Endoscopic Diagnosis and Management of Barrett’s Esophagus with Low-Grade Dysplasia
Abstract
1. Introduction
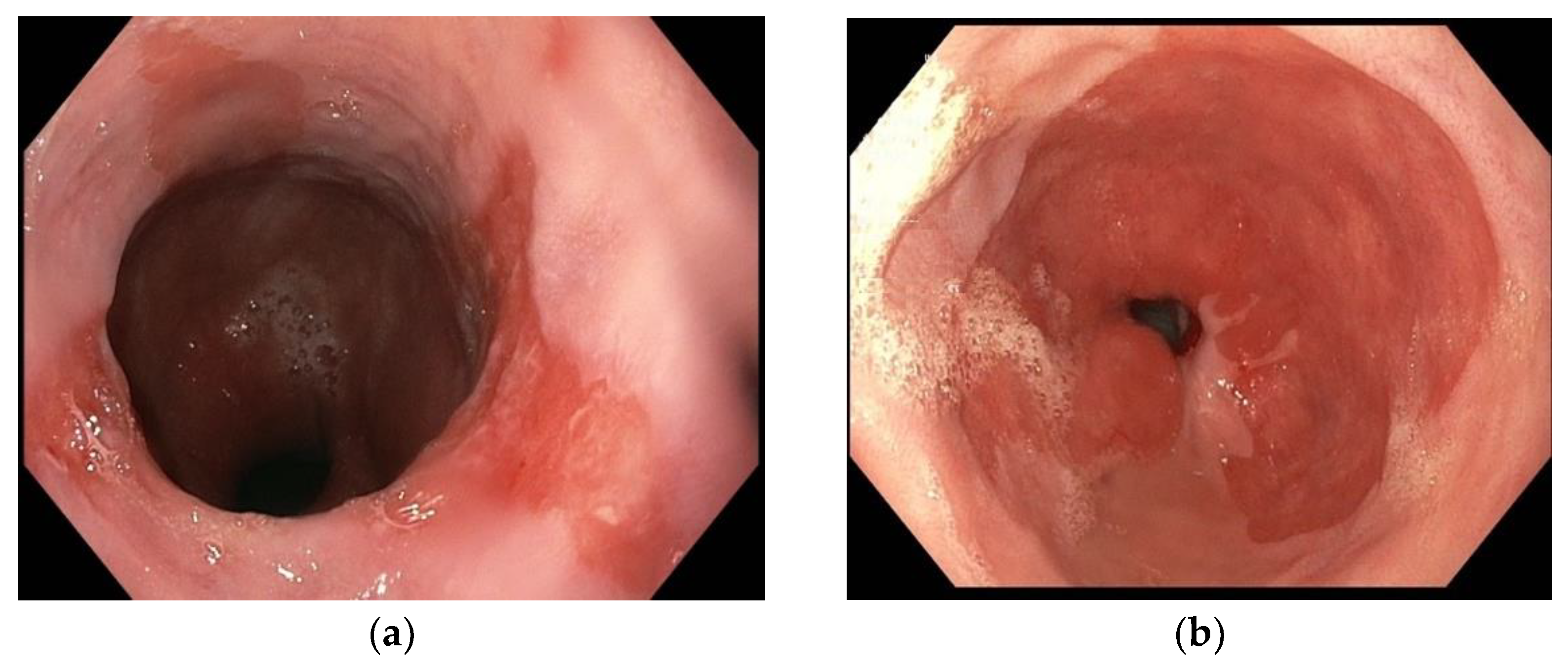
2. Diagnosis
3. Management
| Study | Patients | Achievement of CE-D (%) | Recurrence after CE-D (%) | Number of Sessions for CE-D (Median) | |
|---|---|---|---|---|---|
| Konda et al. [53] | EMR | 107 | 80% (80/107) | 8.1% (9/107) | - |
| Gerke et al. [54] | EMR | 41 | 85.4% (36/41) | 21.9% (9/41) | 2.4 |
| Shaheen et al. [47] | RFA | 42 | 90.5% (38/42) | 5% (2/42) | - |
| Shaheen et al. [62] | RFA | 52 | 98% (51/52) | - | - |
| Phoa et al. [43] | RFA | 68 | 92.6% (63/68) | 1.5% (1/68) | - |
| Small et al. [44] | RFA | 45 | 95.6% (43/45) | 2.2% (1/45) | 2 |
| Vliebergh et al. [63] | RFA | 342 | 93% (318/342) | - | 2 |
| Ghorbani et al. [79] | LNSC | 23 | 91% (21/23) | - | 2.9 |
| Westerlvald et al. [83] | CRYO | 75 | 93.8% (70/75) | - | 1.5 |
| Thota et al. [85] | RFA | 73 | 87.5% (63/73) | 11.1% (7/73) | 3 |
| LNSC | 81 | 78.9% (63/81) | 14.3% (9/81) | 3 | |
| Fasullo et al. [84] | RFA | 100 | 81% (81/100) | 11.1% (11/100) | 2.5 |
| LNSC | 62 | 71% (44/62) | 13.6% (8/62) | 4.8 | |
| van Munster et al. [87] | RFA | 26 | 90% (23/26) | - | - |
| CRYO | 20 | 88% (17/20) | - | - | |
| Manner et al. [91] | Hybrid-APC | 50 | 96% (48/50) | - | 3.5 |
| Wronska et al. [93] | Hybrid-APC | 71 | 93% (66/71) | 4% (3/71) | 2 |
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Cholapranee, A.; Trinidade, A.J. Challenges in Endoscopic Therapy of Dysplastic Barrett’s Esophagus. Curr. Treat Options Gastroenterol. 2019, 17, 32–47. [Google Scholar] [CrossRef] [PubMed]
- De Palma, G.D. Management strategies of Barrett’s esophagus. World J. Gastroenterol. 2012, 18, 6216–6225. [Google Scholar] [CrossRef] [PubMed]
- Shaheen, N.J.; Falk, G.W.; Iyer, P.G. ACG Clinical Guideline: Diagnosis and Management of Barrett’s Esophagus. Am. J. Gastroenterol. 2016, 111, 30–50. [Google Scholar] [CrossRef] [PubMed]
- Hameeteman, W.; Tytgat, G.N.; Houthoff, H.J.; Van Den Tweel, J.G. Barrett’s esophagus: Development of dysplasia and adenocarcinoma. Gastroenterology 1989, 96, 1249–1256. [Google Scholar] [CrossRef]
- Pandey, G.; Mulla, M.; Lewis, W.G. Systematic review and meta-analysis of the effectiveness of radiofrequency ablation in low grade dysplastic Barrett’s esophagus. Endoscopy 2018, 50, 953–960. [Google Scholar] [CrossRef]
- Anand, O.; Wani, S.; Sharma, P. When and how to grade Barrett’s columnar metaplasia: The Prague system. Best Pract. Res. Clin. Gastroenterol. 2008, 22, 661–669. [Google Scholar] [CrossRef]
- Levine, D.S.; Blount, P.L.; Rudolph, R.E. Safety of a systematic endoscopic biopsy protocol in patients with Barrett’s esophagus. Am. J. Gastroenterol. 2000, 95, 1152–1157. [Google Scholar] [CrossRef]
- Khieu, M.; Mukherjee, S. Barrett Esophagus; StatPearls Publishing LLC: Treasure Island, FL, USA, 2021; Volume 11. [Google Scholar]
- Kaye, P.; Haider, S.; Ilyas, M. Barrett’s dysplasia and the Vienna classification: Reproducibility, prediction of progression and impact of consensus reporting and p53 immunohistochemistry. Histopathology 2009, 54, 699–712. [Google Scholar] [CrossRef]
