, D.; Norlén, O.; Lönngren, V.; Kjaer, J.; Eriksson, B.; Welin, S.; Hellman, P.; Rindi, G.; et al. High-Grade Progression Confers Poor Survival in Pancreatic Neuroendocrine Tumors. Neuroendocrinology 2019, 110, 891–898. [Google Scholar] [CrossRef]
- Bahri, H.; Laurence, L.; Edeline, J.; Leghzali, H.; Devillers, A.; Raoul, J.-L.; Cuggia, M.; Mesbah, H.; Clement, B.; Boucher, E.; et al. High Prognostic Value of 18F-FDG PET for Metastatic Gastroenteropancreatic Neuroendocrine Tumors: A Long-Term Evaluation. J. Nucl. Med. 2014, 55, 1786–1790. [Google Scholar] [CrossRef]
- Binderup, T.; Knigge, U.; Johnbeck, C.B.; Loft, A.; Berthelsen, A.K.; Oturai, P.; Mortensen, J.; Federspiel, B.; Langer, S.W.; Kjaer, A. 18F-FDG PET is superior to WHO grading as a prognostic tool in neuroendocrine neo-plasms and useful in guiding PRRT: A prospective 10-year follow-up study. J. Nucl. Med. 2021, 62, 808–815. [Google Scholar] [CrossRef]
- Campana, D.; Ambrosini, V.; Pezzilli, R.; Fanti, S.; Labate, A.M.M.; Santini, D.; Ceccarelli, C.; Nori, F.; Franchi, R.; Corinaldesi, R.; et al. Standardized Uptake Values of 68Ga-DOTANOC PET: A Promising Prognostic Tool in Neuroendocrine Tumors. J. Nucl. Med. 2010, 51, 353–359. [Google Scholar] [CrossRef]
- Haug, A.R.; Auernhammer, C.J.; Wängler, B.; Schmidt, G.P.; Uebleis, C.; Göke, B.; Cumming, P.; Bartenstein, P.; Tiling, R.; Hacker, M. 68Ga-DOTATATE PET/CT for the Early Prediction of Response to Somatostatin Receptor–Mediated Radionuclide Therapy in Patients with Well-Differentiated Neuroendocrine Tumors. J. Nucl. Med. 2010, 51, 1349–1356. [Google Scholar] [CrossRef]
- Sharma, R.; Wang, W.M.; Yusuf, S.; Evans, J.; Ramaswami, R.; Wernig, F.; Frilling, A.; Mauri, F.; Nahhas, A.; Aboagye, E.; et al. 68Ga-DOTATATE PET/CT parameters predict response to peptide receptor radionuclide therapy in neuroendocrine tumours. Radiother. Oncol. 2019, 141, 108–115. [Google Scholar] [CrossRef]
- Chan, D.L.; Pavlakis, N.; Schembri, G.P.; Bernard, E.J.; Hsiao, E.; Hayes, A.; Barnes, T.; Diakos, C.; Khasraw, M.; Samra, J.; et al. Dual Somatostatin Receptor/FDG PET/CT Imaging in Metastatic Neuroendocrine Tumours: Proposal for a Novel Grading Scheme with Prognostic Significance. Theranostics 2017, 7, 1149–1158. [Google Scholar] [CrossRef]
- Karfis, I.; Marin, G.; Levillain, H.; Drisis, S.; Muteganya, R.; Critchi, G.; Taraji-Schiltz, L.; Guix, C.A.; Shaza, L.; Elbachiri, M.; et al. Prognostic value of a three-scale grading system based on combining molecular imaging with 68Ga-DOTATATE and 18F-FDG PET/CT in patients with metastatic gastroenteropancreatic neuroendocrine neoplasias. Oncotarget 2020, 11, 589–599. [Google Scholar] [CrossRef] [PubMed]
- Chan, D.L.; Hayes, A.R.; Karfis, I.; Conner, A.; O’Mahony, L.F.; Mileva, M.; Bernard, E.; Roach, P.; Marin, G.; Pavlakis, N.; et al. Dual [68Ga]DOTATATE and [18F]FDG PET/CT in patients with metastatic gastroentero-pancreatic neuroendocrine neoplasms: A multicentre validation of the NETPET score. Br. J. Cancer 2023, 128, 549–555. [Google Scholar] [CrossRef]
