Prevalence of Monosodium Urate (MSU) Deposits in Cadavers Detected by Dual-Energy Computed Tomography (DECT)
Abstract
1. Introduction
2. Materials and Methods
2.1. Cadavers
2.2. DECT Scan Parameters
2.3. CT and DECT Scoring
- + Head/Neck:
- Cranium/intracerebral vessels, ear cartilage and orbits (lens)
- Supraaortal vessels (Subclavian and Carotid arteries)
- + Body trunk
- Ascending aorta, descending aorta, aortic arch, aortic root, abdominal aorta
- Right coronary artery (RCA), left main artery (LM), circumflex artery (CX) and left anterior descending artery (LAD)
- Tricuspid valve and mitral valve
- Iliac vessels
- Rib cartilages
- Kidney
- + Feet:
- Joints: Metatarsophalangeal (MTP) joints, interphalangeal joints (IP), tibiotalar joint.
- Tendons: Extensor hallucis longus tendon (EHL), tibialis anterior tendon (TAT), tibialis posterior tendon (TPT), flexor hallucis longus tendon (FHL), peroneal tendons (PT), and Achilles tendon (AT).
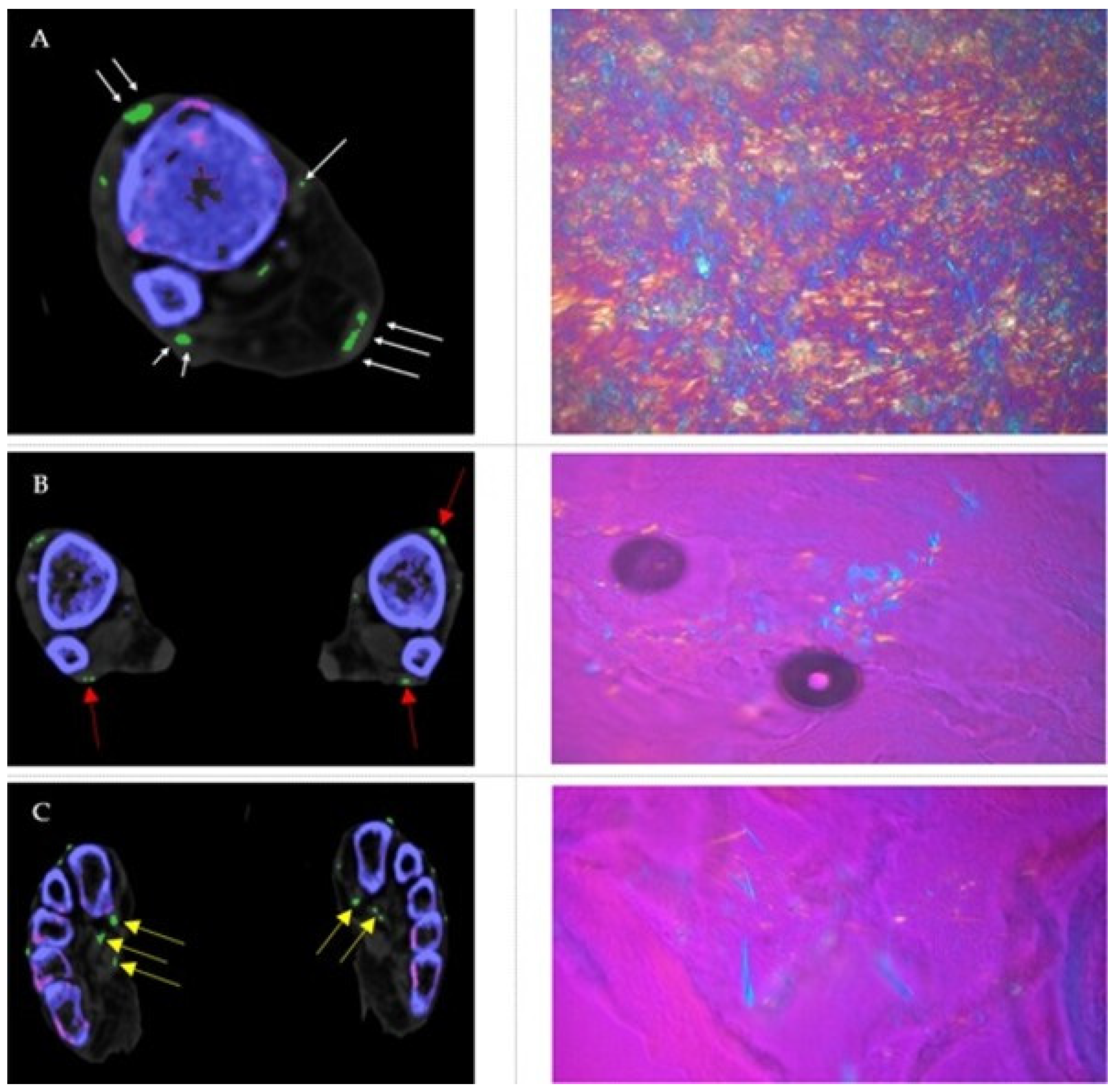
2.4. Polarizing Microscopic Evaluation
2.5. Statistical Analysis
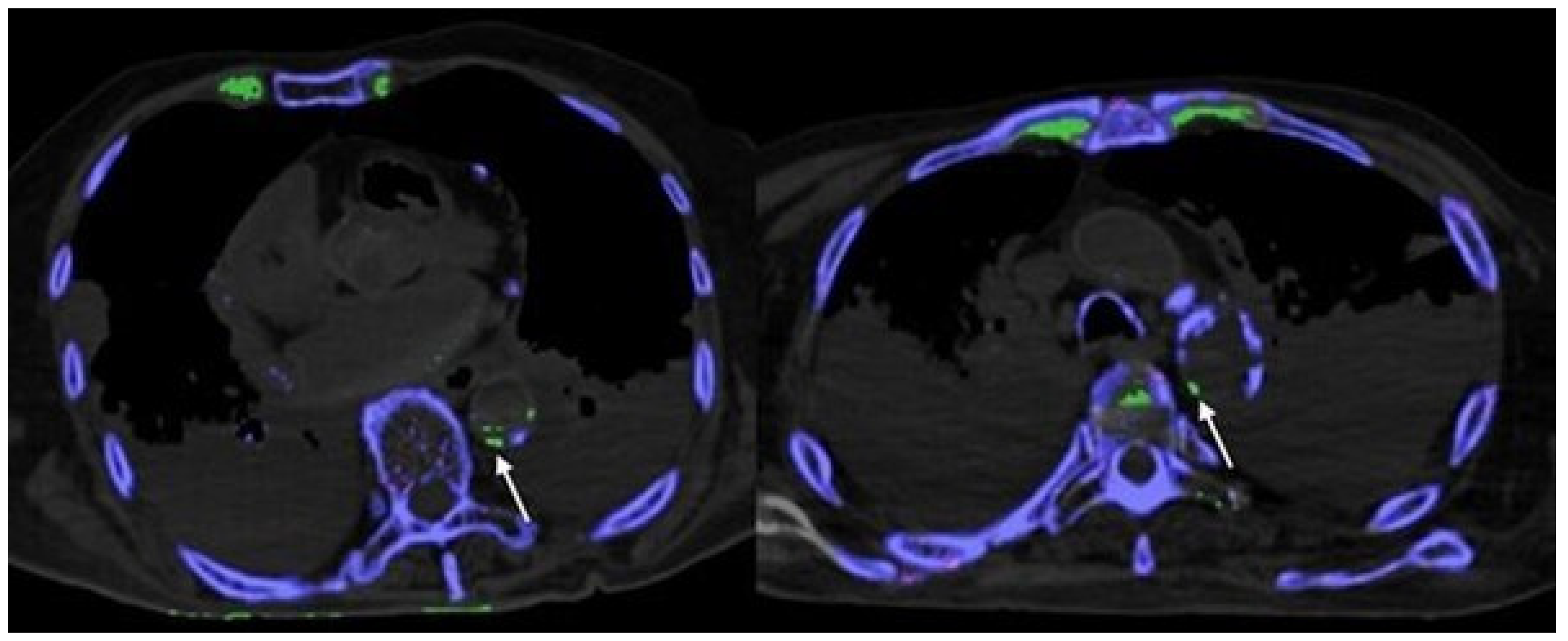
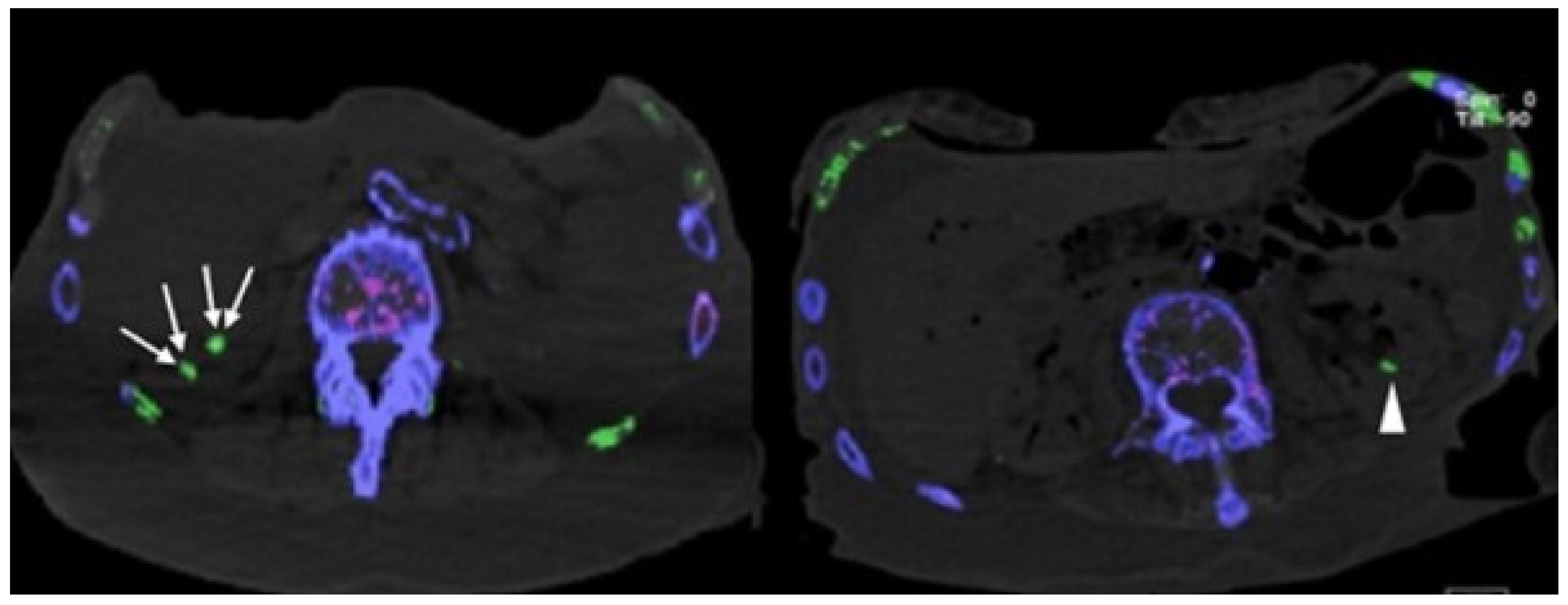
3. Results
3.1. Fresh Cadavers
3.2. Embalmed Cadavers
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Harris, M.D.; Siegel, L.B.; Alloway, J.A. Gout and hyperuricemia. Am. Fam. Phys. 1999, 59, 925–934. [Google Scholar]
- Neogi, T.; Jansen, T.L.; Dalbeth, N.; Fransen, J.; Schumacher, H.R.; Berendsen, D.; Brown, M.; Choi, H.; Edwards, N.L.; Janssens, H.J.E.M.; et al. 2015 Gout classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann. Rheum. Dis. 2015, 74, 1789–1798. [Google Scholar] [CrossRef]
- Richette, P.; Doherty, M.; Pascual, E.; Barskova, V.; Becce, F.; Castaneda, J.; Coyfish, M.; Guillo, S.; Jansen, T.; Janssens, H.; et al. 2018 updated European League Against Rheumatism evidence-based recommendations for the diagnosis of gout. Ann. Rheum. Dis. 2020, 79, 31–38. [Google Scholar] [CrossRef]
- Hu, H.J.; Liao, M.Y.; Xu, L.Y. Clinical utility of dual-energy CT for gout diagnosis. Clin. Imaging 2015, 39, 880–885. [Google Scholar] [CrossRef]
- Schwabl, C.; Taljanovic, M.; Widmann, G.; Teh, J.; Klauser, A.S. Ultrasonography and dual-energy computed tomography: Impact for the detection of gouty deposits. Ultrasonography 2021, 40, 197–206. [Google Scholar] [CrossRef]
- Chhana, A.; Doyle, A.; Sevao, A.; Amirapu, S.; Riordan, P.; Dray, M.; McGlashan, S.; Cornish, J.; Dalbeth, N. Advanced imaging assessment of gout: Comparison of dual-energy CT and MRI with anatomical pathology. Ann. Rheum. Dis. 2018, 77, 629–630. [Google Scholar] [CrossRef]
