Primary Osseous Malignancies of the Spine
Abstract
1. Introduction
2. Imaging Modalities and Techniques
3. Types of Lesions
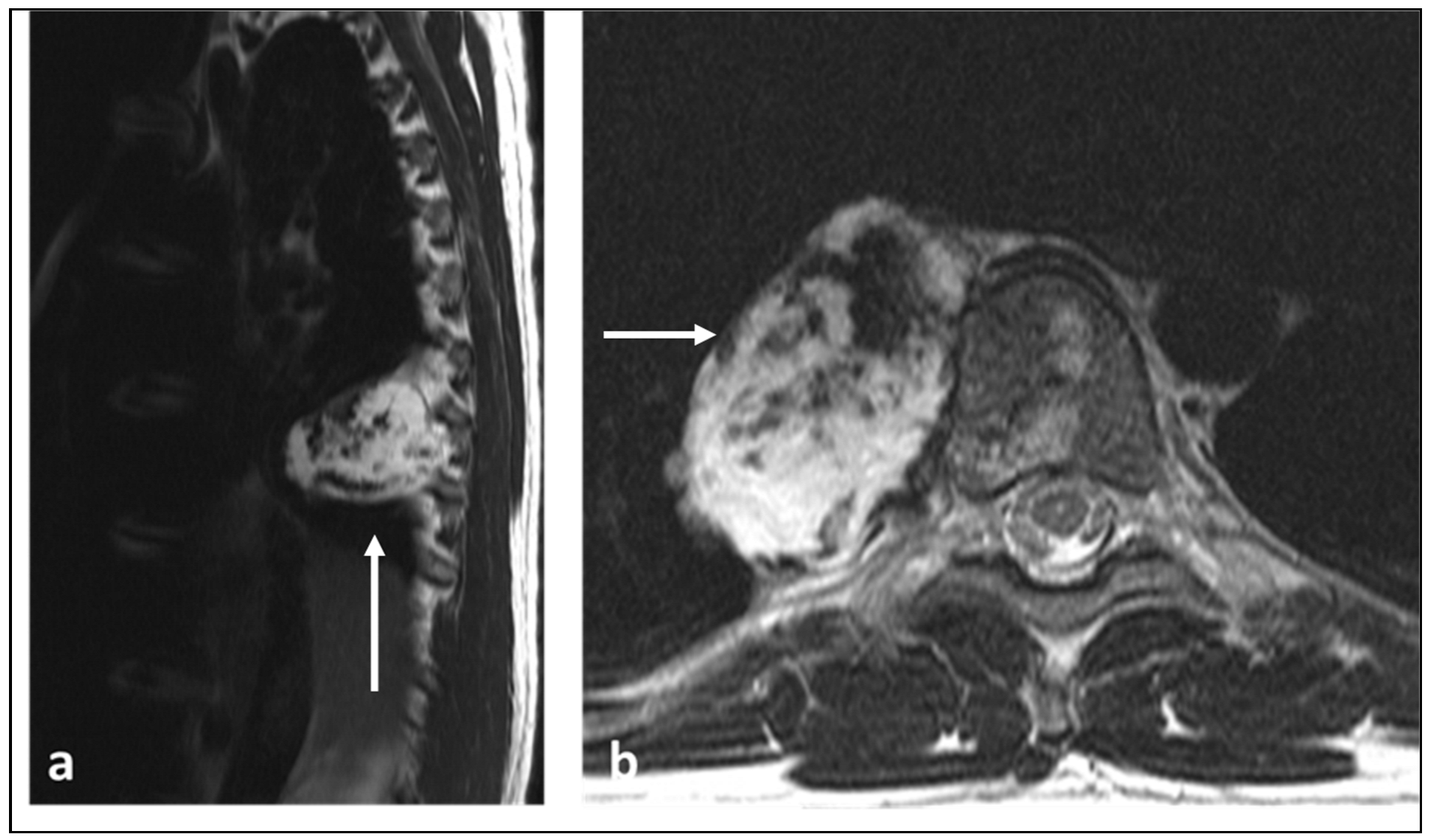
3.1. Osteosarcoma
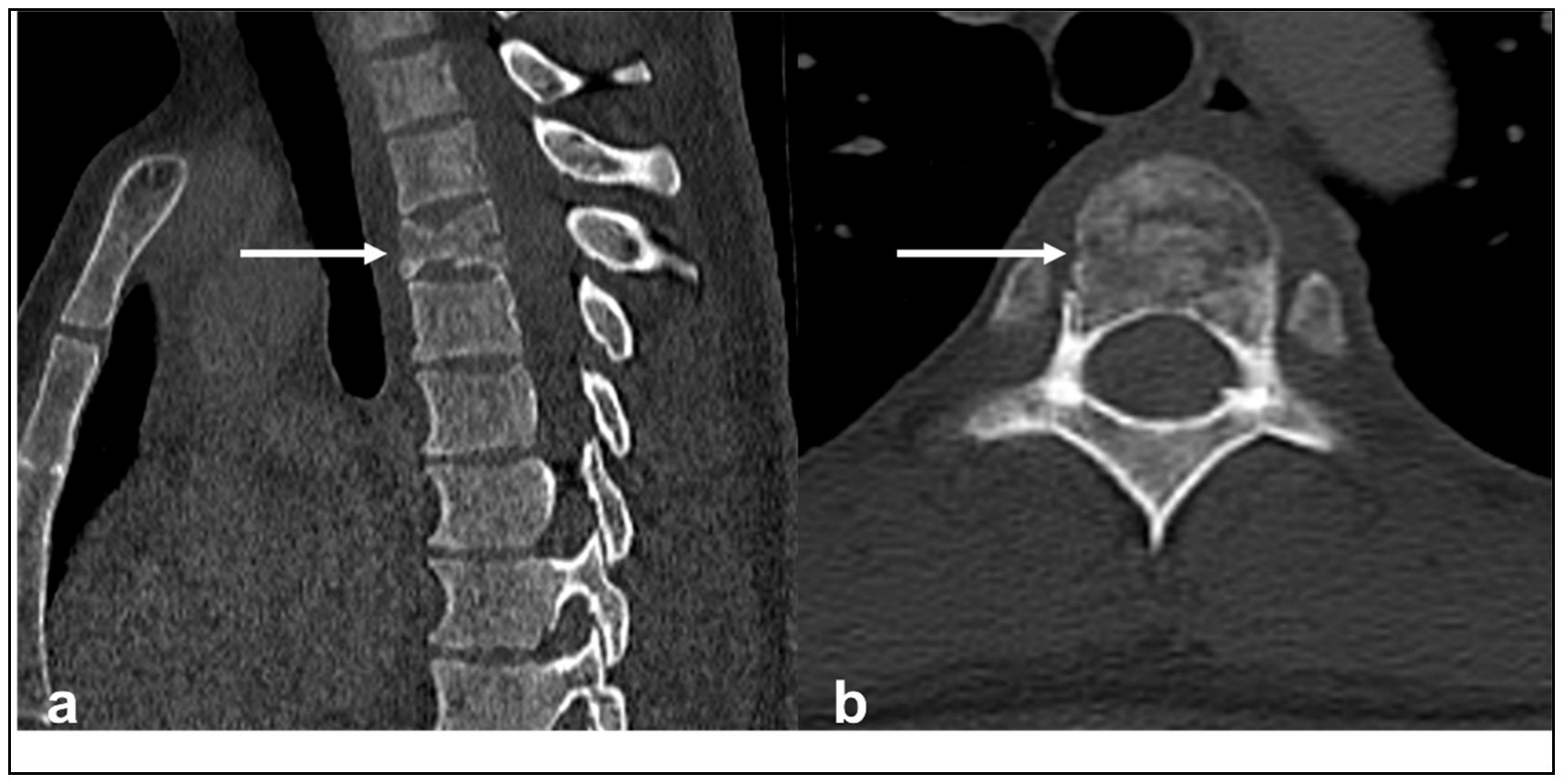
3.2. Ewing Sarcoma
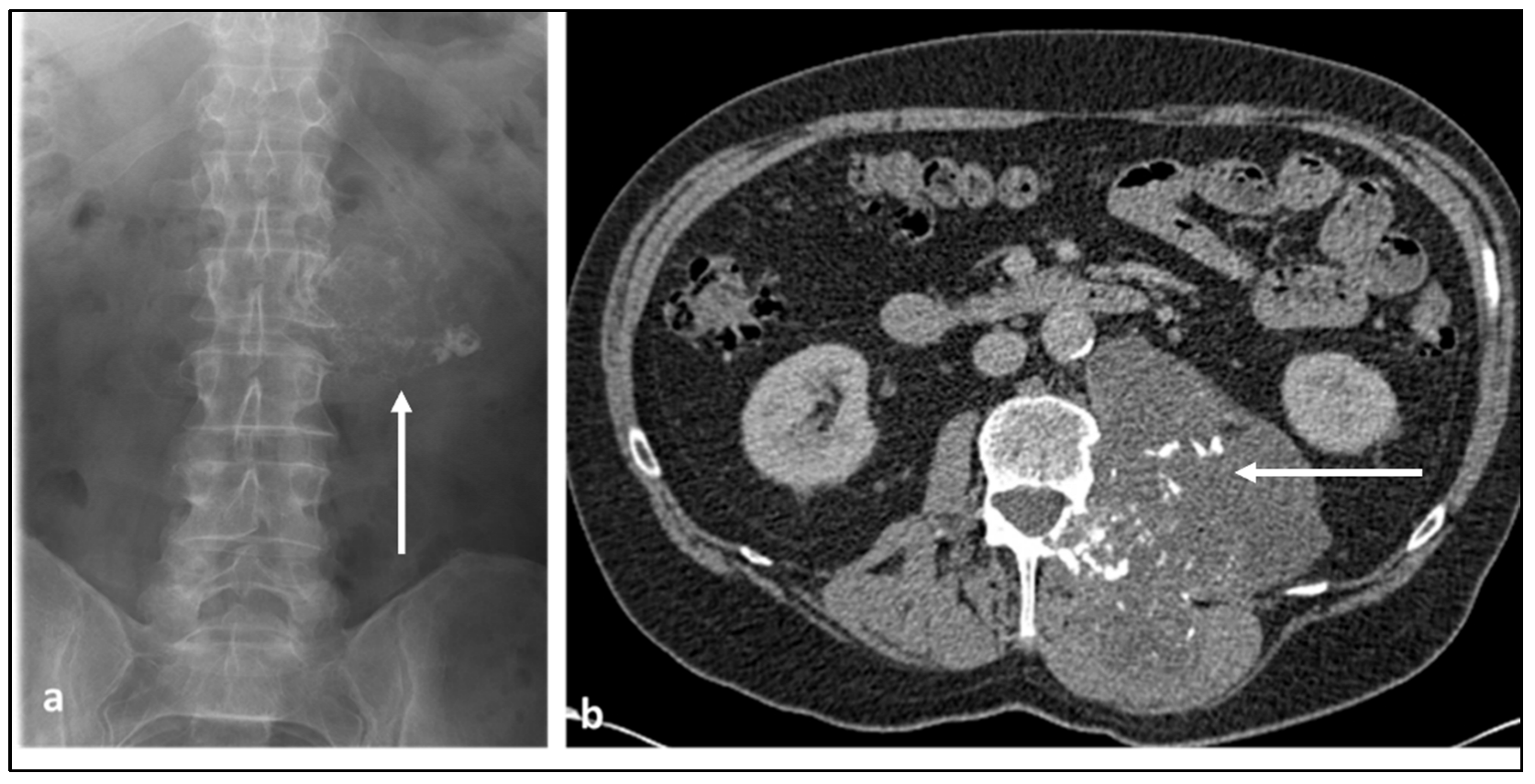
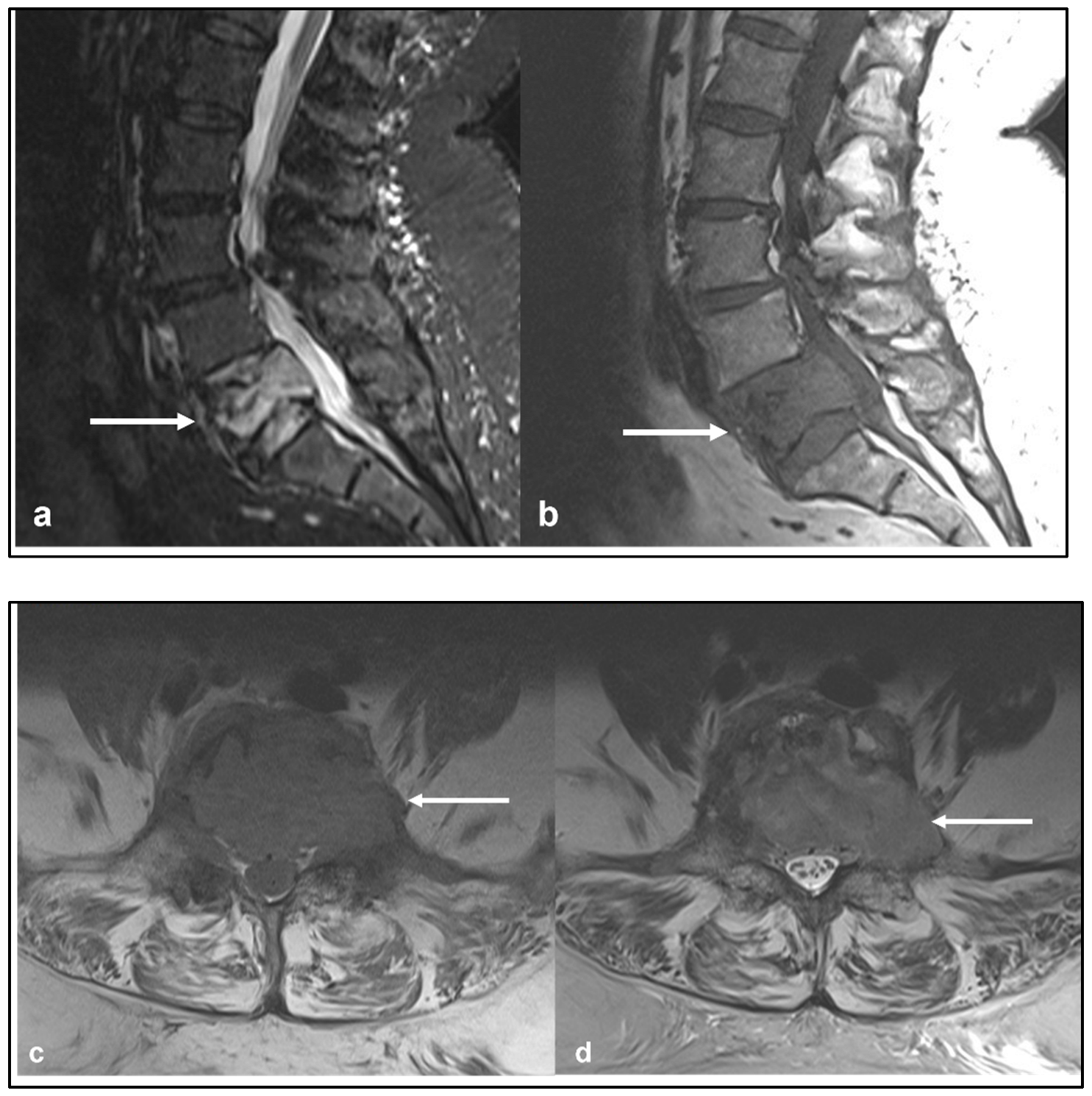
3.3. Chondrosarcoma
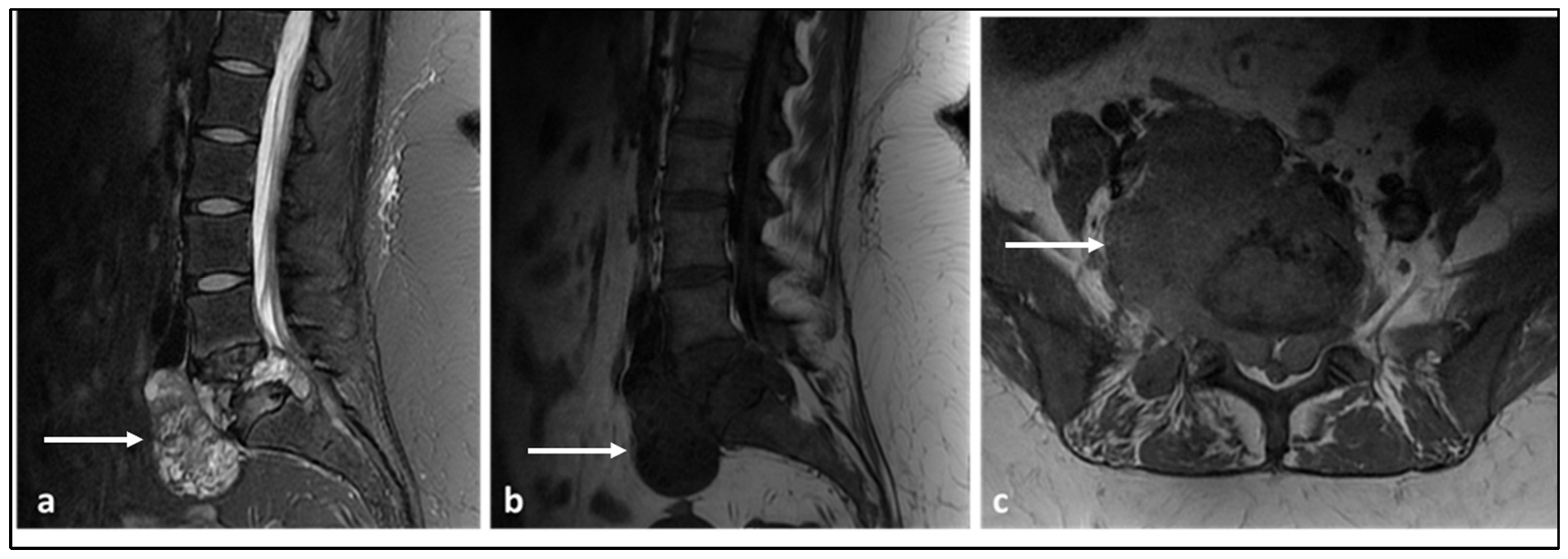
3.4. Chordoma
3.5. Lymphoma
3.6. Plasmacytoma
3.7. Angiosarcoma and Epithelioid Haemangioendothelioma (EHE)
4. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Saifuddin, A.; Tyler, P.; Hargunani, R. Musculoskeletal MRI, 2nd ed.; CRC Press: Boca Raton, FL, USA, 2006; pp. 1116–1152. [Google Scholar]
- Patnaik, S.; Jyotsnarani, Y.; Uppin, S.G.; Susarla, R. Imaging features of primary tumors of the spine: A pictorial essay. Indian J. Radiol. Imaging 2016, 26, 279–289. [Google Scholar] [CrossRef]
- Murphey, M.D.; Andrews, C.L.; Flemming, D.J.; Temple, H.T.; Smith, W.S.; Smirniotopoulos, J.G. From the archives of the AFIP. Primary tumors of the spine: Radiologic pathologic correlation. Radiographics 1996, 16, 1131–1158. [Google Scholar] [CrossRef] [PubMed]
- Orguc, S.; Arkun, R. Primary tumors of the spine. Semin. Musculoskelet. Radiol. 2014, 18, 280–299. [Google Scholar]