- Tsoi, E.; Williams, R.; Christie, M. Not all low grade dysplasia in Barrett’s oesophagus is the same: Using specific histological criteria in predicting progression to neoplasia. Pathology 2021, 53, 700–704. [Google Scholar] [CrossRef]
- Ten Kate, F.; Nieboer, D.; Ten Kate, F. Improved Progression Prediction in Barrett’s Esophagus with Low-grade Dysplasia Using Specific Histologic Criteria. Am. J. Surg. Pathol. 2018, 42, 918–926. [Google Scholar] [CrossRef]
- Vennalaganti, P.; Kanakadandi, V.; Goldblum, J. Discordance among Pathologists in the United States and Europe in Diagnosis of Low-Grade Dysplasia for Patients with Barrett’s Esophagus. Gastroenterology 2017, 152, 564–570. [Google Scholar] [CrossRef] [PubMed]
- Wani, S.; Rubenstein, J.; Vieth, M. Diagnosis and Management of Low-Grade Dysplasia in Barrett’s Esophagus: Expert Review from the Clinical Practice Updates Committee of the American Gastroenterological Association. Gastroenterology 2016, 151, 822–835. [Google Scholar] [CrossRef] [PubMed]
- Kolb, J.M.; Wani, S. Barrett’s esophagus: Current standards in advanced imaging. Transl. Gastroenterol. Hepatol. 2021, 6, 14. [Google Scholar] [CrossRef] [PubMed]
- Nogales, O.; Caballero-Marcos, A.; Clemente-Sánchez, A. Usefulness of Non-magnifying Narrow Band Imaging in EVIS EXERA III Video Systems and High-Definition Endoscopes to Diagnose Dysplasia in Barrett’s Esophagus Using the Barrett International NBI Group (BING) Classification. Dig. Dis. Sci. 2017, 62, 2840–2846. [Google Scholar] [CrossRef] [PubMed]
- Espino, A.; Cirocco, M.; Dacosta, R. Advanced imaging technologies for the detection of dysplasia and early cancer in barrett esophagus. Clin. Endosc. 2014, 47, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Canto, M.I.; Setrakian, S.; Petras, R.E. Methylene blue selectively stains intestinal metaplasia in Barrett’s esophagus. Gastrointest. Endosc. 1996, 44, 1–7. [Google Scholar] [CrossRef]
- Chedgy, F.J.; Subramaniam, S.; Kandiah, K. Acetic acid chromoendoscopy: Improving neoplasia detection in Barrett’s esophagus. World J. Gastroenterol. 2016, 22, 5753–5760. [Google Scholar] [CrossRef][Green Version]
- Longcroft-Wheaton, G.; Brown, J.; Basford, P. Duration of acetowhitening as a novel objective tool for diagnosing high risk neoplasia in Barrett’s esophagus: A prospective cohort trial. Endoscopy 2013, 45, 426–432. [Google Scholar] [CrossRef]
- Pohl, J.; May, A.; Rabenstein, T. Comparison of computed virtual chromoendoscopy and conventional chromoendoscopy with acetic acid for detection of neoplasia in Barrett’s esophagus. Endoscopy 2007, 39, 594–598. [Google Scholar] [CrossRef]
- Mannath, J.; Subramanian, V.; Hawkey, C.J. Narrow band imaging for characterization of high grade dysplasia and specialized intestinal metaplasia in Barrett’s esophagus: A meta-analysis. Endoscopy 2010, 42, 351–359. [Google Scholar] [CrossRef]
- Qumseya, B.J.; Wang, H.; Badie, N. Advanced imaging technologies increase detection of dysplasia and neoplasia in patients with Barrett’s esophagus: A meta-analysis and systematic review. Clin. Gastroenterol. Hepatol. 2013, 11, 1562–1570. [Google Scholar] [CrossRef] [PubMed]
