Measurement of the Depth of Lesions on Proximal Surfaces with SWIR Multispectral Transillumination and Reflectance Imaging
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample Preparation
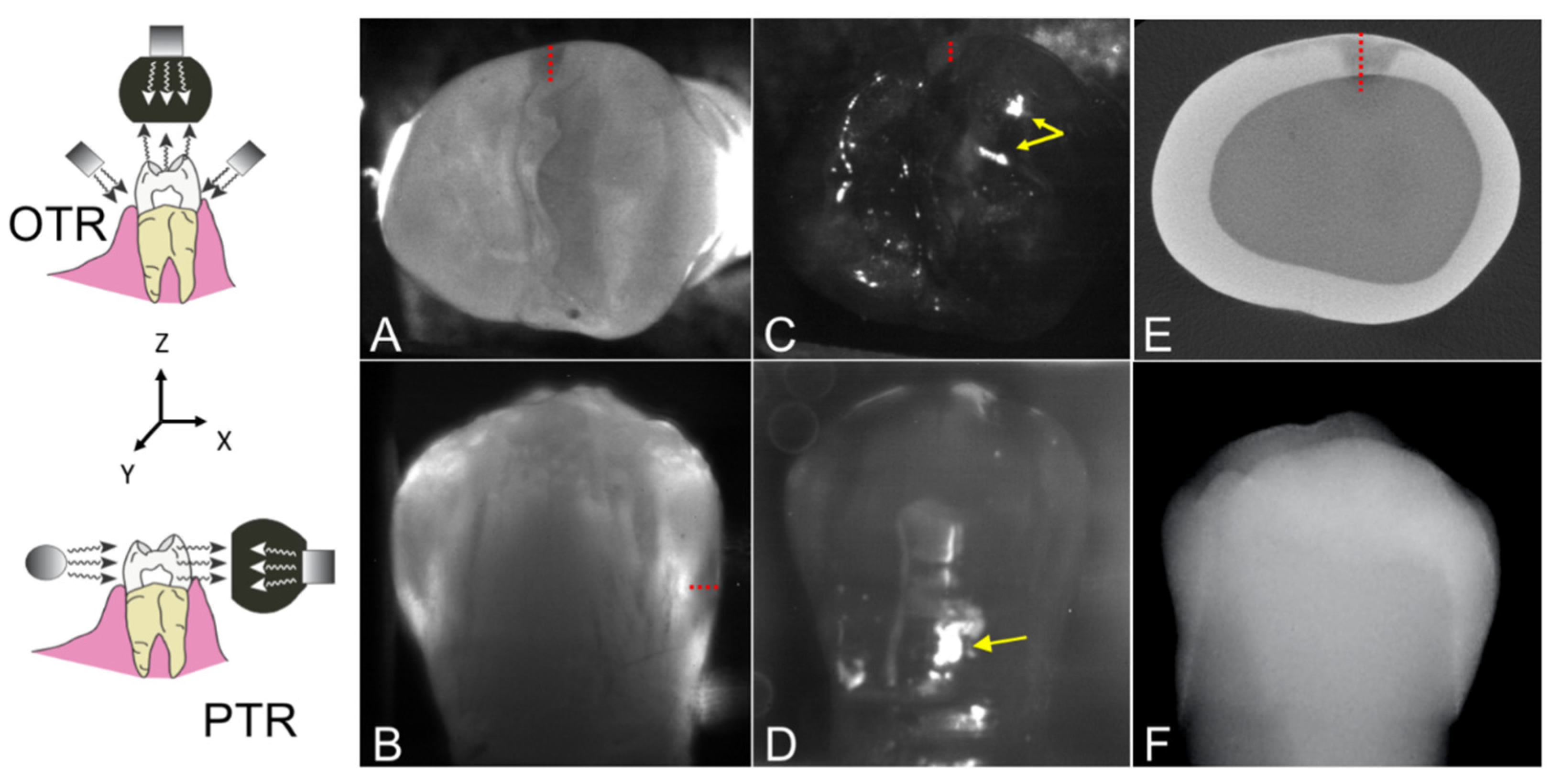
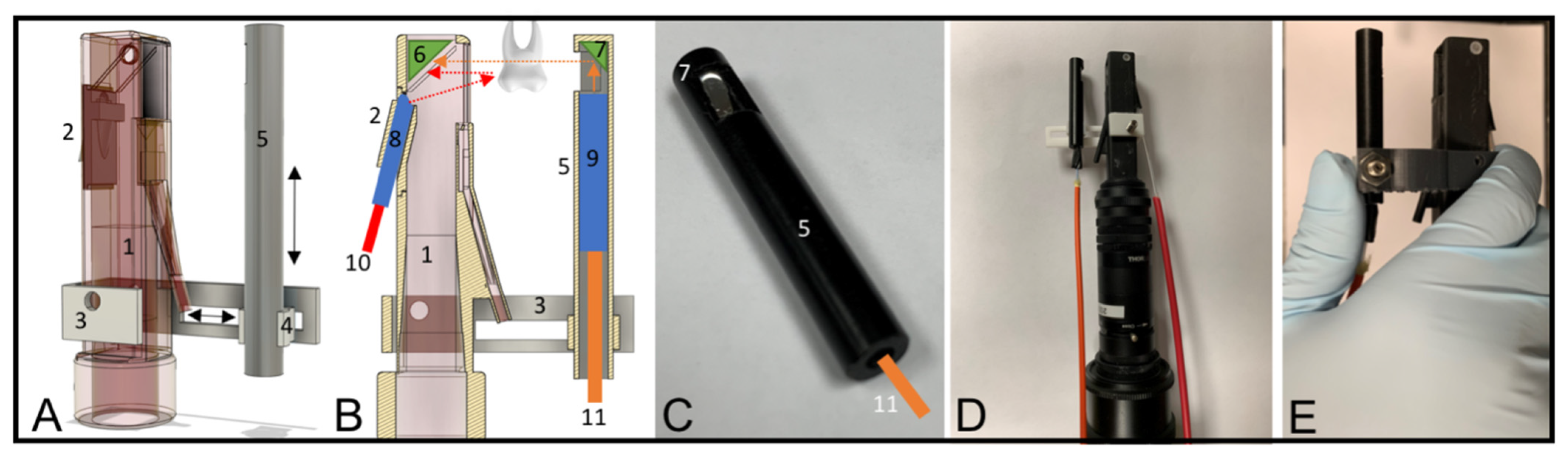
2.2. Design and Fabrication of the Dual Proximal Reflectance and Transillumination SWIR Probe
2.3. Image Acquisition and Analysis
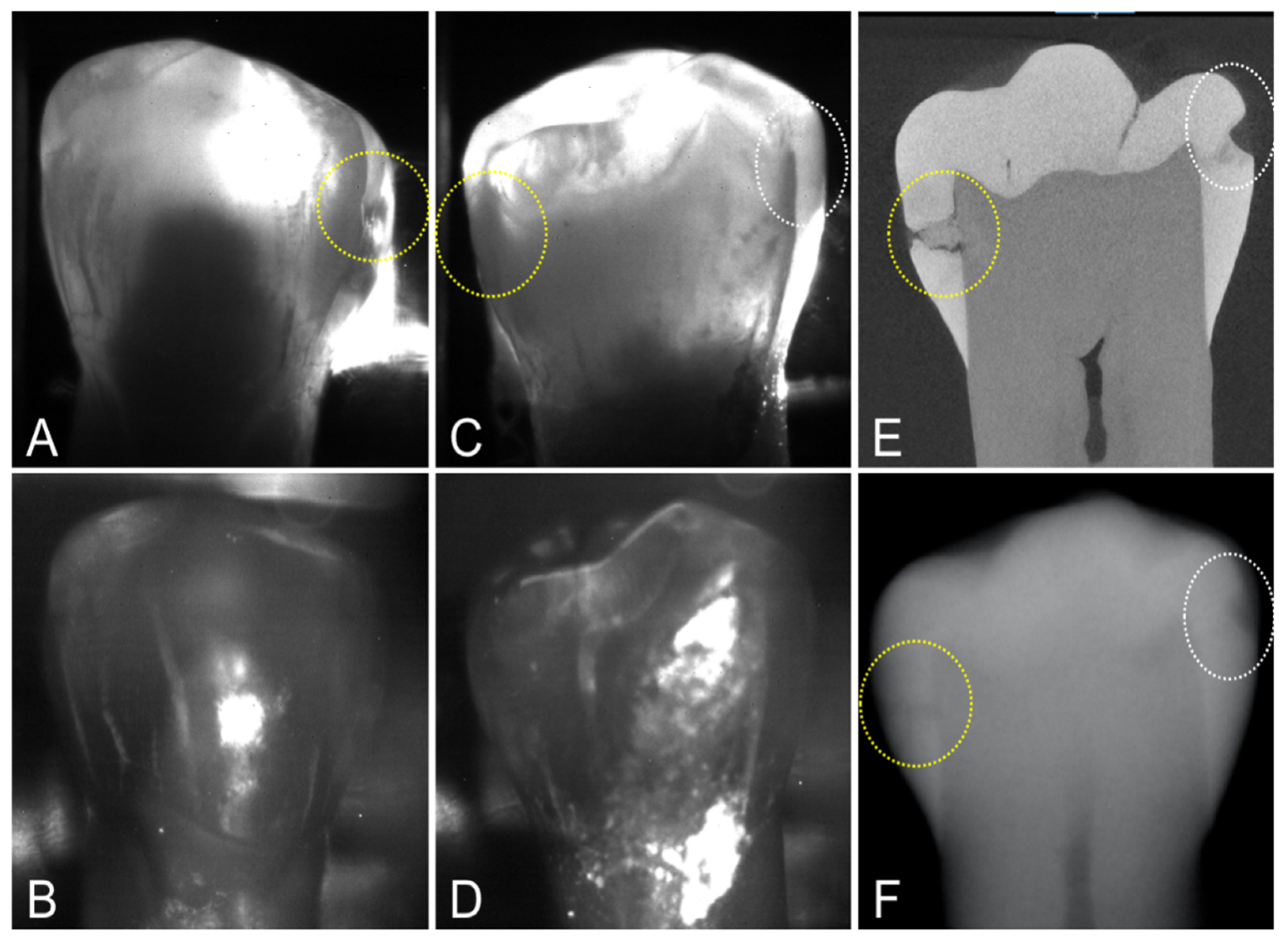
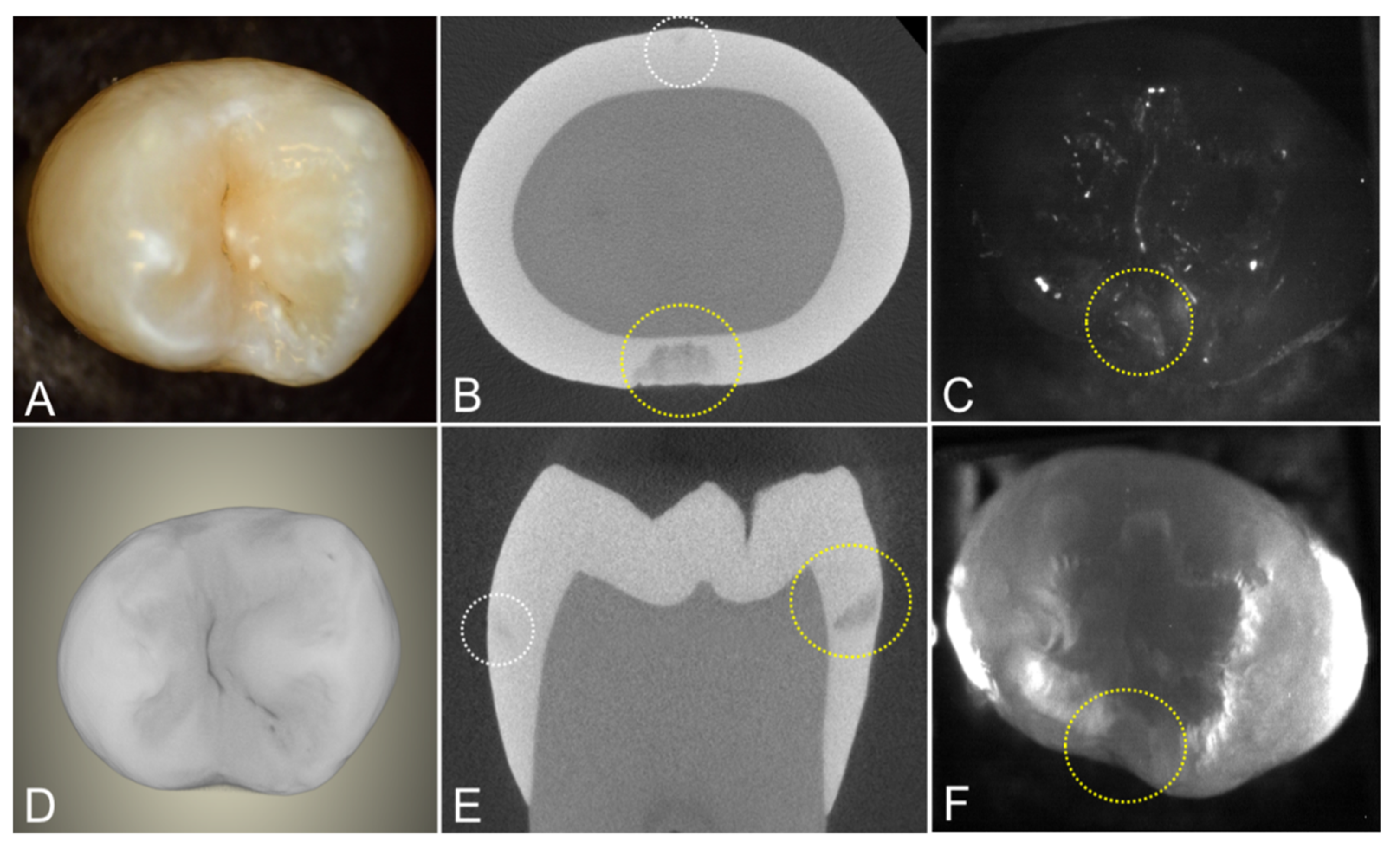
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Buhler, C.; Ngaotheppitak, P.; Fried, D. Imaging of occlusal dental caries (decay) with near-IR light at 1310-nm. Opt. Expr. 2005, 13, 573–582. [Google Scholar] [CrossRef] [PubMed]
- Staninec, M.; Lee, C.; Darling, C.L.; Fried, D. In vivo near-IR imaging of approximal dental decay at 1,310 nm. Lasers Surg. Med. 2010, 42, 292–298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, G.; Jones, R.S.; Fried, D. Transillumination of interproximal caries lesions with 830-nm light. In Proceedings of the Lasers in Dentistry X, Proc SPIE, San Jose, CA, USA, 28 May 2004; Volume 5313, pp. 17–22. [Google Scholar]
- Jones, R.S.; Huynh, G.D.; Jones, G.C.; Fried, D. Near-IR Transillumination at 1310-nm for the Imaging of Early Dental Caries. Opt. Expr. 2003, 11, 2259–2265. [Google Scholar] [CrossRef] [PubMed]
