Evaluation of the Maxillary Sinus of Patients with Maxillary Posterior Implants: A CBCT Cross-Sectional Study
Abstract
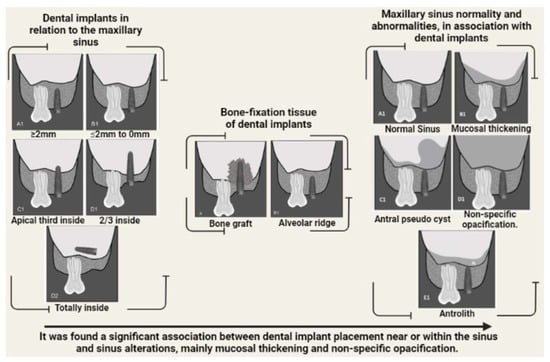
:1. Introduction
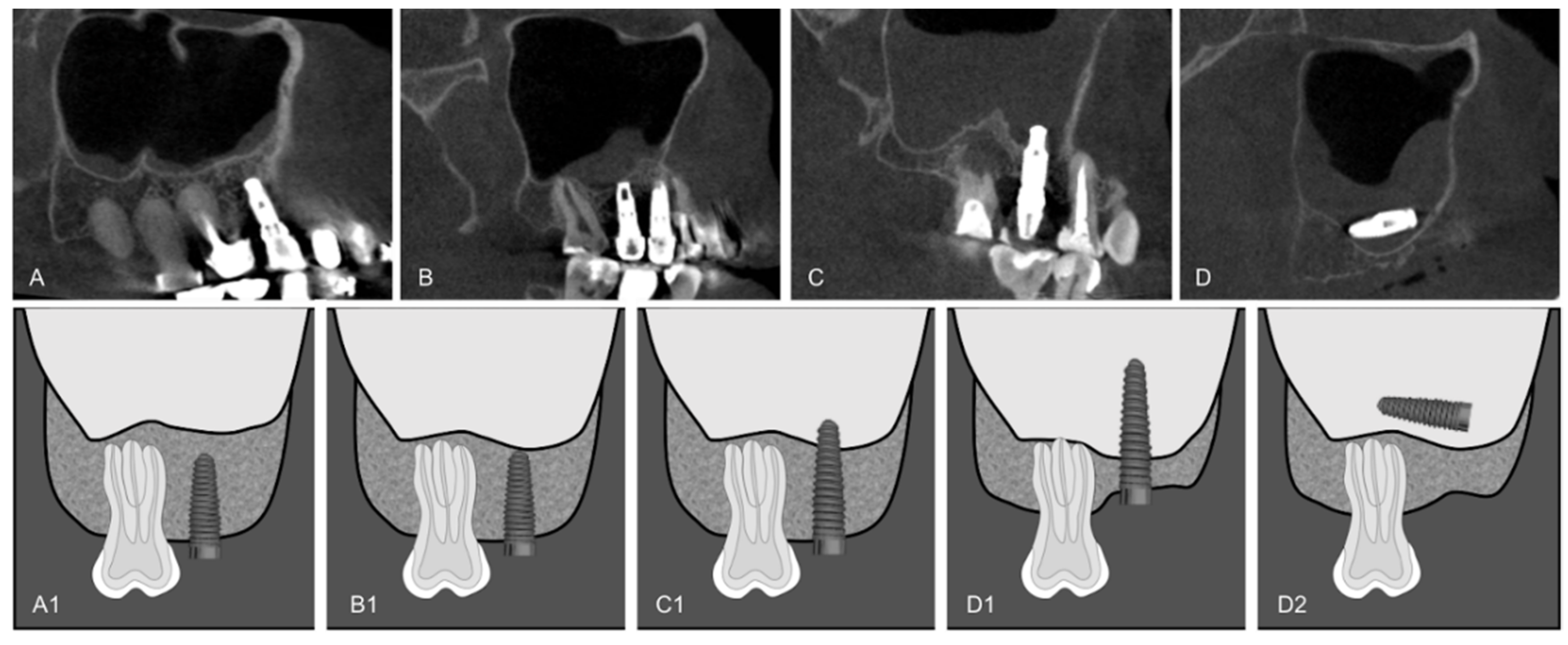
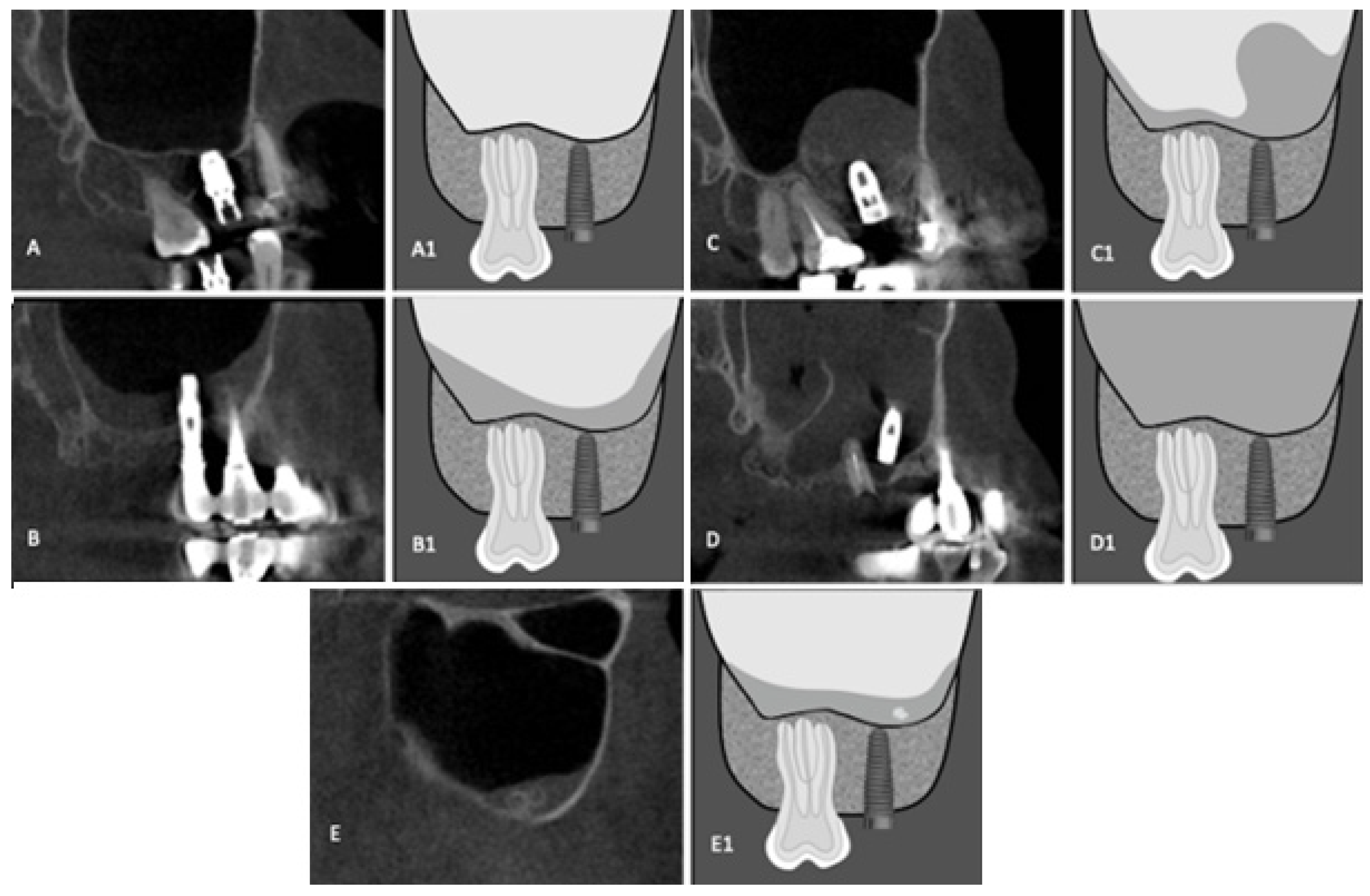
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jeong, K.I.; Kim, S.G.; Oh, J.S.; You, J.S. Implants Displaced Into the Maxillary Sinus: A Systematic Review. Implant Dent. 2016, 25, 547–551. [Google Scholar] [CrossRef] [PubMed]
- Biafora, M.; Bertazzoni, G.; Trimarchi, M. Maxillary sinusitis caused by dental implants extending into the maxillary sinus and the nasal cavities. J. Prosthodont. 2014, 23, 227–231. [Google Scholar] [CrossRef] [PubMed]
- Vogiatzi, T.; Kloukos, D.; Scarfe, W.C.; Bornstein, M.M. Incidence of anatomical variations and disease of the maxillary sinuses as identified by cone beam computed tomography: A systematic review. Int. J. Oral Maxillofac. Implants 2014, 29, 1301–1314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patel, N.A.; Ferguson, B.J. Odontogenic sinusitis: An ancient but under-appreciated cause of maxillary sinusitis. Curr. Opin. Otolaryngol. Head Neck Surg. 2012, 20, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Park, J.S.; Kim, H.T.; Lee, C.H.; Park, Y.H.; Bae, J.H. Clinical features and treatment outcomes of dental implant-related paranasal sinusitis: A 2-year prospective observational study. Clin. Oral Implants Res. 2016, 27, e100–e104. [Google Scholar] [CrossRef] [PubMed]
- Longhini, A.B.; Branstetter, B.F.; Ferguson, B.J. Unrecognized odontogenic maxillary sinusitis: A cause of endoscopic sinus surgery failure. Am. J. Rhinol. Allergy 2010, 24, 296–300. [Google Scholar] [CrossRef]
- Marin, S.; Kirnbauer, B.; Rugani, P.; Payer, M.; Jakse, N. Potential risk factors for maxillary sinus membrane perforation and treatment outcome analysis. Clin. Implant Dent. Relat. Res. 2019, 21, 66–72. [Google Scholar] [CrossRef] [Green Version]
