Long-Term Outcome of Differentiated Thyroid Cancer Patients—Fifty Years of Croatian Thyroid Disease Referral Centre Experience
Abstract
1. Introduction
2. Materials and Methods
Statistical Methods
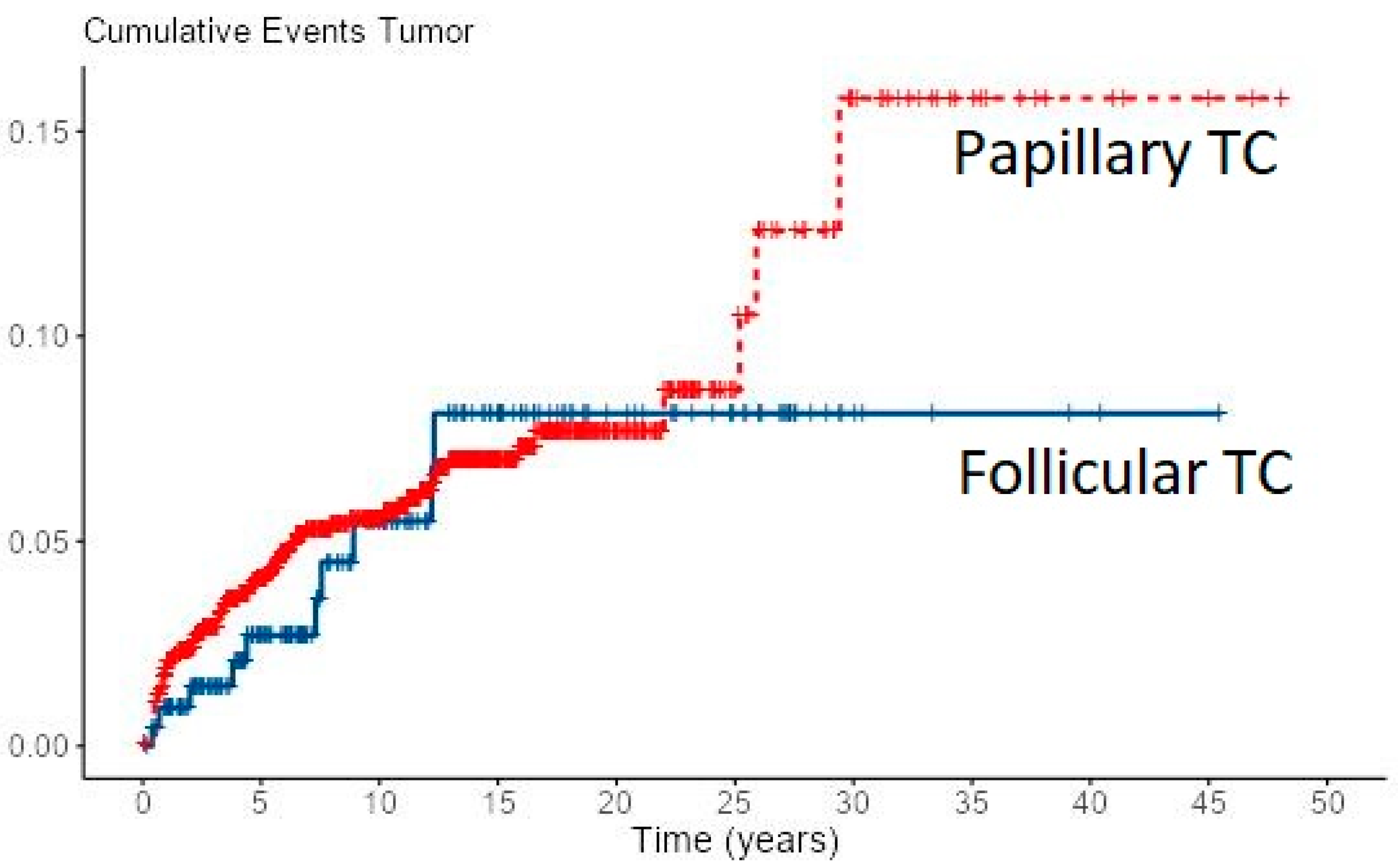
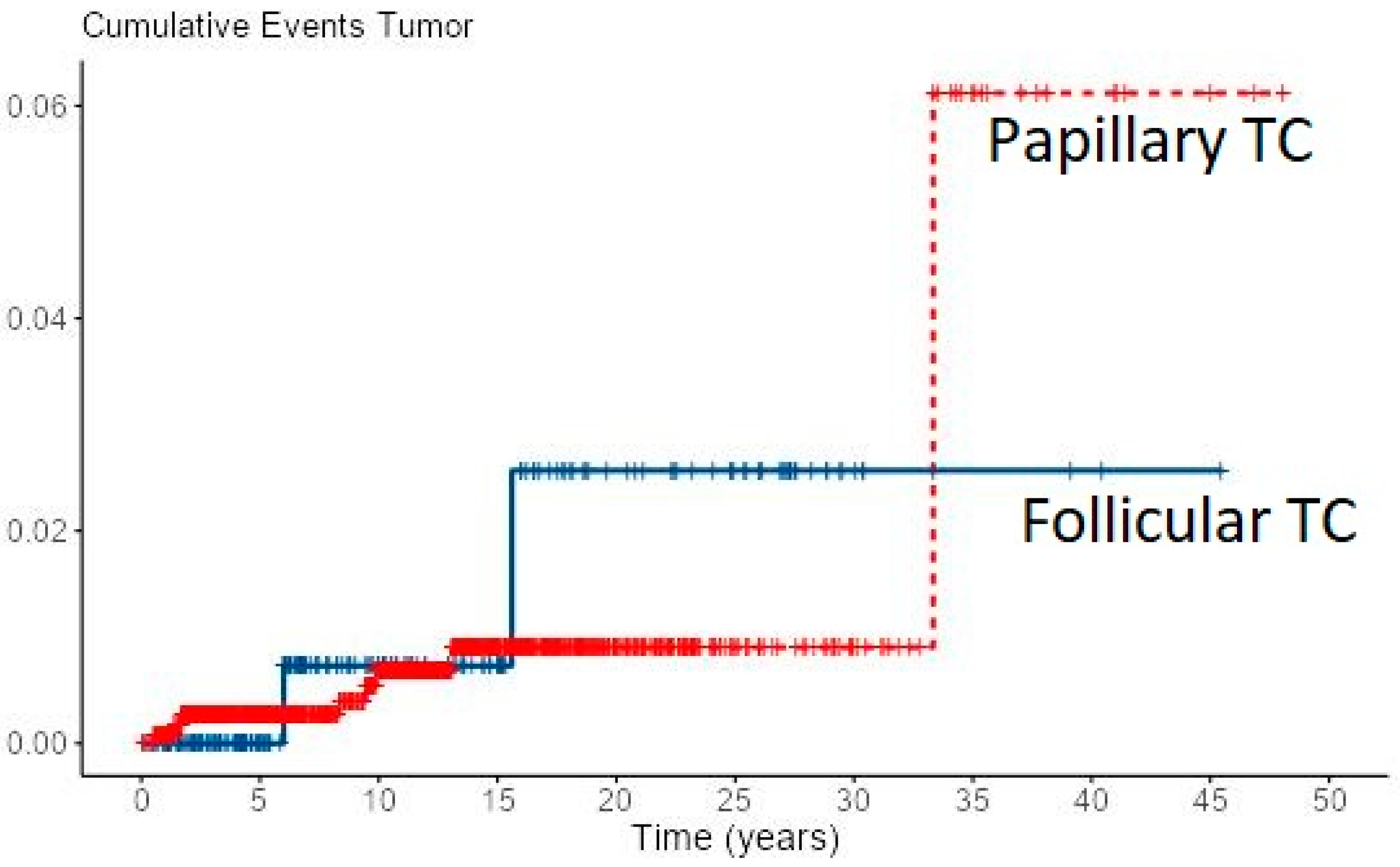
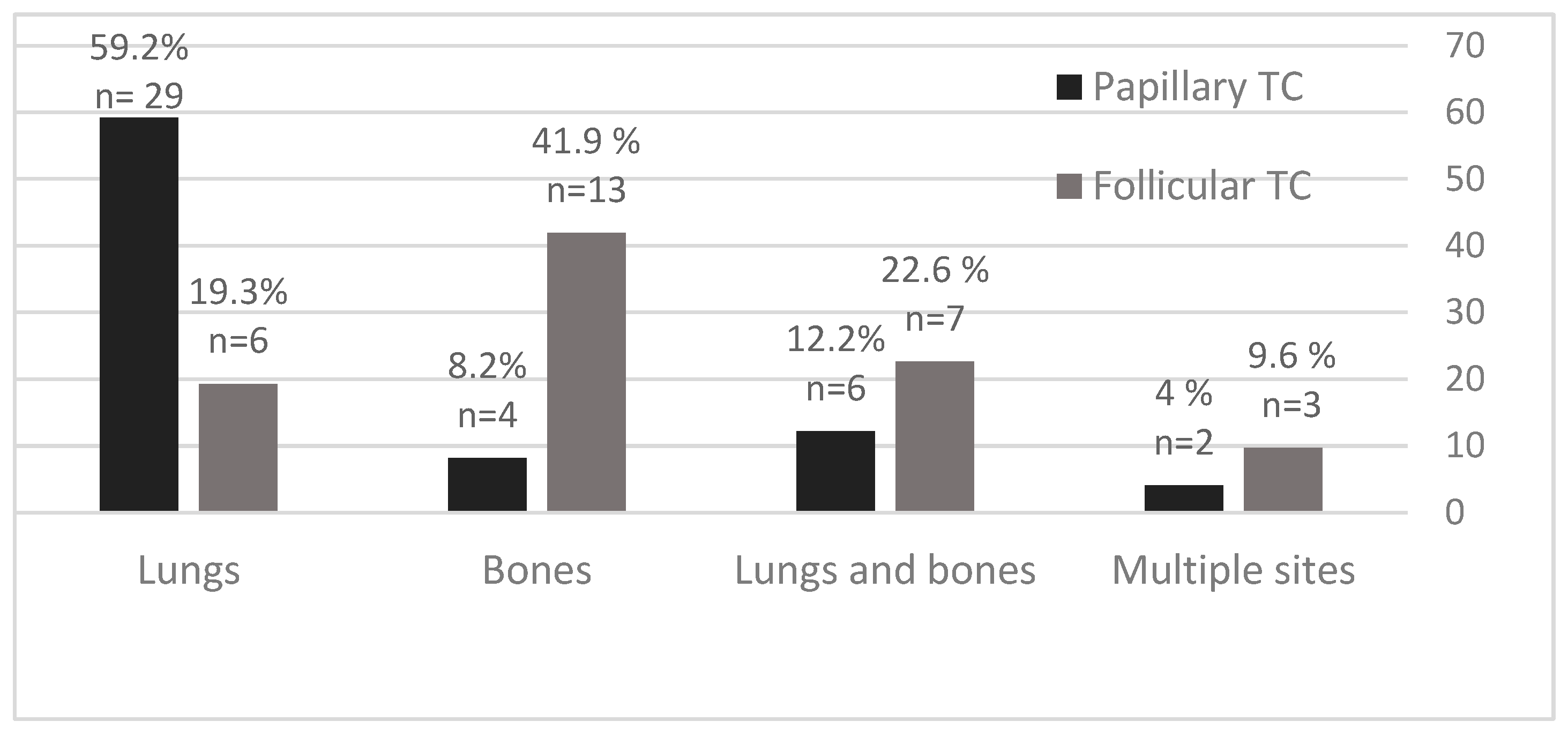