- Klauser, A.S.; Halpern, E.J.; Strobl, S.; Gruber, J.; Feuchtner, G.; Bellmann-Weiler, R.; Weiss, G.; Stofferin, H.; Jaschke, W. Dual-Energy Computed Tomography Detection of Cardiovascular Monosodium Urate Deposits in Patients With Gout. JAMA Cardiol. 2019, 4, 1019–1028. [Google Scholar] [CrossRef]
- Barazani, S.H.; Chi, W.W.; Pyzik, R.; Chang, H.; Jacobi, A.; O’Donnell, T.; Fayad, Z.A.; Ali, Y.; Mani, V. Quantification of uric acid in vasculature of patients with gout using dual-energy computed tomography. World J. Radiol. 2020, 12, 184–194. [Google Scholar] [CrossRef]
- Khanna, P.; Johnson, R.J.; Marder, B.; LaMoreaux, B.; Kumar, A. Systemic Urate Deposition: An Unrecognized Complication of Gout? J. Clin. Med. 2020, 9, 3204. [Google Scholar] [CrossRef]
- Pascart, T.; Carpentier, P.; Choi, H.K.; Norberciak, L.; Ducoulombier, V.; Luraschi, H.; Houvenagel, E.; Legrand, J.; Verclytte, S.; Becce, F.; et al. Identification and characterization of peripheral vascular color-coded DECT lesions in gout and non-gout patients: The VASCURATE study. Semin. Arthritis Rheum. 2021, 51, 895–902. [Google Scholar] [CrossRef]
- Wang, P.; Smith, S.E.; Garg, R.; Lu, F.; Wohlfahrt, A.; Campos, A.; Vanni, K.; Yu, Z.; Solomon, D.H.; Kim, S.C. Identification of monosodium urate crystal deposits in patients with asymptomatic hyperuricemia using dual-energy CT. RMD Open 2018, 4, e000593. [Google Scholar] [CrossRef]
- Dalbeth, N.; Becce, F.; Botson, J.K.; Zhao, L.; Kumar, A. Dual-energy CT assessment of rapid monosodium urate depletion and bone erosion remodelling during pegloticase plus methotrexate co-therapy. Rheumatology 2022. Online ahead of print. [Google Scholar] [CrossRef]
- Pascart, T.; Budzik, J.F. Dual-energy computed tomography in crystalline arthritis: Knowns and unknowns. Curr. Opin. Rheumatol. 2022, 34, 103–110. [Google Scholar] [CrossRef]
- Tse, J.J.; Kondro, D.A.; Kuczynski, M.T.; Pauchard, Y.; Veljkovic, A.; Holdsworth, D.W.; Frasson, V.; Manske, S.L.; MacMullan, P.; Salat, P. Assessing the Sensitivity of Dual-Energy Computed Tomography 3-Material Decomposition for the Detection of Gout. Investig. Radiol. 2022. Online ahead of print. [Google Scholar] [CrossRef]
- Ahn, S.J.; Zhang, D.; Levine, B.D.; Dalbeth, N.; Pool, B.; Ranganath, V.K.; Benhaim, P.; Nelson, S.D.; Hsieh, S.S.; FitzGerald, J.D. Limitations of dual-energy CT in the detection of monosodium urate deposition in dense liquid tophi and calcified tophi. Skelet. Radiol. 2021, 50, 1667–1675. [Google Scholar] [CrossRef]
