Is It Possible to Replace Conventional Radiography (CR) with a Dose Neutral Computed Tomography (CT) of the Cervical Spine in Emergency Radiology—An Experimental Cadaver Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Human Cadaver Study
2.3. Evaluation of IQ and Physical Body Parameters
2.4. Phantom Study
2.5. Estimation of Dose Values
2.6. Statistical Analysis
3. Results
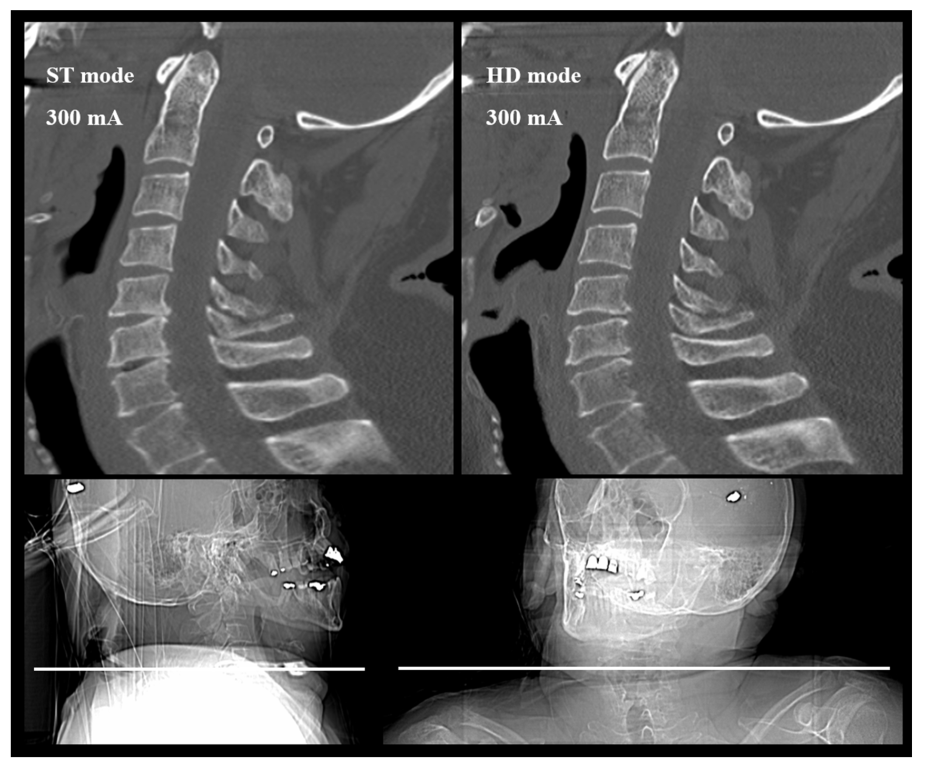
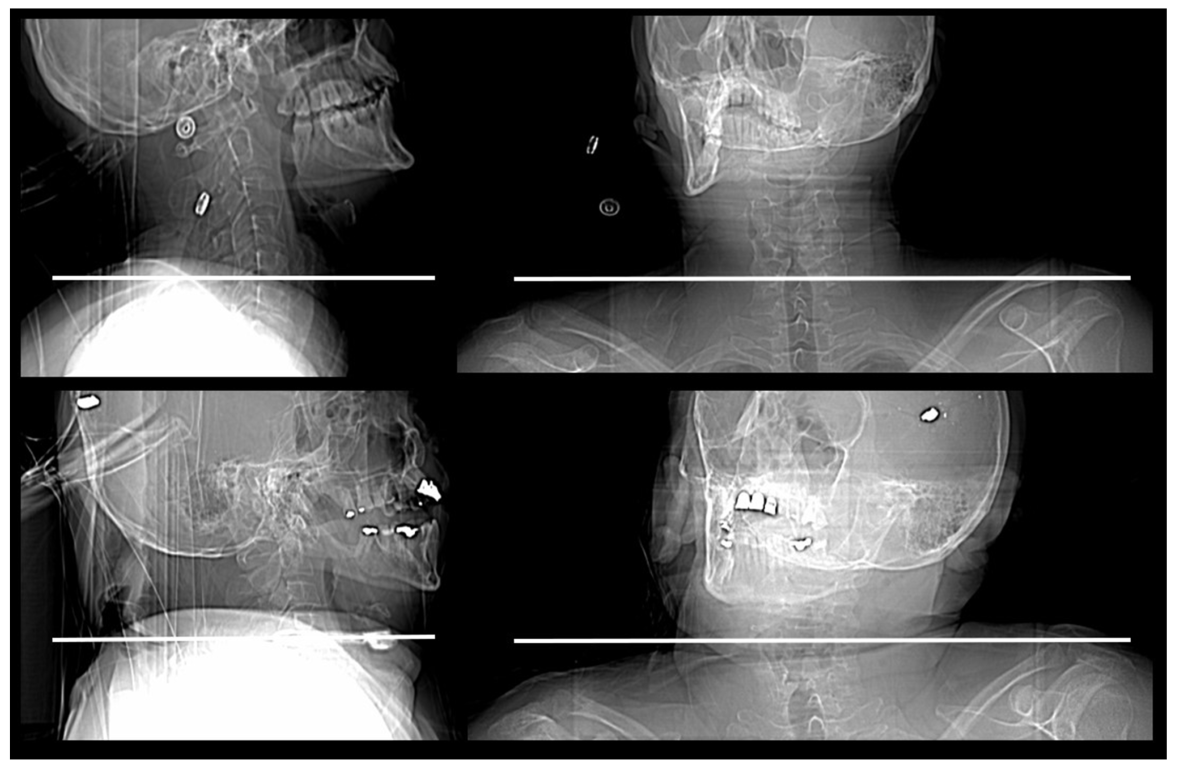
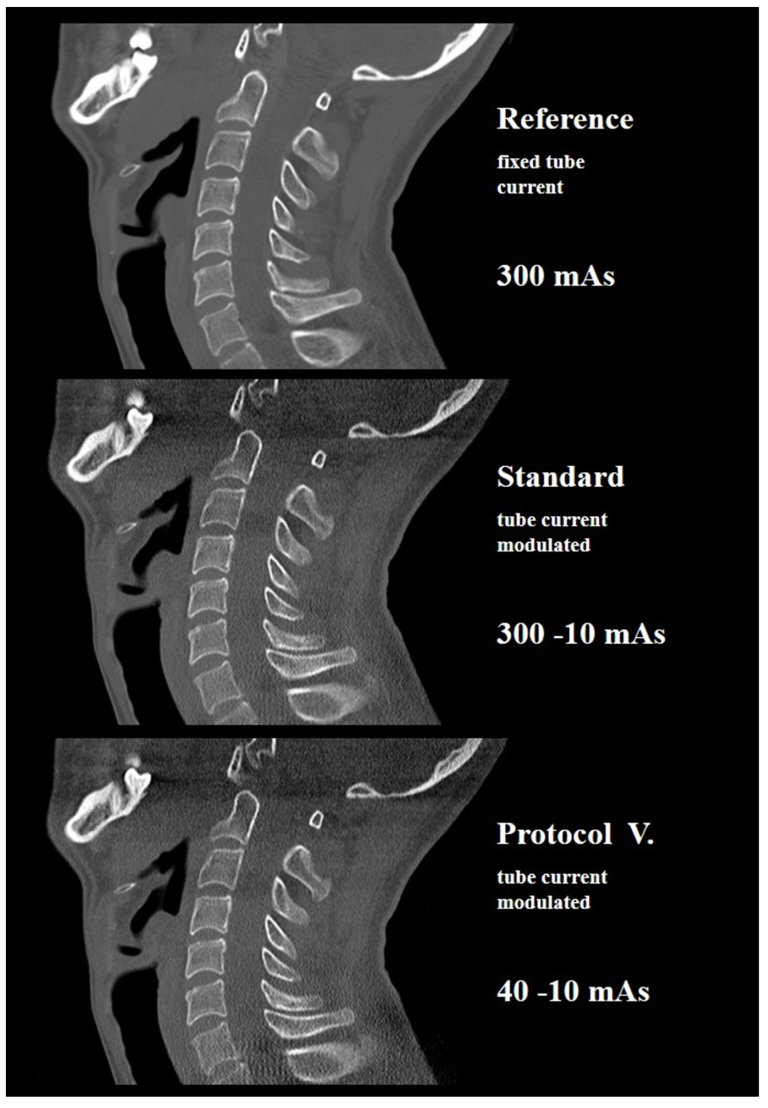
3.1. Cadaver Study
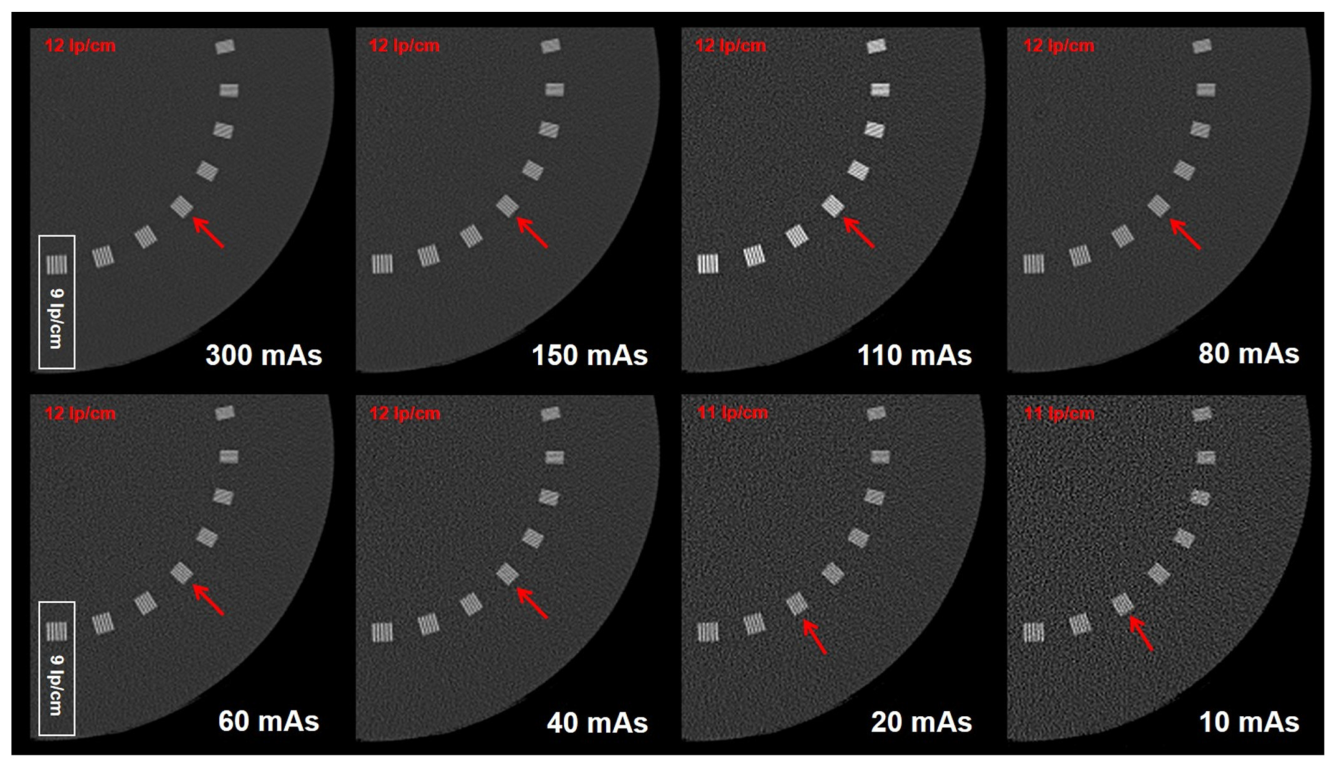
3.2. Phantom Study
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| body mass index | BMI |
| Canadian Cervical Spine Rule | CCR |
| cervical spine | c-spine |
| computed tomography | CT |