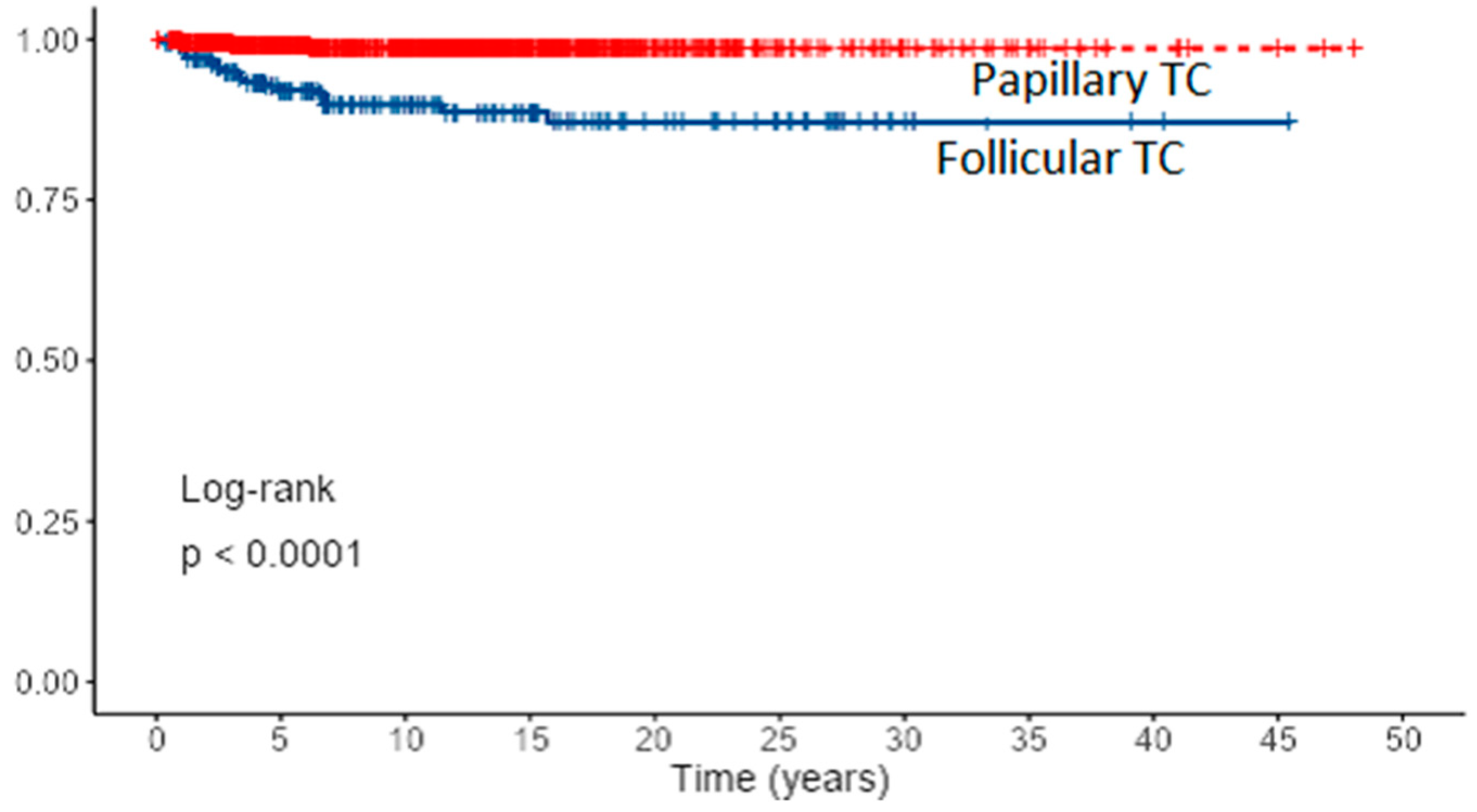
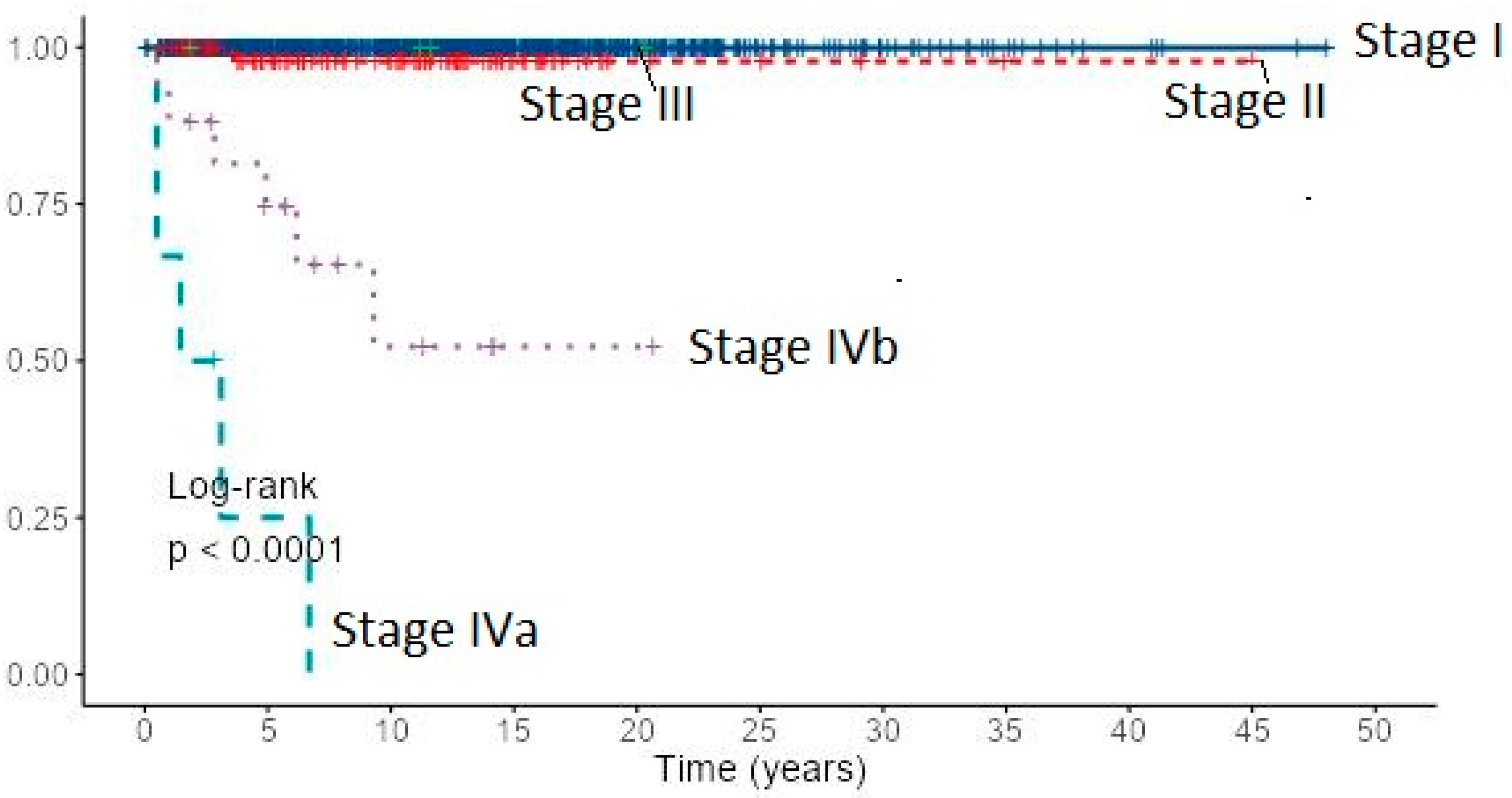
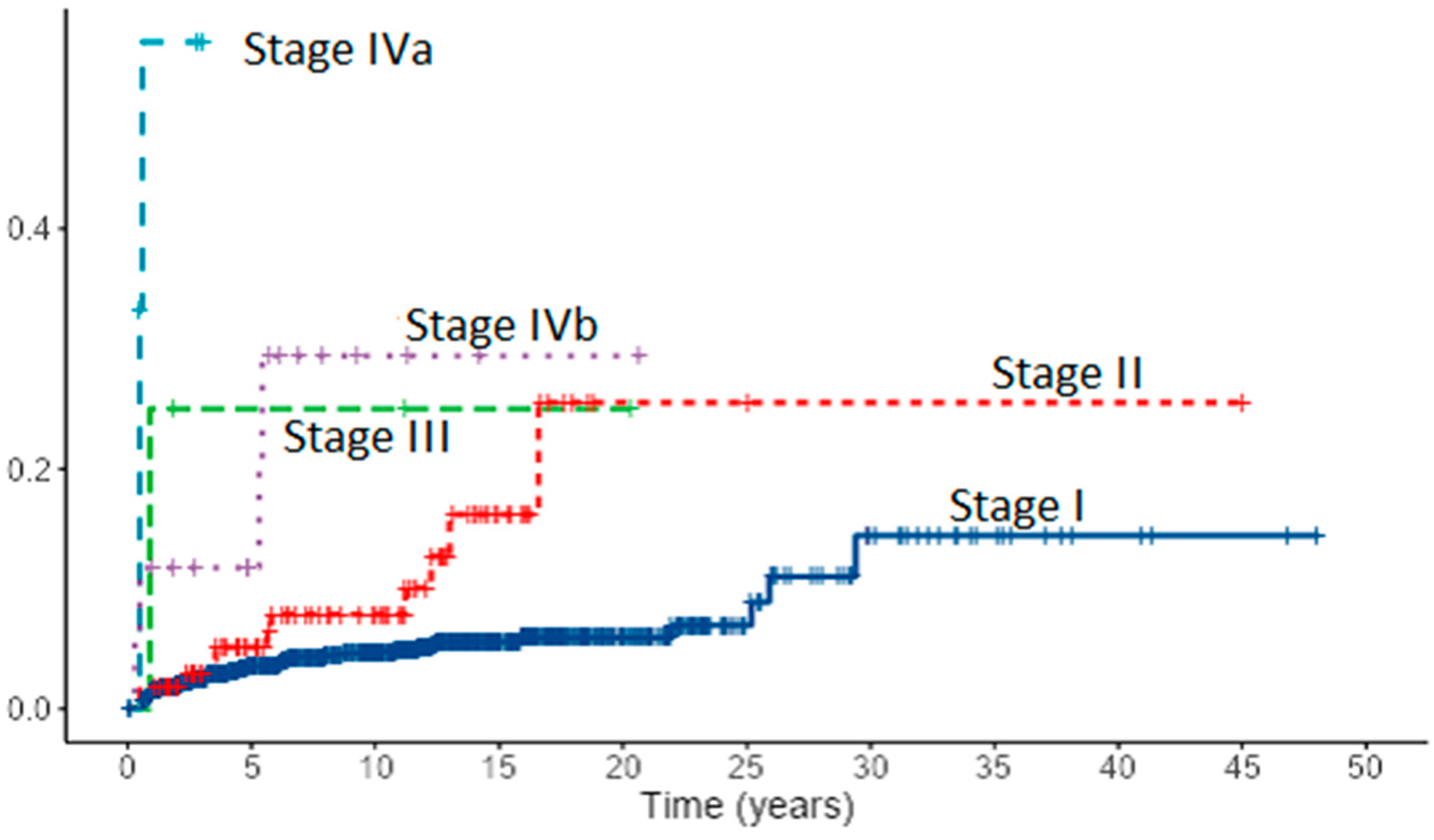
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cancer Today—International Agency for Research on Cancer. Available online: https://gco.iarc.fr/today/ (accessed on 28 February 2022).
