Efficacy of Hip Strengthening on Pain Intensity, Disability, and Strength in Musculoskeletal Conditions of the Trunk and Lower Limbs: A Systematic Review with Meta-Analysis and Grade Recommendations
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy and Inclusion Criteria
2.2. Trial Selection and Methodological Quality Assessment
2.3. Data Extraction
2.4. Data Analysis
3. Results
3.1. Study Characteristics
3.2. Methodological Quality of the Included Trials
3.3. Summary of Evidence for the Short-Term Effects of Hip Strengthening on Pain Intensity, Disability, and Hip Strength in People with Musculoskeletal Health Conditions of the Trunk and Lower Limbs
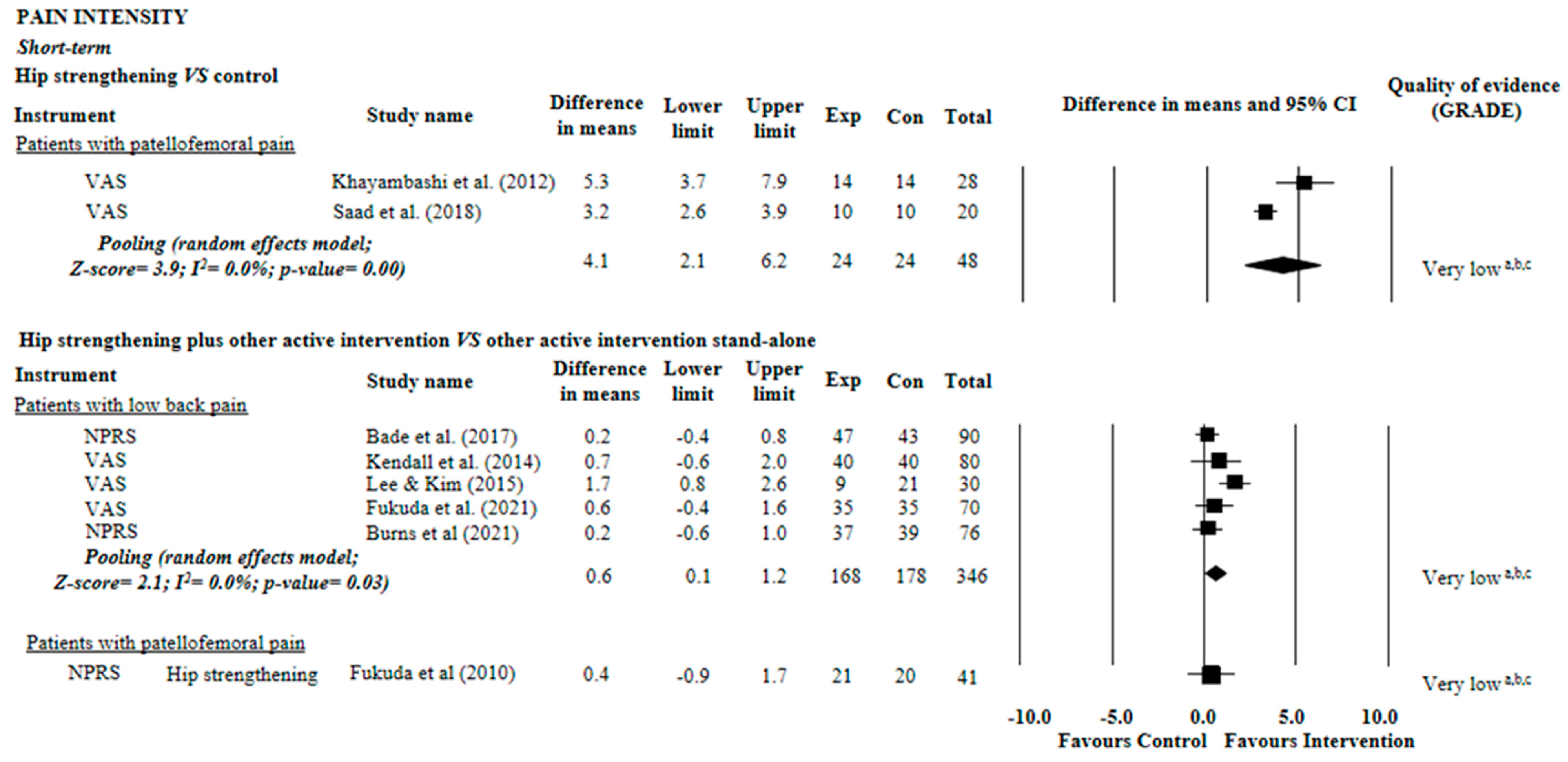
3.4. Pain Intensity
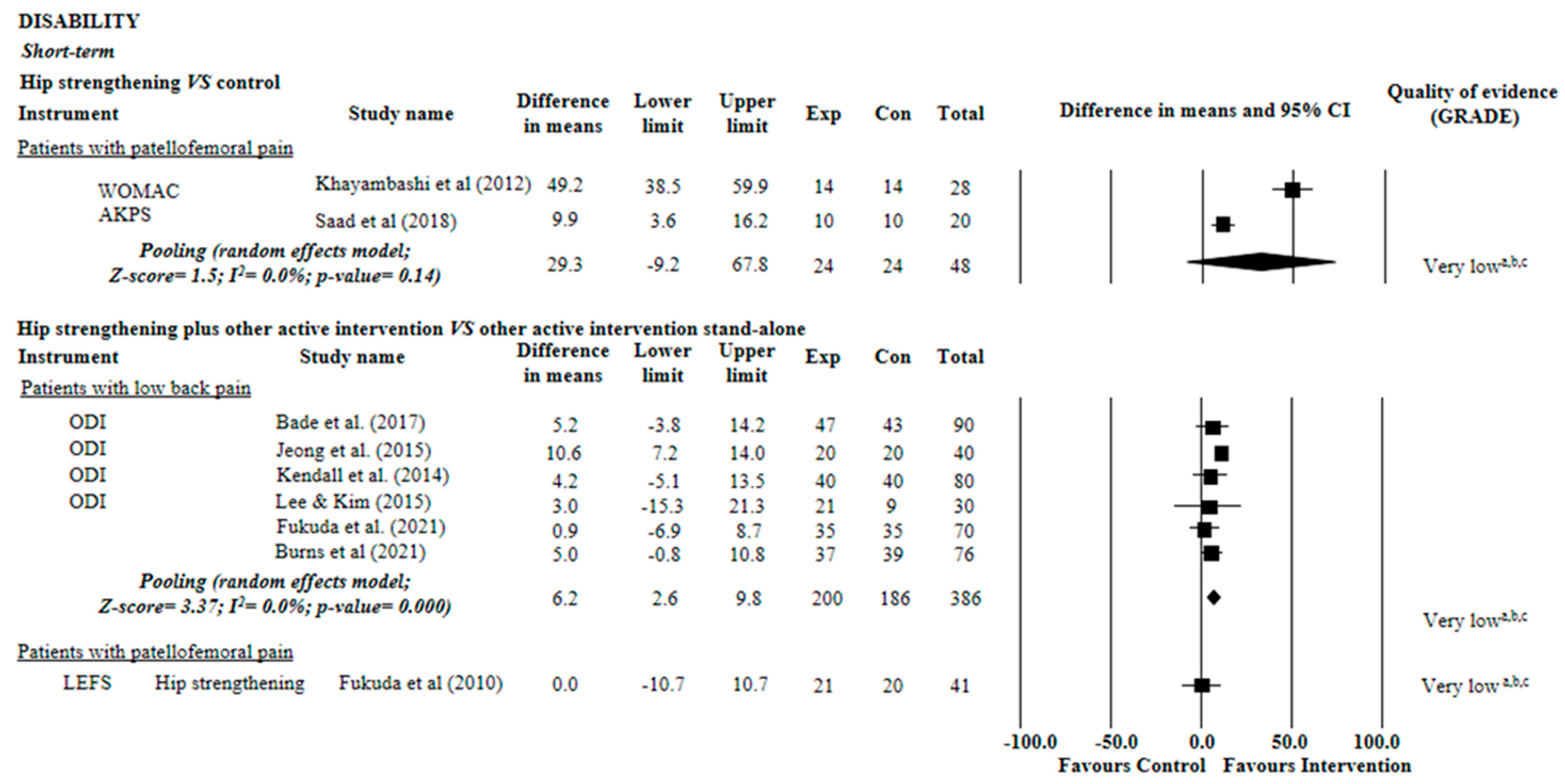
3.5. Disability
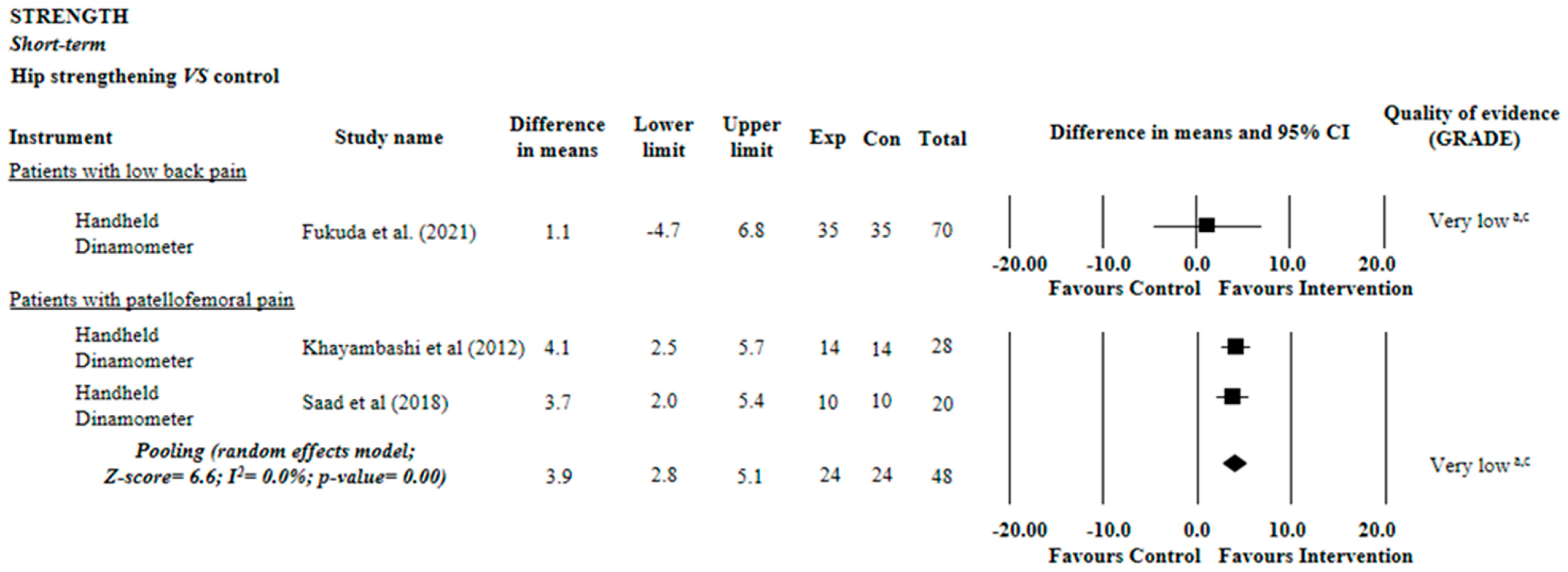
3.6. Hip Strength
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Distefano, L.J.; Blackburn, J.T.; Marshall, S.W.; Padua, D.A. Gluteal muscle activation during common therapeutic exercises. J. Orthop. Sport. Phys. Ther. 2009, 39, 532–540. [Google Scholar] [CrossRef] [PubMed]
- Ebert, J.R.; Edwards, P.K.; Fick, D.P.; Janes, G.C. Systematic review of rehabilitation exercises to progressively load the Gluteus Medius. J. Sport Rehabil. 2017, 26, 418–436. [Google Scholar] [CrossRef] [PubMed]
- Rubinstein, S.M.; van Middelkoop, M.; Assendelft, W.J.J.; de Boer, M.R.; van Tulder, M.W. Spinal manipulative therapy for chronic low-back pain: An update of a cochrane review. Spine 2011, 36, E825–E846. [Google Scholar] [CrossRef] [PubMed]
- Goode, A.P.; Taylor, S.S.; Hastings, S.N.; Stanwyck, C.; Coffman, C.J.; Allen, K.D. Effects of a home-based telephone- Supported physical activity program for older adult veterans with chronic low back pain. Phys. Ther. 2018, 98, 369–380. [Google Scholar] [CrossRef] [PubMed]
- Pareja-Blanco, F.; Alcazar, J.; Cornejo-Daza, P.J.; Sánchez-Valdepeñas, J.; Rodriguez-Lopez, C.; Hidalgo-de Mora, J.; Sánchez-Moreno, M.; Bachero-Mena, B.; Alegre, L.M.; Ortega-Becerra, M. Effects of velocity loss in the bench press exercise on strength gains, neuromuscular adaptations, and muscle hypertrophy. Scand. J. Med. Sci. Sports 2020, 30, 2154–2166. [Google Scholar] [CrossRef] [PubMed]
- Akuthota, V.; Ferreiro, A.; Moore, T.; Fredericson, M. Core stability exercise principles. Curr. Sport. Med. Rep. 2008, 7, 39–44. [Google Scholar] [CrossRef]