| computed tomography dose index | CTDI |
| dose length product | DLP |
| effective dose | ED |
| image quality | IQ |
| mean value | MV |
| National Emergency X-Radiography Utilization Study | NEXUS |
| standard deviation | SD |
| Statistical Package für Social Sciences | SPSS |
References
- Holly, L.T.; Kelly, D.F.; Counelis, G.J.; Blinman, T.; McArthur, D.L.; Cryer, H.G. Cervical spine trauma associated with moderate and severe head injury: Incidence, risk factors, and injury characteristics. J. Neurosurg. 2002, 96 (Suppl. 3), 285–291. [Google Scholar] [CrossRef] [PubMed]
- Tian, H.L.; Guo, Y.; Hu, J.; Rong, B.Y.; Wang, G.; Gao, W.W.; Chen, S.W.; Chen, H. Clinical characterization of comatose patients with cervical spine injury and traumatic brain injury. J. Trauma 2009, 67, 1305–1310. [Google Scholar] [CrossRef]
- Bayless, P.; Ray, V.G. Incidence of cervical spine injuries in association with blunt head trauma. Am. J. Emerg. Med. 1989, 7, 139–142. [Google Scholar] [CrossRef]
- McCaig, L.F.; Ly, N. National Hospital Ambulatory Medical Care Survey: 2000 Emergency Department Summary—Advance Data from vital and Health Statistics; DHHS publication no. 326 (PHS) 2002-1250 02-0259; National Center for Health Statistics: Hyattsville, MD, USA, 2002. [Google Scholar]
- Davis, J.W.; Phreaner, D.L.; Hoyt, D.B.; Mackersie, R.C. The etiology of missed cervical spine injuries. J. Trauma 1993, 34, 342–346. [Google Scholar] [CrossRef] [PubMed]
- Stiell, I.G.; Wells, G.A.; Vandemheen, K.L.; Clement, C.M.; Lesiuk, H.; De Maio, V.J.; Laupacis, A.; Schull, M.; McKnight, R.D.; Verbeek, R.; et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA 2001, 286, 1841–1848. [Google Scholar] [CrossRef]
- Stiell, I.G.; Clement, C.M.; McKnight, R.D.; Brison, R.; Schull, M.J.; Rowe, B.H.; Worthington, J.R.; Eisenhauer, M.A.; Cass, D.; Greenberg, G.; et al. The Canadian C-spine rule versus the NEXUS low-risk criteria in patients with trauma. N. Engl. J. Med. 2003, 349, 2510–2518. [Google Scholar] [CrossRef] [Green Version]
- ACR American College of Radiology. Clinical Condition: Suspected Spine Trauma. Available online: http://www.acr.org/~/media/f579c123f999479c88390a3df976be77.pdf (accessed on 15 March 2019).
