The Comparison of Lower Extremity Length and Angle between Computed Radiography-Based Teleoroentgenogram and EOS® Imaging System
Abstract
:1. Introduction
2. Materials and Methods
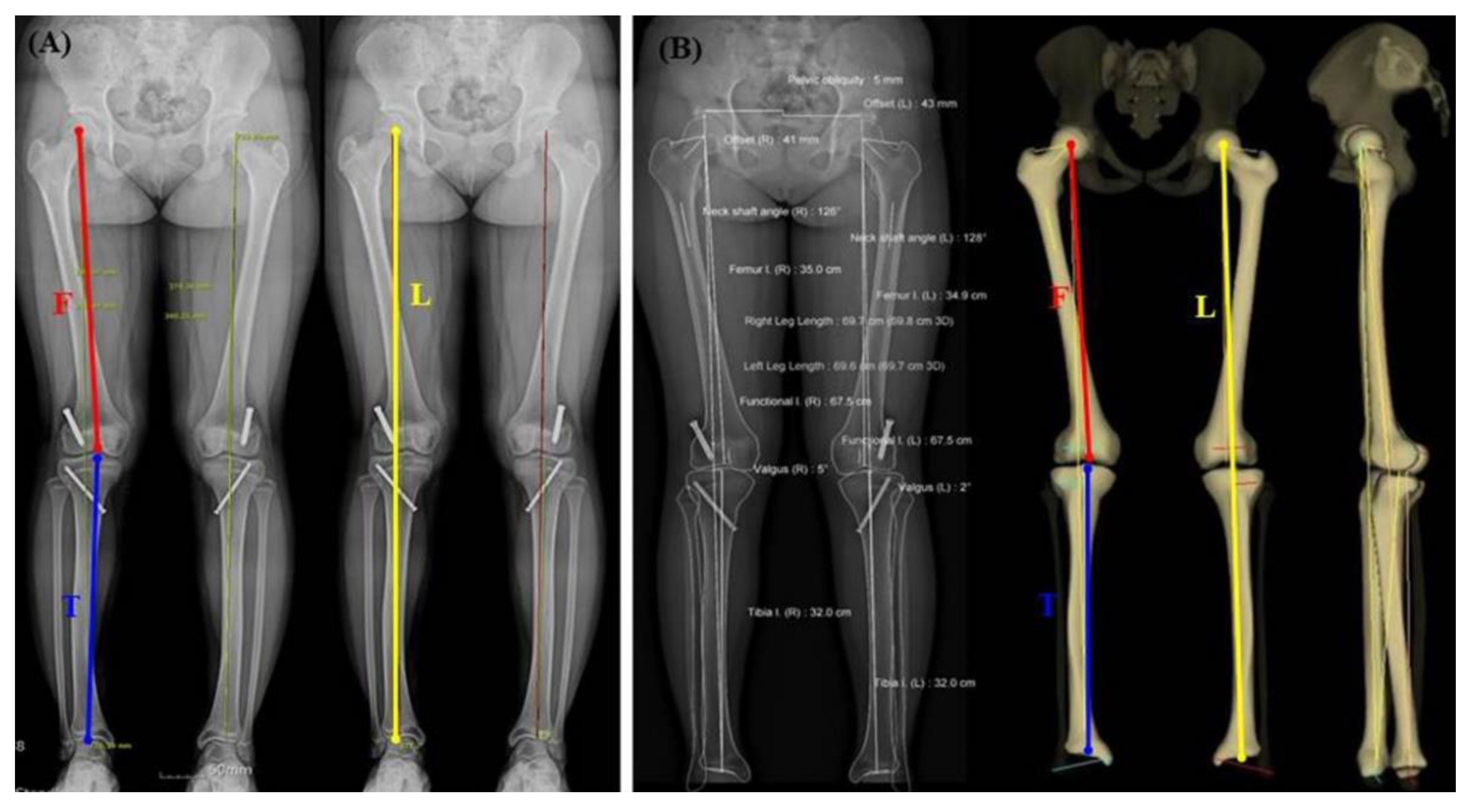
2.1. CR-Based Teleoroentgenogram
2.2. EOS®
2.3. Radiographic Measurement
2.4. Statistical Analysis
3. Results
3.1. Right-Side Comparison
3.2. Left-Side Comparison
3.3. Comparison for Both Sides
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Azizan, N.A.; Basaruddin, K.S.; Salleh, A.F. The effects of leg length discrepancy on stability and kinematics-kinetics deviations: A systematic review. J. Appl. Bionics Biomech. 2018, 2018, 5156348. [Google Scholar] [CrossRef] [PubMed]
- Sheha, E.D.; Steinhaus, M.E.; Kim, H.J.; Cunningham, M.E.; Fragomen, A.T.; Rozbruch, S.R. Leg-Length Discrepancy, Functional Scoliosis, and Low Back Pain. JBJS Rev. 2018, 6, e6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paley, D. Principles of Deformity Correction; Springer: Berlin/Heidelberg, Germany, 2014. [Google Scholar]
- Machen, M.S.; Stevens, P.M. Should full-length standing anteroposterior radiographs replace the scanogram for measurement of limb length discrepancy? J. Pediatr. Orthop. B 2005, 14, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Moseley, C.F. Leg length discrepancy. Orthop. Clin. N. Am 1987, 18, 529–535. [Google Scholar] [CrossRef]
- Applebaum, A.; Nessim, A.; Cho, W. Overview and Spinal Implications of Leg Length Discrepancy: Narrative Review. Clin. Orthop. Surg. 2021, 13, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Sabharwal, S.; Kumar, A. Methods for assessing leg length discrepancy. Clin. Orthop. Relat. Res. 2008, 466, 2910–2922. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Terjesen, T.; Benum, P.; Rossvoll, I.; Svenningsen, S.; Fløystad Isern, A.E.; Nordbø, T. Leg-length discrepancy measured by ultrasonography. Acta Orthop. Scand. 1991, 62, 121–124. [Google Scholar] [CrossRef]
- Aaron, A.; Weinstein, D.; Thickman, D.; Eilert, R. Comparison of orthoroentgenography and computed tomography in the measurement of limb-length discrepancy. J. Bone Jt. Surg. Am. 1992, 74, 897–902. [Google Scholar] [CrossRef]
