Dental and Maxillofacial Cone Beam CT—High Number of Incidental Findings and Their Impact on Follow-Up and Therapy Management
Abstract
:1. Introduction
2. Materials and Methods
2.1. Technical Examination Parameters and Standard Operating Procedure
2.2. Evaluation of the Results
2.3. Subgroup Analysis
2.4. Statistical Methods
3. Results
3.1. Referring Physicians and Primary Indications
3.2. Pathological Findings
3.3. Dental Findings
3.4. Paranasal Sinuses and Airways Findings
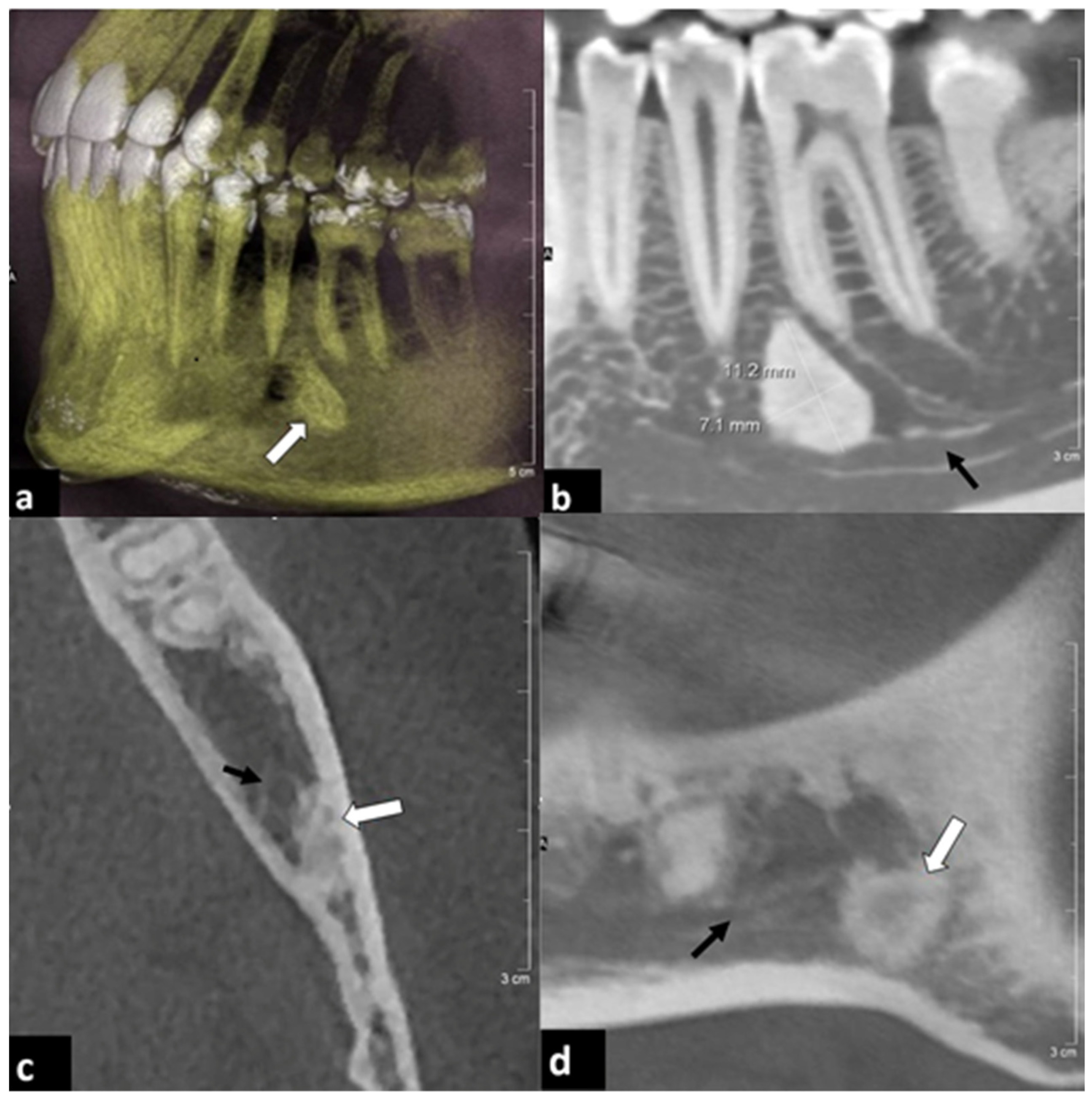
3.5. Osseous Findings
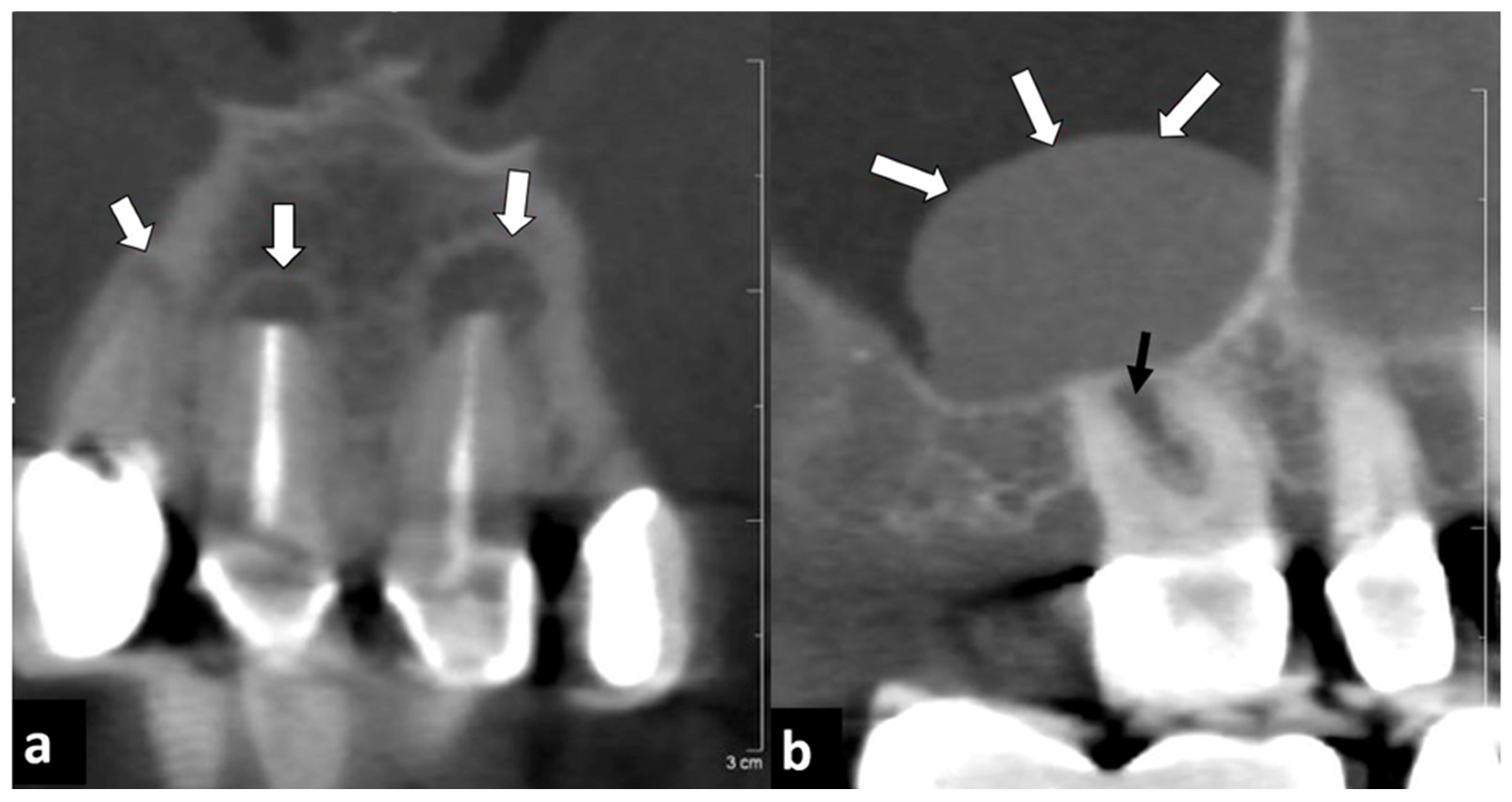
3.6. Soft Tissue Findings
3.7. TMJ Findings
3.8. Clinical Subgroup Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mozzo, P.; Procacci, C.; Tacconi, A.; Martini, P.T.; Andreis, I.A. A new volumetric CT machine for dental imaging based on the cone-beam technique: Preliminary results. Eur. Radiol. 1998, 8, 1558–1564. [Google Scholar] [CrossRef]
- Miracle, A.C.; Mukherji, S.K. Conebeam CT of the head and neck, part 2: Clinical applications. Am. J. Neuroradiol. 2009, 30, 1285–1292. [Google Scholar] [CrossRef] [Green Version]
- Guerrero, M.E.; Noriega, J.; Jacobs, R. Preoperative implant planning considering alveolar bone grafting needs and complication prediction using panoramic versus CBCT images. Imaging Sci. Dent. 2014, 44, 213–220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mubeen, S.; Patel, K.; Cunningham, Z.; O’Rourke, N.; Pandis, N.; Cobourne, M.T.; Seehra, J. Assessing the quality of dental clinical practice guidelines. J. Dent. 2017, 67, 102–106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jeger, F.B.; Lussi, A.; Bornstein, M.M.; Jacobs, R.; Janner, S.F.M. Cone beam computed tomography in endodontics: A review for daily clinical practice. SSO 2013, 123, 661–668. [Google Scholar]