- Cashman, G.E. The effect of weak hip abductors or external rotators on knee valgus kinematics in healthy subjects: A systematic review. J. Sport. Rehabil. 2012, 21, 273–284. [Google Scholar] [CrossRef]
- Parr, M.; Price, P.D.; Cleather, D.J. Effect of a gluteal activation warm-up on explosive exercise performance. BMJ Open Sport Exerc. Med. 2017, 3, e000245. [Google Scholar] [CrossRef]
- Sadler, S.; Cassidy, S.; Peterson, B.; Spink, M.; Chuter, V. Gluteus medius muscle function in people with and without low back pain: A systematic review. BMC Musculoskelet. Disord. 2019, 20, 463. [Google Scholar] [CrossRef]
- Nascimento, L.R.; Teixeira-Salmela, L.F.; Souza, R.B.; Resende, R.A. Hip and knee strengthening is more effective than knee strengthening alone for reducing pain and improving activity in individuals with patellofemoral pain: A systematic review with meta-analysis. J. Orthop. Sport. Phys. Ther. 2018, 48, 19–31. [Google Scholar] [CrossRef]
- Neto, W.K.; Soares, E.G.; Vieira, T.L.; Aguiar, R.; Chola, T.A.; de Lima Sampaio, V.; Gama, E.F. Gluteus maximus activation during common strength and hypertrophy exercises: A systematic review. J. Sport. Sci. Med. 2020, 19, 195. [Google Scholar]
- Thomson, C.; Krouwel, O.; Kuisma, R.; Hebron, C. The outcome of hip exercise in patellofemoral pain: A systematic review. Man. Ther. 2016, 26, 1–30. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An update guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Bushman, B.A.; Battista, R.; Swan, P.; Ransdell, L.; Thompson, W.R. ACSM’s Resources for the Personal Trainer, 4th ed.; Wolters Kluwer Health Adis (ESP): Philadelphia, PA, USA, 2013. [Google Scholar]
- Latessa, I.; Ricciardi, C.; Jacob, D.; Jónsson, H., Jr.; Gambacorta, M.; Improta, G.; Gargiulo, P. Health technology assessment through Six Sigma Methodology to assess cemented and uncemented protheses in total hip arthroplasty. Eur. J. Transl. Myol. 2021, 31. [Google Scholar] [CrossRef]
- Norouzi, A.; Behrouzibakhsh, F.; Kamali, A.; Yazdi, B.; Ghaffari, B. Short-term complications of anesthetic technique used in hip fracture surgery in elderly people. Eur. J. Transl. Myol. 2018, 28. [Google Scholar] [CrossRef]
- Magnússon, B.; Pétursson, Þ.; Edmunds, K.; Magnúsdóttir, G.; Halldórsson, G.; Jónsson, H., Jr.; Gargiulo, P. Improving planning and post-operative assessment for Total Hip Arthroplasty. Eur. J. Transl. Myol. 2015, 25. [Google Scholar] [CrossRef]
