Diagnostic Accuracy of Machine Learning AI Architectures in Detection and Classification of Lung Cancer: A Systematic Review
Abstract
1. Introduction
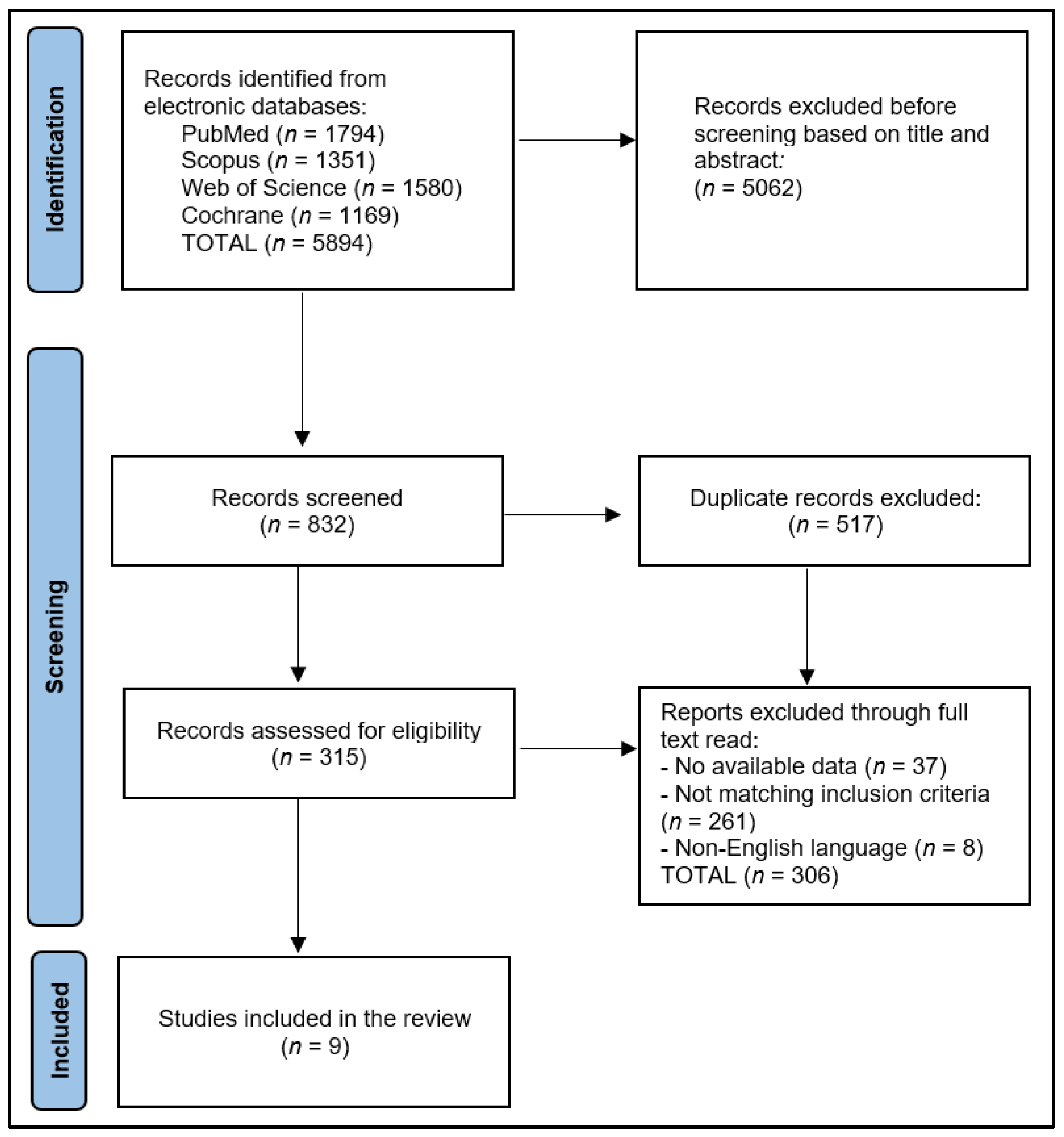
2. Materials and Methods
2.1. Review Protocol
- -
- What is the accuracy of machine learning AI algorithms in lung cancer detection?