- Kasaj, A.; Willershausen, B. Digital volume tomography for diagnostics in periodontology. Int. J. Comput. Dent. 2007, 10, 155–168. [Google Scholar] [PubMed]
- Brown, J.; Jacobs, R.; Levring Jäghagen, E.; Lindh, C.; Baksi, G.; Schulze, D.; Schulze, R.; European Academy of DentoMaxilloFacial Radiology. Basic training requirements for the use of dental CBCT by dentists: A position paper prepared by the European Academy of DentoMaxilloFacial Radiology. Dentomaxillofac Radiol. 2014, 43, 20130291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dief, S.; Veitz-Keenan, A.; Amintavakoli, N.; McGowan, R. A systematic review on incidental findings in cone beam computed tomography (CBCT) scans. Dento Maxillo Facial Radiol. 2019, 48, 20180396. [Google Scholar] [CrossRef]
- Allareddy, V.; Vincent, S.D.; Hellstein, J.W.; Qian, F.; Smoker, W.R.K.; Ruprecht, A. Incidental findings on cone beam computed tomography images. Int. J. Dent. 2012, 2012, 871532. [Google Scholar] [CrossRef] [Green Version]
- Caglayan, F.; Tozoglu, U. Incidental findings in the maxillofacial region detected by cone beam CT. Diagn. Interv. Radiol. 2012, 18, 159–163. [Google Scholar]
- Cha, J.Y.; Mah, J.; Sinclair, P. Incidental findings in the maxillofacial area with 3-dimensional cone-beam imaging. Am. J. Orthod. Dentofacial. Orthop. 2007, 132, 7–14. [Google Scholar] [CrossRef]