- La Vecchia, C.; Malvezzi, M.; Bosetti, C.; Garavello, W.; Bertuccio, P.; Levi, F.; Negri, E. Thyroid Cancer Mortality and Incidence: A Global Overview: Thyroid Cancer Mortality and Incidence. Int. J. Cancer 2015, 136, 2187–2195. [Google Scholar] [CrossRef] [PubMed]
- Hrvatski Zavod za Javno Zdravstvo, Registar za rak Republike Hrvatske. Incidencija raka u Hrvatskoj 2019, Bilten 44, Zagreb. 2021. Available online: https://www.hzjz.hr/wp-content/uploads/2021/12/Bilten44_2019.pdf (accessed on 18 January 2022).
- Dal Maso, L.; Tavilla, A.; Pacini, F.; Serraino, D.; van Dijk, B.A.C.; Chirlaque, M.D.; Capocaccia, R.; Larrañaga, N.; Colonna, M.; Agius, D.; et al. EUROCARE-5 Working Group. Survival of 86,690 patients with thyroid cancer: A population-based study in 29 European countries from EUROCARE-5. Eur. J. Cancer 2017, 77, 140–152. [Google Scholar] [CrossRef] [PubMed]
- Vaccarella, S.; Franceschi, S.; Bray, F.; Wild, C.P.; Plummer, M.; Dal Maso, L. Worldwide Thyroid-Cancer Epidemic? The Increasing Impact of Overdiagnosis. N. Engl. J. Med. 2016, 375, 614–617. [Google Scholar] [CrossRef] [PubMed]
- Cooper, D.S.; Doherty, G.M.; Haugen, B.R.; Kloos, R.T.; Lee, S.L.; Mandel, S.J.; Mazzaferri, E.L.; McIver, B.; Pacini, F.; Schlumberger, M.; et al. Revised American Thyroid Association Management Guidelines for Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2009, 19, 1167–1214. [Google Scholar] [CrossRef] [PubMed]
- Fiorentino, V.; Dell’Aquila, M.; Musarra, T.; Martini, M.; Capodimonti, S.; Fadda, G.; Curatolo, M.; Traini, E.; Raffaelli, M.; Lombardi, C.P.; et al. The Role of Cytology in the Diagnosis of Subcentimeter Thyroid Lesions. Diagnostics 2021, 11, 1043. [Google Scholar] [CrossRef]
- Mazzaferri, E.L.; Kloos, R.T. Carcinoma of follicular epithelium: Radioiodine and other treatments and outcomes. In Werner & Ingbar’s the Thyroid: A Fundamental and Clinical Text, 9th ed.; Braverman, L.E., Utiger, R.D., Eds.; Lippincot Williams & Wilkins: Philadelphia, PA, USA, 2005; pp. 934–966. [Google Scholar]
- Hundahl, S.A.; Fleming, I.D.; Fremgen, A.M.; Menck, H.R. A National Cancer Data Base report on 53,856 cases of thyroid carcinoma treated in the USA, 1985–1995. Cancer 1998, 83, 2638–2648. [Google Scholar] [CrossRef]
- Gilliland, F.D.; Hunt, W.C.; Morris, D.M.; Key, C.R. Prognostic factors for thyroid carcinoma. A population-based study of 15,698 cases from the Surveillance, Epidemiology and End Results (SEER) program 1973–1991. Cancer 1997, 79, 564–573. [Google Scholar] [CrossRef]
- Sobin, L.H.; Gospodarowicz, M.K.; Wittekind, C. TNM Classification of Malignant Tumours, 7th ed.; WileyBlackwell: Oxford, UK, 2010. [Google Scholar]
- Hay, I.D.; Bergstralh, E.J.; Goellner, J.R.; Ebersold, J.R.; Grant, C.S. Predicting outcome in papillary thyroid carcinoma: Development of a reliable prognostic scoring system in a cohort of 1779 patients surgically treated at one institution during 1940 through 1989. Surgery 1993, 114, 1050–1057. [Google Scholar]
- Sugitani, I.; Kasai, N.; Fujimoto, Y.; Yanagisawa, A. A novel classification system for patients with PTC: Addition of the new variables of large (3 cm or greater) nodal metastases and reclassification during the follow-up period. Surgery 2004, 135, 139–148. [Google Scholar] [CrossRef]