- Smith, E.; Hegde, G.; Czyz, M.; Hughes, S.; Haleem, S.; Grainger, M.; James, S.L.; Botchu, R. A Radiologists’ Guide to En Bloc Resection of Primary Tumors in the Spine: What Does the Surgeon Want to Know? Indian J. Radiol. Imaging 2022, 32, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.; Hegde, G.; Czyz, M.; Grainger, M.; James, S.L.; Botchu, R. A guide to assessing post-operative complications following en bloc spinal resection. J. Clin. Orthop. Trauma 2021, 23, 101653. [Google Scholar] [CrossRef] [PubMed]
- Kelley, S.P.; Ashford, R.U.; Rao, A.S.; Dickson, R.A. Primary bone tumours of the spine: A 42-year survey from the Leeds Regional Bone Tumour Registry. Eur. Spine J. 2007, 16, 405–409. [Google Scholar] [CrossRef]
- Charest-Morin, R.; Fisher, C.G.; Sahgal, A.; Boriani, S.; Gokaslan, Z.L.; Lazary, A.; Reynolds, J.; Bettegowda, C.; Rhines, L.D.; Dea, N. Primary Bone Tumor of the Spine-An Evolving Field: What a General Spine Surgeon Should Know. Glob. Spine J. 2019, 9, 108s–116s. [Google Scholar] [CrossRef]
- Patel, A.; James, S.L.; Davies, A.M.; Botchu, R. Spinal imaging update: An introduction to techniques for advanced MRI. Bone Jt. J. 2015, 97, 1683–1692. [Google Scholar] [CrossRef]
- Elawad, A.; Shah, A.; Davies, M.; Botchu, R. The Use of Gadolinium in Musculoskeletal MRI-Time to Rethink? Indian J. Radiol. Imaging 2021, 31, 635–643. [Google Scholar] [CrossRef]
- Hurley, P.; Azzopardi, C.; Botchu, R.; Grainger, M.; Gardner, A. Can MRI be used as a safe and expedient option for calculating Spinal Instability Neoplastic Score for patients with metastatic spinal cord compression? Bone Jt. J. 2021, 103, 971–975. [Google Scholar] [CrossRef]