- Harris, D.; Horner, K.; Gröndahl, K.; Jacobs, R.; Helmrot, E.; Benic, G.I.; Bornstein, M.M.; Dawood, A.; Quirynen, M.E.A.O. guidelines for the use of diagnostic imaging in implant dentistry 2011. A consensus workshop organized by the European Association for Osseointegration at the Medical University of Warsaw. Clin. Oral Implants Res. 2011, 23, 1243–1253. [Google Scholar] [CrossRef]
- Jung, J.-H.; Choi, B.-H.; Jeong, S.-M.; Li, J.; Lee, S.-H.; Lee, H.-J. A retrospective study of the effects on sinus complications of exposing dental implants to the maxillary sinus cavity. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 103, 623–625. [Google Scholar] [CrossRef]
- Felisati, G.; Chiapasco, M.; Lozza, P.; Saibene, A.M.; Pipolo, C.; Zaniboni, M.; Biglioli, F.; Borloni, R. Sinonasal complications resulting from dental treatment: Outcome-oriented proposal of classification and surgical protocol. Am. J. Rhinol. Allergy 2013, 27, e101–e106. [Google Scholar] [CrossRef]
- Nunes, C.A.B.C.M.; Guedes, O.A.; Alencar, A.H.G.; Peters, O.A.; Estrela, C.R.A.; Estrela, C. Evaluation of Periapical Lesions and Their Association with Maxillary Sinus Abnormalities on Cone-beam Computed Tomographic Images. J. Endod. 2016, 42, 42–46. [Google Scholar] [CrossRef] [PubMed]
- Mishra, S.K.; Chowdhary, R.; Chrcanovic, B.R.; Brånemark, P.-I. Osseoperception in Dental Implants: A Systematic Review. J. Prosthodont. 2016, 25, 185–195. [Google Scholar] [CrossRef] [PubMed]
- Abi Najm, S.; Malis, D.; El Hage, M.; Rahban, S.; Carrel, J.-P.; Bernard, J.-P. Potential adverse events of endosseous dental implants penetrating the maxillary sinus: Long-term clinical evaluation. Laryngoscope 2013, 123, 2958–2961. [Google Scholar] [CrossRef] [Green Version]
- Ridaura-Ruiz, L.; Figueiredo, R.; Guinot-Moya, R.; Piñera-Penalva, M.; Sanchez-Garcés, M.A.; Valmaseda-Castellón, E.; Gay-Escoda, C. Accidental displacement of dental implants into the maxillary sinus: A report of nine cases. Clin. Implant Dent. Relat. Res. 2009, 11, e38–e45. [Google Scholar] [CrossRef]
- Goodacre, C.J.; Bernal, G.; Rungcharassaeng, K.; Kan, J.Y.K. Clinical complications with implants and implant prostheses. J. Prosthet. Dent. 2003, 90, 121–132. [Google Scholar] [CrossRef] [PubMed]
