Hereditary Hemorrhagic Telangiectasia—A Case Series Experience from a Liver Transplant Center in Romania
Abstract
1. Introduction
2. Materials and Methods
- Epistaxis (recurrent, spontaneous bleeding episodes with no prior traumatic involvement, night-time nosebleeds).
- Telangiectasis—unevenly distributed on lips, nose, fingers, oral cavity.
- Visceral involvement—AVM in the lungs, brain, liver, stomach, spinal cord.
- A family history of HHT—first-degree relative with a prior diagnosis of HHT.
- None: score 0 or 1;
- Mild: score 1 to 4;
- Moderate: score 4 to 7;
- Severe: score 7 to 10 [12].
3. Results
3.1. Case Series Population
3.2. Clinical Presentation and Lab Testing
4. Discussions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Silvain, C.; Thevenot, T.; Colle, I.; Vilgrain, V.; Dupuis-Girod, S.; Buscarini, E.; Valla, D.; Hillaire, S.; Dutheil, D.; Sitbon, O.; et al. Hereditary hemorrhagic telangiectasia and liver involvement: Vascular liver diseases: Position papers from the francophone network for vascular liver diseases, the French Association for the Study of the Liver (AFEF), and ERN-rare liver. Clin. Res. Hepatol. Gastroenterol. 2020, 44, 426–432. [Google Scholar] [CrossRef] [PubMed]
- Larson, A.M. Liver disease in hereditary hemorrhagic telangiectasia. J. Clin. Gastroenterol. 2003, 36, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Tortora, A.; Riccioni, M.E.; Gaetani, E.; Ojetti, V.; Holleran, G.; Gasbarrini, A. Rendu-Osler-Weber disease: A gastroenterologist’s perspective. Orphanet J. Rare Dis. 2019, 14, 130. [Google Scholar] [CrossRef] [PubMed]
- Siddiki, H.; Doherty, M.G.; Fletcher, J.G.; Stanson, A.W.; Vrtiska, T.J.; Hough, D.M.; Fidler, J.L.; McCollough, C.H.; Swanson, K.L. Abdominal findings in hereditary hemorrhagic telangiectasia: Pictorial essay on 2D and 3D findings with isotropic multiphase CT. RadioGraphics 2008, 28, 171–183. [Google Scholar] [CrossRef]
- Ravard, G.; Soyer, P.; Boudiaf, M.; Terem, C.; Abitbol, M.; Yeh, J.F.; Brouard, R.; Hamzi, L.; Rymer, R. Hepatic involvement in hereditary hemorrhagic telangiectasia: Helical computed tomography features in 24 consecutive patients. J. Comput. Assist. Tomogr. 2004, 28, 488–495. [Google Scholar] [CrossRef]
- Buscarini, E.; Leandro, G.; Conte, D.; Danesino, C.; Daina, E.; Manfredi, G.; Lupinacci, G.; Brambilla, G.; Menozzi, F.; De Grazia, F.; et al. Natural history and outcome of hepatic vascular malformations in a large cohort of patients with hereditary hemorrhagic teleangiectasia. Dig. Dis. Sci. 2011, 56, 2166–2178. [Google Scholar] [CrossRef]
- Choi, H.H.-I.; Manning, M.A.; Mehrotra, A.K.; Wagner, S.; Jha, R.C. Primary hepatic neoplasms of vascular origin: Key imaging features and differential diagnoses with radiology-pathology correlation. Am. J. Roentgenol. 2017, 209, W350–W359. [Google Scholar] [CrossRef]
- Bernabeu, C.; Bayrak-Toydemir, P.; McDonald, J.; Letarte, M. Potential Second-Hits in Hereditary Hemorrhagic Telangiectasia. J. Clin. Med. 2020, 9, 3571. [Google Scholar] [CrossRef]
- Faughnan, M.E.; Mager, J.J.; Hetts, S.W.; Palda, V.A.; Lang-Robertson, K.; Buscarini, E.; Deslandres, E.; Kasthuri, R.S.; Lausman, A.; Poetker, D.; et al. Second International Guidelines for the Diagnosis and Management of Hereditary Hemorrhagic Telangiectasia. Ann. Intern. Med. 2020, 173, 989–1001. [Google Scholar] [CrossRef]
- Shovlin, C.L.; Guttmacher, A.E.; Buscarini, E.; Faughnan, M.E.; Hyland, R.H.; Westermann, C.J.; Kjeldsen, A.D.; Plau-chu, H. Diagnostic criteria for hereditary hemorrhagic telangiectasia (Rendu-Osler-Weber syndrome). Am. J. Med. Genet. 2000, 91, 66–67. [Google Scholar] [CrossRef]
- van Gent, M.W.; Velthuis, S.; Post, M.C.; Snijder, R.J.; Westermann, C.J.; Letteboer, T.G.; Mager, J.J. Hereditary hemorrhagic telangiectasia: How accurate are the clinical criteria? Am. J. Med. Genet. A 2013, 161, 461–466. [Google Scholar] [CrossRef] [PubMed]
- Nosebleed Severity Score (ESS); Cure HHT: Monkton, MD, USA, 2022.