- Ulano, A.; Bredella, M.A.; Burke, P.; Chebib, I.; Simeone, F.J.; Huang, A.J.; Torriani, M.; Chang, C.Y. Distinguishing Untreated Osteoblastic Metastases From Enostoses Using CT Attenuation Measurements. AJR Am. J. Roentgenol. 2016, 207, 362–368. [Google Scholar] [CrossRef] [PubMed]
- Koh, E.; Walton, E.R.; Watson, P. VIBE MRI: An alternative to CT in the imaging of sports-related osseous pathology? Br. J. Radiol. 2018, 91, 20170815. [Google Scholar] [CrossRef] [PubMed]
- Jeffrey, S.; Ross, M.; Kevin, R.; Moore, M. Osteosarcoma. In STATdx Spine; Elsevier Inc.: Amsterdam, The Netherlands, 2023. [Google Scholar]
- Ilaslan, H.; Sundaram, M.; Unni, K.K.; Dekutoski, M.B. Primary Ewing’s sarcoma of the vertebral column. Skelet. Radiol. 2004, 33, 506–513. [Google Scholar] [CrossRef]
- Shin, J.H.; Lee, H.K.; Rhim, S.C.; Cho, K.J.; Choi, C.G.; Suh, D.C. Spinal epidural extraskeletal Ewing sarcoma: MR findings in two cases. AJNR Am. J. Neuroradiol. 2001, 22, 795–798. [Google Scholar]
- Chaudhry, S.R.; Tsetse, C.; Chennan, S.E. Early recognition and diagnosis of Ewing sarcoma of the cervical spine. Radiol. Case Rep. 2019, 14, 160–163. [Google Scholar] [CrossRef]
- Davies, A.M.; Patel, A.; Botchu, R.; Azzopardi, C.; James, S.; Jeys, L. The changing face of central chondrosarcoma of bone. One UK-based orthopaedic oncology unit’s experience of 33 years referrals. J. Clin. Orthop. Trauma 2021, 17, 106–111. [Google Scholar] [CrossRef] [PubMed]