- Shailendra, S.C.; Barham, K.A.; Yasser, M.B. Confocal laser endomicroscopy. Gastrointest. Endosc. 2014, 80, 928–938. [Google Scholar]
- Urquhart, P.; DaCosta, R.; Marcon, N. Endoscopic mucosal imaging of gastrointestinal neoplasia in 2013. Curr. Gastroenterol. Rep. 2013, 15, 330. [Google Scholar] [CrossRef] [PubMed]
- De Palma, G.D. Confocal laser endomicroscopy in the “in vivo” histological diagnosis of the gastrointestinal tract. World J. Gastroenterol. 2009, 15, 5770–5775. [Google Scholar] [CrossRef]
- Sharma, P.; Meining, A.R.; Coron, E. Real-time increased detection of neoplastic tissue in Barrett’s esophagus with probe-based confocal laser endomicroscopy: Final results of an international multicenter, prospective, randomized, controlled trial. Gastrointest. Endosc. 2011, 74, 465–472. [Google Scholar] [CrossRef]
- Pohl, H.; Rösch, T.; Vieth, M. Miniprobe confocal laser microscopy for the detection of invisible neoplasia in patients with Barrett’s oesophagus. Gut 2008, 57, 1648–1653. [Google Scholar] [CrossRef]
- Bajbouj, M.; Vieth, M.; Rösch, T. Probe-based confocal laser endomicroscopy compared with standard four-quadrant biopsy for evaluation of neoplasia in Barrett’s esophagus. Endoscopy 2010, 42, 435–440. [Google Scholar] [CrossRef]
- Dunbar, K.B.; Okolo, P., 3rd; Montgomery, E. Confocal laser endomicroscopy in Barrett’s esophagus and endoscopically inapparent Barrett’s neoplasia: A prospective, randomized, double-blind, controlled, crossover trial. Gastrointest. Endosc. 2009, 70, 645–654. [Google Scholar] [CrossRef]
- Kiesslich, R.; Gossner, L.; Goetz, M. In vivo histology of Barrett’s esophagus and associated neoplasia by confocal laser endomicroscopy. Clin. Gastroenterol. Hepatol. 2006, 4, 979–987. [Google Scholar] [CrossRef]
- ASGE Technology Committee; Thosani, N.; Abu Dayyeh, B. ASGE Technology Committee systematic review and meta-analysis assessing the ASGE Preservation and Incorporation of Valuable Endoscopic Innovations thresholds for adopting real-time imaging-assisted endoscopic targeted biopsy during endoscopic surveillance of Barrett’s esophagus. Gastrointest. Endosc. 2016, 83, 684–698. [Google Scholar]
- De Groof, A.J.; Struyvenberg, M.R.; Can Der Putten, J. Deep-learning system detects neoplasia in patients with Barrett’s esophagus with higher accuracy than endoscopists in a multistep training and validation study with benchmarking. Gastroenterology 2020, 158, 915–929. [Google Scholar] [CrossRef] [PubMed]
- Weston, A.P.; Badr, A.S.; Hassanein, R.S. Prospective multivariate analysis of clinical, endoscopic, and histological factors predictive of the development of Barrett’s multifocal high-grade dysplasia or adenocarcinoma. Am. J. Gastroenterol. 1999, 94, 3413–3419. [Google Scholar] [CrossRef] [PubMed]
- Conio, M.; Blanchi, S.; Lapertosa, G. Long-term endoscopic surveillance of patients with Barrett’s esophagus. Incidence of dysplasia and adenocarcinoma: A prospective study. Am. J. Gastroenterol. 2003, 98, 1931–1939. [Google Scholar] [CrossRef] [PubMed]
- Skacel, M.; Petras, R.; Gramlich, T. The diagnosis of low-grade dysplasia in Barrett’s esophagus and its implication for disease progression. Am. J. Gastroenterol. 2000, 92, 3383–3387. [Google Scholar] [CrossRef] [PubMed]