- Halderman, A.A.; Ryan, M.W.; Marple, B.F.; Sindwani, R.; Reh, D.D.; Poetker, D.M. Bevacizumab for Epistaxis in Hereditary Hemorrhagic Telangiectasia: An Evidence-based Review. Am. J. Rhinol. Allergy 2018, 32, 258–268. [Google Scholar] [CrossRef] [PubMed]
- Proctor, D.D.; Henderson, K.J.; Dziura, J.D.; Longacre, A.V.; White, R.I., Jr. Enteroscopic evaluation of the gastrointestinal tract in symptomatic patients with hereditary hemorrhagic telangiectasia. J. Clin. Gastroenterol. 2005, 39, 115–119. [Google Scholar] [PubMed]
- Faughnan, M.E.; Palda, V.A.; Garcia-Tsao, G.; Geisthoff, U.W.; McDonald, J.; Proctor, D.D.; Spears, J.; Brown, D.H.; Busca-rini, E.; Chesnutt, M.S.; et al. International guidelines for the diagnosis and management of hereditary haemorrhagic telangiectasia. J. Med. Genet. 2011, 48, 73–87. [Google Scholar] [CrossRef] [PubMed]
- Fodstad, P.; Dheyauldeen, S.; Rinde, M.; Bachmann-Harildstad, G. Anti-VEGF with 3-week intervals is effective on anemia in a patient with severe hereditary hemorrhagic telangiectasia. Ann. Hematol. 2011, 90, 611–612. [Google Scholar] [CrossRef] [PubMed]
- Al-Samkari, H.; Albitar, H.A.; Olitsky, S.E.; Clancy, M.S.; Iyer, V.N. Systemic bevacizumab for high-output cardiac failure in hereditary hemorrhagic telangiectasia: An international survey of HHT centers. Orphanet J. Rare Dis. 2019, 14, 256. [Google Scholar] [CrossRef] [PubMed]
- Garg, N.; Khunger, M.; Gupta, A.; Kumar, N. Optimal management of hereditary hemorrhagic telangiectasia. J. Blood Med. 2014, 5, 191–206. [Google Scholar]
- Alabdulghani, F.; Healy, G.; Cantwell, C. Radiological findings in ischaemic cholangiopathy. Clin. Radiol. 2020, 75, 161–168. [Google Scholar] [CrossRef]
- Moulinet, T.; Mohamed, S.; Deibener-Kaminsky, J.; Jankowski, R.; Kaminsky, P.J. High prevalence of arterial aneurysms in hereditary hemorrhagic telangiectasia. Int. J. Cardiol. 2014, 176, 1414–1416. [Google Scholar] [CrossRef]