- Arshi, A.; Sharim, J.; Park, D.Y.; Park, H.Y.; Bernthal, N.M.; Yazdanshenas, H.; Shamie, A.N. Chondrosarcoma of the Osseous Spine: An Analysis of Epidemiology, Patient Outcomes, and Prognostic Factors Using the SEER Registry from 1973 to 2012. Spine 2017, 42, 644–652. [Google Scholar] [CrossRef]
- Yin, H.; Zhou, W.; Meng, J.; Zhang, D.; Wu, Z.; Wang, T.; Wang, J.; Wang, P.; Shi, X.; Wu, S.; et al. Prognostic factors of patients with spinal chondrosarcoma: A retrospective analysis of 98 consecutive patients in a single center. Ann. Surg. Oncol. 2014, 21, 3572–3578. [Google Scholar] [CrossRef]
- York, J.E.; Berk, R.H.; Fuller, G.N.; Rao, J.S.; Abi-Said, D.; Wildrick, D.M.; Gokaslan, Z.L. Chondrosarcoma of the spine: 1954 to 1997. J. Neurosurg. 1999, 90, 73–78. [Google Scholar] [CrossRef]
- Stuckey, R.M.; Marco, R.A. Chondrosarcoma of the mobile spine and sacrum. Sarcoma 2011, 2011, 274281. [Google Scholar] [CrossRef]
- Rajakulasingam, R.; Murphy, J.; Botchu, R.; James, S.L. Osteochondromas of the cervical spine-case series and review. J. Clin. Orthop. Trauma 2020, 11, 905–909. [Google Scholar] [CrossRef] [PubMed]
- Murphey, M.D.; Walker, E.A.; Wilson, A.J.; Kransdorf, M.J.; Temple, H.T.; Gannon, F.H. From the archives of the AFIP: Imaging of primary chondrosarcoma: Radiologic-pathologic correlation. Radiographics 2003, 23, 1245–1278. [Google Scholar]