- Fried, D.; Featherstone, J.D.B.; Darling, C.L.; Jones, R.S.; Ngaotheppitak, P.; Buehler, C.M. Early Caries Imaging and Monitoring with Near-IR Light. Dent. Clin. N. Am. Incip. Hidden Caries 2005, 49, 771–794. [Google Scholar] [CrossRef] [PubMed]
- Hirasuna, K.; Fried, D.; Darling, C.L. Near-IR imaging of developmental defects in dental enamel. J. Biomed. Opt. 2008, 13, 044011. [Google Scholar] [CrossRef]
- Lee, C.; Lee, D.; Darling, C.L.; Fried, D. Nondestructive assessment of the severity of occlusal caries lesions with near-infrared imaging at 1310 nm. J. Biomed. Opt. 2010, 15, 047011. [Google Scholar] [CrossRef] [Green Version]
- Karlsson, L.; Maia, A.M.A.; Kyotoku, B.B.C.; Tranaeus, S.; Gomes, A.S.L.; Margulis, W. Near-infrared transillumination of teeth: Measurement of a system performance. J. Biomed. Opt. 2010, 15, 036001. [Google Scholar]
- Simon, J.C.; Lucas, S.A.; Lee, R.C.; Staninec, M.; Tom, H.; Chan, K.H.; Darling, C.L.; Fried, D. Near-IR Transillumination and Reflectance Imaging at 1300-nm and 1500–1700-nm for in vivo Caries Detection. Lasers Surg. Med. 2016, 48, 828–836. [Google Scholar] [CrossRef] [Green Version]