- Sellier, J.; Karam, C.; Beauchet, A.; Dallongeville, A.; Binsse, S.; Blivet, S.; Bourgault-Villada, I.; Charron, P.; Chinet, T.; Eyries, M.J. Higher prevalence of splenic artery aneurysms in hereditary hemorrhagic telangiectasia: Vascular implications and risk factors. PLoS ONE 2020, 15, e0226681. [Google Scholar] [CrossRef]
- Lerut, J.; Orlando, G.; Adam, R.; Sabba, C.; Pfitzmann, R.; Klempnauer, J.; Belghiti, J.; Pirenne, J.; Thevenot, T.; Hillert, C.; et al. Liver transplantation for hereditary hemorrhagic telangiectasia: Report of the European liver transplant registry. Ann. Surg. 2006, 244, 854–862; discussion 862–864. [Google Scholar] [CrossRef] [PubMed]
- Aseni, P.; Vertemati, M.; Minola, E.; Bonacina, E. Massive haemoptysis after living donor liver transplantation. J. Clin. Pathol. 2003, 56, 876–878. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Meier, N.M.; Foster, M.L.; Battaile, J.T. Hereditary hemorrhagic telangiectasia and pulmonary arteriovenous malformations: Clinical aspects. Cardiovasc. Diagn. Ther. 2018, 8, 316. [Google Scholar] [CrossRef] [PubMed]
| Patient No | Age | Sex | Curaçao Criteria | Molecular Diagnosis | Bleeding | Hepatic MANIFESTATIONS | Cardiac MANIFESTATIONS | Cerebral CT | Chest CT | Abdominal CT |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 47 | F | + | − | + | + | + | + | n/a | + |
| 2 | 68 | F | + | − | + | + | + | n/a | n/a | + |
| 3 | 54 | M | + | − | + | − | + | + | n/a | n/a |
| 4 | 41 | F | − | + | + | − | − | n/a | + | + |
| 5 | 43 | M | + | − | + | + | − | n/a | + | + |
| 6 | 74 | F | + | − | − | + | + | + | n/a | + |
| 7 | 51 | F | + | − | + | − | + | n/a | n/a | n/a |
| 8 | 42 | F | + | − | − | − | + | + | + | n/a |
| 9 | 45 | F | + | − | + | + | + | + | + | + |
| 10 | 49 | F | + | − | + | − | − | n/a | n/a | n/a |
| 11 | 52 | F | + | − | + | + | − | n/a | + | + |
| 12 | 64 | F | + | − | + | − | + | n/a | + | + |
| 13 | 51 | F | + | − | − | + | + | + | + | + |
| 14 | 40 | F | − | + | + | − | − | n/a | + | + |
| Patient No. | Hb (g/dL) | Platelets (/uL × 1000) | Feritin (ng/mL) | INR | GGT (U/L) | ALP (U/L) | AST (IU/L) | ALT (IU/L) | Cholesterol (IU/L) | Creatinine (mg/dL) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 9 | 307 | - | 1.92 | 304 | 259 | 226 | 97 | 187 | 0.99 |