- McLoughlin, E.; Davies, A.M.; Iqbal, A.; James, S.L.; Botchu, R. The diagnostic significance of pulmonary nodules on CT thorax in chondrosarcoma of bone. Clin. Radiol. 2020, 75, 395–405. [Google Scholar] [CrossRef]
- Tokuhashi, Y.; Uei, H.; Oshima, M. Classification and scoring systems for metastatic spine tumors: A literature review. Spine Surg. Relat. Res. 2017, 1, 44–55. [Google Scholar] [CrossRef]
- Bergh, P.; Gunterberg, B.; Meis-Kindblom, J.M.; Kindblom, L.G. Prognostic factors and outcome of pelvic, sacral, and spinal chondrosarcomas: A center-based study of 69 cases. Cancer 2001, 91, 1201–1212. [Google Scholar] [CrossRef] [PubMed]
- Tenny, S.; Varacallo, M. Chordoma. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK430846/ (accessed on 23 March 2023).
- Farsad, K.; Kattapuram, S.; Sacknoff, R.; Ono, J.; Nielsen, G. Sacral Chordoma. Radiographics 2009, 29, 1525–1530. [Google Scholar] [CrossRef]
- Konieczkowski, D.J.; DeLaney, T.F.; Yamada, Y.J. Radiation Strategies for Spine Chordoma: Proton Beam, Carbon Ions, and Stereotactic Body Radiation Therapy. Neurosurg. Clin. N. Am. 2020, 31, 263–2688. [Google Scholar] [CrossRef]
- Shi, C.; Lin, H.; Huang, S.; Xiong, W.; Hu, L.; Choi, I.; Press, R.; Hasan, S.; Simone, C.; Chhabra, A. Comprehensive Evaluation of Carbon-Fiber-Reinforced Polyetheretherketone (CFR-PEEK) Spinal Hardware for Proton and Photon Planning. Technol. Cancer Res. Treat. 2022, 21, 15330338221091700. [Google Scholar] [CrossRef] [PubMed]