- Dubief, B.; Avril, J.; Pascart, T.; Schmitt, M.; Loffroy, R.; Maillefert, J.F.; Ornetti, P.; Ramon, A. Optimization of dual energy computed tomography post-processing to reduce lower limb artifacts in gout. Quant. Imaging Med. Surg. 2022, 12, 539–549. [Google Scholar] [CrossRef]
- Park, E.H.; Yoo, W.H.; Song, Y.S.; Byon, J.H.; Pak, J.; Choi, Y. Not All Green Is Tophi: The Importance of Optimizing Minimum Attenuation and Using a Tin Filter to Minimize Clumpy Artifacts on Foot and Ankle Dual-Energy CT. Am. J. Roentgenol. 2020, 214, 1335–1342. [Google Scholar] [CrossRef]
- Mallinson, P.I.; Coupal, T.; Reisinger, C.; Chou, H.; Munk, P.L.; Nicolaou, S.; Ouellette, H. Artifacts in dual-energy CT gout protocol: A review of 50 suspected cases with an artifact identification guide. Am. J. Roentgenol. 2014, 203, W103–W109. [Google Scholar] [CrossRef]
- Chou, H.; Chin, T.Y.; Peh, W.C. Dual-energy CT in gout–A review of current concepts and applications. J. Med. Radiat. Sci. 2017, 64, 41–51. [Google Scholar] [CrossRef]
- Károlyi, M.; Szilveszter, B.; Kolossváry, M.; Takx, R.A.; Celeng, C.; Bartykowszki, A.; Jermendy, Á.L.; Panajotu, A.; Karády, J.; Raaijmakers, R.; et al. Iterative model reconstruction reduces calcified plaque volume in coronary CT angiography. Eur. J. Radiol. 2017, 87, 83–89. [Google Scholar] [CrossRef]
- Gondrie, M.J.; van der Graaf, Y.; Jacobs, P.C.; Oen, A.L.; Mali, W.P. The association of incidentally detected heart valve calcification with future cardiovascular events. Eur. Radiol. 2011, 21, 963–973. [Google Scholar] [CrossRef]
- Forbess, L.J.; Fields, T.R. The broad spectrum of urate crystal deposition: Unusual presentations of gouty tophi. Semin. Arthritis Rheum. 2012, 42, 146–154. [Google Scholar] [CrossRef]
- Weaver, J.S.; Vina, E.R.; Munk, P.L.; Klauser, A.S.; Elifritz, J.M.; Taljanovic, M.S. Gouty Arthropathy: Review of Clinical Manifestations and Treatment, with Emphasis on Imaging. J. Clin. Med. 2021, 11, 166. [Google Scholar] [CrossRef]
- Gamala, M.; Linn-Rasker, S.P.; Nix, M.; Heggelman, B.G.F.; van Laar, J.M.; Pasker-de Jong, P.C.M.; Jacobs, J.W.G.; Klaasen, R. Gouty arthritis: Decision-making following dual-energy CT scan in clinical practice, a retrospective analysis. Clin. Rheumatol. 2018, 37, 1879–1884. [Google Scholar] [CrossRef]