- Basu, S.; Ranade, R.; Ostwal, V.; Shrikhande, S.V. PET-Based Molecular Imaging in Designing Personalized Management Strategy in Gastroenteropancreatic Neuroendocrine Tumors. PET Clin. 2016, 11, 233–241. [Google Scholar] [CrossRef]
- Adnan, A.; Basu, S. Discordance Between Histopathologic Grading and Dual-Tracer PET/CT Findings in Metastatic NETs and Outcome of 177Lu-DOTATATE PRRT: Does In Vivo Molecular PET Perform Better from the Viewpoint of Prediction of Tumor Biology? J. Nucl. Med. Technol. 2021, 50, 248–255. [Google Scholar] [CrossRef]
- Kuyumcu, S.; Özkan, Z.G.; Sanli, Y.; Yilmaz, E.; Mudun, A.; Adalet, I.; Unal, S. Physiological and tumoral uptake of 68Ga-DOTATATE: Standardized uptake values and challenges in interpretation. Ann. Nucl. Med. 2013, 27, 538–545. [Google Scholar] [CrossRef]
- Mapelli, P.; Tam, H.H.; Sharma, R.; Aboagye, E.; Al-Nahhas, A. Frequency and significance of physiological versus pathological uptake of 68Ga-DOTATATE in the pancreas: Validation with morphological imaging. Nucl. Med. Commun. 2014, 35, 613–619. [Google Scholar] [CrossRef] [PubMed]
- Gugger, M.; Waser, B.; Kappeler, A.; Schonbrunn, A.; Reubi, J.C. Immunohistochemical Localization of Somatostatin Receptor sst2A in Human Gut and Lung Tissue: Possible Implications for Physiology and Carcinogenesis. Ann. N. Y. Acad. Sci. 2004, 1014, 132–136. [Google Scholar] [CrossRef] [PubMed]
- Shastry, M.; Kayani, I.; Wild, D.; Caplin, M.; Visvikis, D.; Gacinovic, S.; Reubi, J.C.; Bomanji, J.B. Distribution pattern of 68Ga-DOTATATE in disease-free patients. Nucl. Med. Commun. 2010, 31, 1025–1032. [Google Scholar] [CrossRef] [PubMed]
- Reubi, J.C.; Horisberger, U.; Studer, U.E.; Waser, B.; Laissue, J.A. Human kidney as target for somatostatin: High affinity receptors in tubules and vasa recta. J. Clin. Endocrinol. Metab. 1993, 77, 1323–1328. [Google Scholar] [CrossRef] [PubMed]
- Theodoropoulou, M.; Stalla, G.K. Somatostatin receptors: From signaling to clinical practice. Front. Neuroendocr. 2013, 34, 228–252. [Google Scholar] [CrossRef] [PubMed]
- Bentestuen, M.; Gossili, F.; Almasi, C.E.; Zacho, H.D. Prevalence and significance of incidental findings on 68 Ga-DOTA-conjugated somatostatin receptor-targeting peptide PET/CT: A systematic review of the literature. Cancer Imaging 2022, 22, 44. [Google Scholar] [CrossRef]
- Balogova, S.; Talbot, J.-N.; Nataf, V.; Michaud, L.; Huchet, V.; Kerrou, K.; Montravers, F. 18F-fluorodihydroxyphenylalanine vs other radiopharmaceuticals for imaging neuroen-docrine tumours according to their type. Eur. J. Nucl. Med. Mol. Imaging 2013, 40, 943–966. [Google Scholar] [CrossRef]