- Ito, Y.; Ichihara, K.; Masuoka, H.; Fukushima, M.; Inoue, H.; Kihara, M.; Tomoda, C.; Higashiyama, T.; Takamura, Y.; Kobayashi, K.; et al. Establishment of an Intraoperative Staging System (IStage) by Improving UICC TNM Classification System for Papillary Thyroid Carcinoma. World J. Surg. 2010, 34, 2570–2580. [Google Scholar] [CrossRef]
- Amin, M.B.; Greene, F.L.; Edge, S.B.; Compton, C.C.; Gershenwald, J.E.; Brookland, R.K.; Meyer, L.; Gress, D.M.; Byrd, D.R.; Winchester, D.P. AJCC Cancer Staging Manual, 8th ed.; Springer: New York, NY, USA, 2017. [Google Scholar]
- Cady, B.; Rossi, R. An expanded view of risk-group definition in differentiated thyroid carcinoma. Surgery 1988, 104, 947–953. [Google Scholar] [PubMed]
- Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; Nikiforov, Y.E.; Pacini, F.; Randolph, G.W.; Sawka, A.M.; Schlumberger, M.; et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016, 26, 1–133. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Tang, J.; Kong, D.; Cui, Q.; Wang, K.; Gong, Y.; Wu, G. Impact of Gender and Age on the Prognosis of Differentiated Thyroid Carcinoma: A Retrospective Analysis Based on SEER. Horm. Cancer 2018, 9, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Kusić, Z.; Jukić, T.; Dabelić, N.; Franceschi, M. Croatian Thyroid Society Guidelines for the management of patients with differentiated thyroid cancer. Liječ Vjesn 2008, 130, 213–227. [Google Scholar] [PubMed]
- Pacini, F.; Schlumberger, M.; Dralle, H.; Elisei, R.; Smit, J.W.A.; Wiersinga, W. European Consensus for the Management of Patients with Differentiated Thyroid Carcinoma of the Follicular Epithelium. Eur. J. Endocrinol. 2006, 154, 787–803. [Google Scholar] [CrossRef] [PubMed]
- Takami, H.; Ito, Y.; Okamoto, T.; Onoda, N.; Noguchi, H.; Yoshida, A. Revisiting the Guidelines Issued by the Japanese Society of Thyroid Surgeons and Japan Association of Endocrine Surgeons: A Gradual Move Towards Consensus Between Japanese and Western Practice in the Management of Thyroid Carcinoma. World J. Surg. 2014, 38, 2002–2010. [Google Scholar] [CrossRef]
- Tuttle, R.M.; Ahuja, S.; Avram, A.M.; Bernet, V.J.; Bourguet, P.; Daniels, G.H.; Dillehay, G.; Draganescu, C.; Flux, G.; Führer, D.; et al. Controversies, Consensus, and Collaboration in the Use of 131 I Therapy in Differentiated Thyroid Cancer: A Joint Statement from the American Thyroid Association, the European Association of Nuclear Medicine, the Society of Nuclear Medicine and Molecular Imaging, and the European Thyroid Association. Thyroid 2019, 29, 461–470. [Google Scholar] [CrossRef]
- Campennì, A.; Barbaro, D.; Guzzo, M.; Capoccetti, F.; Giovanella, L. Personalized Management of Differentiated Thyroid Cancer in Real Life—Practical Guidance from a Multidisciplinary Panel of Experts. Endocrine 2020, 70, 280–291. [Google Scholar] [CrossRef]
- Gillanders, S.L.; O’Neill, J.P. Prognostic Markers in Well Differentiated Papillary and Follicular Thyroid Cancer (WDTC). Eur. J. Surg. Oncol. 2018, 44, 286–296. [Google Scholar] [CrossRef]
- Ito, Y.; Kudo, T.; Kihara, M.; Takamura, Y.; Kobayashi, K.; Miya, A.; Miyauchi, A. Prognosis of Low-Risk Papillary Thyroid Carcinoma Patients: Its Relationship with the Size of Primary Tumors. Endocr. J. 2012, 59, 119–125. [Google Scholar] [CrossRef]
- Lang, B.H.-H.; Lo, C.-Y.; Chan, W.-F.; Lam, K.-Y.; Wan, K.-Y. Prognostic Factors in Papillary and Follicular Thyroid Carcinoma: Their Implications for Cancer Staging. Ann. Surg. Oncol. 2007, 14, 730–738. [Google Scholar] [CrossRef] [PubMed]