- Bailitz, J.; Starr, F.; Beecroft, M.; Bankoff, J.; Roberts, R.; Bokhari, F.; Joseph, K.; Wiley, D.; Dennis, A.; Gilkey, S.; et al. CT should replace three-view radiographs as the initial screening test in patients at high, moderate, and low risk for blunt cervical spine injury: A prospective comparison. J. Trauma 2009, 66, 1605–1609. [Google Scholar] [CrossRef]
- Holmes, J.F.; Akkinepalli, R. Computed tomography versus plain radiography to screen for cervical spine injury: A meta-analysis. J. Trauma 2005, 58, 902–905. [Google Scholar] [CrossRef] [Green Version]
- Hoffman, J.R.; Wolfson, A.B.; Todd, K.; Mower, W.R. Selective cervical spine radiography in blunt trauma: Methodology of the National Emergency X-Radiography Utilization Study (NEXUS). Ann. Emerg. Med. 1998, 32, 461–469. [Google Scholar] [CrossRef]
- Gale, S.C.; Gracias, V.H.; Reilly, P.M.; Schwab, C.W. The inefficiency of plain radiography to evaluate the cervical spine after blunt trauma. J. Trauma 2005, 59, 1121–1125. [Google Scholar] [CrossRef]
- Mettler, F.A., Jr.; Thomadsen, B.R.; Bhargavan, M.; Gilley, D.B.; Gray, J.E.; Lipoti, J.A.; McCrohan, J.; Yoshizumi, T.T.; Mahesh, M. Medical radiation exposure in the U.S. in 2006: Preliminary results. Health Phys. 2008, 95, 502–507. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Larson, D.B.; Johnson, L.W.; Schnell, B.M.; Salisbury, S.R.; Forman, H.P. National trends in CT use in the emergency department: 1995–2007. Radiology 2011, 258, 164–173. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Broder, J.; Warshauer, D.M. Increasing utilization of computed tomography in the adult emergency department, 2000–2005. Emerg. Radiol. 2006, 13, 25–30. [Google Scholar] [CrossRef]
- Richards, P.J.; George, J.; Metelko, M.; Brown, M. Spine computed tomography doses and cancer induction. Spine 2010, 35, 430–433. [Google Scholar] [CrossRef]
- Geyer, L.L.; Körner, M.; Hempel, R.; Deak, Z.; Mueck, F.G.; Linsenmaier, U.; Reiser, M.F.; Wirth, S. Evaluation of a dedicated MDCT protocol using iterative image reconstruction after cervical spine trauma. Clin. Radiol. 2013, 68, e391–e396. [Google Scholar] [CrossRef]
- Weinrich, J.M.; Regier, M.; Well, L.; Bannas, P.; Nykolyn, O.; Heinemann, A.; Sehner, S.; Behzadi, C.; Püschel, K.; Adam, G.; et al. Feasibility of sub-milliSievert CT of the cervical spine: Initial results in fresh human cadavers. Eur. J. Radiol. 2019, 120, 108697. [Google Scholar] [CrossRef] [PubMed]
- Tozakidou, M.; Yang, S.R.; Kovacs, B.K.; Szucs-Farkas, Z.; Studler, U.; Schindera, S.; Hirschmann, A. Dose-optimized computed tomography of the cervical spine in patients with shoulder pull-down: Is image quality comparable with a standard dose protocol in an emergency setting? Eur. J. Radiol. 2019, 120, 108655. [Google Scholar] [CrossRef] [PubMed]
- Tozakidou, M.; Reisinger, C.; Harder, D.; Lieb, J.; Szucs-Farkas, Z.; Müller-Gerbl, M.; Studler, U.; Schindera, S.; Hirschmann, A. Systematic Radiation Dose Reduction in Cervical Spine CT of Human Cadaveric Specimens: How Low Can We Go? AJNR Am. J. Neuroradiol. 2018, 39, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Bongartz, G.; Golding, S.J.; Jurik, A.G.; Leonardi, M.; van Persijn van Meerten, E.; Rodríguez, R.; Schneider, K.; Calzado, A.; Geleijns, J.; Jessen, K.A.; et al. 2004 CT Quality Criteria. European Guidelines for Multislice Computed Tomography. The European Commission. Contract number FIGM-CT2000-20078-CT-TIP. Available online: http://www.drs.dk/guidelines/ct/quality/index.htm (accessed on 15 March 2019).