- Wani, S.; Falk, G.W.; Post, J. Risk factors for progression of low-grade dysplasia in patients with Barrett’s esophagus. Gastroenterology 2011, 141, 1179–1186. [Google Scholar] [CrossRef]
- Weusten, B.; Bisschops, R.; Coron, E. Endoscopic management of Barrett’s esophagus: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy 2017, 49, 191–198. [Google Scholar] [CrossRef]
- Qumseya, B.; Sultan, S.; Bain, P. ASGE guideline on screening and surveillance of Barrett’s esophagus. Gastrointest. Endosc. 2019, 90, 335–359. [Google Scholar] [CrossRef]
- Gupta, S.; Li, D.; El Serag, H. AGA Clinical Practice Guidelines on Management of Gastric Intestinal Metaplasia. Gastroenterology 2020, 158, 693–702. [Google Scholar] [CrossRef]
- Ishihara, R.; Arima, M.; Iizuka, T. Endoscopic submucosal dissection/endoscopic mucosal resection guidelines for esophageal cancer. Dig. Endosc. 2020, 32, 452–493. [Google Scholar] [CrossRef]
- Kew, G.S.; Soh, A.Y.S.; Lee, Y.Y. Multinational survey on the preferred approach to management of Barrett’s esophagus in the Asia-Pacific region. World J. Gastrointest. Oncol. 2021, 13, 279–294. [Google Scholar] [CrossRef]
- Klair, J.S.; Zafar, Y.; Nagra, N. Outcomes of Radiofrequency Ablation versus Endoscopic Surveillance for Barrett’s Esophagus with Low-Grade Dysplasia: A Systematic Review and Meta-Analysis. Dig. Dis. 2021, 39, 561–568. [Google Scholar] [CrossRef] [PubMed]
- Phoa, K.N.; Van Vilsteren, F.G.; Weusten, B.L. Radiofrequency ablation vs. endoscopic surveillance for patients with Barrett esophagus and low-grade dysplasia: A randomized clinical trial. JAMA 2014, 311, 1209–1217. [Google Scholar] [CrossRef] [PubMed]
- Small, A.J.; Araujo, J.L.; Leggett, C.L. Radiofrequency ablation is associated with decreased neoplastic progression in patients with Barrett’s esophagus and confirmed low-grade dysplasia. Gastroenterology 2015, 149, 567–576. [Google Scholar] [CrossRef] [PubMed]
- Barret, M.; Pioche, M.; Terris, B. Endoscopic radiofrequency ablation or surveillance in patients with Barrett’s oesophagus with confirmed low-grade dysplasia: A multicentre randomised trial. Gut 2021, 70, 1014–1022. [Google Scholar] [CrossRef] [PubMed]
- Pouw, R.E.; Wirths, K.; Eisendrath, P. Efficacy of radiofrequency ablation combined with endoscopic resection for Barrett’s esophagus with early neoplasia. Clin. Gastroenterol. Hepatol. 2010, 8, 23–29. [Google Scholar] [CrossRef]
- Shaheen, N.J.; Sharma, P.; Overholt, B.F. Radiofrequency ablation in Barrett’s esophagus with dysplasia. N. Engl. J. Med. 2009, 360, 2277–2288. [Google Scholar] [CrossRef]
- Kahn, A.; Al-Qaisi, M.; Kommineni, V.T. Longitudinal outcomes of radiofrequency ablation versus surveillance endoscopy for Barrett’s esophagus with low-grade dysplasia. Dis. Esophagus 2018, 31, 31. [Google Scholar] [CrossRef]
- Wani, S.; Qumseya, B.; Sultan, S. Endoscopic eradication therapy for patients with Barrett’s esophagus-associated dysplasia and intramucosal cancer. Gastrointest. Endosc. 2018, 87, 907–931. [Google Scholar] [CrossRef]
- Dam, A.N.; Klapman, J. A narrative review of Barrett’s esophagus in 2020, molecular and clinical update. Ann. Transl. Med. 2020, 8, 1107. [Google Scholar] [CrossRef]
