Advances in Imaging for Assessing Pelvic Endometriosis
Abstract
1. Introduction
2. Transvaginal Ultrasound
2.1. Ovarian Endometriosis
2.2. Superficial Endometriosis
2.3. Deep Endometriosis
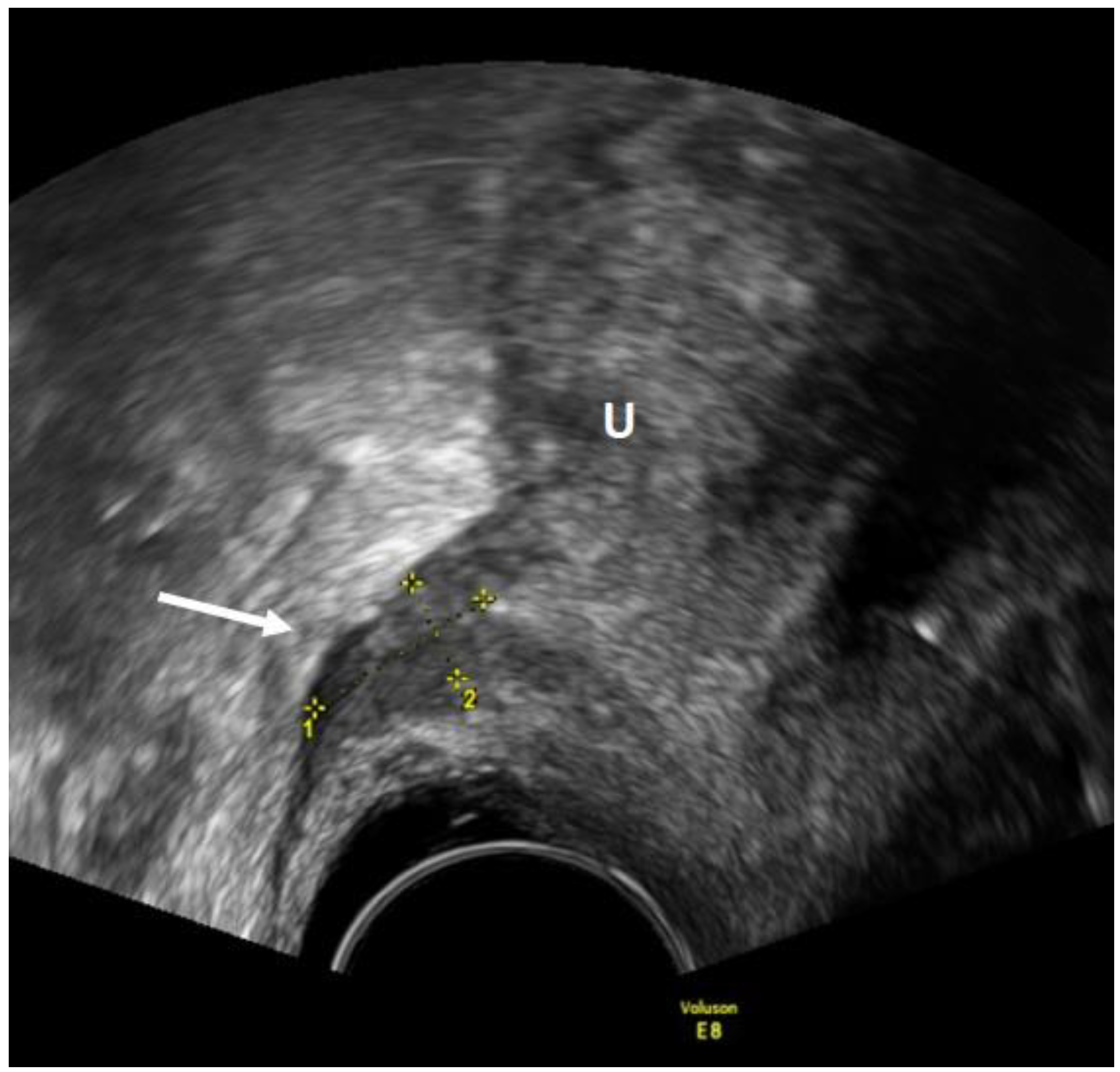
2.3.1. Anterior Endometriosis
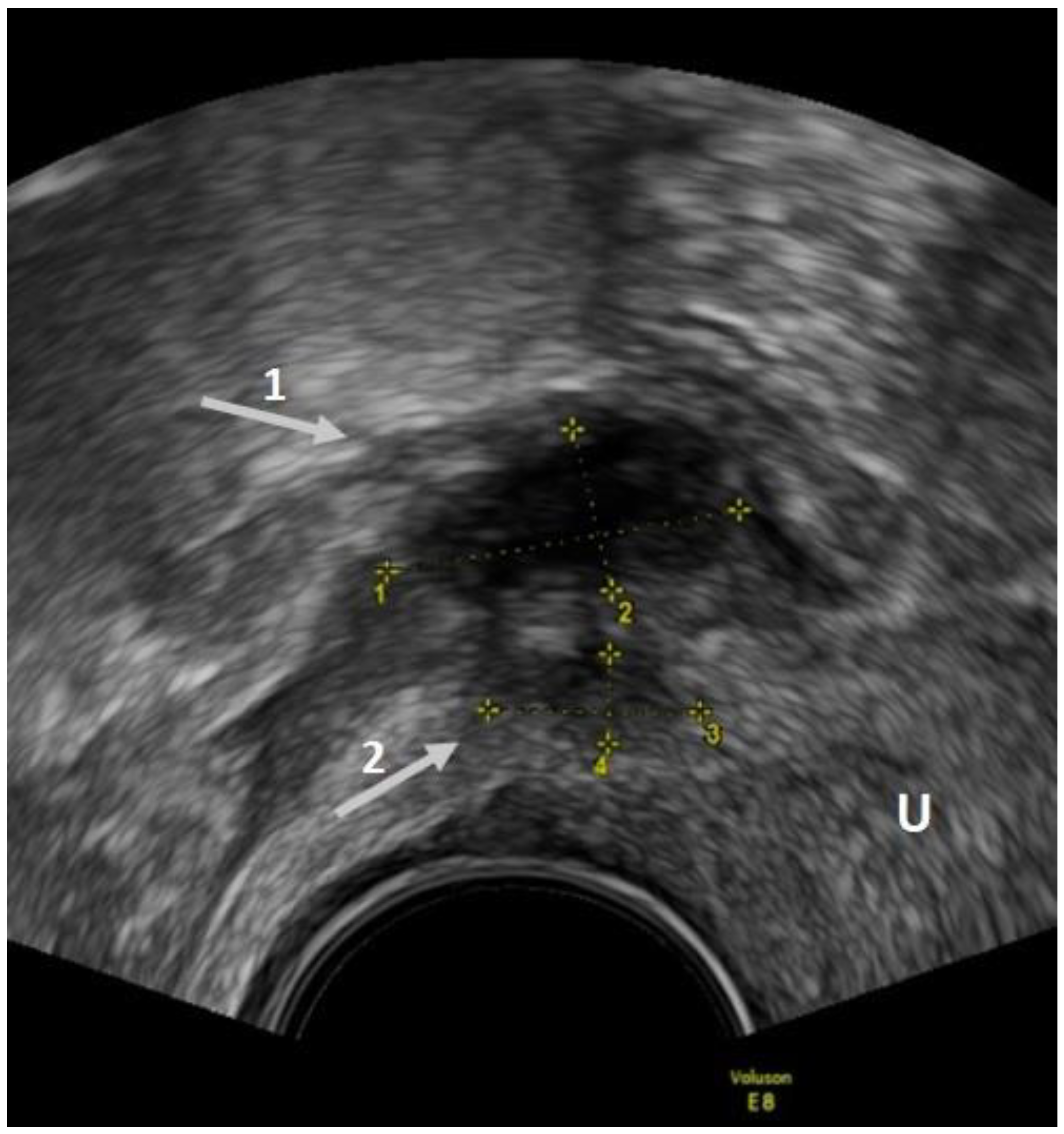
2.3.2. Posterior and Lateral Endometriosis
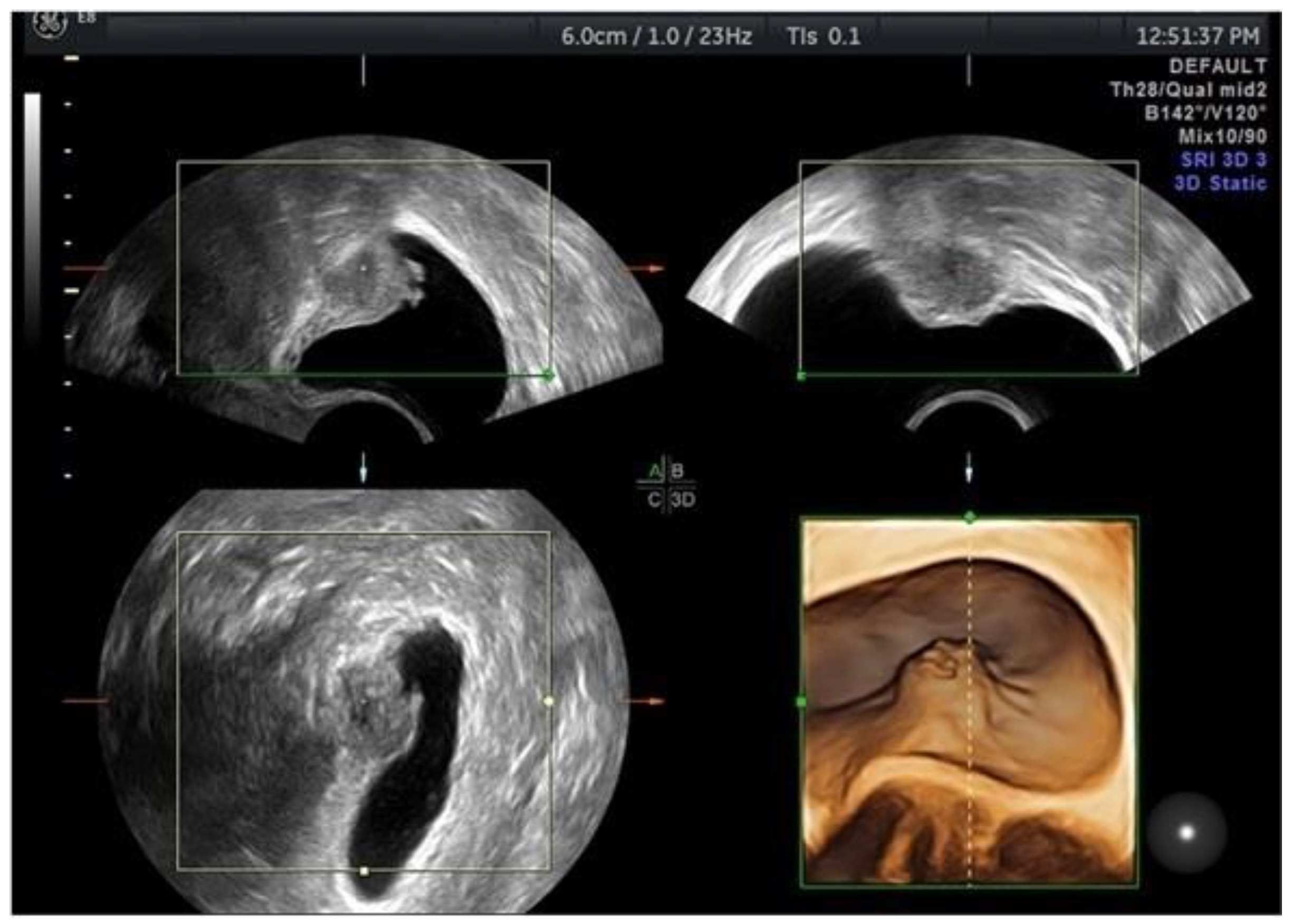
2.3.3. Additional Ultrasonographic Techniques and TVUS Classification Systems
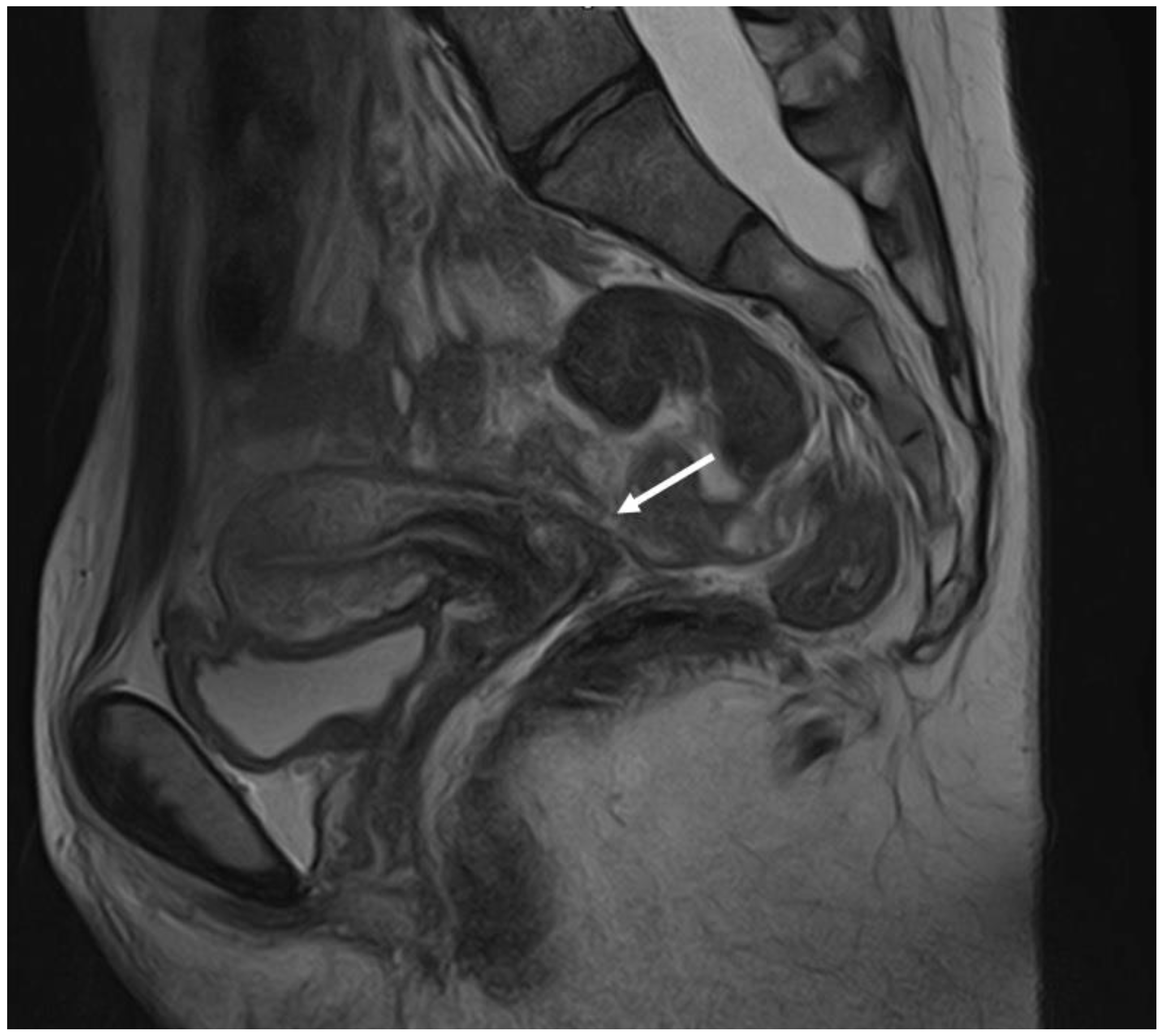
3. Magnetic Resonance Imaging (MRI)
3.1. Ovarian Endometriosis
3.2. Superficial Endometriosis
3.3. Deep Endometriosis
4. Other Imaging Techniques
Author Contributions
Funding
Conflicts of Interest
References
- Taylor, H.S.; Kotlyar, A.M.; A Flores, V. Endometriosis is a chronic systemic disease: Clinical challenges and novel innovations. Lancet 2021, 397, 839–852. [Google Scholar] [CrossRef] [PubMed]
- Tomassetti, C.; Johnson, N.P.; Petrozza, J. An International Terminology for Endometriosis, 2021. J. Minim. Invasive Gynecol. 2021, 28, 1849–1859. [Google Scholar] [CrossRef] [PubMed]
- Exacoustos, C.; De Felice, G.; Pizzo, A.; Morosetti, G.; Lazzeri, L.; Centini, G.; Piccione, E.; Zupi, E. Isolated Ovarian Endometrioma: A History Between Myth and Reality. J. Minim. Invasive Gynecol. 2018, 25, 884–891. [Google Scholar] [CrossRef] [PubMed]
- Menni, K.; Facchetti, L.; Cabassa, P. Extragenital endometriosis: Assessment with MR imaging. A pictorial review. Br. J. Radiol. 2016, 89, 20150672. [Google Scholar] [CrossRef] [PubMed]
- Andres, M.P.; Arcoverde, F.; Souza, C.C.; Fernandes, L.F.C.; Abrão, M.S.; Kho, R.M. Extrapelvic Endometriosis: A Systematic Review. J. Minim. Invasive Gynecol. 2019, 27, 373–389. [Google Scholar] [CrossRef]
- Guerriero, S.; Conway, F.; Pascual, M.A. Ultrasonography and Atypical Sites of Endometriosis. Diagnostics 2020, 10, 345. [Google Scholar] [CrossRef]
- Collins, B.G.; Ankola, A.; Gola, S.; McGillen, K.L. Transvaginal US of Endometriosis: Looking Beyond the Endometrioma with a Dedicated Protocol. RadioGraphics 2019, 39, 1549–1568. [Google Scholar] [CrossRef]
- Guerriero, S.; Van Calster, B.; Somigliana, E.; Ajossa, S.; Froyman, W.; De Cock, B.; Coosemans, A.; Fischerová, D.; Van Holsbeke, C.; Alcazar, J.L.; et al. Age-related differences in the sonographic characteristics of endometriomas. Hum. Reprod. 2016, 31, 1723–1731. [Google Scholar] [CrossRef]
- Van Holsbeke, C.; Van Calster, B.; Guerriero, S. Endometriomas: Their ultrasound characteristics. Ultrasound Obstet. Gynecol. 2010, 35, 730–740. [Google Scholar] [CrossRef]
- Nisenblat, V.; Bossuyt, P.M.M.; Farquhar, C.; Johnson, N.; Hull, M.L. Imaging modalities for the non-invasive diagnosis of endome-triosis. Cochrane Database Syst. Rev. 2016, 2016, CD009591. [Google Scholar]
- Chowdary, P.; Stone, K.; Ma, T. Multicentre retrospective study to assess diagnostic accuracy of ultrasound for superficial endometriosis—Are we any closer? Aust. N. Z. J. Obstet. Gynaecol. 2019, 59, 279–284. [Google Scholar] [CrossRef]
- Robinson, A.J.; Rombauts, L.; Ades, A.; Leong, K.; Paul, E.; Piessens, S. Poor sensitivity of transvaginal ultrasound markers in diagnosis of superficial endometriosis of the uterosacral ligaments. J. Endometr. Pelvic Pain Disord. 2018, 10, 10–17. [Google Scholar] [CrossRef]
- Reid, S.; Leonardi, M.; Lu, C.; Condous, G. The association between ultrasound-based ‘soft markers’ and endometriosis type/location: A prospective observational study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 234, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Leonardi, M.; Robledo, K.; Espada, M.; Vanza, K.; Condous, G. SonoPODography: A new diagnostic technique for visualizing superficial endometriosis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 254, 124–131. [Google Scholar] [CrossRef] [PubMed]
- Guerriero, S.; Condous, G.; van den Bosch, T.; Valentin, L.; Leone, F.P.G.; Van Schoubroeck, D.; Exacoustos, C.; Installé, A.J.F.; Martins, W.P.; Abrao, M.S.; et al. Systematic approach to sonographic evaluation of the pelvis in women with suspected endometriosis, including terms, definitions and measurements: A consensus opinion from the International Deep Endometriosis Analysis (IDEA) group. Ultrasound Obstet. Gynecol. 2016, 48, 318–332. [Google Scholar] [CrossRef] [PubMed]
- Guerriero, S.; Ajossa, S.; Pascual, M.A.; Rodriguez, I.; Piras, A.; Perniciano, M.; Saba, L.; Paoletti, A.M.; Mais, V.; Alcazar, J.L. Ultrasonographic soft markers for detection of rectosigmoid deep endometriosis. Ultrasound Obstet. Gynecol. 2019, 55, 269–273. [Google Scholar] [CrossRef]
- Alcázar, J.L.; Eguez, P.M.; Forcada, P.; Ternero, E.; Martínez, C.; Pascual, M.; Guerriero, S. Diagnostic accuracy of sliding sign for detecting pouch of Douglas obliteration and bowel involvement in women with suspected endometriosis: Systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 2022, 60, 477–486. [Google Scholar] [CrossRef]