- Kuhnisch, J.; Sochtig, F.; Pitchika, V.; Laubender, R.; Neuhaus, K.W.; Lussi, A.; Hickel, R. In vivo validation of near-infrared light transillumination for interproximal dentin caries detection. Clin. Oral. Investig. 2015, 20, 821–829. [Google Scholar] [CrossRef]
- Sochtig, F.; Hickel, R.; Kuhnisch, J. Caries detection and diagnostics with near-infrared light transillumination: Clinical experiences. Quint. Int. 2014, 45, 531–538. [Google Scholar]
- Abdelaziz, M.; Krejci, I. DIAGNOcam—A Near Infrared Digital Imaging Transillumination (NIDIT) technology. Int. J. Esthet Dent. 2015, 10, 158–165. [Google Scholar] [PubMed]
- Abdelaziz, M.; Krejci, I.; Fried, D. Enhancing the detection of proximal cavities on near infrared transillumination images with Indocyanine Green (ICG) as a contrast medium: In vitro proof of concept studies. J. Dent. 2019, 91, 103222. [Google Scholar] [CrossRef] [PubMed]
- Abdelaziz, M.; Krejci, I.; Perneger, T.; Feilzer, A.; Vazquez, L. Near infrared transillumination compared with radiography to detect and monitor proximal caries: A clinical retrospective study. J. Dent. 2018, 70, 40–45. [Google Scholar] [CrossRef]
- Ng, C.; Almaz, E.C.; Simon, J.C.; Fried, D.; Darling, C.L. Near-infrared imaging of demineralization on the occlusal surfaces of teeth without the interference of stains. J. Biomed. Opt. 2019, 24, 036002. [Google Scholar] [CrossRef] [Green Version]