- Ambrosini, V.; Tomassetti, P.; Castellucci, P.; Campana, D.; Montini, G.; Rubello, D.; Nanni, C.; Rizzello, A.; Franchi, R.; Fanti, S. Comparison between 68Ga-DOTA-NOC and 18F-DOPA PET for the detection of gastro-entero-pancreatic and lung neuro-endocrine tumours. Eur. J. Nucl. Med. Mol. Imaging 2008, 35, 1431–1438. [Google Scholar] [CrossRef]
- Putzer, D.; Gabriel, M.; Kendler, D.; Henninger, B.; Knoflach, M.; Kroiss, A.; Vonguggenberg, E.; Warwitz, B.; Virgolini, I.J. Comparison of (68)Ga-DOTA-Tyr(3)-octreotide and (18)F-fluoro-L-dihydroxyphenylalanine positron emission tomography in neuroendocrine tumor patients. Q. J. Nucl. Med. Mol. Imaging 2010, 54, 68–75. [Google Scholar]
- Rasul, S.; Hartenbach, S.; Rebhan, K.; Göllner, A.; Karanikas, G.; Mayerhoefer, M.; Mazal, P.; Hacker, M.; Hartenbach, M. [18F]DOPA PET/ceCT in diagnosis and staging of primary medullary thyroid carcinoma prior to surgery. Eur. J. Nucl. Med. Mol. Imaging 2018, 45, 2159–2169. [Google Scholar] [CrossRef]
- Houseni, M.; Chamroonrat, W.; Zhuang, H.; Hernandez-Pampolini, M.; Alavi, A. Fluorine-18 DOPA-PET and PET/CT Imaging in Congenital Hyperinsulinism. PET Clin. 2008, 3, 577–585. [Google Scholar] [CrossRef]
- Kroiss, A.S.; Uprimny, C.; Shulkin, B.L.; Frech, A.; Tilg, H.; Gasser, R.W.; Sprinzl, G.M.; Gruber, L.; Thomé, C.; Plangger, C.; et al. Compared to (123)I-MIBG SPECT/CT, (18)F-DOPA PET/CT provides accurate tumor extent in patients with extra- adrenal paraganglioma. Ann. Nucl. Med. 2017, 31, 357–365. [Google Scholar] [CrossRef]
- Reubi, J.C.; Waser, B. Concomitant expression of several peptide receptors in neuroendocrine tumours: Molecular basis for in vivo multireceptor tumour targeting. Eur. J. Nucl. Med. Mol. Imaging 2003, 30, 781–793. [Google Scholar] [CrossRef]
- Baggio, L.L.; Drucker, D.J. Biology of Incretins: GLP-1 and GIP. Gastroenterology 2007, 132, 2131–2157. [Google Scholar] [CrossRef] [PubMed]
- Antwi, K.; Fani, M.; Heye, T.; Nicolas, G.; Rottenburger, C.; Kaul, F.; Merkle, E.; Zech, C.J.; Boll, D.; Vogt, D.R.; et al. Comparison of glucagon-like peptide-1 receptor (GLP-1R) PET/CT, SPECT/CT and 3T MRI for the localisation of occult insulinomas: Evaluation of diagnostic accuracy in a prospective crossover imaging study. Eur. J. Nucl. Med. Mol. Imaging 2018, 45, 2318–2327. [Google Scholar] [CrossRef] [PubMed]
- Wild, D.; Christ, E.; Caplin, M.E.; Kurzawinski, T.R.; Forrer, F.; Brändle, M.; Seufert, J.; Weber, W.A.; Bomanji, J.; Perren, A.; et al. Glucagon-Like Peptide-1 Versus Somatostatin Receptor Targeting Reveals 2 Distinct Forms of Malignant Insulinomas. J. Nucl. Med. 2011, 52, 1073–1078. [Google Scholar] [CrossRef] [PubMed]
- Blažević, A.; Hofand, J.; Hofand, L.J.; Feelders, R.A.; de Herder, W.W. Small intestinal neuroendocrine tumours and fbrosis: An entangled conundrum. Endocr. Relat. Cancer 2018, 25, R115–R130. [Google Scholar] [CrossRef]