- Mulligan, M.E.; McRae, G.A.; Murphey, M.D. Imaging features of primary lymphoma of bone. AJR Am. J. Roentgenol. 1999, 173, 1691–1697. [Google Scholar] [CrossRef]
- Bindal, P.; Desai, A.; Delasos, L.; Mulay, S.; Vredenburgh, J. Primary Bone Lymphoma: A Case Series and Review of Literature. Case Rep. Hematol. 2020, 2020, 4254803. [Google Scholar] [CrossRef]
- Dürr, H.; Müller, P.; Hiller, E.; Maier, M.; Baur, A.; Jansson, V.; Refior, H. Malignant lymphoma of bone. Arch. Orthop. Trauma Surg. 2002, 122, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Steiner, R.M.; Mitchell, D.G.; Rao, V.M.; Schweitzer, M.E. Magnetic resonance imaging of diffuse bone marrow disease. Radiol. Clin. N. Am. 1993, 31, 383–409. [Google Scholar] [CrossRef] [PubMed]
- Beal, K.; Allen, L.; Yahalom, J. Primary bone lymphoma: Treatment results and prognostic factors with long-term follow-up of 82 patients. Cancer 2006, 106, 2652–2656. [Google Scholar] [CrossRef]
- Wang, Y.; Zhu, X.L.; Peeroo, M.W.; Qian, Z.H.; Shi, D.; Wei, S.M.; Yu, R.S. Pelvic solitary plasmacytoma: Computed tomography and magnetic resonance imaging findings with histopathologic correlation. Korean J. Radiol. 2015, 16, 146–153. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.-H.; Lee, S.-T.; Jung, S.-M.; Tu, P.-H. Primary spinal angiosarcoma. J. Clin. Neurosci. 2010, 17, 387–389. [Google Scholar] [CrossRef]


| Classification | Tumour |