- Choi, H.K.; Burns, L.C.; Shojania, K.; Koenig, N.; Reid, G.; Abufayyah, M.; Law, G.; Kydd, A.S.; Ouellette, H.; Nicolaou, S. Dual energy CT in gout: A prospective validation study. Ann. Rheum. Dis. 2012, 71, 1466–1471. [Google Scholar] [CrossRef]
- Strobl, S.; Halpern, E.J.; Ellah, M.A.; Kremser, C.; Gruber, J.; Bellmann-Weiler, R.; Deml, C.; Schmalzl, A.; Rauch, S.; Klauser, A.S. Acute Gouty Knee Arthritis: Ultrasound Findings Compared With Dual-Energy CT Findings. Am. J. Roentgenol. 2018, 210, 1323–1329. [Google Scholar] [CrossRef]
- Klauser, A.S.; Halpern, E.J.; Strobl, S.; Abd Ellah, M.M.H.; Gruber, J.; Bellmann-Weiler, R.; Auer, T.; Feuchtner, G.; Jaschke, W. Gout of hand and wrist: The value of US as compared with DECT. Eur. Radiol. 2018, 28, 4174–4181. [Google Scholar] [CrossRef]
- Stewart, S.; Dalbeth, N.; Vandal, A.C.; Rome, K. The first metatarsophalangeal joint in gout: A systematic review and meta-analysis. BMC Musculoskelet. Disord. 2016, 17, 69. [Google Scholar] [CrossRef]
- Pascart, T.; Grandjean, A.; Capon, B.; Legrand, J.; Namane, N.; Ducoulombier, V.; Motte, M.; Vandecandelaere, M.; Luraschi, H.; Godart, C.; et al. Monosodium urate burden assessed with dual-energy computed tomography predicts the risk of flares in gout: A 12-month observational study: MSU burden and risk of gout flare. Arthritis Res. Ther. 2018, 20, 210. [Google Scholar] [CrossRef]
- Wall, B.; Agudelo, C.A.; Tesser, J.R.; Mountz, J.; Holt, D.; Turner, R.A. An autopsy study of the prevalence of monosodium urate and calcium pyrophosphate dihydrate crystal deposition in first metatarsophalangeal joints. Arthritis Rheum. 1983, 26, 1522–1524. [Google Scholar] [CrossRef]
- Loeb, J.N. The influence of temperature on the solubility of monosodium urate. Arthritis Rheum. 1972, 15, 189–192. [Google Scholar] [CrossRef]
- Radice, F.; Monckeberg, J.E.; Carcuro, G. Longitudinal tears of peroneus longus and brevis tendons: A gouty infiltration. J. Foot Ankle Surg. 2011, 50, 751–753. [Google Scholar] [CrossRef]
- Mahoney, P.G.; James, P.D.; Howell, C.J.; Swannell, A.J. Spontaneous rupture of the Achilles tendon in a patient with gout. Ann. Rheum. Dis. 1981, 40, 416–418. [Google Scholar] [CrossRef]
- Dalbeth, N.; Kalluru, R.; Aati, O.; Horne, A.; Doyle, A.J.; McQueen, F.M. Tendon involvement in the feet of patients with gout: A dual-energy CT study. Ann. Rheum. Dis. 2013, 72, 1545–1548. [Google Scholar] [CrossRef]