- Kratochwil, C.; Flechsig, P.; Lindner, T.; Abderrahim, L.; Altmann, A.; Mier, W.; Adeberg, S.; Rathke, H.; Röhrich, M.; Winter, H.; et al. 68Ga-FAPI PET/CT: Tracer Uptake in 28 Different Kinds of Cancer. J. Nucl. Med. 2019, 60, 801–805. [Google Scholar] [CrossRef]
- Giesel, F.L.; Kratochwil, C.; Lindner, T.; Marschalek, M.M.; Loktev, A.; Lehnert, W.; Debus, J.; Jäger, D.; Flechsig, P.; Altmann, A.; et al. 68Ga-FAPI PET/CT: Biodistribution and Preliminary Dosimetry Estimate of 2 DOTA-Containing FAP-Targeting Agents in Patients with Various Cancers. J. Nucl. Med. 2018, 60, 386–392. [Google Scholar] [CrossRef]
- Kaemmerer, D.; Reimann, C.; Specht, E.; Wirtz, R.M.; Sayeg, M.; Baum, R.P.; Schulz, S.; Lupp, A. Differential expression and prognostic value of the chemokine receptor CXCR4 in bronchopulmonary neuroendocrine neoplasms. Oncotarget 2014, 6, 3346–3358. [Google Scholar] [CrossRef] [PubMed]
- Kaemmerer, D.; Träger, T.; Hoffmeister, M.; Sipos, B.; Hommann, M.; Sänger, J.; Schulz, S.; Lupp, A. Inverse expression of somatostatin and CXCR4 chemokine receptors in gas-troenteropancreatic neuroendocrine neoplasms of different malignancy. Oncotarget 2015, 6, 27566–27579. [Google Scholar] [CrossRef]
- Werner, R.A.; Weich, A.; Higuchi, T.; Schmid, J.S.; Schirbel, A.; Lassmann, M.; Wild, V.; Rudelius, M.; Kudlich, T.; Herrmann, K.; et al. Imaging of Chemokine Receptor 4 Expression in Neuroendocrine Tumors—A Triple Tracer Comparative Approach. Theranostics 2017, 7, 1489–1498. [Google Scholar] [CrossRef]
- Gourni, E.; Waser, B.; Clerc, P.; Fourmy, D.; Reubi, J.C.; Maecke, H.R. The glucose-dependent insulinotropic polypeptide receptor: A novel target for neuroendocrine tumor imaging-frst preclinical studies. J. Nucl. Med. 2014, 55, 976–982. [Google Scholar] [CrossRef]
- Reubi, J.C.; Schaer, J.C.; Waser, B. Cholecystokinin(CCK)-A and CCK-B/gastrin receptors in human tumors. Cancer Res. 1997, 57, 1377–1386. [Google Scholar] [PubMed]
- Kunikowska, J.; Ziemnicka, K.; Pawlak, D.; Ruchała, M.; Kolasa, A.; Janicka-Jedyńska, M.; Woźniak, A.; Mikołajczak, R.; Królicki, L. Medullary thyroid carcinoma—PET/ CT imaging with 68Ga-labelled gastrin and somatostatin analogues. Endokrynol. Pol. 2016, 67, 68–71. [Google Scholar] [CrossRef] [PubMed]
- Rottenburger, C.; Nicolas, G.P.; McDougall, L.; Kaul, F.; Cachovan, M.; Vija, A.H.; Schibli, R.; Geistlich, S.; Schumann, A.; Rau, T.; et al. Cholecystokinin 2 Receptor Agonist (177) Lu-PP-F11N for Radionuclide Therapy of Medullary Thyroid Carcinoma: Results of the Lumed Phase 0a Study. J. Nucl. Med. 2020, 61, 520–526. [Google Scholar] [CrossRef] [PubMed]
- Gu, D.; Hu, Y.; Ding, H.; Wei, J.; Chen, K.; Liu, H.; Zeng, M.; Tian, J. CT radiomics may predict the grade of pancreatic neuroendocrine tumors: A multicenter study. Eur. Radiol. 2019, 29, 6880–6890. [Google Scholar] [CrossRef]