- Price, J.B.; Thaw, K.L.; Tyndall, D.A.; Ludlow, J.B.; Padilla, R.J. Incidental findings from cone beam computed tomography of the maxillofacial region: A descriptive retrospective study. Clin. Oral. Implant. Res. 2012, 23, 1261–1268. [Google Scholar] [CrossRef]
- Drage, N.; Rogers, S.; Greenall, C.; Playle, R. Incidental findings on cone beam computed tomography in orthodontic patients. J. Orthod. 2013, 40, 29–37. [Google Scholar] [CrossRef]
- Pette, G.A.; Norkin, F.J.; Ganeles, J.; Hardigan, P.; Lask, E.; Zfaz, S.; Parker, W. Incidental findings from a retrospective study of 318 cone beam computed tomography consultation reports. Int. J. Oral Maxillofac. Implant. 2012, 27, 595–603. [Google Scholar]
- Pliska, B.; DeRocher, M.; Larson, B.E. Incidence of significant findings on CBCT scans of an orthodontic patient population. Northwest Dent. 2011, 90, 12–16. [Google Scholar]
- Lopes, I.A.; Tucunduva, R.M.; Handem, R.H.; Capelozza, A.L. Study of the frequency and location of incidental findings of the maxillofacial region in different fields of view in CBCT scans. Dento Maxillo Facial Radiol. 2017, 46, 20160215. [Google Scholar] [CrossRef] [Green Version]
- Nguyen, P.N.; Kruger, E.; Huang, T.; Koong, B. Incidental findings detected on cone beam computed tomography in an older population for pre-implant assessment. Aust. Dent. J. 2020, 65, 252–258. [Google Scholar] [CrossRef]
- European Commission. Radiation Protection No 172: Cone Beam CT for Dental and Maxillofacial Radiology. Evidence Based Guidelines. European Commission, Directorate General for Energy Radiation Protection Unit. 2012. Available online: https://ec.europa.eu/energy/sites/ener/files/documents/172.pdf (accessed on 3 April 2022).