- Mehra, P.; Jeong, D. Maxillary sinusitis of odontogenic origin. Curr. Allergy Asthma Rep. 2009, 9, 238–243. [Google Scholar] [CrossRef]
- Zimbler, M.S.; Lebowitz, R.A.; Glickman, R.; Brecht, L.E.; Jacobs, J.B. Antral augmentation, osseointegration, and sinusitis: The otolaryngologist’s perspective. Am. J. Rhinol. 1998, 12, 311–316. [Google Scholar] [CrossRef]
- Raghoebar, G.M.; van Weissenbruch, R.; Vissink, A. Rhino-sinusitis related to endosseous implants extending into the nasal cavity. A case report. Int. J. Oral Maxillofac. Surg. 2004, 33, 312–314. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.H.; Choi, B.H.; Zhu, S.J.; Lee, S.H.; Huh, J.Y.; You, T.M.; Lee, H.J.; Li, J. The effects of exposing dental implants to the maxillary sinus cavity on sinus complications. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 102, 602–605. [Google Scholar] [CrossRef]
- Tabrizi, R.; Amid, R.; Taha Özkan, B.; Khorshidi, H.; Langner, N.J. Effects of Exposing Dental Implant to the Maxillary Sinus Cavity. J. Craniofac. Surg. 2012, 23, 767–769. [Google Scholar] [CrossRef]
- Tadinada, A.; Fung, K.; Thacker, S.; Mahdian, M.; Jadhav, A.; Schincaglia, G.P. Radiographic evaluation of the maxillary sinus prior to dental implant therapy: A comparison between two-dimensional and three-dimensional radiographic imaging. Imaging Sci. Dent. 2015, 45, 169–174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malina-Altzinger, J.; Damerau, G.; Grätz, K.W.; Stadlinger, P.B. Evaluation of the maxillary sinus in panoramic radiography—A comparative study. Int. J. Implant Dent. 2015, 1, 17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dau, M.; Marciak, P.; Al-Nawas, B.; Staedt, H.; Alshiri, A.; Frerich, B.; Kämmerer, P.W. Evaluation of symptomatic maxillary sinus pathologies using panoramic radiography and cone beam computed tomography—Influence of professional training. Int. J. Implant Dent. 2017, 3, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shahbazian, M.; Jacobs, R. Diagnostic value of 2D and 3D imaging in odontogenic maxillary sinusitis: A review of literature. J. Oral Rehabil. 2012, 39, 294–300. [Google Scholar] [CrossRef]