- Guo, C.; Zhuge, X.; Wang, Q.; Xiao, W.; Wang, Z.; Wang, Z.; Feng, Z.; Chen, X. The differentiation of pancreatic neuroendocrine carcinoma from pancreatic ductal adenocar-cinoma: The values of CT imaging features and texture analysis. Cancer Imaging 2018, 18, 37. [Google Scholar] [CrossRef]
- Liang, W.; Yang, P.; Huang, R.; Xu, L.; Wang, J.; Liu, W.; Zhang, L.; Wan, D.; Huang, Q.; Lu, Y.; et al. A combined nomogram model to preoperatively predict histologic grade in pancreatic neu-roendocrine tumors. Clin. Cancer Res. 2019, 25, 584–594. [Google Scholar] [CrossRef]


| Scenario No. | Description | Appropriateness | Score |
|---|---|---|---|
| 1 | Initial staging after histologic diagnosis of NETs | Appropriate | 9 |
| 2 | Localization of primary tumor in patients with known metastatic disease but unknown primary | Appropriate | 9 |
| 3 | Selection of patients for SSTR-targeted PRRT | Appropriate | 9 |
| 4 | Staging NETs before planned surgery | Appropriate | 8 |
| 5 | Evaluation of mass suggestive of NET not amenable to endoscopic or percutaneous biopsy (e.g., ileal lesion, hypervascular pancreatic mass, mesenteric mass) | Appropriate | 8 |
| 6 | Monitoring of NETs seen predominantly on SSTR PET | Appropriate | 8 |
| 7 | Evaluation of patients with biochemical evidence and symptoms of NET without evidence on CI and without prior histologic diagnosis of NET | Appropriate | 7 |
| 8 | Restaging at time of clinical or laboratory progression without progression on CI | Appropriate | 7 |
| 9 | New indeterminate lesion on CI, with unclear progression | Appropriate | 7 |
| 10 | Restaging of patients with NETs at initial follow-up after resection with curative intent | May be appropriate | 6 |
| 11 | Selection of patients with nonfunctional NETs for SSA treatment | May be appropriate | 6 |
| 12 | Monitoring in patients with NETs seen on both CI and SSTR PET with active disease and no clinical evidence of progression | May be appropriate | 5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adnan, A.; Basu, S. Somatostatin Receptor Targeted PET-CT and Its Role in the Management and Theranostics of Gastroenteropancreatic Neuroendocrine Neoplasms. Diagnostics 2023, 13, 2154. https://doi.org/10.3390/diagnostics13132154
Adnan A, Basu S. Somatostatin Receptor Targeted PET-CT and Its Role in the Management and Theranostics of Gastroenteropancreatic Neuroendocrine Neoplasms. Diagnostics. 2023; 13(13):2154. https://doi.org/10.3390/diagnostics13132154
Chicago/Turabian StyleAdnan, Aadil, and Sandip Basu. 2023. "Somatostatin Receptor Targeted PET-CT and Its Role in the Management and Theranostics of Gastroenteropancreatic Neuroendocrine Neoplasms" Diagnostics 13, no. 13: 2154. https://doi.org/10.3390/diagnostics13132154
APA StyleAdnan, A., & Basu, S. (2023). Somatostatin Receptor Targeted PET-CT and Its Role in the Management and Theranostics of Gastroenteropancreatic Neuroendocrine Neoplasms. Diagnostics, 13(13), 2154. https://doi.org/10.3390/diagnostics13132154