- Prpić, M.; Jukić, T.; Murgić, J.; Borić, M.; Staničić, J.; Kusić, Z. Postoperative Use of Radioiodine (131-I). Review of Recommendations and Guidelines. Coll. Antropol. 2011, 35, 587–594. [Google Scholar] [PubMed]
- Prpic, M.; Kruljac, I.; Kust, D.; Kirigin, L.S.; Jukic, T.; Dabelic, N.; Bolanca, A.; Kusic, Z. Re-ablation I-131 activity does not predict treatment success in low- and intermediate-risk patients with differentiated thyroid carcinoma. Endocrine 2016, 52, 602–608. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Franceschi, M.; Kusić, Z.; Franceschi, D.; Lukinac, L.; Roncević, S. Thyroglobulin determination, neck ultrasonography and iodine-131 whole-body scintigraphy in differentiated thyroid carcinoma. J. Nucl. Med. 1996, 37, 446–451. [Google Scholar]
- Prpić, M. Thyroglobulin as a Tumor Marker in Differentiated Thyroid Cancer—Clinical Considerations. Acta Clin. Croat. 2018, 57, 518–526. [Google Scholar] [CrossRef]
- Brierley, J.; Tsang, R.; Panzarella, T.; Bana, N. Prognostic Factors and the Effect of Treatment with Radioactive Iodine and External Beam Radiation on Patients with Differentiated Thyroid Cancer Seen at a Single Institution over 40 Years. Clin. Endocrinol. 2005, 63, 418–427. [Google Scholar] [CrossRef]
- Tsang, R.W.; Brierley, J.D.; Simpson, W.J.; Panzarella, T.; Gospodarowicz, M.K.; Sutcliffe, S.B. The Effects of Surgery, Radioiodine, and External Radiation Therapy on the Clinical Outcome of Patients with Differentiated Thyroid Carcinoma. Cancer 1998, 82, 375–388. [Google Scholar] [CrossRef]
- Cushing, S.L.; Palme, C.E.; Audet, N.; Eski, S.; Walfish, P.G.; Freeman, J.L. Prognostic Factors in Well-Differentiated Thyroid Carcinoma. Laryngoscope 2004, 114, 2110–2115. [Google Scholar] [CrossRef]
- Haq, M.; Harmer, C. Differentiated Thyroid Carcinoma with Distant Metastases at Presentation: Prognostic Factors and Outcome. Clin. Endocrinol. 2005, 63, 87–93. [Google Scholar] [CrossRef]
- Shoup, M.; Stojadinovic, A.; Nissan, A.; Ghossein, R.A.; Freedman, S.; Brennan, M.F.; Shah, J.P.; Shaha, A.R. Prognostic Indicators of Outcomes in Patients with Distant Metastases from Differentiated Thyroid Carcinoma. J. Am. Coll. Surg. 2003, 197, 191–197. [Google Scholar] [CrossRef]
- Mazzaferri, E.L.; Jhiang, S.M. Long-Term Impact of Initial Surgical and Medical Therapy on Papillary and Follicular Thyroid Cancer. Am. J. Med. 1994, 97, 418–428. [Google Scholar] [CrossRef]
- Sawka, A.M.; Brierley, J.D.; Tsang, R.W.; Thabane, L.; Rotstein, L.; Gafni, A.; Straus, S.; Goldstein, D.P. An Updated Systematic Review and Commentary Examining the Effectiveness of Radioactive Iodine Remnant Ablation in Well-Differentiated Thyroid Cancer. Endocrinol. Metab. Clin. N. Am. 2008, 37, 457–480. [Google Scholar] [CrossRef] [PubMed]
- Verburg, F.A.; Flux, G.; Giovanella, L.; van Nostrand, D.; Muylle, K.; Luster, M. Differentiated Thyroid Cancer Patients Potentially Benefitting from Postoperative I-131 Therapy: A Review of the Literature of the Past Decade. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 78–83. [Google Scholar] [CrossRef] [PubMed]
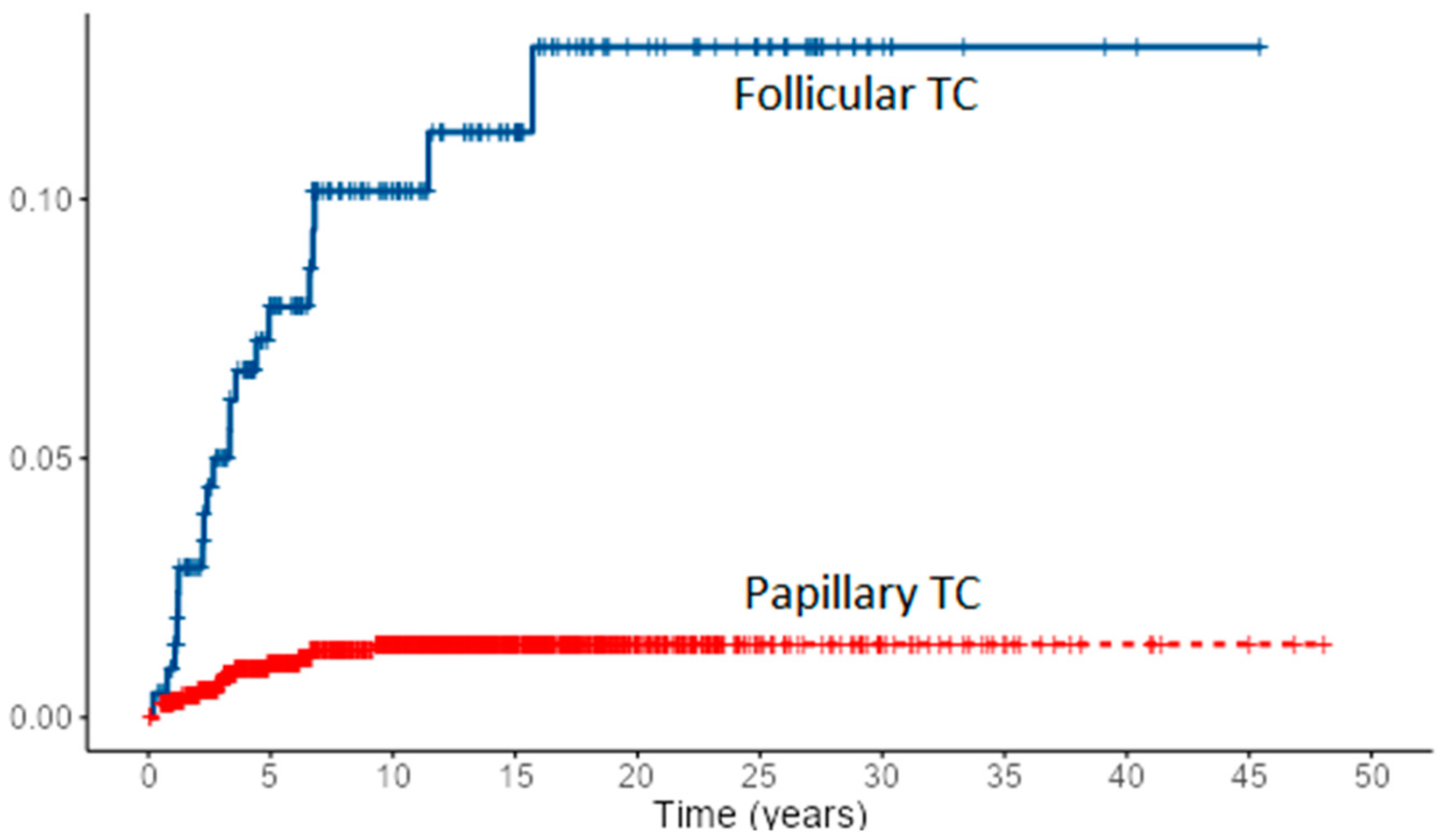
| PTC | FTC | |
|---|---|---|
| N | 1167 | 215 |
| Sex, F/M n (%) | 934 (80%)/233 (20%) | 158 (73%)/57 (27%) |
| Age at diagnosis, median (range) years | 47 (6–83) | 48 (13–81) |