- International Statistical Classification of Diseases, German Modification. Available online: https://www.bfarm.de/EN/Code-systems/Classifications/ICD/ICD-10-GM/_node.html (accessed on 3 April 2022).
- Kachlan, M.O.; Yang, J.; Balshi, T.J.; Wolfinger, G.J.; Balshi, S.F. Incidental Findings in Cone Beam Computed Tomography for Dental Implants in 1002 Patients. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2021, 30, 665–675. [Google Scholar] [CrossRef]
- Kurtuldu, E.; Alkis, H.T.; Yesiltepe, S.; Sumbullu, M.A. Incidental findings in patients who underwent cone beam computed tomography for implant treatment planning. Niger. J. Clin. Pract. 2020, 23, 329–336. [Google Scholar] [CrossRef]
- Mutalik, S.; Rengasamy, K.; Tadinada, A. Incidental findings based on anatomical location and clinical significance in CBCT scans of dental implant patients. Quintessence Int. 2018, 49, 419–426. [Google Scholar] [CrossRef]
- Tyndall, D.A.; Price, J.B.; Tetradis, S.; Ganz, S.D.; Hildebolt, C.; Scarfe, W.C. Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2012, 113, 817–826. [Google Scholar] [CrossRef]
- Horner, K.; O’Malley, L.; Taylor, K.; Glenny, A.-M. Guidelines for clinical use of CBCT: A review. Dentomaxillofac Radiol. 2015, 44, 20140225. [Google Scholar] [CrossRef] [Green Version]
- Edwards, R.; Alsufyani, N.; Heo, G.; Flores-Mir, C. The frequency and nature of incidental findings in large-field cone beam computed tomography scans of an orthodontic sample. Prog. Orthod. 2014, 15, 37. [Google Scholar] [CrossRef] [Green Version]
- Johnson, S.; Fluckiger, J.; Parashar, V.; Beals, D.; Agostini, G. Frequency and types of incidental findings on limited field of view CBCT scans. Gen. Dent. 2021, 69, 42–45. [Google Scholar]
- Oser, D.G.; Henson, B.R.; Shiang, E.Y.; Finkelman, M.D.; Amato, R.B. Incidental Findings in Small Field of View Cone-beam Computed Tomography Scans. J. Endod. 2017, 43, 901–904. [Google Scholar] [CrossRef] [PubMed]
- Rege, I.C.C.; Sousa, T.O.; Leles, C.R.; Mendonça, E.F. Occurrence of maxillary sinus abnormalities detected by cone beam CT in asymptomatic patients. BMC Oral. Health 2012, 12, 30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khalifa, H.M.; Felemban, O.M. Nature and clinical significance of incidental findings in maxillofacial cone-beam computed tomography: A systematic review. Oral. Radiol. 2021, 37, 547–559. [Google Scholar] [CrossRef]
- Warhekar, S.; Nagarajappa, S.; Dasar, P.L.; Warhekar, A.M.; Parihar, A.; Phulambrikar, T.; Airen, B.; Jain, D. Incidental findings on cone beam computed tomography and reasons for referral by dental practitioners in indore city (m.p). J. Clin. Diagn. Res. JCDR 2015, 9, ZC21–ZC24. [Google Scholar] [CrossRef] [PubMed]