- Yuan, Y.; Liu, C.; Xiang, X.; Yuan, T.L.; Qiu, L.; Liu, Y.; Luo, Y.B.; Zhao, Y. Ultrasound scans and dual energy CT identify tendons as preferred anatomical location of MSU crystal depositions in gouty joints. Rheumatol. Int. 2018, 38, 801–811. [Google Scholar] [CrossRef]
- Strobl, S.; Kremser, C.; Taljanovic, M.; Gruber, J.; Stofferin, H.; Bellmann-Weiler, R.; Klauser, A.S. Impact of Dual-Energy CT Postprocessing Protocol for the Detection of Gouty Arthritis and Quantification of Tophi in Patients Presenting With Podagra: Comparison With Ultrasound. Am. J. Roentgenol. 2019, 213, 1315–1323. [Google Scholar] [CrossRef]
- Anagnostakos, K.; Thiery, A.; Meyer, C.; Tapos, O. An Untypical Case of Gouty Infiltration of Both Peroneal Tendons and a Longitudinal Lesion of the Peroneus Brevis Tendon Mimicking Synovial Sarcoma. Case Rep. Orthop. 2018, 2018, 8790916. [Google Scholar] [CrossRef]
- Sakhaee, K. Epidemiology and clinical pathophysiology of uric acid kidney stones. J. Nephrol. 2014, 27, 241–245. [Google Scholar] [CrossRef]
- Nestler, T.; Nestler, K.; Neisius, A.; Isbarn, H.; Netsch, C.; Waldeck, S.; Schmelz, H.U.; Ruf, C. Diagnostic accuracy of third-generation dual-source dual-energy CT: A prospective trial and protocol for clinical implementation. World J. Urol. 2019, 37, 735–741. [Google Scholar] [CrossRef]
- Li, Z.X.; Jiao, G.L.; Zhou, S.M.; Cheng, Z.Y.; Bashir, S.; Zhou, Y. Evaluation of the chemical composition of nephrolithiasis using dual-energy CT in Southern Chinese gout patients. BMC Nephrol. 2019, 20, 273. [Google Scholar] [CrossRef]
- Sharon, Y.; Schlesinger, N. Beyond Joints: A Review of Ocular Abnormalities in Gout and Hyperuricemia. Curr. Rheumatol. Rep. 2016, 18, 37. [Google Scholar] [CrossRef]
- Lin, J.; Zhao, G.Q.; Che, C.Y.; Yang, S.S.; Wang, Q.; Li, C.G. Characteristics of ocular abnormalities in gout patients. Int. J. Ophthalmol. 2013, 6, 307–311. [Google Scholar]
- Yourish, N. Conjunctival tophi associated with gout. AMA Arch. Ophthalmol. 1953, 50, 370–371. [Google Scholar] [CrossRef] [PubMed]
- Ferry, A.P.; Safir, A.; Melikian, H.E. Ocular abnormalities in patients with gout. Ann. Ophthalmol. 1985, 17, 632–635. [Google Scholar] [PubMed]
- Carr, A.; Doyle, A.J.; Dalbeth, N.; Aati, O.; McQueen, F.M. Dual-Energy CT of Urate Deposits in Costal Cartilage and Intervertebral Disks of Patients With Tophaceous Gout and Age-Matched Controls. AJR Am. J. Roentgenol. 2016, 206, 1063–1067. [Google Scholar] [CrossRef] [PubMed]
- Chabra, I.; Singh, R. Gouty tophi on the ear: A review. Cutis 2013, 92, 190–192. [Google Scholar]