| Tumor size, median (range) mm | 12 (1–100) *** | 32 (7–90) *** |
| Total thyroidectomy | 1162 | 214 |
| Lobectomy | 3 | 1 |
| Thyroglossal duct excision | 2 | 0 |
| Iodine-131 therapy n (%) | 1084 (92.9%) | 210 (97.7%) |
| Cervical nodal metastases et presentation | 254/962 (26.4%) ** | 18/122 (14,8) ** |
| Multifocality | 256/601 (42.6%) *** | 11/204 (5.4%) *** |
| Capsular invasion | 125/714 (17.5%) * | 18/56 (32.1%) * |
| Distant metastases at presentation | 41 (3.5%) *** | 29 (13.5%) *** |
| AJCC 8th edition | ||
| I | 1033 (88.6%) | 168 (78.1%) |
| II | 106 (9.1%) | 21(9.8%) |
| III | 4 (0.3%) | 2 (0.9%) |
| IVa | 6 (0.5%) | 1 (0.5%) |
| IVb | 17 (1.5%) *** | 23 (10.7%) *** |
| Follow-up (median, range) years | 12 (0.2–48) | 11 (0.4–46) |
| Recurrence—neck Recurrence—distant | 71 (6.1%) 8 (0.7%) | 10 (4.7%) 2 (0.9%) |
| Outcome | ||
| Died of disease | 14 (1.2%) *** | 20 (9.3%) *** |
| Persistent disease—local | 33 (2.8%) | 7 (3.3%) |
| Persistent disease—distant | 16 (1.4%) | 7 (3.3%) |
| Disease free | 1104 (94.6%) | 181 (84.1%) |
| TNM Stage | PTC | FTC | ||
|---|---|---|---|---|
| 5-Year (%) | 10-Year (%) | 5-Year (%) | 10-Year (%) | |
| I | 99.9 | 99.9 | 100 | 100 |
| II | 97.8 | 97.8 | 94.4 | 94.4 |
| IVa | 25.0 | 0 | 0 | 0 |
| IVb | 74.0 | 52.3 | 38.0 | 15.2 |
| Factors Associated with Survival | p Value | |
|---|---|---|
| PTC | FTC | |
| Age at diagnosis | <0.001 | <0.001 |
| Female vs. male | <0.001 | 0.044 |
| Primary tumor size | <0.001 | <0.001 |
| Lymph node metastases | 0.012 | <0.001 |
| Capsular invasion | <0.001 | <0.001 |
| Distant metastases | <0.001 | <0.001 |
| TNM stage | ||
| I | - | - |
| II | 0.014 | 0.630 |
| III | 0.998 | 0.995 |
| IVa | <0.001 | 0.008 |
| IVb | <0.001 | <0.001 |
| Neck recurrence | <0.001 | 0.002 |
| New distant metastases | <0.001 | 0.174 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jukić, T.; Blažeković, I.; Franceschi, M.; Ovčariček, P.P.; Butković, M.B.; Dabelić, N.; Granić, R.; Punda, M.; Sonicki, Z.; Vagić, D.; et al. Long-Term Outcome of Differentiated Thyroid Cancer Patients—Fifty Years of Croatian Thyroid Disease Referral Centre Experience. Diagnostics 2022, 12, 866. https://doi.org/10.3390/diagnostics12040866
Jukić T, Blažeković I, Franceschi M, Ovčariček PP, Butković MB, Dabelić N, Granić R, Punda M, Sonicki Z, Vagić D, et al. Long-Term Outcome of Differentiated Thyroid Cancer Patients—Fifty Years of Croatian Thyroid Disease Referral Centre Experience. Diagnostics. 2022; 12(4):866. https://doi.org/10.3390/diagnostics12040866
Chicago/Turabian StyleJukić, Tomislav, Ivan Blažeković, Maja Franceschi, Petra Petranović Ovčariček, Marija Bosak Butković, Nina Dabelić, Roko Granić, Marija Punda, Zdenko Sonicki, Davor Vagić, and et al. 2022. "Long-Term Outcome of Differentiated Thyroid Cancer Patients—Fifty Years of Croatian Thyroid Disease Referral Centre Experience" Diagnostics 12, no. 4: 866. https://doi.org/10.3390/diagnostics12040866
APA StyleJukić, T., Blažeković, I., Franceschi, M., Ovčariček, P. P., Butković, M. B., Dabelić, N., Granić, R., Punda, M., Sonicki, Z., Vagić, D., Fröbe, A., & Kusić, Z. (2022). Long-Term Outcome of Differentiated Thyroid Cancer Patients—Fifty Years of Croatian Thyroid Disease Referral Centre Experience. Diagnostics, 12(4), 866. https://doi.org/10.3390/diagnostics12040866