- Elkins, M.R.; Moseley, A.M.; Sherrington, C.; Herbert, R.D.; Maher, C.G. Growth in the Physiotherapy Evidence Database (PEDro) and use of the PEDro scale. Br. J. Sport. Med. 2013, 47, 188–189. [Google Scholar] [CrossRef]
- Yamato, T.P.; Maher, C.; Koes, B.; Moseley, A. The PEDro scale had acceptably high convergent validity, construct validity, and interrater reliability in evaluating methodological quality of pharmaceutical trials. J. Clin. Epidemiol. 2017, 86. [Google Scholar] [CrossRef]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef]
- Feldwieser, F.; Kiselev, J.; Hardy, S.; Garcia-Agundez, A.; Eicher, C.; Steinhagen-Thiessen, E.; Göbel, S. Evaluation of biofeedback based bridging exercises on older adults with low back pain: A randomized controlled trial. Physiother. Pract. Res. 2018, 39. [Google Scholar] [CrossRef]
- Amaral, L.K.; Souza, M.B.; Campos, M.G.; Mendonça, V.A.; Bastone, A.; Pereira, L.S.; Mascarenhas, R.O.; Oliveira, V.C. Efficacy of conservative therapy in older people with nonspecific low back pain: A systematic review with meta-analysis and GRADE recommendations. Arch. Gerontol. Geriatr. 2020, 90, 104177. [Google Scholar] [CrossRef] [PubMed]
- Ioannidis, J.P.A. Integration of evidence from multiple meta-analyses: A primer on umbrella reviews, treatment networks and multiple treatments meta-analyses. CMAJ Can. Med. Assoc. J. 2009, 181, 488–493. [Google Scholar] [CrossRef] [PubMed]
- Deeks, J.J.; Higgins, J.P.; Altman, D.G. Chapter 10: Analysing data and undertaking meta-analyses. In Cochrane Handbook for Systematic Reviews of Interventions Version 6.2; Cochrane: London, UK, 2021; Volume 3. [Google Scholar]
- Higgins, J.P.; Green, S. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 (Updated July 2019); Cochrane: London, UK, 2019; Available online: www.training.cochrane.org/handbook (accessed on 31 March 2020).
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924. [Google Scholar] [CrossRef] [PubMed]
- Balshem, H.; Helfand, M.; Schünemann, H.J.; Oxman, A.D.; Kunz, R.; Brozek, J.; Vist, G.E.; Falck-Ytter, Y.; Meerpohl, J.; Norris, S.; et al. GRADE guidelines: 3. Rating the quality of evidence. J. Clin. Epidemiol. 2011, 64, 401–406. [Google Scholar] [CrossRef]