- Stepniewska, A.K.; Clarizia, R.; De Mitri, P. Role of ultrasonographic parameters for predicting tubal involvement in infertile patients affected by endometriosis: A ret-rospective cohort study. J. Gynecol. Obstet. Hum. Reprod. 2021, 50, 102208. [Google Scholar] [CrossRef]
- Keckstein, J.; Saridogan, E.; Ulrich, U.A.; Sillem, M.; Oppelt, P.; Schweppe, K.W.; Krentel, H.; Janschek, E.; Exacoustos, C.; Malzoni, M.; et al. The #Enzian classification: A comprehensive non-invasive and surgical description system for endometriosis. Acta Obstet. Gynecol. Scand. 2021, 100, 1165–1175. [Google Scholar] [CrossRef]
- Mariani, L.L.; Mancarella, M.; Novara, L.; Biglia, N. Sonographic features of endometriosis infiltrating the lateral parametrium. J. Gynecol. Obstet. Hum. Reprod. 2021, 50, 102116. [Google Scholar] [CrossRef]
- Bazot, M.; Delaveau, M.-C.; Daraï, E.; Bendifallah, S. Value of sonography in assessing parametrial endometriotic involvement: Preliminary results. J. Endometr. Pelvic Pain Disord. 2021, 13, 58–65. [Google Scholar] [CrossRef]
- Taksøe-Vester, C.; Dreisler, E.; Andreasen, L.A.; Dyre, L.; Ringsted, C.; Tabor, A.; Tolsgaard, M.G. Up or down? A randomized trial comparing image orientations during transvaginal ultrasound training. Acta Obstet. Gynecol. Scand. 2018, 97, 1455–1462. [Google Scholar] [CrossRef] [PubMed]
- Guerriero, S.; Ajossa, S.; Minguez, J.A.; Jurado, M.; Mais, V.; Melis, G.B.; Alcazar, J.L. Accuracy of transvaginal ultrasound for diagnosis of deep endometriosis in uterosacral ligaments, rectovaginal septum, vagina and bladder: Systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 2015, 46, 534–545. [Google Scholar] [CrossRef] [PubMed]
- Gerges, B.; Li, W.; Leonardi, M.; Mol, B.; Condous, G. Meta-analysis and systematic review to determine the optimal imaging modality for the detection of bladder deep endometriosis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021, 261, 124–133. [Google Scholar] [CrossRef]
- Carfagna, P.; De Cicco Nardone, C.; De Cicco Nardone, A. Role of transvaginal ultrasound in evaluation of ureteral in-volvement in deep infiltrating endometriosis. Ultrasound Obstet. Gynecol. 2018, 51, 550–555. [Google Scholar] [CrossRef]
- Pateman, K.; Holland, T.K.; Knez, J. Should a detailed ultrasound examination of the complete urinary tract be routinely performed in women with suspected pelvic endometriosis? Hum. Reprod. 2015, 30, 2802–2807. [Google Scholar] [CrossRef]
- Chamié, L.P. Ultrasound evaluation of deeply infiltrative endometriosis: Technique and interpretation. Abdom. Radiol. 2019, 45, 1648–1658. [Google Scholar] [CrossRef]
- Guerriero, S.; Ajossa, S.; Orozco, R. Accuracy of transvaginal ultrasound for diagnosis of deep endometriosis in the rec-tosigmoid: Systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 2016, 47, 281–289. [Google Scholar] [CrossRef]
- Aas-Eng, M.K.; Lieng, M.; Dauser, B.; Diep, L.M.; Leonardi, M.; Condous, G.; Hudelist, G. Transvaginal sonography determines accurately extent of infiltration of rectosigmoid deep endometriosis. Ultrasound Obstet. Gynecol. 2021, 58, 933–939. [Google Scholar] [CrossRef]
- Aas-Eng, M.K.; Dauser, B.; Lieng, M.; Diep, L.M.; Leonardi, M.; Condous, G.; Hudelist, G. Transvaginal sonography accurately measures lesion-to-anal-verge distance in women with deep endometriosis of the rectosigmoid. Ultrasound Obstet. Gynecol. 2020, 56, 766–772. [Google Scholar] [CrossRef]
- Di Giovanni, A.; Casarella, L.; Coppola, M.; Iuzzolino, D.; Rasile, M.; Malzoni, M. Combined Transvaginal/Transabdominal Pelvic Ultrasonography Accurately Predicts the 3 Dimensions of Deep Infiltrating Bowel Endometriosis Measured after Surgery: A Prospective Study in a Specialized Center. J. Minim. Invasive Gynecol. 2018, 25, 1231–1240. [Google Scholar] [CrossRef] [PubMed]
- Leonardi, M.; Uzuner, C.; Mestdagh, W.; Lu, C.; Guerriero, S.; Zajicek, M.; Dueckelmann, A.; Filippi, F.; Buonomo, F.; Pascual, M.A.; et al. Diagnostic accuracy of transvaginal ultrasound for detection of endometriosis using International Deep Endometriosis Analysis (IDEA) approach: Prospective international pilot study. Ultrasound Obstet. Gynecol. 2022, 60, 404–413. [Google Scholar] [CrossRef] [PubMed]
- Exacoustos, C.; Manganaro, L.; Zupi, E. Imaging for the evaluation of endometriosis and adenomyosis. Best Pr. Res. Clin. Obstet. Gynaecol. 2014, 28, 655–681. [Google Scholar] [CrossRef] [PubMed]
- Mabrouk, M.; Raimondo, D.; Arena, A.; Iodice, R.; Altieri, M.; Sutherland, N.; Salucci, P.; Moro, E.; Seracchioli, R. Parametrial Endometriosis: The Occult Condition that Makes the Hard Harder. J. Minim. Invasive Gynecol. 2018, 26, 871–876. [Google Scholar] [CrossRef]