- Chung, S.; Fried, D.; Staninec, M.; Darling, C.L. Multispectral near-IR reflectance and transillumination imaging of teeth. Biomed. Opt. Expr. 2011, 2, 2804–2814. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fried, W.A.; Chan, K.H.; Fried, D.; Darling, C.L. High Contrast Reflectance Imaging of Simulated Lesions on Tooth Occlusal Surfaces at Near-IR Wavelengths. Lasers Surg. Med. 2013, 45, 533–541. [Google Scholar] [CrossRef] [Green Version]
- Salsone, S.; Taylor, A.; Gomez, J.; Pretty, I.; Ellwood, R.; Dickinson, M.; Lombardo, G.; Zakian, C. Histological validation of near-infrared reflectance multispectral imaging technique for caries detection and quantification. J. Biomed. Opt. 2012, 17, 076009. [Google Scholar] [CrossRef] [Green Version]
- Zakian, C.; Pretty, I.; Ellwood, R. Near-infrared hyperspectral imaging of teeth for dental caries detection. J. Biomed. Opt. 2009, 14, 064047. [Google Scholar] [CrossRef] [Green Version]
- Tom, H.; Simon, J.C.; Chan, K.H.; Darling, C.L.; Fried, D. Near-infrared imaging of demineralization under sealants. J. Biomed. Opt. 2014, 19, 77003. [Google Scholar] [CrossRef] [Green Version]