- Foley, N.C.; Teasell, R.W.; Bhogal, S.K.; Speechley, M.R. Stroke rehabilitation evidence-based review: Methodology. Top. Stroke Rehabil. 2003, 10, 1–7. [Google Scholar] [CrossRef]
- Hart, R.G.; Pearce, L.A.; Aguilar, M.I. Meta-analysis: Antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann. Intern. Med. 2007, 146. [Google Scholar] [CrossRef]
- Fukuda, T.Y.; Rossetto, F.M.; Magalhães, E.; Bryk, F.F.; Lucareli, P.R.G.; de Almeida Carvalho, N.A. Short-term effects of hip abductors and lateral rotators strengthening in females with patellofemoral pain syndrome: A randomized controlled clinical trial. J. Orthop. Sport. Phys. Ther. 2010, 40, 736–742. [Google Scholar] [CrossRef]
- Khayambashi, K.; Mohammadkhani, Z.; Ghaznavi, K.; Lyle, M.A.; Powers, C.M. The effects of isolated hip abductor and external rotator muscle strengthening on pain, health status, and hip strength in females with patellofemoral pain: A randomized controlled trial. J. Orthop. Sport. Phys. Ther. 2012, 42, 22–29. [Google Scholar] [CrossRef]
- Saad, M.C.; de Vasconcelos, R.A.; de Oliveira Mancinelli, L.V.; de Barros Munno, M.S.; Liporaci, R.F.; Grossi, D.B. Is hip strengthening the best treatment option for females with patellofemoral pain? A randomized controlled trial of three different types of exercises. Braz. J. Phys. Ther. 2018, 22, 408–416. [Google Scholar] [CrossRef]
- Bade, M.; Cobo-Estevez, M.; Neeley, D.; Pandya, J.; Gunderson, T.; Cook, C. Effects of manual therapy and exercise targeting the hips in patients with low-back pain—A randomized controlled trial. J. Eval. Clin. Pract. 2017, 23, 734–740. [Google Scholar] [CrossRef]
- Jeong, U.C.; Sim, J.H.; Kim, C.Y.; Hwang-Bo, G.; Nam, C.W. The effects of gluteus muscle strengthening exercise and lumbar stabilization exercise on lumbar muscle strength and balance in chronic low back pain patients. J. Phys. Ther. Sci. 2015, 27, 3813–3816. [Google Scholar] [CrossRef] [PubMed]
- Kendall, K.D.; Emery, C.A.; Wiley, J.P.; Ferber, R. The effect of the addition of hip strengthening exercises to a lumbopelvic exercise programme for the treatment of non-specific low back pain: A randomized controlled trial. J. Sci. Med. Sport 2015, 18, 626–631. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.W.; Kim, S.Y. Effects of hip exercises for chronic low-back pain patients with lumbar instability. J. Phys. Ther. Sci. 2015, 27, 345–348. [Google Scholar] [CrossRef] [PubMed]