- Zehetner, J.; DeMeester, S.R.; Hagen, J.A. Endoscopic resection and ablation versus esophagectomy for high-grade dysplasia and intramucosal adenocarcinoma. J. Thorac. Cardiovasc. Surg. 2011, 141, 39–47. [Google Scholar] [CrossRef]
- Maione, F.; Chini, A.; Milone, M. Diagnosis and Management of Rectal Neuroendocrine Tumors (NETs). Diagnostics 2021, 11, 771. [Google Scholar] [CrossRef] [PubMed]
- Konda, V.J.; Gonzalez Haba Ruiz, M.; Koons, A. Complete endoscopic mucosal resection is effective and durable treatment for Barrett’s-associated neoplasia. Clin. Gastroenterol. Hepatol. 2014, 12, 2002–2010. [Google Scholar] [CrossRef] [PubMed]
- Gerke, H.; Siddiqui, J.; Nasr, I. Efficacy and safety of EMR to completely remove Barrett’s esophagus: Experience in 41 patients. Gastrointest. Endosc. 2011, 74, 761–771. [Google Scholar] [CrossRef] [PubMed]
- Soehendra, N.; Seewald, S.; Groth, S. Use of modified multiband ligator facilitates circumferential EMR in Barrett’s esophagus (with video). Gastrointest. Endosc. 2006, 63, 847–852. [Google Scholar] [CrossRef]
- Zeki, S.S.; Bergman, J.J.; Dunn, J.M. Endoscopic management of dysplasia and early oesophageal cancer. Best Pract. Res. Clin. Gastroenterol. 2018, 36, 27–36. [Google Scholar] [CrossRef]
- Moss, A.; Bourke, M.J.; Hourigan, L.F. Endoscopic resection for Barrett’s high-grade dysplasia and early esophageal adenocarcinoma: An essential staging procedure with long-term therapeutic benefit. Am. J. Gastroenterol. 2010, 105, 1276–1283. [Google Scholar] [CrossRef]
- Wani, S.; Abrams, J.; Edmundowicz, S.A. Endoscopic mucosal resection results in change of histologic diagnosis in Barrett’s esophagus patients with visible and flat neoplasia: A multicenter cohort study. Dig. Dis. Sci. 2013, 58, 1703–1709. [Google Scholar] [CrossRef]
- Sayana, H.; Wani, S.; Keighley, J. Endoscopic mucosal resection (EMR) as a diagnostic tool in Barrett’s esophagus (BE) patients with high-grade dysplasia (HGD) and early esophageal adenocarcinoma (EAC): A systematic review. Gastroenterology 2008, 132, W1878. [Google Scholar] [CrossRef]
- Brown, J.; Alsop, B.; Gupta, N. Effectiveness of focal vs. balloon radiofrequency ablation devices in the treatment of Barrett’s esophagus. United Eur. Gastroenterol. J. 2016, 4, 236–241. [Google Scholar] [CrossRef]
- Orman, E.S.; Li, N.; Shaheen, N.J. Efficacy and durability of radiofrequency ablation for Barrett’s Esophagus: Systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 2013, 11, 1245–1255. [Google Scholar] [CrossRef]
- Shaheen, N.J.; Overholt, B.F.; Sampliner, R.E. Durability of radiofrequency ablation in Barrett’s esophagus with dysplasia. Gastroenterology 2011, 141, 460–468. [Google Scholar] [CrossRef] [PubMed]
- Vliebergh, J.H.; Deprez, P.H.; De Looze, D. Efficacy and safety of radiofrequency ablation of Barrett’s esophagus in the absence of reimbursement: A multicenter prospective Belgian registry. Endoscopy 2019, 51, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Desai, M.; Saligram, S.; Gupta, N. Efficacy and safety outcomes of multimodal endoscopic eradication therapy in Barrett’s esophagus-related neoplasia: A systematic review and pooled analysis. Gastrointest. Endosc. 2017, 85, 482–495. [Google Scholar] [CrossRef] [PubMed]