- Simuntis, R.; Kubilius, R.; Padervinskis, E.; Ryškienė, S.; Tušas, P.; Vaitkus, S. Clinical efficacy of main radiological diagnostic methods for odontogenic maxillary sinusitis. Eur. Arch. Otorhinolaryngol. 2017, 274, 3651–3658. [Google Scholar] [CrossRef]
- Liang, X.; Jacobs, R.; Hassan, B.; Li, L.; Pauwels, R.; Corpas, L.; Souza, P.C.; Martens, W.; Shahbazian, M.; Alonso, A.; et al. A comparative evaluation of cone beam computed tomography (CBCT) and multi-slice CT (MSCT) Part I. On subjective image quality. Eur. J. Radiol. 2010, 75, 265–269. [Google Scholar] [CrossRef]
- Shahbazian, M.; Vandewoude, C.; Wyatt, J.; Jacobs, R. Comparative assessment of panoramic radiography and CBCT imaging for radiodiagnostics in the posterior maxilla. Clin. Oral Investig. 2014, 18, 293–300. [Google Scholar] [CrossRef]
- Maillet, M.; Bowles, W.R.; McClanahan, S.L.; John, M.T.; Ahmad, M. Cone-beam computed tomography evaluation of maxillary sinusitis. J. Endod. 2011, 37, 753–757. [Google Scholar] [CrossRef]
- Nair, U.P.; Nair, M.K. Maxillary sinusitis of odontogenic origin: Cone-beam volumetric computerized tomography–aided diagnosis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 110, e53–e57. [Google Scholar] [CrossRef]
- Troeltzsch, M.; Pache, C.; Troeltzsch, M.; Kaeppler, G.; Ehrenfeld, M.; Otto, S.; Probst, F. Etiology and clinical characteristics of symptomatic unilateral maxillary sinusitis: A review of 174 cases. J. Cranio-Maxillofac. Surg. 2015, 43, 1522–1529. [Google Scholar] [CrossRef]
- Zahedi, C. Treatment of Orally Handicapped Edentulous Older Adults Using Dental Implants. Dent. Clin. N. Am. 2016, 60, 663–691. [Google Scholar] [CrossRef] [PubMed]
- da Mata, C.; Cronin, M.; O’Mahony, D.; McKenna, G.; Woods, N.; Allen, P.F. Subjective impact of minimally invasive dentistry in the oral health of older patients. Clin. Oral Investig. 2015, 19, 681–687. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.-D.; Chen, X.; Frencken, J.; Du, M.-Q.; Chen, Z. Dental caries and first permanent molar pit and fissure morphology in 7- to 8-year-old children in Wuhan, China. Int. J. Oral Sci. 2012, 4, 157–160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bozga, A.; Stanciu, R.P.; Mănuc, D. A study of prevalence and distribution of tooth agenesis. J. Med. Life 2014, 7, 551–554. [Google Scholar] [PubMed]