- Simon, J.C.; Lucas, S.A.; Lee, R.C.; Darling, C.L.; Staninec, M.; Vaderhobli, R.; Pelzner, R.; Fried, D. Near-infrared imaging of secondary caries lesions around composite restorations at wavelengths from 1300-1700-nm. Dent. Mater. 2016, 32, 587–595. [Google Scholar] [CrossRef] [Green Version]
- Kooistra, S.; Dennison, J.B.; Yaman, P.; Burt, B.A.; Taylor, G.W. Radiographic versus clinical extension of Class II carious lesions using an F-speed film. Oper. Dent. 2005, 30, 719–726. [Google Scholar] [PubMed]
- Jessee, S.A.; Makins, S.R.; Bretz, W.A. Accuracy of proximal caries depth determination using two intraoral film speeds. Gen. Dent. 1999, 47, 88–93. [Google Scholar] [PubMed]
- Bin-Shuwaish, M.; Dennison, J.B.; Yaman, P.; Neiva, G. Estimation of clinical axial extension of Class II caries lesions with ultraspeed and digital radiographs: An in-vivo study. Oper. Dent. 2008, 33, 613–621. [Google Scholar] [CrossRef]
- Simon, J.C.; Lucas, S.A.; Staninec, M.; Tom, H.; Chan, K.H.; Darling, C.L.; Fried, D. Transillumination and reflectance probes for near-IR imaging of dental caries. In Proceedings of the Lasers in Dentistry XX, Proc SPIE, San Francisco, CA, USA, 18 February 2014; Volume 8929, pp. D1–D7. [Google Scholar]