- Haidry, R.J.; Butt, M.A.; Dunn, J.M. UK RFA Registry. Improvement over time in outcomes for patients undergoing endoscopic therapy for Barrett’s oesophagus-related neoplasia: 6-year experience from the first 500 patients treated in the UK patient registry. Gut 2015, 64, 1192–1199. [Google Scholar] [CrossRef] [PubMed]
- Chadwick, G.; Groene, O.; Markar, S.R. Systematic review comparing radiofrequency ablation and complete endoscopic resection in treating dysplastic Barrett’s esophagus: A critical assessment of histologic outcomes and adverse events. Gastrointest. Endosc. 2014, 19, 718–731. [Google Scholar] [CrossRef] [PubMed]
- Qumseya, B.J.; Wani, S.; Desai, M. Adverse Events after Radiofrequency Ablation in Patients with Barrett’s Esophagus: A Systematic Review and Meta-analysis. Clin. Gastroenterol. Hepatol. 2016, 14, 1086–1095. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, C.R.; Triadafilopoulos, G. Endoscopic treatments for dysplastic Barrett’s esophagus: Resection, ablation, what else? World J. Surg. 2015, 39, 597–605. [Google Scholar] [CrossRef]
- Gupta, M.; Iyer, P.G.; Lutzke, L. Recurrence of esophageal intestinal metaplasia after endoscopic mucosal resection and radiofrequency ablation of Barrett’s esophagus: Results from a US Multicenter Consortium. Gastroenterology 2013, 145, 79–86. [Google Scholar] [CrossRef]
- Orman, E.S.; Kim, H.P.; Bulsiewicz, W.J. Intestinal metaplasia recurs infrequently in patients successfully treated for Barrett’s esophagus with radiofrequency ablation. Am. J. Gastroenterol. 2013, 108, 187–195. [Google Scholar] [CrossRef]
- Cotton, C.C.; Wolf, W.A.; Overholt, B.F. AIM Dysplasia Trial Group. Late Recurrence of Barrett’s Esophagus after Complete Eradication of Intestinal Metaplasia is Rare: Final Report from Ablation in Intestinal Metaplasia Containing Dysplasia Trial. Gastroenterology 2017, 153, 681–688. [Google Scholar] [CrossRef]
- Cotton, C.C.; Haidry, R.; Thrift, A.P. Development of Evidence-Based Surveillance Intervals After Radiofrequency Ablation of Barrett’s Esophagus. Gastroenterology 2018, 155, 316–326. [Google Scholar] [CrossRef] [PubMed]
- Sami, S.S.; Ravindran, A.; Kahn, A. Timeline and location of recurrence following successful ablation in Barrett’s oesophagus: An international multicentre study. Gut 2019, 68, 1379–1385. [Google Scholar] [CrossRef] [PubMed]
- Mohy-Ud-Din, N.; Krill, T.S.; Shah, A.R. Barrett’s esophagus: What do we need to know? Dis. Mon. 2020, 66, 100850. [Google Scholar] [CrossRef] [PubMed]
- Lal, P.; Thota, P.N. Cryotherapy in the management of premalignant and malignant conditions of the esophagus. World J. Gastroenterol. 2018, 24, 4862–4869. [Google Scholar] [CrossRef] [PubMed]
- Johnston, C.M.; Schoenfeld, L.P.; Mysore, J.V. Endoscopic spray cryotherapy: A new technique for mucosal ablation in the esophagus. Gastrointest. Endosc. 1999, 50, 86–92. [Google Scholar] [CrossRef]
- Das, K.K.; Falk, G.W. Long-term outcomes for cryotherapy in Barrett’s esophagus with high-grade dysplasia: Just cracking the ice. Gastrointest. Endosc. 2017, 86, 633–635. [Google Scholar] [CrossRef][Green Version]