- -
- What machine learning architectures are currently in use?
- -
- What is the clinical relevance of these diagnostic imaging methods?
2.2. Data Extraction
2.3. Study Selection and Quality Assessment
3. Results
3.1. Overview
3.2. Performance Evaluation
4. Discussion
4.1. Summary and Contributions
4.2. Study Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Thandra, K.C.; Barsouk, A.; Saginala, K.; Aluru, J.S.; Barsouk, A. Epidemiology of lung cancer. Contemp. Oncol. 2021, 25, 45–52. [Google Scholar] [CrossRef]
- Septimiu-Radu, S.; Gadela, T.; Gabriela, D.; Oancea, C.; Rosca, O.; Lazureanu, V.E.; Fericean, R.M.; Bratosin, F.; Dumitrescu, A.; Stoicescu, E.R.; et al. A Systematic Review of Lung Autopsy Findings in Elderly Patients after SARS-CoV-2 Infection. J. Clin. Med. 2023, 12, 2070. [Google Scholar] [CrossRef]
- Toma, A.-O.; Boeriu, E.; Decean, L.; Bloanca, V.; Bratosin, F.; Levai, M.C.; Vasamsetti, N.G.; Alambaram, S.; Oprisoni, A.L.; Miutescu, B.; et al. The Effects of Lack of Awareness in Age-Related Quality of Life, Coping with Stress, and Depression among Patients with Malignant Melanoma. Curr. Oncol. 2023, 30, 1516–1528. [Google Scholar] [CrossRef]
- Knight, S.B.; Phil, A.; Crosbie, P.A.; Balata, H.; Chudziak, J.; Hussell, T.; Dive, C. Progress and prospects of early detection in lung cancer. Open Biol. 2017, 7, 170070. [Google Scholar] [CrossRef]
- Tudorache, E.; Motoc, N.S.; Pescaru, C.; Crisan, A.; Ciumarnean, L. Impact of pulmonary rehabilitation programs in improving health status in COPD patients. Balneo Res. J. 2019, 10, 472–477. [Google Scholar] [CrossRef]
- Lee, S.-H.; Cho, H.-H.; Lee, H.Y.; Park, H. Clinical impact of variability on CT radiomics and suggestions for suitable feature selection: A focus on lung cancer. Cancer Imaging 2019, 19, 54. [Google Scholar] [CrossRef]
- Panunzio, A.; Sartori, P. Lung Cancer and Radiological Imaging. Curr. Radiopharm. 2020, 13, 238–242. [Google Scholar] [CrossRef]
- Albasri, A.M. A histopathological analysis of lung cancers. An 11-year retrospective study from Al-Madinah Al-Munawwarah, Saudi Arabia. Saudi Med. J. 2019, 40, 503–506. [Google Scholar] [CrossRef]
- Mambetsariev, I.; Pharaon, R.; Nam, A.; Knopf, K.; Djulbegovic, B.; Villaflor, V.M.; Vokes, E.E.; Salgia, R. Heuristic value-based framework for lung cancer decision-making. Oncotarget 2018, 9, 29877–29891. [Google Scholar] [CrossRef]
- Wu, J.; Zan, X.; Gao, L.; Zhao, J.; Fan, J.; Shi, H.; Wan, Y.; Yu, E.; Li, S.; Xie, X. A Machine Learning Method for Identifying Lung Cancer Based on Routine Blood Indices: Qualitative Feasibility Study. JMIR Public Health Surveill. 2019, 7, e13476. [Google Scholar] [CrossRef]
- Mathew, C.J.; David, A.M.; Mathew, C.M.J. Artificial Intelligence and its future potential in lung cancer screening. EXCLI J. 2020, 19, 1552–1562. [Google Scholar] [CrossRef]
- Waller, J.; O’connor, A.; Raafat, E.; Amireh, A.; Dempsey, J.; Martin, C.; Umair, M. Applications and challenges of artificial intelligence in diagnostic and interventional radiology. Pol. J. Radiol. 2022, 87, 113–117. [Google Scholar] [CrossRef]
- Sarker, I.H. AI-Based Modeling: Techniques, Applications and Research Issues Towards Automation, Intelligent and Smart Systems. SN Comput. Sci. 2022, 3, 158. [Google Scholar] [CrossRef]