- Psillas, G.; Papaioannou, D.; Petsali, S.; Dimas, G.G.; Constantinidis, J. Odontogenic maxillary sinusitis: A comprehensive review. J. Dent. Sci. 2021, 16, 474–481. [Google Scholar] [CrossRef] [PubMed]
- Lechien, J.R.; Filleul, O.; Costa de Araujo, P.; Hsieh, J.W.; Chantrain, G.; Saussez, S. Chronic maxillary rhinosinusitis of dental origin: A systematic review of 674 patient cases. Int. J. Otolaryngol. 2014, 2014, 465173. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| (a) | |
| FOV in mm2 | Number of Examinations |
| 100 × 100 | 275 |
| 80 × 80 | 44 |
| 140 × 140 | 18 |
| 60 × 60 | 14 |
| 170 × 170 | 13 |
| 40 × 40 | 5 |
| Other | 5 |
| (b) | |
| Voxel Size in μm. | Number of Examinations |
| 250 | 308 |
| 160 | 44 |
| 125 | 16 |
| 80 | 5 |
| 260 | 1 |
| Exposition, DLP (mGy × cm) | Number of Examinations |
|---|---|
| 52 | 1 |
| 70 | 13 |
| 72 | 1 |
| 87 | 97 |
| 105 | 41 |
| 122 | 127 |
| 140 | 63 |
| 154 | 3 |
| 157 | 9 |
| 175 | 15 |
| 215 | 1 |
| 246 | 3 |
| (a) | |
| Referring Physicians | Number of Referred Patients |
| General dentist | 252 |
| Orthodontic dentist | 50 |
| Otolaryngologists | 28 |
| Others | 44 |
| (b) | |
| Primary Indication | Number of Examinations |
| implantology | 191 |
| orthodonctics | 56 |
| ENT | 36 |
| endodontics | 21 |
| teeth removal | 18 |
| oncology | 13 |
| trauma | 8 |
| TMJ | 3 |
| parodontics | 1 |
| other | 27 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Braun, M.J.; Rauneker, T.; Dreyhaupt, J.; Hoffmann, T.K.; Luthardt, R.G.; Schmitz, B.; Dammann, F.; Beer, M. Dental and Maxillofacial Cone Beam CT—High Number of Incidental Findings and Their Impact on Follow-Up and Therapy Management. Diagnostics 2022, 12, 1036. https://doi.org/10.3390/diagnostics12051036
Braun MJ, Rauneker T, Dreyhaupt J, Hoffmann TK, Luthardt RG, Schmitz B, Dammann F, Beer M. Dental and Maxillofacial Cone Beam CT—High Number of Incidental Findings and Their Impact on Follow-Up and Therapy Management. Diagnostics. 2022; 12(5):1036. https://doi.org/10.3390/diagnostics12051036
Chicago/Turabian StyleBraun, Michael J., Thaddaeus Rauneker, Jens Dreyhaupt, Thomas K. Hoffmann, Ralph G. Luthardt, Bernd Schmitz, Florian Dammann, and Meinrad Beer. 2022. "Dental and Maxillofacial Cone Beam CT—High Number of Incidental Findings and Their Impact on Follow-Up and Therapy Management" Diagnostics 12, no. 5: 1036. https://doi.org/10.3390/diagnostics12051036
APA StyleBraun, M. J., Rauneker, T., Dreyhaupt, J., Hoffmann, T. K., Luthardt, R. G., Schmitz, B., Dammann, F., & Beer, M. (2022). Dental and Maxillofacial Cone Beam CT—High Number of Incidental Findings and Their Impact on Follow-Up and Therapy Management. Diagnostics, 12(5), 1036. https://doi.org/10.3390/diagnostics12051036