- Trindade, A.J.; Pleskow, D.K.; Sengupta, N. Efficacy of liquid nitrogen cryotherapy for Barrett’s esophagus after endoscopic resection of intramucosal cancer: A multicenter study. J. Gastroenterol. Hepatol. 2018, 33, 461–465. [Google Scholar] [CrossRef]
- Ghorbani, S.; Tsai, F.C.; Greenwald, B.D. Safety and efficacy of endoscopic spray cryotherapy for Barrett’s dysplasia: Results of the National Cryospray Registry. Dis. Esophagus 2016, 29, 241–247. [Google Scholar] [CrossRef]
- Mohan, B.P.; Krishnamoorthi, R.; Ponnada, S. Liquid Nitrogen Spray Cryotherapy in Treatment of Barrett’s Esophagus, where do we stand? A Systematic Review and Meta-Analysis. Dis. Esophagus. 2019, 32, doy130. [Google Scholar] [CrossRef]
- Hamade, N.; Desai, M.; Thoguluva Chandrasekar, V. Efficacy of cryotherapy as first line therapy in patients with Barrett’s neoplasia: A systematic review and pooled analysis. Dis. Esophagus 2019, 32, doz040. [Google Scholar] [CrossRef]
- Tariq, R.; Enslin, S.; Hayat, M. Efficacy of Cryotherapy as a Primary Endoscopic Ablation Modality for Dysplastic Barrett’s Esophagus and Early Esophageal Neoplasia: A Systematic Review and Meta-Analysis. Cancer Control 2020, 27, 1073274820976668. [Google Scholar] [CrossRef] [PubMed]
- Westerveld, D.R.; Nguyen, K.; Banerjee, D. Safety and effectiveness of balloon cryoablation for treatment of Barrett’s associated neoplasia: Systematic review and meta-analysis. Endosc. Int. Open. 2020, 8, E172–E178. [Google Scholar] [CrossRef] [PubMed]
- Fasullo, M.; Shah, T.; Patel, M. Outcomes of Radiofrequency Ablation Compared to Liquid Nitrogen Spray Cryotherapy for the Eradication of Dysplasia in Barrett’s Esophagus. Dig. Dis. Sci. 2021, 1–7. [Google Scholar] [CrossRef]
- Thota, P.N.; Arora, Z.; Dumot, J.A. Cryotherapy and Radiofrequency Ablation for Eradication of Barrett’s Esophagus with Dysplasia or Intramucosal Cancer. Dig. Dis. Sci. 2018, 63, 1311–1319. [Google Scholar] [CrossRef]
- Solomon, S.S.; Kothari, S.; Smallfield, G.B. Liquid Nitrogen Spray Cryotherapy is associated with Less Postprocedural Pain Than Radiofrequency Ablation in Barrett’s Esophagus: A Multicenter Prospective Study. J. Clin. Gastroenterol. 2019, 53, e84–e90. [Google Scholar] [CrossRef]
- Van Munster, S.N.; Overwater, A.; Haidry, R. Focal cryoballoon versus radiofrequency ablation of dysplastic Barrett’s esophagus: Impact on treatment response and postprocedural pain. Gastrointest. Endosc. 2018, 88, 795–803. [Google Scholar] [CrossRef] [PubMed]
- Sengupta, N.; Ketwaroo, G.A.; Bak, D.M. Salvage cryotherapy after failed radiofrequency ablation for Barrett’s esophagus-related dysplasia is safe and effective. Gastrointest. Endosc. 2015, 82, 443–448. [Google Scholar] [CrossRef]
- Visrodia, K.; Zakko, L.; Wang, K.K. Mucosal Ablation in Patients with Barrett’s Esophagus: Fry or Freeze? Dig. Dis. Sci. 2018, 63, 2129–2135. [Google Scholar] [CrossRef]
- Trindade, A.J.; Inamdar, S.; Kothari, S. Feasibility of liquid nitrogen cryotherapy after failed radiofrequency ablation for Barrett’s esophagus. Dig. Endosc. 2017, 29, 680–685. [Google Scholar] [CrossRef]
- Manner, H.; May, A.; Kouti, I. Efficacy and safety of Hybrid-APC for the ablation of Barrett’s esophagus. Surg. Endosc. 2016, 30, 1364–1370. [Google Scholar] [CrossRef]
