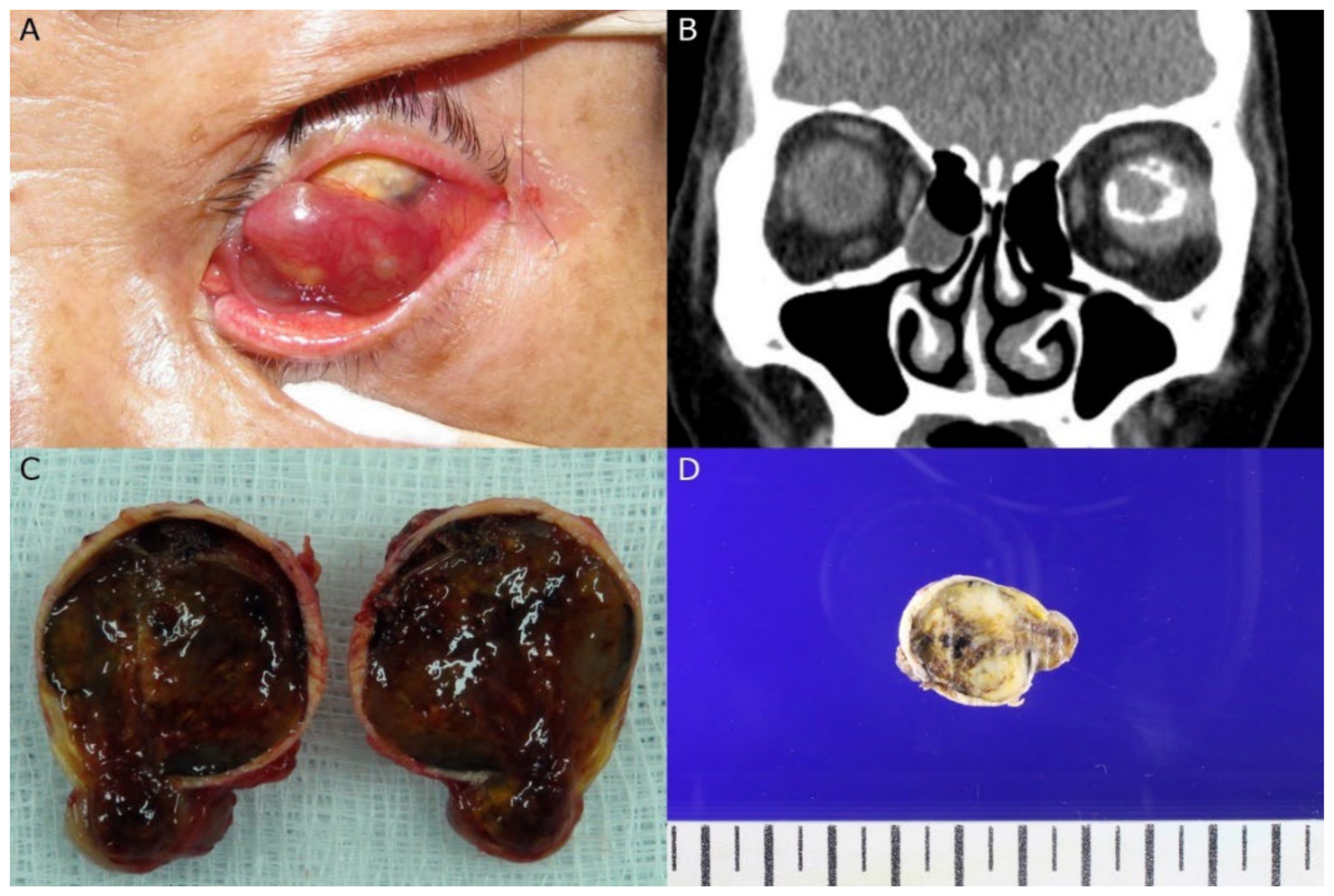
Massive Retinal Gliosis Mistaken as a Malignant Intraocular Tumor in Phthisis Bulbi
Abstract
:

Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Yanoff, M.; Zimmerman, L.E.; Davis, R.L. Massive gliosis of the retina. Int. Ophthalmol. Clin. 1971, 11, 211–229. [Google Scholar] [PubMed]
- Houston, S.K.; Bourne, T.D.; Lopes, M.B.; Ghazi, N.G. Bilateral massive retinal gliosis associated with retinopathy of prematurity. Arch. Pathol. Lab. Med. 2009, 133, 1242–1245. [Google Scholar] [CrossRef] [PubMed]
- Irvine, F.; O’Donnell, N.; Kemp, E.; Lee, W.R. Retinal vasoproliferative tumors: Surgical management and histological findings. Arch. Ophthalmol. 2000, 118, 563–569. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Essa, R.S.; Alkatan, H.M.; Arafah, M.A.; Al-Faky, Y.H. Massive Retinal Gliosis in an Infant Microphthalmic Globe: A Case Report. Am. J. Case Rep. 2021, 22, e929363. [Google Scholar] [CrossRef] [PubMed]
- Shields, J.A.; Shields, C.L. Glial tumors of the retina. The 2009 King Khaled Memorial Lecture. Saudi J. Ophthalmol. 2009, 23, 197–201. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Im, S.; Park, H.S.; Cho, U.; La, T.Y. Massive Retinal Gliosis Mistaken as a Malignant Intraocular Tumor in Phthisis Bulbi. Diagnostics 2022, 12, 3090. https://doi.org/10.3390/diagnostics12123090
Im S, Park HS, Cho U, La TY. Massive Retinal Gliosis Mistaken as a Malignant Intraocular Tumor in Phthisis Bulbi. Diagnostics. 2022; 12(12):3090. https://doi.org/10.3390/diagnostics12123090
Chicago/Turabian StyleIm, Soyoung, Hong Sik Park, Uiju Cho, and Tae Yoon La. 2022. "Massive Retinal Gliosis Mistaken as a Malignant Intraocular Tumor in Phthisis Bulbi" Diagnostics 12, no. 12: 3090. https://doi.org/10.3390/diagnostics12123090
APA StyleIm, S., Park, H. S., Cho, U., & La, T. Y. (2022). Massive Retinal Gliosis Mistaken as a Malignant Intraocular Tumor in Phthisis Bulbi. Diagnostics, 12(12), 3090. https://doi.org/10.3390/diagnostics12123090