- Sabharwal, S.; Zhao, C.; McKeon, J.J.; McClemens, E.; Edgar, M.; Behrens, F. Computed radiographic measurement of limb-length discrepancy. Full-length standing anteroposterior radiograph compared with scanogram. J. Bone Jt. Surg. Am. 2006, 88, 2243–2251. [Google Scholar] [CrossRef] [Green Version]
- Stanitski, D.F. Limb-length inequality: Assessment and treatment options. J. Am. Acad. Orthop. Surg. 1999, 7, 143–153. [Google Scholar] [CrossRef]
- Kalifa, G.; Charpak, Y.; Maccia, C.; Fery-Lemonnier, E.; Bloch, J.; Boussard, J.M.; Attal, M.; Dubousset, J.; Adamsbaum, C. Evaluation of a new low-dose digital x-ray device: First dosimetric and clinical results in children. Pediatr. Radiol. 1998, 28, 557–561. [Google Scholar] [CrossRef] [PubMed]
- Escott, B.G.; Ravi, B.; Weathermon, A.C.; Acharya, J.; Gordon, C.L.; Babyn, P.S.; Kelley, S.P.; Narayanan, U.G. EOS low-dose radiography: A reliable and accurate upright assessment of lower-limb lengths. J. Bone Jt. Surg. Am. 2013, 95, e1831–e1837. [Google Scholar] [CrossRef] [PubMed]
- Huurman, W.W.; Jacobsen, F.S.; Anderson, J.C.; Chu, W.K. Limb-length discrepancy measured with computerized axial tomographic equipment. J. Bone Jt. Surg. Am. 1987, 69, 699–705. [Google Scholar] [CrossRef]
- Ko, D.O.; Lee, S.; Kim, J.H.; Hwang, I.C.; Jang, S.J.; Jung, J. The Influence of Femoral Internal Rotation on Patellar Tracking in Total Knee Arthroplasty Using Gap Technique. Clin. Orthop. Surg. 2021, 13, 352–357. [Google Scholar] [CrossRef] [PubMed]
- Leitzes, A.H.; Potter, H.G.; Amaral, T.; Marx, R.G.; Lyman, S.; Widmann, R.F. Reliability and accuracy of MRI scanogram in the evaluation of limb length discrepancy. J. Pediatr. Orthop. 2005, 25, 747–749. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]
- Altongy, J.F.; Harcke, H.T.; Bowen, J.R. Measurement of leg length inequalities by Micro-Dose digital radiographs. J. Pediatr. Orthop. 1987, 7, 311–316. [Google Scholar] [CrossRef]
- Deschênes, S.; Charron, G.; Beaudoin, G.; Labelle, H.; Dubois, J.; Miron, M.C.; Parent, S. Diagnostic imaging of spinal deformities: Reducing patients radiation dose with a new slot-scanning X-ray imager. Spine 2010, 35, 989–994. [Google Scholar] [CrossRef]