- Simon, J.C.; Curtis, D.A.; Darling, C.L.; Fried, D. Multispectral near-infrared reflectance and transillumination imaging of occlusal carious lesions: Variations in lesion contrast with lesion depth. In Proceedings of the Lasers in Dentistry XXIV, Proc SPI, San Francisco, CA, USA, 8 February 2018; Volume 10473, p. 1047305. [Google Scholar]
- Simon, J.C.; Darling, C.L.; Fried, D. Assessment of cavitation in artificial approximal dental lesions with near-IR imaging. In Proceedings of the Lasers in Dentistry XXIII, Proc SPIE, San Francisco, CA, USA, 8 February 2017; Volume 10044, p. 1004407. [Google Scholar]
- Zhu, Y.; Abdelaziz, M.; Simon, J.; Le, O.; Fried, D. Dual short wavelength infrared transillumination/reflectance mode imaging for caries detection. J. Biomed. Opt. 2021, 26, 043004. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Chang, N.; Fried, W.A.; Yang, V.; Fried, D. A dual handheld SWIR transillumination/reflectance probe for imaging lesions on tooth occlusal and proximal surfaces. In Proceedings of the Lasers in Dentistry XXVI, Proc SPIE, San Francisco, CA, USA, 19 February 2020; Volume 11217, p. 112170J. [Google Scholar]
- Zhu, Y.; Simon, J.; Ng, C.; Fried, D. Compact in vivo handheld dual SWIR transillumination/reflectance imaging system for the detection of proximal and occlusal lesions. In Photonic Therapeutics and Diagnostics in Dentistry, Head and Neck Surgery, and Otolaryngology; SPIE: Bellingham, DC, USA, 2021; p. 116270N. [Google Scholar]