- Chiantera, V.; Petrillo, M.; Abesadze, E.; Sozzi, G.; Dessole, M.; Di Donna, M.C.; Scambia, G.; Sehouli, J.; Mechsner, S. Laparoscopic Neuronavigation for Deep Lateral Pelvic Endometriosis: Clinical and Surgical Implications. J. Minim. Invasive Gynecol. 2018, 25, 1217–1223. [Google Scholar] [CrossRef]
- Guerriero, S.; Martinez, L.; Gomez, I.; Pascual, M.A.; Ajossa, S.; Pagliuca, M.; Alcázar, J.L. Diagnostic accuracy of transvaginal sonography for detecting parametrial involvement in women with deep endometriosis: Systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 2021, 58, 669–676. [Google Scholar] [CrossRef]
- Leonardi, M.; Martins, W.P.; Espada, M.; Arianayagam, M.; Condous, G. Proposed technique to visualize and classify uterosacral ligament deep endometriosis with and without infiltration into parametrium or torus uterinus. Ultrasound Obstet. Gynecol. 2019, 55, 137–139. [Google Scholar] [CrossRef]
- Guerriero, S.; Ajossa, S.; Gerada, M.; D’Aquila, M.; Piras, B.; Melis, G.B. “Tenderness-guided” transvaginal ultrasonography: A new method for the detection of deep endometriosis in patients with chronic pelvic pain. Fertil. Steril. 2007, 88, 1293–1297. [Google Scholar] [CrossRef]
- Guerriero, S.; Ajossa, S.; Gerada, M.; Virgilio, B.; Angioni, S.; Melis, G.B. Diagnostic value of transvaginal “tenderness-guided” ul-trasonography for the prediction of location of deep endometriosis. Hum. Reprod. 2008, 23, 2452–2457. [Google Scholar] [CrossRef]
- Hudelist, G.; Ballard, K.; English, J.; Wright, J.; Banerjee, S.; Mastoroudes, H.; Thomas, A.; Singer, C.F.; Keckstein, J. Transvaginal sonography vs. clinical examination in the preoperative diagnosis of deep infiltrating endometriosis. Ultrasound Obstet. Gynecol. 2011, 37, 480–487. [Google Scholar] [CrossRef]
- Ros, C.; Rius, M.; Abrao, M.S.; Deguirior, C.; Martínez-Zamora, M.; Gracia, M.; Carmona, F. Bowel preparation prior to transvaginal ultrasound improves detection of rectosigmoid deep infiltrating endometriosis and is well tolerated: Prospective study of women with suspected endometriosis without surgical criteria. Ultrasound Obstet. Gynecol. 2020, 57, 335–341. [Google Scholar] [CrossRef] [PubMed]
- Ferrero, S.; Scala, C.; Stabilini, C.; Vellone, V.G.; Barra, F.; Maggiore, U.L.R. Transvaginal sonography with vs without bowel preparation in diagnosis of rectosigmoid endometriosis: Prospective study. Ultrasound Obstet. Gynecol. 2019, 53, 402–409. [Google Scholar] [CrossRef]
- Reid, S.; Lu, C.; Hardy, N.; Casikar, I.; Reid, G.; Cario, G.; Chou, D.; Almashat, D.; Condous, G. Office gel sonovaginography for the prediction of posterior deep infiltrating endometriosis: A multicenter prospective observational study. Ultrasound Obstet. Gynecol. 2014, 44, 710–718. [Google Scholar] [CrossRef] [PubMed]
- Reid, S.; Winder, S.; Condous, G. Sonovaginography: Redefining the concept of a “normal pelvis” on transvaginal ultrasound pre-laparoscopic intervention for suspected endometriosis. Australas. J. Ultrasound Med. 2011, 14, 21–24. [Google Scholar] [CrossRef] [PubMed]
- Barra, F.; Maggiore, U.L.R.; Evangelisti, G.; Scala, C.; Alessandri, F.; Vellone, V.G.; Stabilini, C.; Ferrero, S. A prospective study comparing rectal water contrast-transvaginal ultrasonography with sonovaginography for the diagnosis of deep posterior endometriosis. Acta Obstet. et Gynecol. Scand. 2021, 100, 1700–1711. [Google Scholar] [CrossRef]
- Puppo, A.; Olearo, E.; Gattolin, A.; Rimonda, R.; Novelli, A.; Ceccaroni, M. Intraoperative Ultrasound for Bowel Deep Infiltrating Endometriosis: A Preliminary Report. J. Ultrasound Med. 2021, 40, 1417–1425. [Google Scholar] [CrossRef] [PubMed]
- Tomassetti, C.; Bafort, C.; Vanhie, A.; Meuleman, C.; Fieuws, S.; Welkenhuysen, M.; Timmerman, D.; Van Schoubroeck, D.; D’Hooghe, T. Estimation of the Endometriosis Fertility Index prior to operative laparoscopy. Hum. Reprod. 2020, 36, 636–646. [Google Scholar] [CrossRef] [PubMed]
- Ichikawa, M.; Akira, S.; Kaseki, H.; Watanabe, K.; Ono, S.; Takeshita, T. Accuracy and clinical value of an adhesion scoring system: A preoperative diagnostic method using transvaginal ultrasonography for endometriotic adhesion. J. Obstet. Gynaecol. Res. 2020, 46, 466–478. [Google Scholar] [CrossRef] [PubMed]
- Chattot, C.; Huchon, C.; Paternostre, A.; Du Cheyron, J.; Chouillard, E.; Fauconnier, A. Endorect: A preoperative score to accu-rately predict rectosigmoid involvement in patients with endometriosis. Hum. Reprod. Open 2019, 2019, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Menakaya, U.; Reid, S.; Lü, C.; Bassem, G.; Infante, F.; Condous, G. Performance of ultrasound-based endometriosis staging system (UBESS) for predicting level of complexity of laparoscopic surgery for endometriosis. Ultrasound Obstet. Gynecol. 2016, 48, 786–795. [Google Scholar] [CrossRef]