- Wirth, S.; Meindl, T.; Treitl, M.; Pfeifer, K.J.; Reiser, M. Comparison of different patient positioning strategies to minimize shoulder girdle artifacts in head and neck CT. Eur. Radiol. 2006, 16, 1757–1762. [Google Scholar] [CrossRef]
- Wu, T.H.; Hung, S.C.; Sun, J.Y.; Lin, C.J.; Lin, C.H.; Chiu, C.F.; Liu, M.J.; Teng, M.M.; Guo, W.Y.; Chang, C.Y. How far can the radiation dose be lowered in head CT with iterative reconstruction? Analysis of imaging quality and diagnostic accuracy. Eur. Radiol. 2013, 23, 2612–2621. [Google Scholar] [CrossRef]
- Mueck, F.G.; Roesch, S.; Geyer, L.; Scherr, M.; Seidenbusch, M.; Stahl, R.; Deak, Z.; Wirth, S. Emergency CT head and neck imaging: Effects of swimmer’s position on dose and image quality. Eur. Radiol. 2014, 24, 969–979. [Google Scholar] [CrossRef] [PubMed]
- Kane, A.G.; Reilly, K.C.; Murphy, T.F. Swimmer’s CT: Improved imaging of the lower neck and thoracic inlet. AJNR Am. J. Neuroradiol. 2004, 25, 859–862. [Google Scholar]
- Deak, P.D.; Smal, Y.; Kalender, W.A. Multisection CT protocols: Sex- and age-specific conversion factors used to determine effective dose from dose-length product. Radiology 2010, 257, 158–166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Niiniviita, H.; Kiljunen, T.; Huuskonen, M.; Teperi, S.; Kulmala, J. Dose monitoring in pediatric and young adult head and cervical spine CT studies at two emergency duty departments. Emerg. Radiol. 2018, 25, 153–159. [Google Scholar] [CrossRef]
- Holroyd, J.R.; Edyvean, S. Doses from cervical spine computed tomography (CT) examinations in the UK. Br. J. Radiol. 2018, 91, 20170834. [Google Scholar] [CrossRef]
- Vilar-Palop, J.; Vilar, J.; Hernández-Aguado, I.; González-Álvarez, I.; Lumbreras, B. Updated effective doses in radiology. J. Radiol. Prot. 2016, 36, 975–990. [Google Scholar] [CrossRef] [PubMed]
- Mettler, F.A., Jr.; Huda, W.; Yoshizumi, T.T.; Mahesh, M. Effective doses in radiology and diagnostic nuclear medicine: A catalog. Radiology 2008, 248, 254–263. [Google Scholar] [CrossRef] [PubMed]
- Metaxas, V.I.; Messaris, G.A.; Lekatou, A.N.; Petsas, T.G. Patient doses in common diagnostic X-ray examinations. Radiat. Prot. Dosim. 2019, 184, 12–27. [Google Scholar] [CrossRef] [PubMed]
- Raine, S.; Twomey, L. Posture of the head, shoulders and thoracic spine in comfortable erect standing. Aust. J. Physiother. 1994, 40, 25–32. [Google Scholar] [CrossRef] [Green Version]
- Raine, S.; Twomey, L.T. Head and shoulder posture variations in 160 asymptomatic women and men. Arch. Phys. Med. Rehabil. 1997, 78, 1215–1223. [Google Scholar] [CrossRef]
- Liu, R.R.; Prado, K.L.; Cody, D. Optimal acquisition parameter selection for CT simulators in radiation oncology. J. Appl. Clin. Med. Phys. 2008, 9, 2878. [Google Scholar] [CrossRef] [PubMed]