- Dubousset, J.; Charpak, G.; Skalli, W.; de Guise, J.; Kalifa, G.; Wicart, P. Skeletal and spinal imaging with EOS system. Arch. Pediatrie Organe Off. Soc. Fr. Pediatrie 2008, 15, 665–666. [Google Scholar] [CrossRef]
- Thelen, P.; Delin, C.; Folinais, D.; Radier, C. Evaluation of a new low-dose biplanar system to assess lower-limb alignment in 3D: A phantom study. Skelet. Radiol. 2012, 41, 1287–1293. [Google Scholar] [CrossRef]
- Dubousset, J.; Charpak, G.; Dorion, I.; Skalli, W.; Lavaste, F.; Deguise, J.; Kalifa, G.; Ferey, S. A new 2D and 3D imaging approach to musculoskeletal physiology and pathology with low-dose radiation and the standing position: The EOS system. Bull. Acad. Natl. Med. 2005, 189, 287–297, discussion 297–300. [Google Scholar] [PubMed]
- Dubousset, J.; Charpak, G.; Skalli, W.; Kalifa, G.; Lazennec, J.Y. EOS stereo-radiography system: Whole-body simultaneous anteroposterior and lateral radiographs with very low radiation dose. Rev. Chir. Orthop. Reparatrice Appar. Mot. 2007, 93, 141–143. [Google Scholar] [CrossRef]
- Delin, C.; Silvera, S.; Radier, C.; Bassinet, C.; Rehel, J.-L.; Djian, P.; Legmann, P.; Folinais, D. Dosimétrie des mesures de torsion et d’antéversion des membres inférieurs utilisant l’EOS et le scanner. Rev. Chir. Orthop. 2011, 97, S298. [Google Scholar] [CrossRef]
| Variable | N (%) |
|---|---|
| Gender | |
| Female | 56 (55.45) |
| Male | 45 (44.55) |
| Age (years old) | 39.39 ± 28.75: range (1–83) |
| Disease | |
| Limb length discrepancy | 40 (39.60) |
| Angular deformity | 57 (56.44) |
| Traumatic osteoarthritis | 2 (1.98) |
| Baseline evaluation | 2 (1.98) |
| Total | 101 (100) |
| Parameters | EOS® | CR Based Teleoroentgenogram | Magnification (mm) | Magnification Percentage (%) | p Value |
|---|---|---|---|---|---|
| Leg length [L] | 669.84 ± 114.25 | 723.54 ± 123.52 | 53.7 ± 13.77 | 8.01 ± 1.62 | <0.001 * |
| Femur + Tibia [F + T] | 669.80 ± 116.46 | 715.99± 127.11 | 46.2 ± 28.70 | 6.85 ± 4.22 | <0.001 * |
| Femur [F] | 360.62 ± 62.80 | 391.06 ± 68.24 | 30.45 ± 7.36 | 8.44 ± 1.37 | <0.001 * |
| Tibia [T] | 309.18 ± 56.03 | 324.93 ± 60.40 | 15.75 ± 2.63 | 5.12 ± 0.83 | <0.001 * |
| Hip-Knee-Ankle Angle | 1.07 ± 5.10 | 1.40 ± 4.62 | 0.181 |
| Parameters | EOS® | CR Based Teleoroentgenogram | Magnification (mm) | Magnification Percentage (%) | p Value |