- Chan, H.P.; Hadjiiski, L.M.; Samala, R.K. Computer-aided diagnosis in the era of deep learning. Med. Phys. 2020, 47, e218–e227. [Google Scholar] [CrossRef]
- Firmino, M.; Angelo, G.; Morais, H.; Dantas, M.R.; Valentim, R. Computer-aided detection (CADe) and diagnosis (CADx) system for lung cancer with likelihood of malignancy. Biomed. Eng. Online 2016, 15, 2. [Google Scholar] [CrossRef]
- Neelakantan, S.; Xin, Y.; Gaver, D.P.; Cereda, M.; Rizi, R.; Smith, B.J.; Avazmohammadi, R. Computational lung modelling in respiratory medicine. J. R. Soc. Interface 2022, 19, 20220062. [Google Scholar] [CrossRef]
- Wang, H.; Li, Y.; Liu, S.; Yue, X. Design Computer-Aided Diagnosis System Based on Chest CT Evaluation of Pulmonary Nodules. Comput. Math. Methods Med. 2022, 2022, 7729524. [Google Scholar] [CrossRef]
- Zhang, H.; Meng, D.; Cai, S.; Guo, H.; Chen, P.; Zheng, Z.; Zhu, J.; Zhao, W.; Wang, H.; Zhao, S.; et al. The application of artificial intelligence in lung cancer: A narrative review. Transl. Cancer Res. 2021, 10, 2478–2487. [Google Scholar] [CrossRef]
- Dhammi, I.K.; Kumar, S. Medical subject headings (MeSH) terms. Indian J. Orthop. 2014, 48, 443–444. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, M.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Schiavo, J.H. PROSPERO: An International Register of Systematic Review Protocols. Med. Ref. Serv. Q. 2019, 38, 171–180. [Google Scholar] [CrossRef]
- Foster, M.E.D.; Deardorff, M.A. Open Science Framework (OSF). J. Med. Libr. Assoc. 2017, 105, 203–206. [Google Scholar] [CrossRef]
- Santos, M.K.; Júnior, J.R.F.; Wada, D.T.; Tenório, A.P.M.; Nogueira-Barbosa, M.H.; Marques, P.M.D.A. Artificial intelligence, machine learning, computer-aided diagnosis, and radiomics: Advances in imaging towards to precision medicine. Radiol. Bras. 2019, 52, 387–396. [Google Scholar] [CrossRef]
- Prisciandaro, E.; Sedda, G.; Cara, A.; Diotti, C.; Spaggiari, L.; Bertolaccini, L. Artificial Neural Networks in Lung Cancer Research: A Narrative Review. J. Clin. Med. 2023, 12, 880. [Google Scholar] [CrossRef]
- Farrah, K.; Young, K.; Tunis, M.C.; Zhao, L. Risk of bias tools in systematic reviews of health interventions: An analysis of PROSPERO-registered protocols. Syst. Rev. 2019, 8, 280. [Google Scholar] [CrossRef]
- Dandil, E.; Cakiroglu, M.; Eksi, Z.; Ozkan, M.; Kurt, O.K.; Canan, A. Artificial neural network-based classification system for lung nodules on computed tomography scans. In Proceedings of the 2014 6th International Conference of Soft Computing and Pattern Recognition (SoCPaR), Tunis, Tunisia, 11–14 August 2014. [Google Scholar] [CrossRef]
- Wu, Q.; Zhao, W. Small-Cell Lung Cancer Detection Using a Supervised Machine Learning Algorithm. In Proceedings of the 2017 International Symposium on Computer Science and Intelligent Controls (ISCSIC), Budapest, Hungary, 20–22 October 2017. [Google Scholar] [CrossRef]
- Woźniak, M.; Połap, D.; Capizzi, G.; Sciuto, G.L.; Kośmider, L.; Frankiewicz, K. Small lung nodules detection based on local variance analysis and probabilistic neural network. Comput. Methods Programs Biomed. 2018, 161, 173–180. [Google Scholar] [CrossRef]