- Tompsett, J.; Leonardi, M.; Gerges, B. Ultrasound-Based Endometriosis Staging System: Validation Study to Predict Com-plexity of Laparoscopic Surgery. J. Minim. Invasive Gynecol. 2019, 26, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Espada, M.; Leonardi, M.; Aas-Eng, K. A Multicenter International Temporal and External Validation Study of the Ultra-sound-based Endometriosis Staging System. J. Minim. Invasive Gynecol. 2021, 28, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Young, S.W.; Groszmann, Y.; Dahiya, N.; Caserta, M.; Yi, J.; Wasson, M.; Patel, M.D. Sonographer-acquired ultrasound protocol for deep endometriosis. Abdom. Radiol. 2019, 45, 1659–1669. [Google Scholar] [CrossRef] [PubMed]
- Deslandes, A.; Parange, N.; Childs, J.T. How long does a transvaginal ultrasound examination for endometriosis take in comparison to a routine transvaginal ultrasound examination? Australas J. Ultrasound Med. 2022, 25, 20–27. [Google Scholar] [CrossRef]
- Downey, D.B.; Fenster, A.; Williams, J.C. Clinical Utility of Three-dimensional US. RadioGraphics 2000, 20, 559–571. [Google Scholar] [CrossRef]
- Raine-Fenning, N.; Jayaprakasan, K.; Deb, S. Three-dimensional ultrasonographic characteristics of endometriomata. Ultrasound Obstet. Gynecol. 2008, 31, 718–724. [Google Scholar] [CrossRef]
- Guerriero, S.; Alcázar, J.L.; Ajossa, S.; Pilloni, M.; Melis, G.B. Three-Dimensional Sonographic Characteristics of Deep Endometriosis. J. Ultrasound Med. 2009, 28, 1061–1066. [Google Scholar] [CrossRef]
- Barra, F.; Alessandri, F.; Scala, C.; Ferrero, S. Ultrasonographic 3D Evaluation in the Diagnosis of Bladder Endometriosis: A Pro-spective Comparative Diagnostic Accuracy Study. Gynecol. Obstet. Investig. 2021, 86, 299–306. [Google Scholar] [CrossRef]
- Guerriero, S.; Saba, L.; Ajossa, S.; Peddes, C.; Angiolucci, M.; Perniciano, M.; Melis, G.B.; Alcázar, J.L. Three-dimensional ultrasonography in the diagnosis of deep endometriosis. Hum. Reprod. 2014, 29, 1189–1198. [Google Scholar] [CrossRef]
- Guerriero, S.; Pilloni, M.; Alcazar, J.L. Tissue characterization using mean gray value analysis in deep infiltrating endome-triosis. Ultrasound Obstet Gynecol. 2013, 41, 459–464. [Google Scholar] [CrossRef]
- Pascual, M.A.; Guerriero, S.; Hereter, L.; Barri-Soldevila, P.; Ajossa, S.; Graupera, B.; Rodriguez, I. Diagnosis of endometriosis of the rectovaginal septum using introital three-dimensional ultrasonography. Fertil. Steril. 2010, 94, 2761–2765. [Google Scholar] [CrossRef] [PubMed]
- Guerriero, S.; Pascual, M.A.; Ajossa, S. The reproducibility of ultrasonographic findings of rectosigmoid endometriosis among examiners with different level of expertise. J. Ultrasound Med. 2022, 41, 403–408. [Google Scholar] [CrossRef] [PubMed]
- Bazot, M.; Bharwani, N.; Huchon, C.; Kinkel, K.; Cunha, T.M.; Guerra, A.; Manganaro, L.; Buñesch, L.; Kido, A.; Togashi, K.; et al. European society of urogenital radiology (ESUR) guidelines: MR imaging of pelvic endometriosis. Eur. Radiol. 2016, 27, 2765–2775. [Google Scholar] [CrossRef] [PubMed]
- Jha, P.; Sakala, M.; Chamie, L.P.; Feldman, M.; Hindman, N.; Huang, C.; Kilcoyne, A.; Laifer-Narin, S.; Nicola, R.; Poder, L.; et al. Endometriosis MRI lexicon: Consensus statement from the society of abdominal radiology endometriosis disease-focused panel. Abdom. Imaging 2019, 45, 1552–1568. [Google Scholar] [CrossRef]
- Coutinho, A.; Bittencourt, L.K.; Pires, C.E.; Junqueira, F.; Lima, C.M.A.D.O.; Coutinho, E.; Domingues, M.A.; Domingues, R.C.; Marchiori, E. MR Imaging in Deep Pelvic Endometriosis: A Pictorial Essay. Radiographics 2011, 31, 549–567. [Google Scholar] [CrossRef] [PubMed]
- Lorusso, F.; Scioscia, M.; Rubini, D.; Ianora, A.A.S.; Scardigno, D.; Leuci, C.; De Ceglie, M.; Sardaro, A.; Lucarelli, N.; Scardapane, A. Magnetic resonance imaging for deep infiltrating endometriosis: Current concepts, imaging technique and key findings. Insights Imaging 2021, 12, 1–12. [Google Scholar] [CrossRef]
- Bazot, M.; Gasner, A.; Ballester, M.; Daraï, E. Value of thin-section oblique axial T2-weighted magnetic resonance images to assess uterosacral ligament endometriosis. Hum. Reprod. 2010, 26, 346–353. [Google Scholar] [CrossRef]
- Suzuki, S.; Yasumoto, M.; Matsumoto, R.; Andoh, A. MR findings of ruptured endometrial cyst: Comparison with tubo-ovarian abscess. Eur. J. Radiol. 2012, 81, 3631–3637. [Google Scholar] [CrossRef]
- Corwin, M.T.; Gerscovich, E.O.; Lamba, R.; Wilson, M.; McGahan, J.P. Differentiation of Ovarian Endometriomas from Hemorrhagic Cysts at MR Imaging: Utility of the T2 Dark Spot Sign. Radiology 2014, 271, 126–132. [Google Scholar] [CrossRef]