- Lee, R.C.; Darling, C.L.; Fried, D. Assessment of remineralization via measurement of dehydration rates with thermal and near-IR reflectance imaging. J. Dent. 2015, 43, 1032–1042. [Google Scholar] [CrossRef] [Green Version]
- Lee, R.C.; Darling, C.L.; Fried, D. Activity assessment of root caries lesions with thermal and near-infrared imaging methods. J. Biophoton. 2016, 10, 433–445. [Google Scholar] [CrossRef] [Green Version]
- Lee, R.C.; Staninec, M.; Le, O.; Fried, D. Infrared methods for assessment of the activity of natural enamel caries lesions. IEEE J. Select. Top. Quant. Electron. 2014, 22, 6803609. [Google Scholar] [CrossRef] [Green Version]
- Yang, V.B.; Curtis, D.A.; Fried, D. Cross-polarization reflectance imaging of root caries and dental calculus at wavelengths from 400–2350-nm. J. Biophoton. 2018, 11, e201800113. [Google Scholar] [CrossRef]
- Kashirtsev, F.; Tressel, J.; Simon, J.C.; Fried, D. High contrast imaging of dental fluorosis in the short wavelength infrared (SWIR). J. Biophoton. 2021, 14, e202100145. [Google Scholar] [CrossRef]


| Proximal Transillumination | Occlusal Transillumination | Occlusal Reflectance | Radiograph | |