- Khan, S.A.; Hussain, S.; Yang, S.; Iqbal, K. Effective and Reliable Framework for Lung Nodules Detection from CT Scan Images. Sci. Rep. 2019, 9, 4989. [Google Scholar] [CrossRef]
- Petousis, P.; Winter, A.; Speier, W.; Aberle, D.R.; Hsu, W.; Bui, A.A.T. Using Sequential Decision Making to Improve Lung Cancer Screening Performance. IEEE Access 2019, 7, 119403–119419. [Google Scholar] [CrossRef]
- Capizzi, G.; Sciuto, G.L.; Napoli, C.; Polap, D.; Wozniak, M. Small Lung Nodules Detection Based on Fuzzy-Logic and Probabilistic Neural Network With Bioinspired Reinforcement Learning. IEEE Trans. Fuzzy Syst. 2019, 28, 1178–1189. [Google Scholar] [CrossRef]
- Chauvie, S.; SOS Study Team; De Maggi, A.; Baralis, I.; Dalmasso, F.; Berchialla, P.; Priotto, R.; Violino, P.; Mazza, F.; Melloni, G.; et al. Artificial intelligence and radiomics enhance the positive predictive value of digital chest tomosynthesis for lung cancer detection within SOS clinical trial. Eur. Radiol. 2020, 30, 4134–4140. [Google Scholar] [CrossRef]
- Hoque, A.; Farabi, A.A.; Ahmed, F.; Islam, Z. Automated Detection of Lung Cancer Using CT Scan Images. In Proceedings of the 2020 IEEE Region 10 Symposium (TENSYMP), Dhaka, Bangladesh, 5–7 June 2020; pp. 1030–1033. [Google Scholar] [CrossRef]
- Kumar, C.A.; Harish, S.; Ravi, P.; Svn, M.; Kumar, B.P.P.; Mohanavel, V.; Alyami, N.M.; Priya, S.S.; Asfaw, A.K. Lung Cancer Prediction from Text Datasets Using Machine Learning. BioMed Res. Int. 2022, 2022, 6254177. [Google Scholar] [CrossRef]
- Nasrullah, N.; Sang, J.; Alam, M.S.; Mateen, M.; Cai, B.; Hu, H. Automated Lung Nodule Detection and Classification Using Deep Learning Combined with Multiple Strategies. Sensors 2019, 19, 3722. [Google Scholar] [CrossRef]
- Ardila, D.; Kiraly, A.P.; Bharadwaj, S.; Choi, B.; Reicher, J.J.; Peng, L.; Tse, D.; Etemadi, M.; Ye, W.; Corrado, G.; et al. End-to-end lung cancer screening with three-dimensional deep learning on low-dose chest computed tomography. Nat. Med. 2019, 25, 954–961. [Google Scholar] [CrossRef]
- Nam, J.G.; Park, S.; Hwang, E.J.; Lee, J.H.; Jin, K.-N.; Lim, K.Y.; Vu, T.H.; Sohn, J.H.; Hwang, S.; Goo, J.M.; et al. Development and Validation of Deep Learning–based Automatic Detection Algorithm for Malignant Pulmonary Nodules on Chest Radiographs. Radiology 2019, 290, 218–228. [Google Scholar] [CrossRef]
- Aggarwal, R.; Sounderajah, V.; Martin, G.; Ting, D.S.W.; Karthikesalingam, A.; King, D.; Ashrafian, H.; Darzi, A. Diagnostic accuracy of deep learning in medical imaging: A systematic review and meta-analysis. NPJ Digit. Med. 2021, 4, 65. [Google Scholar] [CrossRef]
- Nakaura, T.; Higaki, T.; Awai, K.; Ikeda, O.; Yamashita, Y. A primer for understanding radiology articles about machine learning and deep learning. Diagn. Interv. Imaging 2020, 101, 765–770. [Google Scholar] [CrossRef]
- Elaziz, M.A.; Dahou, A.; Mabrouk, A.; Ibrahim, R.A.; Aseeri, A.O. Medical Image Classifications for 6G IoT-Enabled Smart Health Systems. Diagnostics 2023, 13, 834. [Google Scholar] [CrossRef]
- Manco, L.; Maffei, N.; Strolin, S.; Vichi, S.; Bottazzi, L.; Strigari, L. Basic of machine learning and deep learning in imaging for medical physicists. Phys. Med. 2021, 83, 194–205. [Google Scholar] [CrossRef]