- Kumral, E.; Karaman, B.; Orman, M.; Kabaroglu, C. Association of uric acid and carotid artery disease in patients with ischemic stroke. Acta. Neurol. Scand. 2014, 130, 11–17. [Google Scholar] [CrossRef]
- Karagiannis, A.; Mikhailidis, D.P.; Tziomalos, K.; Sileli, M.; Savvatianos, S.; Kakafika, A.; Gossios, T.; Krikis, N.; Moschou, I.; Xochellis, M.; et al. Serum uric acid as an independent predictor of early death after acute stroke. Circ. J. 2007, 71, 1120–1127. [Google Scholar] [CrossRef][Green Version]
- McFarland, N.R.; Burdett, T.; Desjardins, C.A.; Frosch, M.P.; Schwarzschild, M.A. Postmortem brain levels of urate and precursors in Parkinson’s disease and related disorders. Neurodegener. Dis. 2013, 12, 189–198. [Google Scholar] [CrossRef]
- Disveld, I.J.M.; Fransen, J.; Rongen, G.A.; Kienhorst, L.B.E.; Zoakman, S.; Janssens, H.; Janssen, M. Crystal-proven Gout and Characteristic Gout Severity Factors Are Associated with Cardiovascular Disease. J. Rheumatol. 2018, 45, 858–863. [Google Scholar] [CrossRef]
- Andrés, M.; Quintanilla, M.A.; Sivera, F.; Sánchez-Payá, J.; Pascual, E.; Vela, P.; Ruiz-Nodar, J.M. Silent Monosodium Urate Crystal Deposits Are Associated With Severe Coronary Calcification in Asymptomatic Hyperuricemia: An Exploratory Study. Arthritis Rheumatol. 2016, 68, 1531–1539. [Google Scholar] [CrossRef]
- Pascart, T.; Capon, B.; Grandjean, A.; Legrand, J.; Namane, N.; Ducoulombier, V.; Motte, M.; Vandecandelaere, M.; Luraschi, H.; Godart, C.; et al. The lack of association between the burden of monosodium urate crystals assessed with dual-energy computed tomography or ultrasonography with cardiovascular risk in the commonly high-risk gout patient. Arthritis Res. Ther. 2018, 20, 97. [Google Scholar] [CrossRef]
- Iacobellis, G. A rare and asymptomatic case of mitral valve tophus associated with severe gouty tophaceous arthritis. J. Endocrinol. Investig. 2004, 27, 965–966. [Google Scholar] [CrossRef] [PubMed]
- Feuchtner, G.M.; Plank, F.; Beyer, C.; Schwabl, C.; Held, J.; Bellmann-Weiler, R.; Weiss, G.; Gruber, J.; Widmann, G.; Klauser, A.S. Monosodium Urate Crystal Deposition in Coronary Artery Plaque by 128-Slice Dual-Energy Computed Tomography: An Ex Vivo Phantom and In Vivo Study. J. Comput. Assist. Tomogr. 2021, 45, 856–862. [Google Scholar] [CrossRef] [PubMed]