- Fukuda, T.Y.; Aquino, L.M.; Pereira, P.; Ayres, I.; Feio, A.F.; de Jesus, F.L.A.; Neto, M.G. Does adding hip strengthening exercises to manual therapy and segmental stabilization improve outcomes in patients with nonspecific low back pain? A randomized controlled trial. Braz. J. Phys. Ther. 2021, 25, 900–907. [Google Scholar] [CrossRef]
- Burns, S.A.; Cleland, J.A.; Rivett, D.A.; O’Hara, M.C.; Egan, W.; Pandya, J.; Snodgrass, S.J. When Treating Coexisting Low Back Pain and Hip Impairments, Focus on the Back: Adding Specific Hip Treatment Does Not Yield Additional Benefits-A Randomized Controlled Trial. J. Orthop. Sport. Phys. Ther. 2021, 51, 581–601. [Google Scholar] [CrossRef]
- de Jesus, F.L.A.; Fukuda, T.Y.; Souza, C.; Guimarães, J.; Aquino, L.; Carvalho, G.; Powers, C.; Gomes-Neto, M. Addition of specific hip strengthening exercises to conventional rehabilitation therapy for low back pain: A systematic review and meta-analysis. Clin. Rehabil. 2020, 34, 1368–1377. [Google Scholar] [CrossRef]
- Rogan, S.; Haehni, M.; Luijckx, E.; Dealer, J.; Reuteler, S.; Taeymans, J. Effects of Hip Abductor Muscles Exercises on Pain and Function in Patients With Patellofemoral Pain: A Systematic Review and Meta-Analysis. J. Strength Cond. Res. 2019, 33, 3174–3187. [Google Scholar] [CrossRef]
- Kambič, T.; Lainščak, M.; Hadžić, V. Reproducibility of isokinetic knee testing using the novel isokinetic SMM iMoment dynamometer. PLoS ONE 2020, 15, e0237842. [Google Scholar] [CrossRef]
- van der Heijden, R.A.; Lankhorst, N.E.; van Linschoten, R.; Bierma-Zeinstra, S.M.A.; van Middelkoop, M. Exercise for treating patellofemoral pain syndrome: An abridged version of Cochrane Systematic Review. Eur. J. Phys. Rehabil. Med. 2016, 51, 110–133. [Google Scholar]
- Johnsen, L.G.; Hellum, C.; Nygaard, Ø.P.; Storheim, K.; Brox, J.I.; Rossvoll, I.; Leivseth, G.; Grotle, M. Comparison of the SF6D, the EQ5D, and the oswestry disability index in patients with chronic low back pain and degenerative disc disease. BMC Musculoskelet. Disord. 2013, 14, 148. [Google Scholar] [CrossRef]
- Youdas, J.W.; Mraz, S.T.; Norstad, B.J.; Schinke, J.J.; Hollman, J.H. Determining meaningful changes in hip abductor muscle strength obtained by handheld dynamometry. Physiother. Theory Pract. 2008, 24, 215–220. [Google Scholar] [CrossRef] [PubMed]