|---|---|
| Osteogenic | Osteosarcoma |
| Round cell tumours | Ewing sarcoma |
| Chondrogenic | Chondrosarcoma |
| Notochordal origin | Chordoma |
| Haematopoietic | Lymphoma Plasmacytoma |
| Vascular | Angiosarcoma Epithelioid Haemangioendothelioma |
| Tumour | CT Features | MRI Features |
|---|---|---|
| Osteosarcoma | Osteoid matrix with sclerotic and lytic areas. Contrast can obscure osteoid matrix. | Extra-osseous soft tissue component. Low T2 signal foci corresponding to mineralisation. Secondary ABC change with fluid–fluid levels (this can be seen with telangiectatic osteosarcoma also). |
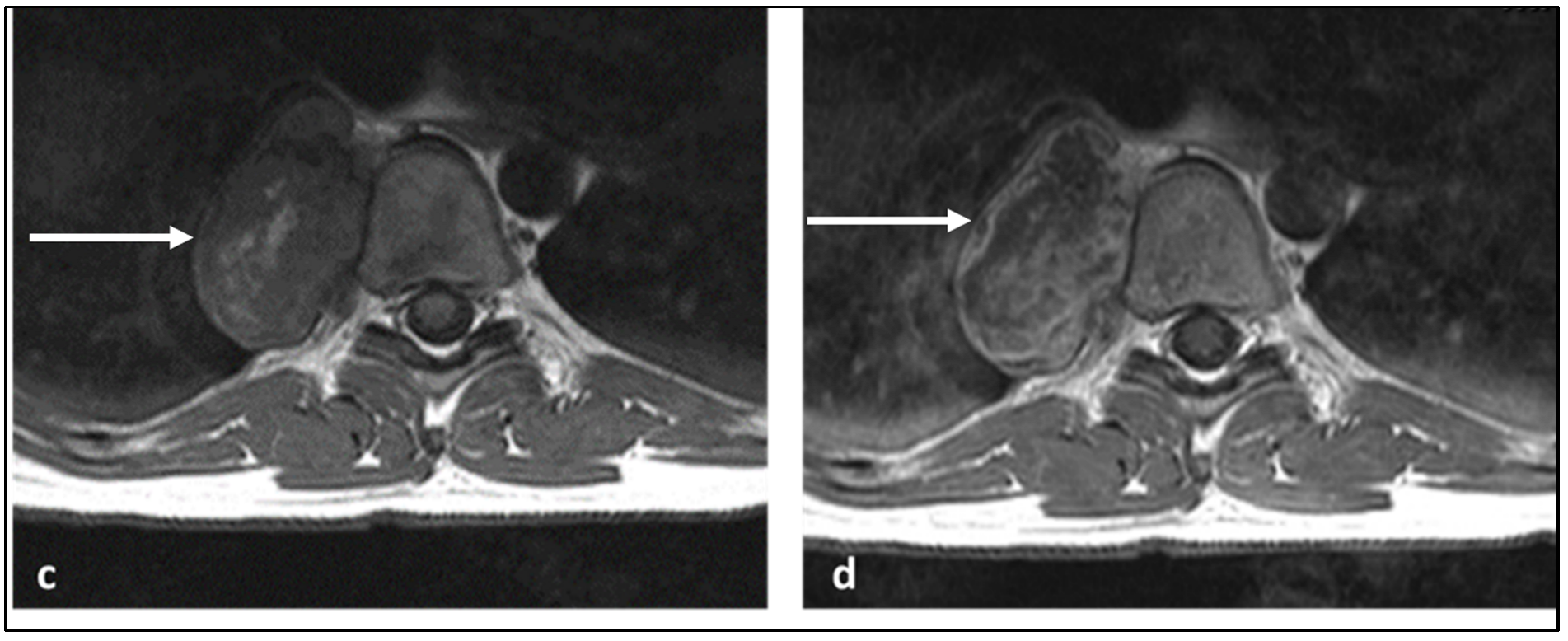
| Ewing sarcoma | Lytic lesion. Vertebral collapse. | Low to intermediate signal T1 and intermediate to high signal T2 lesion. Enhancing extra-osseous soft tissue component. |
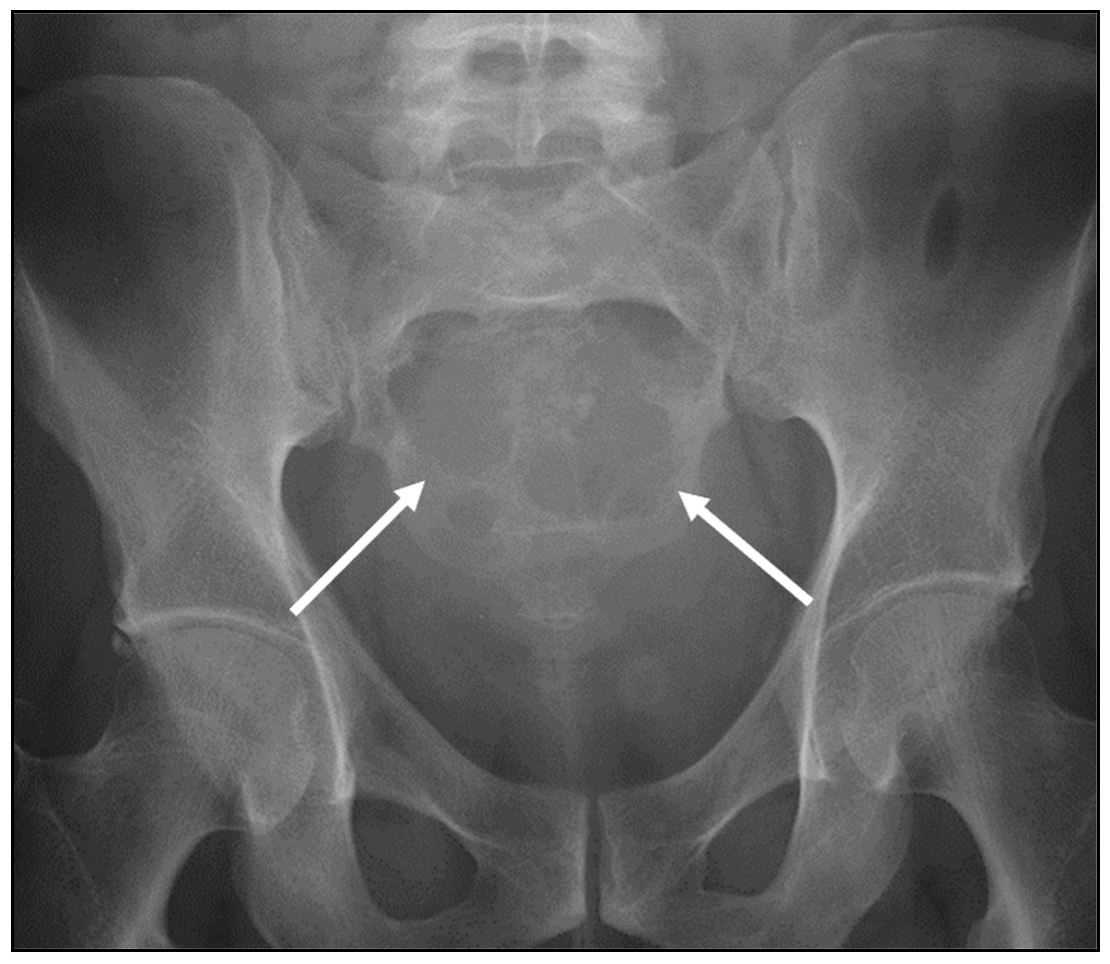
| Chondrosarcoma | Lytic lesion. ‘Rings and arcs’ calcification characteristic of chondroid matrix. | High T2 signal due to cartilage and myxoid content. Peripheral and septal enhancement. Enhancing extra-osseous soft tissue component. |
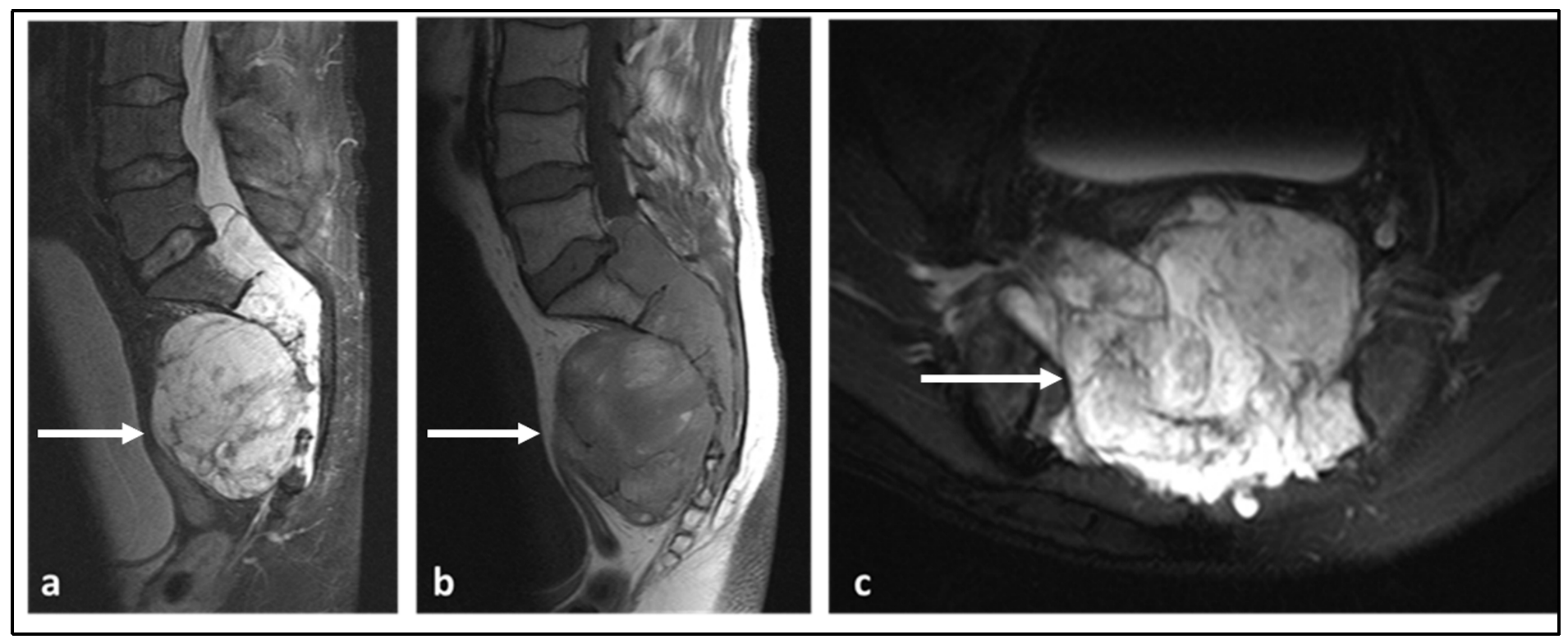
| Chordoma | Low attenuation lytic lesion. | Loculated high T2 signal mass, usually with extra-osseous soft tissue component. High T1 signal due to haemorrhagic and calcified components. |
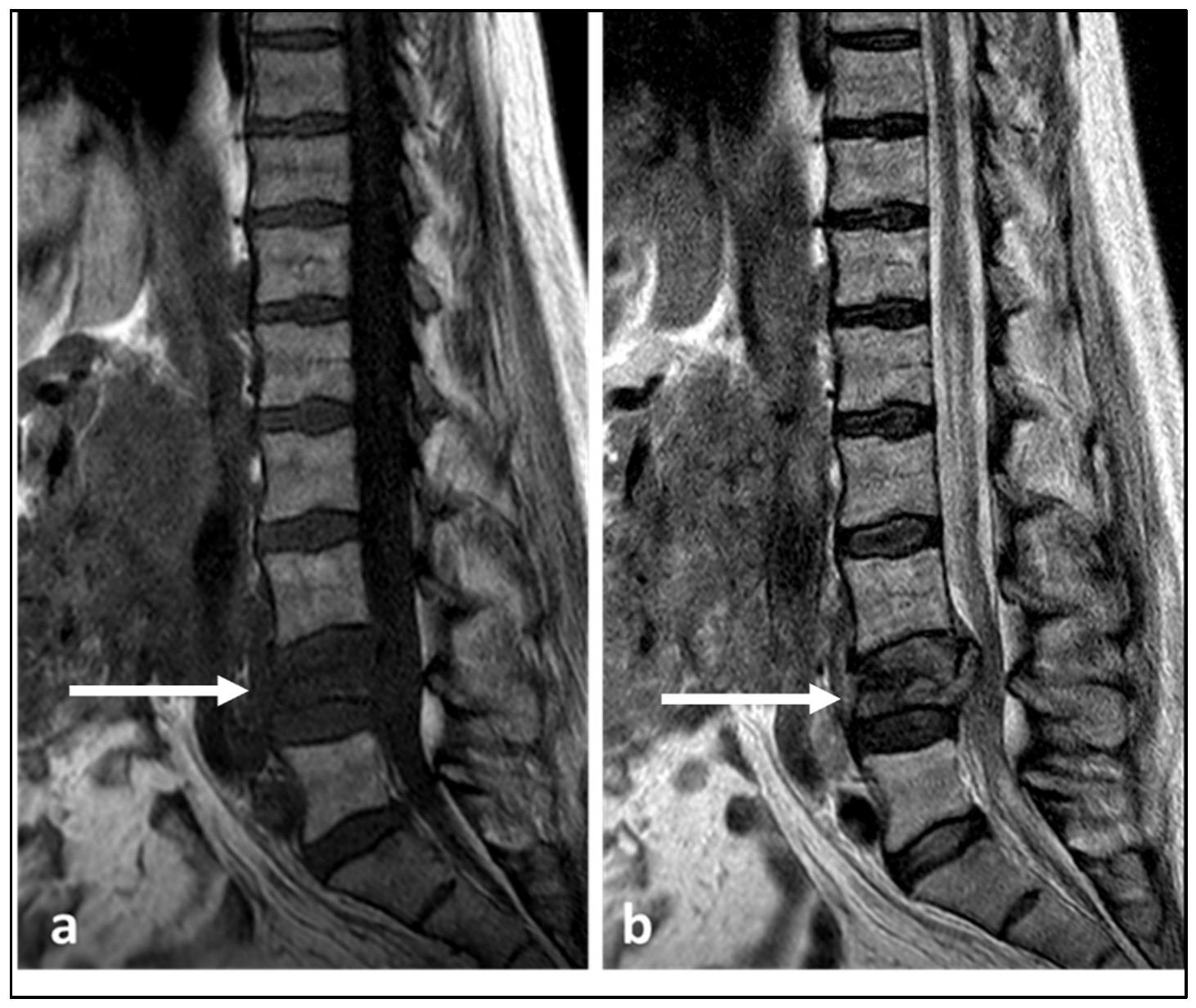