- Liu, S.; Yao, W. Prediction of lung cancer using gene expression and deep learning with KL divergence gene selection. BMC Bioinform. 2022, 23, 175. [Google Scholar] [CrossRef]
- Wang, S.; Shi, J.; Ye, Z.; Dong, D.; Yu, D.; Zhou, M.; Liu, Y.; Gevaert, O.; Wang, K.; Zhu, Y.; et al. Predicting EGFR mutation status in lung adenocarcinoma on computed tomography image using deep learning. Eur. Respir. J. 2019, 53, 1800986. [Google Scholar] [CrossRef]
| Study and Author | Country | Study Year | Study Design | Study Quality |
|---|---|---|---|---|
| 1 [26] Dandil et al. | Turkey | 2014 | Retrospective cohort | Excellent |
| 2 [27] Wu et al. | USA | 2017 | Retrospective cohort | Fair |
| 3 [28] Wozniak et al. | Poland | 2018 | Case–control | Fair |
| 4 [29] Khan et al. | Pakistan | 2019 | Case–control | Good |
| 5 [30] Petousis et al. | USA | 2019 | Case–control | Good |
| 6 [31] Capizzi et al. | Poland | 2020 | Case–control | Fair |
| 7 [32] Chauvie et al. | Italy | 2020 | Prospective cohort | Good |
| 8 [33] Hoque et al. | Bangladesh | 2020 | Case–control | Fair |
| 9 [34] Kumar et al. | India | 2022 | Retrospective cohort | Fair |
| Study | Number of Patients | AI Architecture | Comparison Group | Type of Lesions |
|---|---|---|---|---|
| 1 [26] Dandil et al. | 47 | ANN | Microscopic analysis | SCLC |
| 2 [27] Wu et al. | 72 | EDM | Random slices from healthy lung scans | SCLC |
| 3 [28] Wozniak et al. | 404 for training, 100 for testing | PNN | Random X-rays | Malignant vs. benign |
| 4 [29] Khan et al. | 84 | SVM | Expert radiologists | Malignant vs. benign |
| 5 [30] Petousis et al. | 5402 | POMDP | Expert radiologists | Malignant vs. benign |
| 6 [31] Capizzi et al. | 320 for training, 120 for testing | PNN | Random X-rays | Malignant vs. benign |
| 7 [32] Chauvie et al. | 1594 | RFNN | Microscopic analysis | Malignant vs. benign |
| 8 [33] Hoque et al. | 78 | SVM | Random slices from healthy lung scans | Malignant vs. benign |
| 9 [34] Kumar et al. | 32 | SVM | Expert radiologists | NSCLC |
| Study | TP | TN | FP | FN | Images Used for Testing |
|---|---|---|---|---|---|
| 1 [26] Dandil et al. | 24 | 34 | 4 | 2 | 128 CTs |
| 2 [27] Wu et al. | 30 | 26 | 10 | 6 | 12 HRCTs (100–500 slices) |
| 3 [28] Wozniak et al. | 40 | 52 | 6 | 2 | 100 X-rays (80 healthy) |
| 4 [29] Khan et al. | 383 | 389 | 4 | 10 | CT scans |
| 5 [30] Petousis et al. | 31 | 482 | 565 | 1 | LDCT |
| 6 [31] Capizzi et al. | 43 | 68 | 7 | 2 | X-rays |
| 7 [32] Chauvie et al. | 18 | 1573 | 1 | 2 | RADS |
| 8 [33] Hoque et al. | 71 | 3 | 3 | 1 | CT scans |
| 9 [34] Kumar et al. | 32 | 6 | 2 | 2 | CT scans |
| Study | Sensitivity | Specificity | Accuracy | Particularities |
|---|---|---|---|---|
| 1 [26] Dandil et al. | 0.92 | 0.89 | 92.3% | The designed CAD system provides the segmentation of nodules on the lobes with a neural networks model of SOM and ensures classification between benign and malignant nodules with the help of ANN. |
| 2 [27] Wu et al. | 0.83 | 0.72 | 77.8% | The algorithm makes 10 false positive predictions among 36 tests and misses 6 cases. |