| Study | Source | Participants | Intervention | Outcome Measures |
|---|---|---|---|---|
| Bade et al. (2017) [33] | Patients with low back pain Location: Germany | N = 90 Age 46.4 (SD 2.8) Gender M: 53 F: 37 | Exp1 = lumbar strengthening (exercises for low back pain treatment) 2x/week, 50 min/session, over 2 weeks (n = 43, age: 48.1 (SD 2.4)) Exp2 = lumbar + hip strengthening (exercises for low back pain treatment associated with exercises to strengthen hip-stabilizing muscles) 2x/week, 50 min/session, over 2 weeks (n = 47, age: 44.8 (SD 2.3)) | Pain intensity: NPRS (0–10) Disability: ODI (0–50) Follow-up: 2 weeks (short-term) |
| Burns et al. (2021) [38] | Patients with low back pain Location: multicenter | N = 76 Age 40.05 (SD 2.21) Gender M: 29 F: 47 | Exp 1 = treatment of the lumbar spine only (LBO group) 2 to 3x/week, approximately 45 to 60 min/session (n = 39, age: 40.2 (SD 19.9)) Exp2 = lumbar spine and hip treatments (LBH group) 2 to 3x/week, approximately 45 to 60 min/session (n = 37, age: 39.9 (SD 18)) | Pain intensity: NPRS (0–10) Disability: ODI (0–100) Follow-up: 7 weeks (short-term) |
| Fukuda et al. (2021) [37] | Patients with low back pain Location: Brazil | N = 70 Age 37.7 (SD 3.53) Gender S/N | Exp1 = a manual therapy and lumbar segmental stabilization group (MTLS) 2x/week, 30 min/session, over 5 weeks (n = 35, age: 35.2 (SD 12.5)) Exp2 = specific hip-strengthening exercises plus manual therapy and lumbar segmental stabilization group (MTLSHS) 2x/week, 45 min/session, over 5 weeks (n = 35, age: 40.2 (SD 12.4)) | Pain intensity: VAS (0–10) Disability: Roland–Morris (0–24) Strength: Force dynamometer Follow-up: 5 weeks (short-term) |
| Fukuda et al. (2010) [30] | Patients with patellofemoral pain Location: Brazil | N = 66 Age 24.6 (SD 6.6) Gender M: 0 F: 66 | Exp1 = knee strengthening (exercises to strengthen quadriceps) 3x/week, 50 min/session, over 4 weeks (n = 20, age: 25.0 (SD 6.0)) Exp2 = knee + hip strengthening (exercises to strengthen quadriceps and exercises to strengthen the hip abductor and lateral rotator muscles) 3x/week, 50 min/session, over 4 weeks (n = 21, age: 25.0 (SD 7.0)) Con = no intervention (n = 25, age 24.0 (SD 7.0)) | Pain intensity: NPRS (0–10) Disability: LEFS (0–80) Follow-up: 4 weeks (short-term) |