| 1PM a | 2PM b | 1M c | 2M d | Total | p Value | |
|---|---|---|---|---|---|---|
| Relationship to maxillary sinus | ||||||
| Up to 2 mm from the maxillary sinus cortex | 81 (17.647%) | 34 (7.407%) | 21 (4.575%) | 7 (1.525%) | 143 (31.154%) | <0.0001 |
| Within 2 mm to intimate contact with the maxillary sinus cortex | 63 (13.725%) | 83 (18.082%) | 68 (14.814%) | 31 (6.753%) | 245 (53.376%) | |
| Apical third inside the maxillary sinus | 11 (2.396%) | 19 (4.139%) | 20 (4.357%) | 16 (3.485%) | 66 (14.379%) | |
| Two-thirds or more inside the maxillary sinus | 0 | 1 (0.217%) | 2 (0.435%) | 2 (0.435%) | 5 (1.089%) | |
| Bone-fixation tissue | ||||||
| Alveolar ridge | 151 (32.897%) | 126 (27.450%) | 98 (21.350%) | 48 (10.457%) | 423 (92.156%) | 0.01 |
| Bone graft | 4 (0.871%) | 11 (2.396%) | 13 (2.832%) | 8 (1.742%) | 36 (7.843%) | |
| Maxillary sinus abnormalities | ||||||
| Normal MS | 91 (19.825%) | 82 (17.864%) | 60 (13.071%) | 28 (6.100%) | 261 (56.862%) | 0.708 |
| Mucosal thickening | 39 (8.496%) | 41 (8.932%) | 37 (8.061%) | 22 (4.793%) | 139 (30.283%) | |
| Antral pseudo cyst | 2 (0.435%) | 1 (0.217%) | 5 (1.089%) | 1 (0.217%) | 9 (1.960%) | |
| Non-specific opacification | 21 (4.575%) | 12 (2.614%) | 8 (1.742%) | 5 (1.089%) | 46 (10.021%) | |
| Antrolith | 2 (0.435%) | 1 (0.217%) | 1 (0.217%) | 0 | 4 (0.871%) |
| Relationship to Maxillary Sinus | Normal MS | Mucosal Thickening | Antral Pseudo Cyst | Non-Specific Opacification | Antrolith | p Valor |
|---|---|---|---|---|---|---|
| Up to 2 mm from the maxillary sinus cortex | 81 (17.647%) | 44 (9.586%) | 1 (0.217%) | 14 (3.050%) | 3 (0.653%) | 0.047 |
| Within 2 mm to intimate contact with the maxillary sinus cortex | 145 (31.590%) | 69 (15.032%) | 7 (1.525%) | 23 (5.010%) | 1 (0.217%) | |
| Apical third inside the maxillary sinus | 35 (7.625%) | 23 (5.010%) | 1 (0.217%) | 7 (1.525%) | 0 | |
| Two-thirds or more inside the maxillary sinus | 0 | 3 (0.653%) | 0 | 2 (0.435%) | 0 | |