- Estifan, E.; Cavanagh, Y.; Grossman, M.A. Hybrid Argon Plasma Coagulation for Treatment of Gastric Intestinal Metaplasia. Cureus 2020, 12, e7427. [Google Scholar] [CrossRef] [PubMed]
- Wronska, E.; Polkowski, M.; Orlowska, J. Argon plasma coagulation for Barrett’s esophagus with low-grade dysplasia: A randomized trial with long-term follow-up on the impact of power setting and proton pump inhibitor dose. Endoscopy 2021, 53, 123–132. [Google Scholar] [PubMed]

| Category | Diagnosis |
|---|---|
| 1 | Negative for neoplasia (ND) |
| 2 | Indefinite for neoplasia (ID) |
| 3 | Mucosal low-grade neoplasia (LGD) Low-grade adenoma Low-grade dysplasia |
| 4 | Mucosal high-grade neoplasia (HGD) |
| 4.1 | High-grade adenoma/dysplasia |
| 4.2 | Non-invasive carcinoma (carcinoma in situ) |
| 4.3 | Suspicious for invasive carcinoma |
| 4.4 | Intramucosal carcinoma |
| 5 | Submucosal invasion by carcinoma |
| Study | Patients | Time of Follow-Up | Ratio of Disease Progression with RFA to HGD | Ratio of Disease Progression with RFA to IMC/EAC | Ratio of Disease Progression with Surveillance to HGD | Ratio of Disease Progression with Surveillance to IMC/EAC | CE-D in RFA Group (%) | CE-D in Surveillance Group (%) | |
|---|---|---|---|---|---|---|---|---|---|
| Barret et al., [45] | Randomized trial | 82 | 36 months | 5/40 | - | 11/42 | - | - | - |
| Phoa et al., [43] | Randomized trial | 136 | 36 months | 1/68 | 1/68 | 18/68 | 6/68 | 98.4% | 27.9% |
| Pouw et al., [46] | Randomized trial | 136 | 22 months | 0/68 | 0/68 | 4/68 | 1/68 | 95% | - |
| Shaheen et al., [47] | Randomized trial | 64 | 12 months | 2/42 | 0/42 | 3/22 | 0/22 | 90.5% | 22.7% |
| Small et al., [44] | Retrospective study | 170 | 28 months | 0/45 | 1/45 | 29/125 | 7/125 | 95.6% | 31.2% |
| Kahn et al., [48] | Retrospective study | 173 | 90 months | 7/79 | 14/94 | 97.5% | 61.7% | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maione, F.; Chini, A.; Maione, R.; Manigrasso, M.; Marello, A.; Cassese, G.; Gennarelli, N.; Milone, M.; De Palma, G.D. Endoscopic Diagnosis and Management of Barrett’s Esophagus with Low-Grade Dysplasia. Diagnostics 2022, 12, 1295. https://doi.org/10.3390/diagnostics12051295
Maione F, Chini A, Maione R, Manigrasso M, Marello A, Cassese G, Gennarelli N, Milone M, De Palma GD. Endoscopic Diagnosis and Management of Barrett’s Esophagus with Low-Grade Dysplasia. Diagnostics. 2022; 12(5):1295. https://doi.org/10.3390/diagnostics12051295
Chicago/Turabian StyleMaione, Francesco, Alessia Chini, Rosa Maione, Michele Manigrasso, Alessandra Marello, Gianluca Cassese, Nicola Gennarelli, Marco Milone, and Giovanni Domenico De Palma. 2022. "Endoscopic Diagnosis and Management of Barrett’s Esophagus with Low-Grade Dysplasia" Diagnostics 12, no. 5: 1295. https://doi.org/10.3390/diagnostics12051295
APA StyleMaione, F., Chini, A., Maione, R., Manigrasso, M., Marello, A., Cassese, G., Gennarelli, N., Milone, M., & De Palma, G. D. (2022). Endoscopic Diagnosis and Management of Barrett’s Esophagus with Low-Grade Dysplasia. Diagnostics, 12(5), 1295. https://doi.org/10.3390/diagnostics12051295