| Phantom Study | Patient Study | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Protocol no. | Tube Current (mAs) | CT Dose Index Volume (mGy) | Protocol no. | Tube Current (mAs) | CT Dose Index Volume (mGy) | Dose Length Product (cm*mGy) | Effective Dose (mSv) | ||||||
| Mean SD | Range Min Max | Mean SD | Range Min Max | Mean SD | Range Min Max | ||||||||
| I. | 300 | 34.82 | REFERENCE | 300 | 34.14 ± 0 | 34.14 | 34.14 | 733 ± 253 | 679 | 953 | 4.11 ± 1.29 | 3.47 | 4.87 |
| II. | 150 | 17.41 | STANDARD | 300–10 | 12.44 ± 4.56 | 10.25 | 16.19 | 287 ± 107 | 198 | 374 | 1.46 ± 0.55 | 1.01 | 1.91 |
| III. | 110 | 12.77 | I. | 150–10 | 5.50 ± 2.18 | 3.74 | 7.85 | 125 ± 49 | 76 | 175 | 0.64 ± 0.25 | 0.39 | 0.89 |
| IV. | 80 | 9.28 | II. | 110–10 | 4.77 ± 1.86 | 3.53 | 6.92 | 109 ± 42 | 72 | 149 | 0.56 ± 0.21 | 0.37 | 0.76 |
| V. | 60 | 6.96 | III. | 80–10 | 4.01 ± 1.49 | 3.19 | 5.74 | 92 ± 34 | 65 | 119 | 0.47 ± 0.17 | 0.33 | 0.61 |
| VI. | 40 | 4.64 | IV. | 60–10 | 3.37 ± 1.22 | 2.92 | 4.76 | 78 ± 29 | 60 | 103 | 0.40 ± 0.15 | 0.30 | 0.52 |
| VII. | 20 | 2.32 | V. | 40–10 | 2.60 ± 0.93 | 2.41 | 3.66 | 60 ± 21 | 49 | 76 | 0.31 ± 0.11 | 0.25 | 0.39 |
| VIII. | 10 | 1.16 | VI. | 20–10 | 1.69 ± 0.58 | 1.66 | 2.25 | 39 ± 13 | 34 | 47 | 0.20 ± 0.07 | 0.17 | 0.24 |
| Protocols | Vertebra C3 Axial Sagittal | Vertebra C7 Axial Sagittal | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Range Min Max | Median | p value | Cronbach’s α | Range Min Max | Median | p value | Cronbach’s α | Range Min Max | Median | p value | Cronbach’s α | Range Min Max | Median | p value | Cronbach’s α | |||||
| REFERENCE | 2 | 2 | 2 | - | 1.000 | 2 | 2 | 2 | - | 1.000 | 1 | 2 | 2 | - | 0.836 | 1 | 2 | 2 | - | 0.847 |
| STANDARD | 2 | 2 | 2 | >0.99999 | 1.000 | 2 | 2 | 2 | >0.99999 | 1.000 | 1 | 2 | 2 | 0.15700 | 0.729 | 1 | 2 | 2 | 0.52700 | 0.872 |
| I. | 1 | 2 | 2 | 0.15700 | 0.750 | 1 | 2 | 2 | 0.01600* | 0.902 | 0 | 2 | 1 | <0.00001 * | 0.961 | 0 | 2 | 1 | <0.00001 * | 0.961 |
| II. | 1 | 2 | 2 | 0.25000 | 0.897 | 1 | 2 | 2 | 0.01600 * | 0.943 | 0 | 2 | 1 | <0.00001 * | 0.884 | 0 | 2 | 1 | <0.00001 * | 0.923 |
| III. | 1 | 2 | 2 | 0.12500 | 0.919 | 1 | 2 | 2 | 0.00800 * | 0.943 | 0 | 2 | 1 | <0.00001 * | 0.810 | 0 | 2 | 1 | <0.00001 * | 0.910 |
| IV. | 1 | 2 | 2 | 0.12500 | 0.919 | 1 | 2 | 2 | 0.00800 * | 0.949 | 0 | 2 | 1 | <0.00001* | 0.865 | 0 | 2 | 1 | <0.00001 * | 0.919 |
| V. | 1 | 2 | 2 | 0.01600 * | 0.789 | 1 | 2 | 2 | <0.00001 * | 0.938 | 0 | 2 | 0 | <0.00001 * | 0.789 | 0 | 1 | 0 | <0.00001 * | 0.832 |
| VI. | 1 | 2 | 2 | 0.00200 * | 0.949 | 1 | 2 | 2 | <0.00001 * | 0.826 | 0 | 2 | 0 | <0.00001 * | 0.848 | 0 | 1 | 0 | <0.00001 * | 0.872 |
| Patients | Patients’ Physical Parameters | Protocols | |||||||
|---|---|---|---|---|---|---|---|---|---|
| BMI (kg/m2) | Height (m) | Weight (kg) | Lateral Diameter (cm) | Anteroposterior | Shoulder Position | ||||