- Foti, P.V.; Farina, R.; Palmucci, S.; Vizzini, I.A.A.; Libertini, N.; Coronella, M.; Spadola, S.; Caltabiano, R.; Iraci, M.; Basile, A.; et al. Endometriosis: Clinical features, MR imaging findings and pathologic correlation. Insights Imaging 2018, 9, 149–172. [Google Scholar] [CrossRef]
- Del Frate, G.; Bazzocchi, M.; Zuiani, C. Pelvic Endometriosis: MR Imaging Appearance with Laparoscopic correlation. Radiographics 2006, 9, 1705–1719. [Google Scholar] [CrossRef] [PubMed]
- Krüger, K.; Gilly, L.; Niedobitek-Kreuter, G.; Mpinou, L.; Ebert, A.D. Bladder endometriosis: Characterization by magnetic resonance imaging and the value of documenting ureteral involvement. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014, 176, 39–43. [Google Scholar] [CrossRef] [PubMed]
- Maccagnano, C.; Pellucchi, F.; Rocchini, L.; Ghezzi, M.; Scattoni, V.; Montorsi, F.; Rigatti, P.; Colombo, R. Diagnosis and Treatment of Bladder Endometriosis: State of the Art. Urol. Int. 2012, 89, 249–258. [Google Scholar] [CrossRef] [PubMed]
- Gui, B.; Valentini, A.L.; Ninivaggi, V. Shining light in a dark landscape: MRI evaluation of unusual localization of endome-triosis. Diagn. Interv. Radiol. 2017, 23, 272–281. [Google Scholar] [CrossRef]
- Sillou, S.; Poirée, S.; Millischer, A.; Chapron, C.; Hélénon, O. Urinary endometriosis: MR Imaging appearance with surgical and histological correlations. Diagn. Interv. Imaging 2015, 96, 373–381. [Google Scholar] [CrossRef]
- Medeiros, L.R.; Rosa, M.I.; Silva, B.R.; Reis, M.E.; Simon, C.S.; Dondossola, E.R.; Filho, J.S.D.C. Accuracy of magnetic resonance in deeply infiltrating endometriosis: A systematic review and meta-analysis. Arch. Gynecol. Obstet. 2014, 291, 611–621. [Google Scholar] [CrossRef]
- Bazot, M.; Darai, E.; Hourani, R.; Thomassin, I.; Cortez, A.; Uzan, S.; Buy, J.-N. Deep Pelvic Endometriosis: MR Imaging for Diagnosis and Prediction of Extension of Disease. Radiology 2004, 232, 379–389. [Google Scholar] [CrossRef]
- Kinkel, K.; Frei, K.A.; Balleyguier, C.; Chapron, C. Diagnosis of endometriosis with imaging: A review. Eur. Radiol. 2005, 16, 285–298. [Google Scholar] [CrossRef]
- Pereira, R.M.A.; Zanatta, A.; Serafini, P.C.; Redwine, D. The feasibility of laparoscopic bowel resection performed by a gynaecologist to treat endometriosis. Curr. Opin. Obstet. Gynecol. 2010, 22, 344–353. [Google Scholar] [CrossRef]
- Abrao, M.S.; Gonçalves, M.O.D.C.; Dias, J.A.; Podgaec, S.; Chamie, L.P.; Blasbalg, R. Comparison between clinical examination, trans-vaginal sonography and magnetic resonance imaging for the diagnosis of deep endometriosis. Hum. Reprod. 2007, 22, 3092–3097. [Google Scholar] [CrossRef]
- Saba, L.; Guerriero, S.; Sulcis, R. MRI and “tenderness Guided” transvaginal ultrasonography in the diagnosis of rec-to-sigmoid endometriosis. J. Magn. Reson. Imaging. 2012, 35, 352–360. [Google Scholar] [CrossRef] [PubMed]
- Crispi, C.P.; Salomão, A.C.C.B.; Belem, L.C.; Crispi, F.D.P.; Fonseca, M.D.F. Lateral Compartment Endometriosis is Associated with Retraction of the Obliterated Umbilical Artery. JSLS J. Soc. Laparoendosc. Surg. 2021, 25, e2021.00038. [Google Scholar] [CrossRef] [PubMed]
- Guerriero, S.; Saba, L.; Pascual, M.A.; Ajossa, S.; Rodriguez, I.; Mais, V.; Alcazar, J.L. Transvaginal ultrasound vs magnetic resonance imaging for diagnosing deep infiltrating endometriosis: Systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 2018, 51, 586–595. [Google Scholar] [CrossRef] [PubMed]
- Gerges, B.; Li, W.; Leonardi, M.; Mol, B.W.; Condous, G. Optimal imaging modality for detection of rectosigmoid deep endometriosis: Systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 2020, 58, 190–200. [Google Scholar] [CrossRef] [PubMed]
- Gerges, B.; Li, W.; Leonardi, M.; Mol, B.W.; Condous, G. Meta-analysis and systematic review to determine the optimal imaging modality for the detection of uterosacral ligaments/torus uterinus, rectovaginal septum and vaginal deep endometriosis. Hum. Reprod. Open 2021, 2021, hoab041. [Google Scholar] [CrossRef] [PubMed]
- Bazot, M.; Spagnioli, F.; Guerriero, S. Magnetic resonance imaging and ultrasound fusion technique in gynecology. Ultrasound Obstet. Gynecol. 2021, 59, 141–145. [Google Scholar] [CrossRef]
- Millischer, A.-E.; Salomon, L.J.; Santulli, P.; Borghese, B.; Dousset, B.; Chapron, C. Fusion imaging for evaluation of deep infiltrating endometriosis: Feasibility and preliminary results. Ultrasound Obstet. Gynecol. 2014, 46, 109–117. [Google Scholar] [CrossRef]
- Berger, J.; Henneman, O.; Rhemrev, J.; Smeets, M.; Jansen, F.W. MRI-Ultrasound Fusion Imaging for Diagnosis of Deep Infiltrating Endometriosis—A Critical Appraisal. Ultrasound Int. Open. 2018, 4, E85–E90. [Google Scholar] [CrossRef]
- Gordon, R.L.; Evers, K.; Laufer, I.; Herlinger, H.; Thompson, J.J. Double-Contrast Enema Pelvic Endometriosis in through. AJR Am. J. Roentgenol. 1982, 138, 549–552. [Google Scholar] [CrossRef]