|---|---|---|---|---|---|
| Leg length [L] | 671.79 ± 114.19 | 722.92 ± 123.18 | 51.13 ± 11.60 | 7.61 ± 1.13 | <0.001 * |
| Femur + Tibia [F + T] | 667.61 ± 114.67 | 707.58 ± 126.68 | 44.34 ± 4.43 | 6.05 ± 5.67 | <0.001 * |
| Femur [F] | 360.21 ± 62.68 | 384.20 ± 76.75 | 23.99 ± 4.37 | 6.81 ± 1.14 | <0.001 * |
| Tibia [T] | 307.40 ± 52.47 | 323.39 ± 55.51 | 15.99 ± 6.30 | 5.20 ± 1.79 | <0.001 * |
| Hip-Knee-Ankle Angle | 1.25 ± 5.29 | 1.60 ± 4.96 | 0.66 |
| Parameters | EOS® | CR Based Teleoroentgenogram | Magnification (mm) | Magnification Percentage (%) | p Value |
|---|---|---|---|---|---|
| Leg length [L] | 670.82 ± 113.94 | 723.23 ± 123.05 | 52.42 ± 12.76 | 7.80 ± 1.41 | <0.001 * |
| Femur + Tibia [F + T] | 668.7 ± 115.29 | 711.79 ± 126.65 | 43.09 ± 3.74 | 6.45 ± 5.01 | <0.001 * |
| Femur [F] | 360.41 ± 62.58 | 387.63 ± 72.52 | 27.21 ± 3.14 | 7.63 ± 1.25 | <0.001 * |
| Tibia [T] | 308.29 ± 54.15 | 324.16 ± 57.87 | 15.87 ± 1.91 | 5.16 ± 0.94 | <0.001 * |
| Hip-Knee-Ankle Angle | 1.16 ± 5.19 | 1.51 ± 4.78 | 0.177 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, K.-R.; Lee, J.-H.; Kim, D.-S.; Ryu, H.; Kim, J.; Yon, C.-J.; Lee, S.-W. The Comparison of Lower Extremity Length and Angle between Computed Radiography-Based Teleoroentgenogram and EOS® Imaging System. Diagnostics 2022, 12, 1052. https://doi.org/10.3390/diagnostics12051052
Park K-R, Lee J-H, Kim D-S, Ryu H, Kim J, Yon C-J, Lee S-W. The Comparison of Lower Extremity Length and Angle between Computed Radiography-Based Teleoroentgenogram and EOS® Imaging System. Diagnostics. 2022; 12(5):1052. https://doi.org/10.3390/diagnostics12051052
Chicago/Turabian StylePark, Kwang-Rak, Jae-Ho Lee, Dae-Soo Kim, Ho Ryu, Jaeho Kim, Chang-Jin Yon, and Si-Wook Lee. 2022. "The Comparison of Lower Extremity Length and Angle between Computed Radiography-Based Teleoroentgenogram and EOS® Imaging System" Diagnostics 12, no. 5: 1052. https://doi.org/10.3390/diagnostics12051052
APA StylePark, K.-R., Lee, J.-H., Kim, D.-S., Ryu, H., Kim, J., Yon, C.-J., & Lee, S.-W. (2022). The Comparison of Lower Extremity Length and Angle between Computed Radiography-Based Teleoroentgenogram and EOS® Imaging System. Diagnostics, 12(5), 1052. https://doi.org/10.3390/diagnostics12051052