| Lymphoma | Permeative bone loss without overt destruction. | T1 and T2 signal is reduced, but nodular sclerosing lymphoma can be T2 hyperintense. Extra-osseous soft tissue component. |
| Plasmacytoma | Lytic and destructive, vertebral collapse. Soap bubble appearance. | Low to intermediate signal on T1 and increased signal on fluid-sensitive sequences and enhancement post-contrast. Extra-osseous soft tissue component. Multiple trabeculae within the lesion, with a characteristic soap bubble appearance. |
| Angiosarcoma and Epithelioid Haemangioendothelioma | Lytic lesion. | High flow serpiginous vascular channels. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ariyaratne, S.; Jenko, N.; Iyengar, K.P.; James, S.; Mehta, J.; Botchu, R. Primary Osseous Malignancies of the Spine. Diagnostics 2023, 13, 1801. https://doi.org/10.3390/diagnostics13101801
Ariyaratne S, Jenko N, Iyengar KP, James S, Mehta J, Botchu R. Primary Osseous Malignancies of the Spine. Diagnostics. 2023; 13(10):1801. https://doi.org/10.3390/diagnostics13101801
Chicago/Turabian StyleAriyaratne, Sisith, Nathan Jenko, Karthikeyan P. Iyengar, Steven James, Jwalant Mehta, and Rajesh Botchu. 2023. "Primary Osseous Malignancies of the Spine" Diagnostics 13, no. 10: 1801. https://doi.org/10.3390/diagnostics13101801
APA StyleAriyaratne, S., Jenko, N., Iyengar, K. P., James, S., Mehta, J., & Botchu, R. (2023). Primary Osseous Malignancies of the Spine. Diagnostics, 13(10), 1801. https://doi.org/10.3390/diagnostics13101801