| 2 | 10 | 211 | - | 1.29 | 156 | 138 | 25 | 15 | 165 | |
| 3 | 7.5 | 235 | 20.2 | 1.13 | 40 | 76 | 22 | 22 | 198 | 1.15 |
| 4 | 7.1 | 338 | 3.6 | 1.07 | 20 | 64 | 24 | 28 | 187 | 0.86 |
| 5 | 15.6 | 303 | 43 | 0.96 | 16 | 68 | 20 | 21 | 198 | 0.97 |
| 6 | 12.3 | 31 | 85.6 | 1.43 | 450 | 160 | 77 | 29 | 157 | 1.37 |
| 7 | 11.6 | 300 | 14.3 | 1.12 | 20 | 103 | 27 | 25 | 189 | 1.01 |
| 8 | 11.1 | 432 | 27.7 | 1.06 | 122 | 219 | 19 | 16 | 176 | 0.74 |
| 9 | 10.7 | 355 | 6.7 | 1.08 | 39 | 85 | 25 | 30 | 177 | 0.63 |
| 10 | 12.4 | 182 | 8.5 | 0.96 | 5 | 46 | 19 | 14 | 191 | 0.84 |
| 11 | 6.8 | 222 | 6 | 1.2 | 208 | 231 | 25 | 22 | 185 | 0.8 |
| 12 | 5.7 | 126 | 45.9 | 1.75 | 75 | 70 | 22 | 27 | 168 | 0.93 |
| 13 | 9.7 | 255 | 21 | 0.91 | 39 | 97 | 29 | 40 | 230 | 0.79 |
| 14 | 11.4 | 381 | 20.2 | 0.97 | 3 | 70 | 24 | 16 | 245 | 0.78 |
| Mean | 10.35 | 277.5 | 20.2 | 1.1 | 39.5 | 91.1 | 24.5 | 23.5 | 187.0 | 0.9 |
| Range | 7.1–15.6 | 31.000–432.000 | 3.6–85.6 | 0.91–1.75 | 3–450 | 46–259 | 19–226 | 14–97 | 157–245 | 0.63–1.37 |
| Patient No. | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
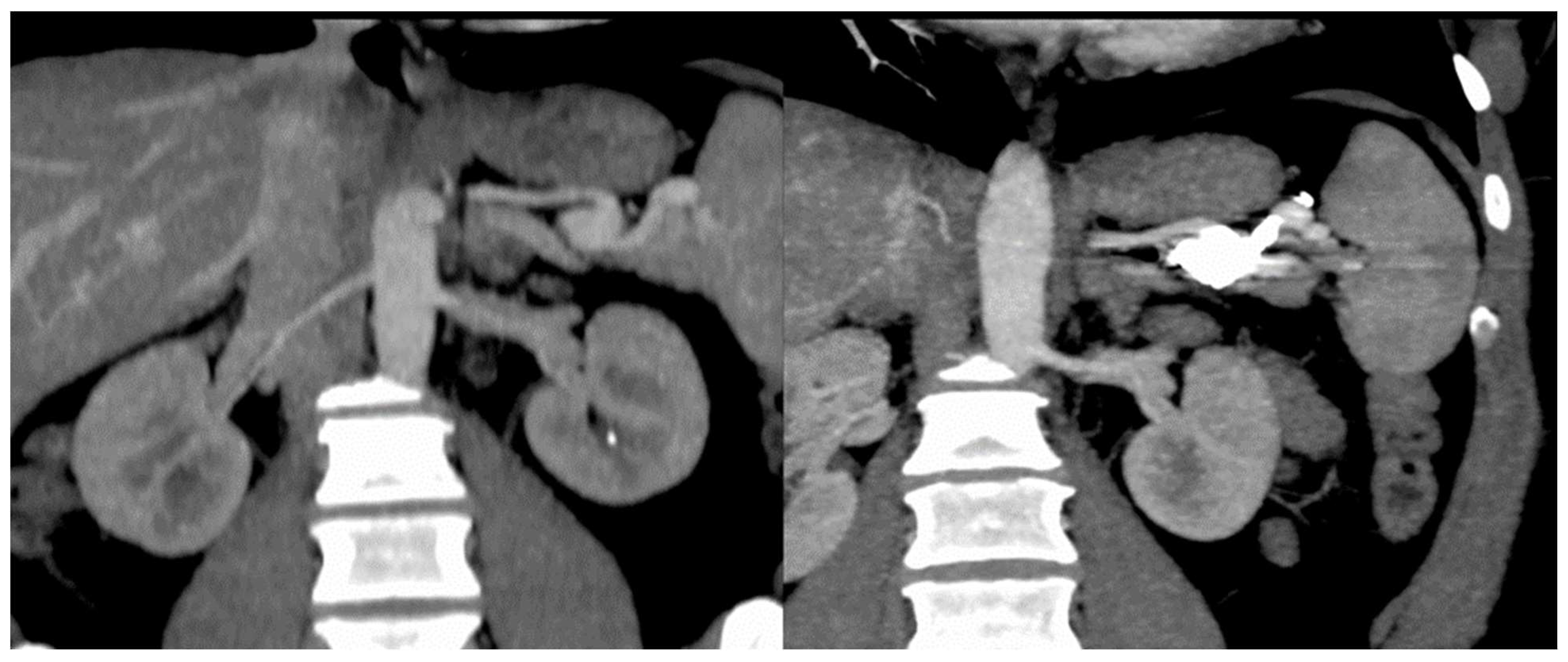
| Hepatomegaly | + | + | + | + | + | + | + | + | + | + | + | + | − | + | 13 |
| Splenomegaly | − | − | − | − | − | + | − | − | + | − | + | − | − | − | 3 |
| Cirrhotic liver | − | + | + | − | − | − | − | − | − | + | + | + | − | − | 5 |
| HA diameter (mm) | + | 14 | 13 | − | − | 12 | 11 | 11 | 10 | 13 | 14 | + | 14 | 10 | Mean −12.2 |
| Dilated/tortuous intrahepatic artery branches | + | + | + | − | − | − | − | − | − | + | + | + | − | − | 6 |
| HA to HV shunting | + | + | + | + | + | + | − | + | + | − | + | + | + | − | 11 |
| HA to PV shunting | + | + | + | − | − | − | − | − | − | − | + | + | − | − | 5 |
| PV to PV shunting | − | + | + | − | − | − | − | − | − | − | − | − | − | − | 2 |
| Intrahepatic telangiectasis | + | + | + | + | + | + | − | + | + | + | + | + | + | − | 12 |