| Jeong et al. (2015) [34] | Patients with low back pain Location: Korea | N = 40 Age 41.2 (SD 6.1) Gender M: 0 F: 40 | Exp1 = lumbopelvic muscle + gluteus strengthening (exercises to strengthen gluteus) 3x/week, 50 min/session, over 6 weeks (n = 20, age: 41.2 (SD 5.5)) Exp2 = lumbopelvic muscle strengthening (exercises to strengthen lumbopelvic muscles) 3x/week, 50 min/session, over 6 weeks (n = 20, age: 41.2 (SD 6.7)) | Disability: ODI (0–50) Follow-up: 6 weeks (short-term) |
| Kendall et al. (2014) [35] | Patients with low back pain Location: Brazil | N = 80 Age 37 (SD 35.5) Gender M: 0 F: 80 | Exp1 = lumbopelvic muscle strengthening (focused on the performance of the motor skill of co-contracting the transversus abdominis, multifidus, and pelvic floor muscles), 6 weeks (n = 40, age: 33 (SD 33.4)) Exp2 = lumbopelvic muscle + hip strengthening (co-contracting the transversus abdominis, multifidus, and pelvic floor muscles associated with open and closed kinetic chain hip-strengthening exercises), 6 weeks (n = 40, age: 41 (SD 37.45)) | Pain intensity: VAS (0–100) Disability: ODI (0–50) Strength: Force dynamometer Follow-up: 6 weeks (short-term) |
| Khayambashi et al. (2012) [31] | Patients with patellofemoral pain (PFP) Location: Iran | N = 28 Age 29.7 (SD 5.3) Gender M: 0 F: 28 | Exp1 = hip strengthening (exercises to strengthen hip external rotator muscles) 3x/week, 30 min/session, over 8 weeks (n = 14, age: 28.9 (SD 5.8)) Con = no intervention (n = 14, age 30.5 (SD 4.8)) | Pain intensity: VAS (0–10) Disability: WOMAC (0–100) Strength: Handheld isometric dynamometer Follow-up: 8 weeks (short-term) |
| Lee and Kim (2015) [36] | Patients with low back pain Location: Iran | N = 33 Age 60.46 (SD 14.4) Gender: S/N | Exp = hip strengthening + lumbar strengthening (exercises to strengthen hip, including flexion, extension, abduction, adduction, internal rotation, and external rotation) 3x/week, 20 min/session, over 6 weeks (n = 22, age:61.0 (SD 13.2)) Con = lumbar strengthening (exercises for lumbar stabilization) 3x/week, 20 min/session, over 6 weeks (n = 11, age:59.38 (SD 17.3)) | Pain intensity: VAS (0–100) Disability: ODI (0–50) Follow-up: 3 weeks (short-term) |