| Bone fixation tissue | ||||||
| Alveolar ridge | 241 (52.505%) | 125 (27.233%) | 9 (1.960%) | 44 (9.586%) | 4 (0.871%) | 0.812 |
| Bone graft | 20 (4.357%) | 14 (3.050%) | 0 | 2 (0.435%) | 0 |
| Relationship to Maxillary Sinus | Alveolar Ridge | Bone Graft | Total | p Value |
|---|---|---|---|---|
| Up to 2 mm from the maxillary sinus cortex | 130 (28.32%) | 13 (2.832%) | 143 (31.152%) | 0.121 |
| Within 2 mm to intimate contact with the maxillary sinus cortex | 223 (48.583%) | 22 (4.793%) | 245 (53.376%) | |
| Apical third inside the maxillary sinus | 65 (14.161%) | 1 (0.217%) | 66 (14.378%) | |
| Two-thirds or more inside the maxillary sinus | 5 (1.089%) | 0 | 5 (1.089%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chaves, L.L.V.; Lopes Rosado, L.P.; Piccolo, S.M.; Ferreira, L.M.; Kamburoglu, K.; Junqueira, R.B.; Aquino de Castro, M.A.; Verner, F.S. Evaluation of the Maxillary Sinus of Patients with Maxillary Posterior Implants: A CBCT Cross-Sectional Study. Diagnostics 2022, 12, 3169. https://doi.org/10.3390/diagnostics12123169
Chaves LLV, Lopes Rosado LP, Piccolo SM, Ferreira LM, Kamburoglu K, Junqueira RB, Aquino de Castro MA, Verner FS. Evaluation of the Maxillary Sinus of Patients with Maxillary Posterior Implants: A CBCT Cross-Sectional Study. Diagnostics. 2022; 12(12):3169. https://doi.org/10.3390/diagnostics12123169
Chicago/Turabian StyleChaves, Lucas Lenyn Vieira, Lucas P. Lopes Rosado, Saulo Machado Piccolo, Liana Matos Ferreira, Kivanç Kamburoglu, Rafael Binato Junqueira, Maurício Augusto Aquino de Castro, and Francielle Silestre Verner. 2022. "Evaluation of the Maxillary Sinus of Patients with Maxillary Posterior Implants: A CBCT Cross-Sectional Study" Diagnostics 12, no. 12: 3169. https://doi.org/10.3390/diagnostics12123169
APA StyleChaves, L. L. V., Lopes Rosado, L. P., Piccolo, S. M., Ferreira, L. M., Kamburoglu, K., Junqueira, R. B., Aquino de Castro, M. A., & Verner, F. S. (2022). Evaluation of the Maxillary Sinus of Patients with Maxillary Posterior Implants: A CBCT Cross-Sectional Study. Diagnostics, 12(12), 3169. https://doi.org/10.3390/diagnostics12123169