|---|---|---|---|---|
| Mean Lesion Contrast ± s.d. | 0.49 ± 0.11 | 0.45 ± 0.16 | 0.55 ± 0.21 | 0.26 ± 0.10 |
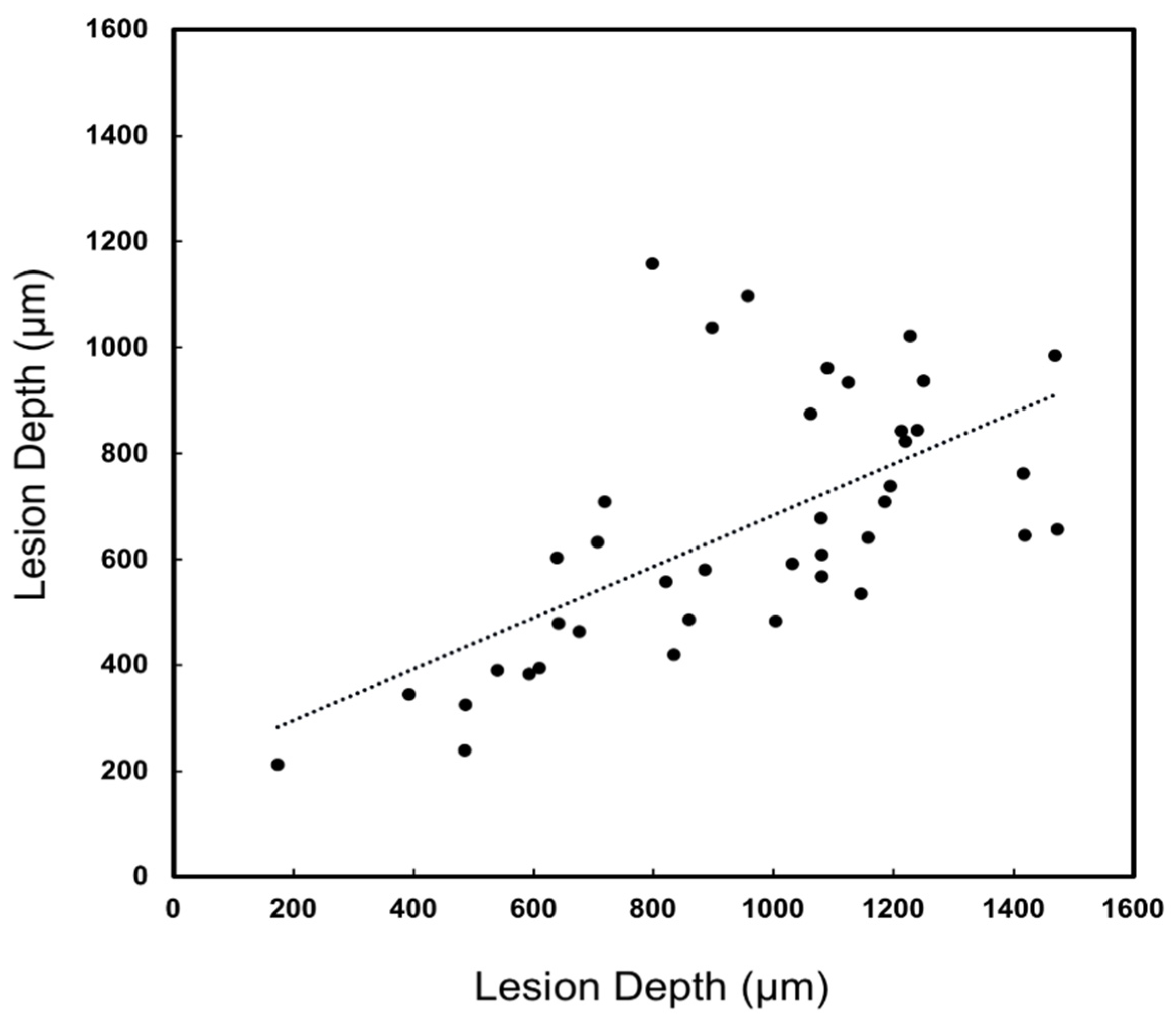
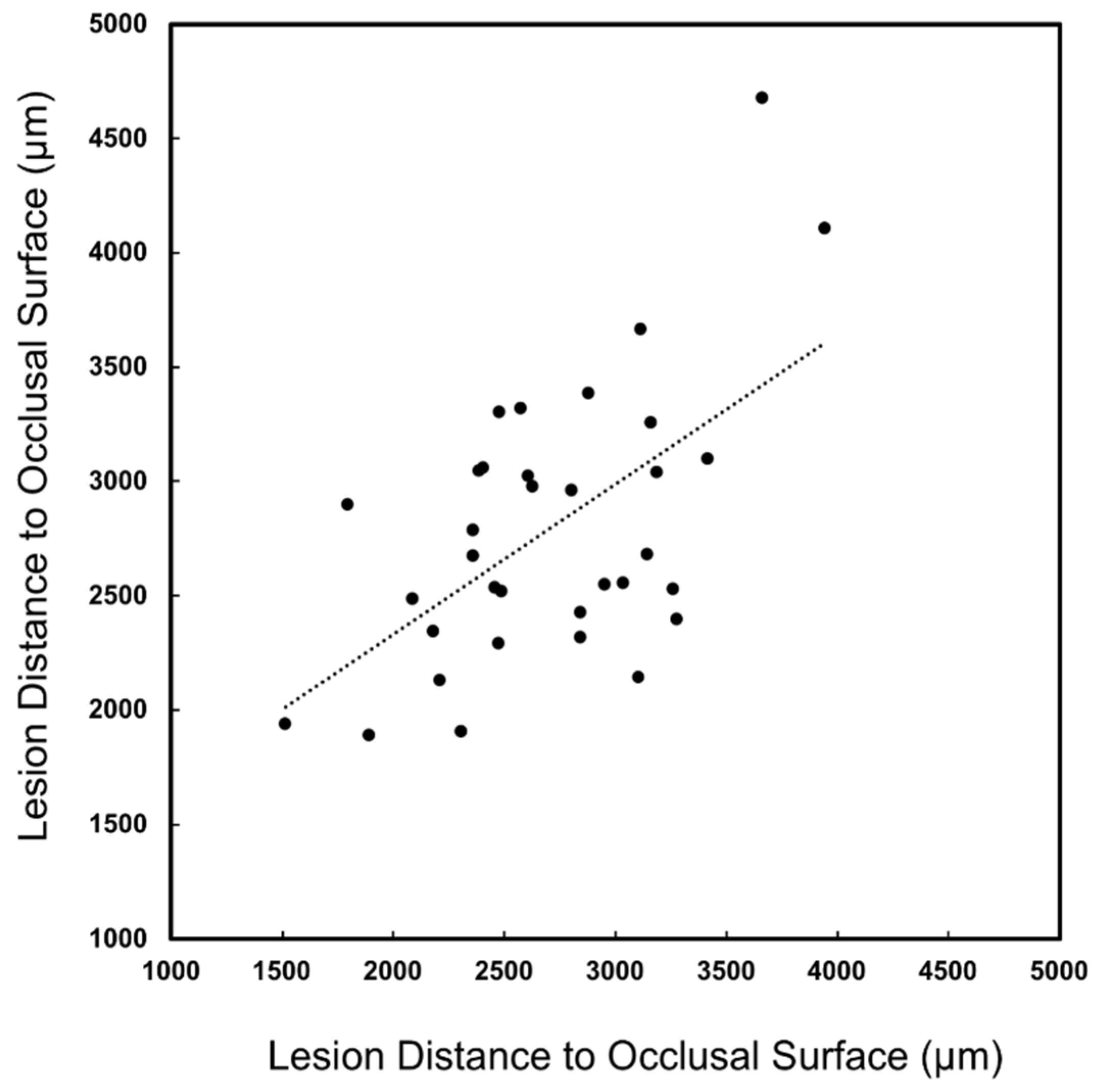
| Lesion Depth Correlation (R2) | 0.40 | 0.80 | 0.38 | N/A |
| Lesions Visible (N) | 40 | 51 | 45 | 22 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, Y.; Fried, D. Measurement of the Depth of Lesions on Proximal Surfaces with SWIR Multispectral Transillumination and Reflectance Imaging. Diagnostics 2022, 12, 597. https://doi.org/10.3390/diagnostics12030597
Zhu Y, Fried D. Measurement of the Depth of Lesions on Proximal Surfaces with SWIR Multispectral Transillumination and Reflectance Imaging. Diagnostics. 2022; 12(3):597. https://doi.org/10.3390/diagnostics12030597
Chicago/Turabian StyleZhu, Yihua, and Daniel Fried. 2022. "Measurement of the Depth of Lesions on Proximal Surfaces with SWIR Multispectral Transillumination and Reflectance Imaging" Diagnostics 12, no. 3: 597. https://doi.org/10.3390/diagnostics12030597
APA StyleZhu, Y., & Fried, D. (2022). Measurement of the Depth of Lesions on Proximal Surfaces with SWIR Multispectral Transillumination and Reflectance Imaging. Diagnostics, 12(3), 597. https://doi.org/10.3390/diagnostics12030597