- Jiang, J.; Liu, Y.; Wang, K.; Wu, X.; Tang, Y. Rectal water contrast transvaginal ultrasound versus double-contrast barium enema in the diagnosis of bowel endometriosis. BMJ Open 2017, 7, e017216. [Google Scholar] [CrossRef]
- Savelli, L.; Manuzzi, L.; Coe, M.; Mabrouk, M.; Di Donato, N.; Venturoli, S.; Seracchioli, R. Comparison of transvaginal sonography and double-contrast barium enema for diagnosing deep infiltrating endometriosis of the posterior compartment. Ultrasound Obstet. Gynecol. 2011, 38, 466–471. [Google Scholar] [CrossRef] [PubMed]
- Faccioli, N.; Manfredi, R.; Mainardi, P.; Chiara, E.D.; Spoto, E.; Minelli, L.; Mucelli, R.P. Barium Enema Evaluation of Colonic Involvement in Endometriosis. Am. J. Roentgenol. 2008, 190, 1050–1054. [Google Scholar] [CrossRef]
- Ribeiro, H.S.A.A.; Ribeiro, P.A.; Rossini, L.; Rodrigues, F.C.; Donadio, N.; Aoki, T. Double-Contrast Barium Enema and Transrectal Endoscopic Ultrasonography in the Diagnosis of Intestinal Deeply Infiltrating Endometriosis. J. Minim. Invasive Gynecol. 2008, 15, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Faccioli, N.; Foti, G.; Manfredi, R.; Mainardi, P.; Spoto, E.; Ruffo, G.; Minelli, L.; Mucelli, R.P. Evaluation of colonic involvement in endometriosis: Double-contrast barium enema vs. magnetic resonance imaging. Gastrointest. Radiol. 2009, 35, 414–421. [Google Scholar] [CrossRef] [PubMed]
- Landi, S.; Barbieri, F.; Fiaccavento, A.; Mainardi, P.; Ruffo, G.; Selvaggi, L.; Syed, R.; Minelli, L. Preoperative Double-Contrast Barium Enema in Patients with Suspected Intestinal Endometriosis. J. Am. Assoc. Gynecol. Laparoscopists 2004, 11, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Chapron, C.; Vieira, M.; Chopin, N.; Balleyguier, C.; Barakat, H.; Dumontier, I.; Roseau, G.; Fauconnier, A.; Foulot, H.; Dousset, B. Accuracy of rectal endoscopic ultrasonography and magnetic resonance imaging in the diagnosis of rectal involvement for patients presenting with deeply infiltrating endometriosis. Ultrasound Obstet. Gynecol. 2004, 24, 175–179. [Google Scholar] [CrossRef]
- Gedgaudas, R.K.; Kelvin, F.M.; Thompson, W.M.; Rice, R.P. The value of the preoperative barium-enema examination in the as-sessment of pelvic masses. Radiology 1983, 146, 609–613. [Google Scholar] [CrossRef]
- Glaser, F.; Schlag, P.; Herfarth, C. Endorectal ultrasonography for the assessment of invasion of rectal tumours and lymph node involvement. Br. J. Surg. 1990, 77, 883–887. [Google Scholar] [CrossRef]
- Bahr, A.; De Parades, V.; Gadonneix, P.; Etienney, I.; Salet-Lizée, D.; Villet, R.; Atienza, P. Endorectal Ultrasonography in Predicting Rectal Wall Infiltration in Patients With Deep Pelvic Endometriosis: A Modern Tool for an Ancient Disease. Dis. Colon Rectum 2006, 49, 869–875. [Google Scholar] [CrossRef]
- Abrão, M.S.; Neme, R.M.; Averbach, M.; Petta, C.A.; Aldrighi, J.M. Rectal Endoscopic Ultrasound with a Rectovaginal Endometriosis. Obstet. Gynecol. 2004, 11, 50–54. [Google Scholar]
- Bazot, M.; Malzy, P.; Cortez, A.; Roseau, G.; Amouyal, P.; Daraï, E. Accuracy of transvaginal sonography and rectal endoscopic sonography in the diagnosis of deep infiltrating endometriosis. Ultrasound Obstet. Gynecol. 2007, 30, 994–1001. [Google Scholar] [CrossRef]
- Bazot, M.; Bornier, C.; Dubernard, G.; Roseau, G.; Cortez, A.; Daraï, E. Accuracy of magnetic resonance imaging and rectal endoscopic sonography for the prediction of location of deep pelvic endometriosis. Hum. Reprod. 2007, 22, 1457–1463. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chapron, C.; Dumontier, I.; Dousset, B.; Fritel, X.; Tardif, D.; Roseau, G.; Chaussade, S.; Couturier, D.; Dubuisson, J.B. Results and role of rectal endoscopic ultrasonography for patients with deep pelvic endometriosis. Hum. Reprod. 1998, 13, 2266–2270. [Google Scholar] [CrossRef]
- Desplats, V.; Vitte, R.L.; Du Cheyron, J.; Roseau, G.; Fauconnier, A.; Moryoussef, F. Preoperative Rectosigmoid endoscopic ultraso-nography predicts the need for bowel resection in endometriosis. World J. Gastroenterol. 2019, 25, 696–706. [Google Scholar] [CrossRef] [PubMed]
- Noventa, M.; Scioscia, M.; Schincariol, M. Imaging modalities for diagnosis of deep pelvic endometriosis: Comparison be-tween trans-vaginal sonography, rectal endoscopy sonography and magnetic resonance imaging. A Head-to-Head me-ta-analysis. Diagnostics 2019, 9, 225. [Google Scholar] [CrossRef]
- Soyer, P.; Sirol, M.; Dray, X.; Placé, V.; Pautrat, K.; Hamzi, L.; Boudiaf, M. Detection of colorectal tumors with water enema-multidetector row computed tomography. Gastrointest. Radiol. 2012, 37, 1092–1100. [Google Scholar] [CrossRef]