| 3 [28] Wozniak et al. | 0.95 | 0.90 | 92.0% | This method starts with the localization and extraction of the lung nodules by computing, for each pixel of the original image, the local variance obtaining an output image with the same size as the original image. The PNN architecture has a lower computational complexity, and it can detect low-contrast nodules. |
| 4 [29] Khan et al. | 0.97 | 0.99 | 98.0% | The ML architecture consists of multiple phases that include image contrast enhancement, segmentation, and optimal feature extraction, followed by the employment of these features for training and testing of SVM. |
| 5 [30] Petousis et al. | 0.97 | 0.46 | NR | The ML algorithm reduced the rate of false positives yet preserved a high rate of true positives comparable to that of human experts and identified lung malignancies earlier. |
| 6 [31] Capizzi et al. | 0.96 | 0.91 | 92.5% | The algorithm can identify nodules with a diameter ≤ 20 mm and minimal contrast. |
| 7 [32] Chauvie et al. | 0.90 | 1.00 | 100% | Given the various radiological characteristics of nodules on CT and DTS, the lung-RADS category did not improve the diagnostic accuracy of visual examination. The neural network was the only technique to achieve a high PPV without sacrificing sensitivity, as compared with binary visual analysis, logistic regression, and random forest algorithm. |
| 8 [33] Hoque et al. | 0.99 | 0.50 | 95.0% | The improved SVM model achieved higher accuracy in identifying regions of interest in the lung area where the cancer was localized. |
| 9 [34] Kumar et al. | 0.81 | 0.82 | 98.8% | The SVM model achieved higher precision than KNN, naïve Bayes, and J48 classifier, with or without SMOTE. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pacurari, A.C.; Bhattarai, S.; Muhammad, A.; Avram, C.; Mederle, A.O.; Rosca, O.; Bratosin, F.; Bogdan, I.; Fericean, R.M.; Biris, M.; et al. Diagnostic Accuracy of Machine Learning AI Architectures in Detection and Classification of Lung Cancer: A Systematic Review. Diagnostics 2023, 13, 2145. https://doi.org/10.3390/diagnostics13132145
Pacurari AC, Bhattarai S, Muhammad A, Avram C, Mederle AO, Rosca O, Bratosin F, Bogdan I, Fericean RM, Biris M, et al. Diagnostic Accuracy of Machine Learning AI Architectures in Detection and Classification of Lung Cancer: A Systematic Review. Diagnostics. 2023; 13(13):2145. https://doi.org/10.3390/diagnostics13132145
Chicago/Turabian StylePacurari, Alina Cornelia, Sanket Bhattarai, Abdullah Muhammad, Claudiu Avram, Alexandru Ovidiu Mederle, Ovidiu Rosca, Felix Bratosin, Iulia Bogdan, Roxana Manuela Fericean, Marius Biris, and et al. 2023. "Diagnostic Accuracy of Machine Learning AI Architectures in Detection and Classification of Lung Cancer: A Systematic Review" Diagnostics 13, no. 13: 2145. https://doi.org/10.3390/diagnostics13132145
APA StylePacurari, A. C., Bhattarai, S., Muhammad, A., Avram, C., Mederle, A. O., Rosca, O., Bratosin, F., Bogdan, I., Fericean, R. M., Biris, M., Olaru, F., Dumitru, C., Tapalaga, G., & Mavrea, A. (2023). Diagnostic Accuracy of Machine Learning AI Architectures in Detection and Classification of Lung Cancer: A Systematic Review. Diagnostics, 13(13), 2145. https://doi.org/10.3390/diagnostics13132145