| Splenic artery thrombosis | + | − | + | − | − | − | − | − | + | − | − | − | − | − | 3 |
| Heterogenous enhancement on arterial phase | + | + | + | + | + | − | − | + | + | + | + | + | − | − | 10 |
| PV enlargement | − | + | + | − | − | + | − | − | + | − | + | + | − | − | 6 |
| HV enlargement | + | + | + | + | − | − | − | + | + | + | + | + | − | − | 10 |
| Collateral circulation | + | + | − | − | − | − | − | + | + | − | + | − | − | − | 5 |
| IHBD dilatations | − | + | + | − | − | + | + | − | − | + | − | − | − | − | 5 |
| Biliary cyst | − | − | − | − | − | − | − | + | − | − | − | − | − | − | 1 |
| Hemangioma | − | + | + | + | − | + | − | + | + | − | − | − | − | − | 6 |
| Nodular hyperplasia | − | + | − | − | − | − | − | − | − | + | − | − | − | − | 2 |
| Ascites | − | + | + | + | − | − | − | + | − | + | + | − | − | + | 7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pavel, C.; Cabel, T.; Dinuță, D.; Zaharia, A.; Dima, S.O.; Sandru, V.; Grasu, M.C.; Mihaila, M. Hereditary Hemorrhagic Telangiectasia—A Case Series Experience from a Liver Transplant Center in Romania. Diagnostics 2022, 12, 2959. https://doi.org/10.3390/diagnostics12122959
Pavel C, Cabel T, Dinuță D, Zaharia A, Dima SO, Sandru V, Grasu MC, Mihaila M. Hereditary Hemorrhagic Telangiectasia—A Case Series Experience from a Liver Transplant Center in Romania. Diagnostics. 2022; 12(12):2959. https://doi.org/10.3390/diagnostics12122959
Chicago/Turabian StylePavel, Christopher, Teodor Cabel, Dragoș Dinuță, Alexandru Zaharia, Simona Olimpia Dima, Vasile Sandru, Mugur Cristian Grasu, and Mariana Mihaila. 2022. "Hereditary Hemorrhagic Telangiectasia—A Case Series Experience from a Liver Transplant Center in Romania" Diagnostics 12, no. 12: 2959. https://doi.org/10.3390/diagnostics12122959
APA StylePavel, C., Cabel, T., Dinuță, D., Zaharia, A., Dima, S. O., Sandru, V., Grasu, M. C., & Mihaila, M. (2022). Hereditary Hemorrhagic Telangiectasia—A Case Series Experience from a Liver Transplant Center in Romania. Diagnostics, 12(12), 2959. https://doi.org/10.3390/diagnostics12122959