- Ferrero, S.; Biscaldi, E.; Vellone, V.G.; Venturini, P.L.; Leone Roberti Maggiore, U. Computed tomographic colonography vs rectal water- contrast transvaginal sonography in diagnosis of rectosigmoid endometriosis: A pilot study. Ultrasound Obstet. Gynecol. 2017, 49, 515–523. [Google Scholar] [CrossRef] [PubMed]
- Mehedințu, C.; Brîndușe, L.A.; Brătilă, E. Does Computed Tomography–Based Virtual Colonoscopy Improve the Accuracy of Preoperative Assessment Based on Magnetic Resonance Imaging in Women Managed for Colorectal Endometriosis? J. Minim. Invasive Gynecol. 2018, 25, 1009–1017. [Google Scholar] [CrossRef]
- Biscaldi, E.; Ferrero, S.; Maggiore, U.L.R.; Remorgida, V.; Venturini, P.L.; Rollandi, G.A. Multidetector computerized tomography enema versus magnetic resonance enema in the diagnosis of rectosigmoid endometriosis. Eur. J. Radiol. 2014, 83, 261–267. [Google Scholar] [CrossRef]
- Biscaldi, E.; Barra, F.; Maggiore, U.L.R.; Ferrero, S. Other imaging techniques: Double-contrast barium enema, endoscopic ultrasonography, multidetector CT enema, and computed tomography colonoscopy. Best Pr. Res. Clin. Obstet. Gynaecol. 2020, 71, 64–77. [Google Scholar] [CrossRef]
- Biscaldi, E.; Ferrero, S.; Remorgida, V.; Rollandi, G.A. Bowel endometriosis: CT-enteroclysis. Gastrointest. Radiol. 2006, 32, 441–450. [Google Scholar] [CrossRef] [PubMed]
- Ferrero, S.; Biscaldi, E.; Morotti, M. Multidetector computerized tomography enteroclysis vs. rectal water contrast trans-vaginal ultrasonography in determining the presence and extent of bowel endometriosis. Ultrasound Obstet. Gynecol. 2011, 37, 603–613. [Google Scholar] [CrossRef]
- Biscaldi, E.; Barra, F.; Scala, C.; Stabilini, C.; Vellone, V.G.; Ferrero, S. Magnetic Resonance Rectal Enema Versus Computed Tomo-graphic Colonography in the Diagnosis of Rectosigmoid Endometriosis. J. Comput. Assist. Tomogr. 2020, 44, 501–510. [Google Scholar] [CrossRef] [PubMed]
- Jeong, S.Y.; Chung, D.J.; Myung Yeo, D.; Lim, Y.T.; Hahn, S.T.; Lee, J.M. The Usefulness of computed tomographic colonography for evaluation of deep infiltrating endometriosis: Comparison with magnetic resonance imaging. J. Comput. Assist. Tomogr. 2013, 37, 809–814. [Google Scholar] [CrossRef] [PubMed]
- van der Wat, J.; Kaplan, M.D. Modified virtual colonoscopy: A noninvasive technique for the diagnosis of rectovaginal septum and deep infiltrating pelvic endometriosis. J. Minim. Invasive Gynecol. 2007, 14, 638–643. [Google Scholar] [CrossRef]
- Koutoukos, I.; Langebrekke, A.; Young, V.; Qvigstad, E. Imaging of endometriosis with computerized tomography colonography. Fertil. Steril. 2011, 95, 259–260. [Google Scholar] [CrossRef]
- Coppola, F.; Paradisi, R.; Zanardi, S. Computed tomography–colonography with intravenous contrast medium and uro-graphic phase for the evaluation of pelvic deep infiltrating endometriosis of intestinal and urinary tract. J. Comput. Assist. Tomogr. 2019, 43, 513–518. [Google Scholar] [CrossRef]
- Park, S.H.; Yee, J.; Se, H.K.; Young, H.K. Fundamental elements for successful performance of CT colonography (virtual colonos-copy). Korean J. Radiol. 2007, 8, 264–275. [Google Scholar] [CrossRef]
- Roman, H.; Carilho, J.; Da Costa, C. Computed tomography-based virtual colonoscopy in the assessment of bowel endo-metriosis: The surgeon’s point of view. Gynecol Obstet. Fertil. 2016, 44, 3–10. [Google Scholar] [CrossRef]
- Zannoni, L.; Del Forno, S.; Coppola, F.; Papadopoulos, D.; Valerio, D.; Golfieri, R.; Caprara, G.; Paradisi, R.; Seracchioli, R. Comparison of transvaginal sonography and computed tomography–colonography with contrast media and urographic phase for diagnosing deep infiltrating endometriosis of the posterior compartment of the pelvis: A pilot study. Jpn. J. Radiol. 2017, 35, 546–554. [Google Scholar] [CrossRef]
- Cosma, S.; Salgarello, M.; Ceccaroni, M.; Gorgoni, G.; Riboni, F.; La Paglia, E.; Danese, S.; Benedetto, C. Accuracy of a new diagnostic tool in deep infiltrating endometriosis: Positron emission tomography-computed tomography with 16α-[18F]fluoro-17β-estradiol. J. Obstet. Gynaecol. Res. 2016, 42, 1724–1733. [Google Scholar] [CrossRef] [PubMed]
- Mulette, P.; Jacquet, A.; Durlach, A. Pulmonary cavitations with increased 18F-FDG uptake revealing a thoracic endome-triosis: A case report. Medicine 2021, 100, e27550. [Google Scholar] [CrossRef] [PubMed]
- Balogova, S.; Daraï, E.; Noskovicova, L.; Lukac, L.; Talbot, J.-N.; Montravers, F. Interference of Known or Suspected Endometriosis in Reporting FDG PET/CT Performed in Another Indication. Clin. Nucl. Med. 2022, 47, 305–313. [Google Scholar] [CrossRef] [PubMed]





| Classification/Staging System | Pub. Year | Based on | Based Only on Ultrasound | Aim of Classification |
|---|---|---|---|---|
| #Enzian classification [19] | 2021 | Surgical observation/MRI/ultrasound | No | Description of endometriosis |