- Neogi, T. Clinical practice. Gout. N. Engl. J. Med. 2011, 364, 443–452. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Zhang, X.; Sun, Y.; Chen, H.; Kong, X.; Zhou, J.; Ma, L.; Jiang, L. New urate depositions on dual-energy computed tomography in gouty arthritis during urate-lowering therapy. Rheumatol. Int. 2017, 37, 1365–1372. [Google Scholar] [CrossRef]
- Mushtaq, M.; Akram, M.U.; Alghamdi, N.S.; Fatima, J.; Masood, R.F. Localization and Edge-Based Segmentation of Lumbar Spine Vertebrae to Identify the Deformities Using Deep Learning Models. Sensors 2022, 22, 1547. [Google Scholar] [CrossRef]
- Sirshar, M.; Hassan, T.; Akram, M.U.; Khan, S.A. An incremental learning approach to automatically recognize pulmonary diseases from the multi-vendor chest radiographs. Comput. Biol. Med. 2021, 134, 104435. [Google Scholar] [CrossRef]
- Akbar, S.; Sharif, M.; Akram, M.U.; Saba, T.; Mahmood, T.; Kolivand, M. Automated techniques for blood vessels segmentation through fundus retinal images: A review. Microsc. Res. Tech. 2019, 82, 153–170. [Google Scholar] [CrossRef]

| Anatomical Location | Score 0 | Score 1 | Score 2 | Score 3 |
|---|---|---|---|---|
| Aorta | ||||
| root | 6/41 (14.6%) 31/41 (75.6%) | 0/41 (0%) 10/41 (24%) | 11/41 (26.9%) 0/41 (0%) | 24/41 (58.5%) 0/41 (0%) |
| ascending | 13/41 (31.7%) 34/41 (82.9%) | 0/41 (0%) 7/41 (17.1%) | 7/41 (17.1%) 0/41 (0%) | 21/41 (51.2%) 0/41 (0%) |
| arch | 1/41 (2.4%) 31/41 (75.6%) | 0/41 (0%) 10/41 (24%) | 3/41 (7.3%) 0/41 (0%) | 37/41 (90.2%) 0/41 (0%) |
| descending | 2/41 (4.9%) 13/41 (31.7%) | 0/41 (0%) 22/41 (53.7%) | 3/41 (7.3%) 2/41 (4.9%) | 36/41 (87.9%) 4/41 (9.8%) |
| abdominal | 0/41 (0%) 40/41 (97.6%) | 2/41 (4.9%) 1/41 (2.4%) | 0/41 (0%) 0/41 (0%) | 39/41 (95.1%) 0/41 (0%) |
| Supraaortal vessels | 2/41 (4.9%) 28/41 (68.3%) | 0/41 (0%) 12/41 (29.3%) | 6/41 (14.6%) 1/41 (2.4%) | 33/41 (80.5%) 0/41 (0%) |
| Iliac vessels | 0/41 (0%) 36/41 (87.8%) | 2/41 (4.9%) 5/41 (12.2%) | 0/41 (0%) 0/41 (0%) | 39/41 (95.1) 0/41 (0%) |
| Valves | ||||
| tricuspid | 41/41 (100%) 41/41 (100%) | 0/41 (0%) 0/41 (0%) | 0/41 (0%) 0/41 (0%) | 0/41 (0%) 0/41 (0%) |
| mitral | 41/41 (100%) 41/41 (100%) | 0/41 (0%) 0/41 (0%) | 0/41 (0%) 0/41 (0%) | 0/41 (0%) 0/41 (0%) |
| Coronary arteries | ||||
| LAD | 2/41 (4.9%) 41/41 (100%) | 0/41 (0% 0/41 (0%) | 3/41 (7.3%) 0/41 (0%) | 36/41 (87.9%) 0/41 (0%) |
| LM | 11/41 (26.8%) 41/41 (100%) | 0/41 (0% 0/41 (0%) | 3/41 (7.3%) 0/41 (0%) | 27/41 (65.9%) 0/41 (0%) |
| RCA | 8/41 (19.5%) 41/41 (100%) | 0/41 (0% 0/41 (0%) | 5/41 (12.2%) 0/41 (0%) | 28/41 (68.3%) 0/41 (0%) |