| Diameter (cm) | Anatomic | Nominal Value | Vertebra C3 | Vertebra C7 | |||||
| Level | |||||||||
| 1 | 30.9 | 1.8 | 100 | 48 | 26 | C4/5 | 3 | VI. | ST |
| 2 | 27.5 | 1.63 | 73 | 46 | 25 | C4 | 3.5 | VI. | ST |
| 3 | 27.2 | 1.83 | 91 | 47 | 22 | C4/5 | 3 | VI. | ST |
| 4 | 25.5 | 1.75 | 78 | 44 | 22 | C5/6 | 2 | VI. | IV. |
| 5 | 24.9 | 1.69 | 68 | 46 | 19 | “swimmer” | VI. | V. | |
| 6 | 23.8 | 1.8 | 71 | 45 | 20 | C4/5 | 3 | VI. | II. |
| 7 | 21.9 | 1.92 | 80 | 44 | 17 | C5/6 | 2 | VI. | V. |
| 8 | 21.7 | 1.83 | 73 | 44 | 16 | C6/7 | 1 | VI. | V. |
| 9 | 21.4 | 1.87 | 75 | 46 | 20 | C5/6 | 2 | VI. | V. |
| 10 | 20.3 | 1.66 | 56 | 40 | 18 | C4/5 | 3 | VI. | IV. |
| Protocol no. | Tube current (mAs) | Reader—1 | Reader—2 | Reader—3 | Reader—4 | Reader—5 |
|---|---|---|---|---|---|---|
| STANDARD | 300 | 0.042 | 0.042 | 0.038 | 0.038 | 0.038 |
| I. | 150 | 0.042 | 0.042 | 0.038 | 0.038 | 0.038 |
| II. | 110 | 0.042 | 0.042 | 0.038 | 0.038 | 0.038 |
| III. | 80 | 0.042 | 0.042 | 0.042 | 0.042 | 0.038 |
| IV. | 60 | 0.042 | 0.042 | 0.042 | 0.042 | 0.042 |
| V. | 40 | 0.042 | 0.042 | 0.042 | 0.042 | 0.042 |
| VI. | 20 | 0.045 | 0.045 | 0.045 | 0.045 | 0.045 |
| VII. | 10 | 0.045 | 0.045 | 0.045 | 0.045 | 0.045 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Deak, Z.; Brummund, L.; Kirchhoff, S.; Körner, M.; Geyer, L.; Mück, F.; Scaglione, M.; Reiser, M.; Linsenmaier, U. Is It Possible to Replace Conventional Radiography (CR) with a Dose Neutral Computed Tomography (CT) of the Cervical Spine in Emergency Radiology—An Experimental Cadaver Study. Diagnostics 2022, 12, 1872. https://doi.org/10.3390/diagnostics12081872
Deak Z, Brummund L, Kirchhoff S, Körner M, Geyer L, Mück F, Scaglione M, Reiser M, Linsenmaier U. Is It Possible to Replace Conventional Radiography (CR) with a Dose Neutral Computed Tomography (CT) of the Cervical Spine in Emergency Radiology—An Experimental Cadaver Study. Diagnostics. 2022; 12(8):1872. https://doi.org/10.3390/diagnostics12081872
Chicago/Turabian StyleDeak, Zsuzsanna, Lindis Brummund, Sonja Kirchhoff, Markus Körner, Lucas Geyer, Fabian Mück, Mariano Scaglione, Maximilian Reiser, and Ulrich Linsenmaier. 2022. "Is It Possible to Replace Conventional Radiography (CR) with a Dose Neutral Computed Tomography (CT) of the Cervical Spine in Emergency Radiology—An Experimental Cadaver Study" Diagnostics 12, no. 8: 1872. https://doi.org/10.3390/diagnostics12081872
APA StyleDeak, Z., Brummund, L., Kirchhoff, S., Körner, M., Geyer, L., Mück, F., Scaglione, M., Reiser, M., & Linsenmaier, U. (2022). Is It Possible to Replace Conventional Radiography (CR) with a Dose Neutral Computed Tomography (CT) of the Cervical Spine in Emergency Radiology—An Experimental Cadaver Study. Diagnostics, 12(8), 1872. https://doi.org/10.3390/diagnostics12081872