| Endometriosis Fertility Index (EFI) [47] | 2021 | Surgical observation/ultrasound/clinical examination | No | Probability of pregnancy after endometriosis surgery |
| Adhesion scoring system [48] | 2020 | Ultrasound | Yes | Prediction of the pelvic adhesions |
| ENDORECT * [49] | 2019 | MRI/ultrasound/clinical examination | No | Prediction of rectosigmoid involvement |
| Preoperative ultrasound-based endometriosis staging system (UBESS) [50,51,52] | 2016 | Ultrasound | Yes | Prediction of the level of complexity of laparoscopic surgery |
| Imaging Technique | Time | Advantages | Disadvantages | Sensitivity | Specificity | Rad. Dose |
|---|---|---|---|---|---|---|
| TVUS | 15–20 min | High specificity and high sensitivity for ovarian endometriosis High accuracy in detecting deep endometriosis and POD obliteration High tolerability Cost-effective Offers the opportunity to provide visual evidence to people Dynamic nature for organ mobility Consensus about the descriptions regarding the different locations Allows for anatomical mapping | Limited ability to detect superficial endometriosis The detection of deep endometriosis requires highly trained sonographers Operator dependent Examination may be considered painful | Depends on the location: - Bladder 62% - Rectosigma 95% - ULS 53% - Vaginal fornix 58% - Rectovaginal septum 49% - Parametrium 31% | Depends on the location: - Bladder 100% - Rectosigma 97% - USL 93% - Vaginal fornix 96% - Rectovaginal septum 98% - Parametrium 98% | None |
| MRI | 30–40 min | Images obtained appear the same to all viewers Overall high accuracy in detecting DE and extra-pelvic endometriosis Allows for anatomical mapping Offers an opportunity to provide visual evidence to people Not painful No radiation exposure | Operator-dependent Static assessment Variable imaging protocols reported in the literature Less accurate in defining the bowel depth of invasion Limited ability to detect superficial endometriosis No consensus on how to describe the findings Higher cost compared with ultrasound Training specifically in endometriosis diagnosis needed | Depends on the location: - Bladder 88% - Rectosigma 73% - ULS 85% | Depends on the location: - Bladder 99% - Rectosigma 90% - USL 80% | None |
| DBCE | 7–15 min | Complete overview of the entire colon via retrograde distention Less expensive than REU and MRI | It does not allow for identifying the cause of the mass effect Low specificity Only used in rectosigmoid endometriosis | 42.9–100% * | 93–100% * | <5 mSv |
| REU | 15–20 min | Useful in a virgo patient Estimates the distance between lesions and the anal verge | Investigating only the distal part of the bowel (rectosigmoid) Poor sensitivity for ovarian endometrioma It does not allow for identifying anterior pelvis lesions Only used in rectosigmoid endometriosis | 88.9–97.1% * | 89.4–93.1% * | None |
| MDCT-e | 30 min | Accurate and reproducible in diagnosing intestinal endometriosis Assessing endometriosis’ characteristics: the largest diameter of the nodule, the distance between the distal part of the nodule and the anal verge, and ddepth of infiltration of endometriosis in the intestinal wall | Administration of iodinated contrast medium and radiation exposure Only used in rectosigmoid endometriosis | 93.3–100% * | 96.6–100.0% * | 12–15.8 mSv |
| CTC | 15–24 min | High spatial resolution It allows for estimating the degree of intestinal stenosis Minimally painful | Radiation exposure and the process may require the administration of an iodinated contrast medium Only used in rectosigmoid endometriosis | 68–96% * | 48–86.7% * | 9 mSv |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guerriero, S.; Ajossa, S.; Pagliuca, M.; Borzacchelli, A.; Deiala, F.; Springer, S.; Pilloni, M.; Taccori, V.; Pascual, M.A.; Graupera, B.; et al. Advances in Imaging for Assessing Pelvic Endometriosis. Diagnostics 2022, 12, 2960. https://doi.org/10.3390/diagnostics12122960
Guerriero S, Ajossa S, Pagliuca M, Borzacchelli A, Deiala F, Springer S, Pilloni M, Taccori V, Pascual MA, Graupera B, et al. Advances in Imaging for Assessing Pelvic Endometriosis. Diagnostics. 2022; 12(12):2960. https://doi.org/10.3390/diagnostics12122960
Chicago/Turabian StyleGuerriero, Stefano, Silvia Ajossa, Mariachiara Pagliuca, Antonietta Borzacchelli, Fabio Deiala, Serena Springer, Monica Pilloni, Valeria Taccori, Maria Angela Pascual, Betlem Graupera, and et al. 2022. "Advances in Imaging for Assessing Pelvic Endometriosis" Diagnostics 12, no. 12: 2960. https://doi.org/10.3390/diagnostics12122960
APA StyleGuerriero, S., Ajossa, S., Pagliuca, M., Borzacchelli, A., Deiala, F., Springer, S., Pilloni, M., Taccori, V., Pascual, M. A., Graupera, B., Saba, L., & Alcazar, J. L. (2022). Advances in Imaging for Assessing Pelvic Endometriosis. Diagnostics, 12(12), 2960. https://doi.org/10.3390/diagnostics12122960