| CX | 8/41 (19.5%) 41/41 (100%) | 0/41 (0% 0/41 (0%) | 4/41 (9.8%) 0/41 (0%) | 29/41 (70.7%) 0/41 (0%) |
| Anatomical Location | Positive Joints | Score 0 | Score 1 | Score 2 | Score 3 |
|---|---|---|---|---|---|
| MTP joints | 11/41 (26.8%) | 30/41 (73.2%) | 2/41 (4.9%) | 6/41 (14.6%) | 3/41 (7.3%) |
| MTP I | 6/11 (54.5%) | 1/6 (16.7%) | 3/6 (50%) | 2/6 (33.3%) | |
| MTP I − V | 4/11 (36.4%) | 0/4 (0%) | 3/4 (75%) | 1/4 (25%) | |
| MTP I + V | 1/11 (10%) | 1/1 (100%) | 0/1 (0%) | 0/1 (0%) | |
| Interphalangeal joint | 0/41 (0%) | ||||
| Ankle | 0/41 (0%) | ||||
| Tarsus | 0/41 (0%) |
| Anatomical Location | Score 0 | Score 1 | Score 2 | Score 3 |
|---|---|---|---|---|
| EHL | 1/41 (2.4%) | 24/41 (58.5%) | 11/41 (27.5%) | 5/41 (12.2) |
| FHL | 1/41 (2.4%) | 31/41 (75.6%) | 8/41 (19.5%) | 1/41 (2.4%) |
| TAT | 1/41 (2.4%) | 13/41 (31.7%) | 19/41 (46.3%) | 8/41 (19.5%) |
| TPT | 1/41 (2.4%) | 31/41 (75.6) | 8/41 (19.5%) | 1/41 (2.4%) |
| PT | 1/41 (2.4%) | 19/41 (46.3%) | 18/41 (43.9%) | 3/41 (7.3%) |
| AT | 1/41 (2.4%) | 22/41 (53.6%) | 5/41 (12.2.%) | 13/41 (31.7%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Klauser, A.S.; Strobl, S.; Schwabl, C.; Klotz, W.; Feuchtner, G.; Moriggl, B.; Held, J.; Taljanovic, M.; Weaver, J.S.; Reijnierse, M.; et al. Prevalence of Monosodium Urate (MSU) Deposits in Cadavers Detected by Dual-Energy Computed Tomography (DECT). Diagnostics 2022, 12, 1240. https://doi.org/10.3390/diagnostics12051240
Klauser AS, Strobl S, Schwabl C, Klotz W, Feuchtner G, Moriggl B, Held J, Taljanovic M, Weaver JS, Reijnierse M, et al. Prevalence of Monosodium Urate (MSU) Deposits in Cadavers Detected by Dual-Energy Computed Tomography (DECT). Diagnostics. 2022; 12(5):1240. https://doi.org/10.3390/diagnostics12051240
Chicago/Turabian StyleKlauser, Andrea S., Sylvia Strobl, Christoph Schwabl, Werner Klotz, Gudrun Feuchtner, Bernhard Moriggl, Julia Held, Mihra Taljanovic, Jennifer S. Weaver, Monique Reijnierse, and et al. 2022. "Prevalence of Monosodium Urate (MSU) Deposits in Cadavers Detected by Dual-Energy Computed Tomography (DECT)" Diagnostics 12, no. 5: 1240. https://doi.org/10.3390/diagnostics12051240
APA StyleKlauser, A. S., Strobl, S., Schwabl, C., Klotz, W., Feuchtner, G., Moriggl, B., Held, J., Taljanovic, M., Weaver, J. S., Reijnierse, M., Gizewski, E. R., & Stofferin, H. (2022). Prevalence of Monosodium Urate (MSU) Deposits in Cadavers Detected by Dual-Energy Computed Tomography (DECT). Diagnostics, 12(5), 1240. https://doi.org/10.3390/diagnostics12051240