| Saad et al. (2018) [32] | Patients with patellofemoral pain (PFP) Location: Brazil | N = 20 Age 22.85 (SD 1.1) Gender M: 0 F: 20 | Exp2 = hip strengthening (exercises to strengthen hip-stabilizing muscles) 2x/week, 50 min/session, over 8 weeks (n = 10, age: 22.5 (SD 1.08)) Con = no intervention (n = 10, age 23.2 (SD 1.03)) | Pain intensity: VAS (0–10) Disability: AKPS (0–100) Strength: Handheld isometric dynamometer Follow-up: 8 weeks (short-term) |
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bade et al. (2017) [33] | Yes | No | Yes | No | No | No | Yes | No | Yes | Yes | 5 |
| Burns et al. (2021) [38] | Yes | Yes | No | No | No | No | No | Yes | Yes | Yes | 5 |
| Fukuda et al. (2021) [37] | Yes | Yes | Yes | No | No | No | Yes | Yes | Yes | Yes | 7 |
| Fukuda et al. (2010) [30] | Yes | Yes | Yes | No | Yes | Yes | Yes | No | Yes | Yes | 8 |
| Jeong et al. (2015) [34] | Yes | No | No | No | No | No | Yes | No | Yes | Yes | 4 |
| Kendall et al. (2014) [35] | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | 9 |
| Khayambashi et al. (2012) [31] | Yes | Yes | No | No | No | No | Yes | No | Yes | Yes | 5 |
| Lee and Kim (2015) [36] | Yes | No | Yes | No | No | No | Yes | No | Yes | Yes | 5 |
| Saad et al. (2018) [32] | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | 9 |
| Total, n (%) | 9 (100) | 6 (66.6) | 6 (66.6) | 9 (100) | 3 (33.3) | 3 (33.3) | 8 (88.8) | 4 (44.4) | 9 (100) | 9 (100) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de F. Silva, A.; Maia, L.B.; Mendonça, V.A.; dos Santos, J.M.; Coelho-Oliveira, A.C.; Santos, J.N.V.; Moreira, L.L.V.; Mascarenhas, R.d.O.; Gonçalves, G.T.; Oliveira, V.C.; et al. Efficacy of Hip Strengthening on Pain Intensity, Disability, and Strength in Musculoskeletal Conditions of the Trunk and Lower Limbs: A Systematic Review with Meta-Analysis and Grade Recommendations. Diagnostics 2022, 12, 2910. https://doi.org/10.3390/diagnostics12122910
de F. Silva A, Maia LB, Mendonça VA, dos Santos JM, Coelho-Oliveira AC, Santos JNV, Moreira LLV, Mascarenhas RdO, Gonçalves GT, Oliveira VC, et al. Efficacy of Hip Strengthening on Pain Intensity, Disability, and Strength in Musculoskeletal Conditions of the Trunk and Lower Limbs: A Systematic Review with Meta-Analysis and Grade Recommendations. Diagnostics. 2022; 12(12):2910. https://doi.org/10.3390/diagnostics12122910
Chicago/Turabian Stylede F. Silva, Angélica, Laísa B. Maia, Vanessa A. Mendonça, Jousielle M. dos Santos, Ana C. Coelho-Oliveira, Joyce N. V. Santos, Leticia L. V. Moreira, Rodrigo de O. Mascarenhas, Gabriele T. Gonçalves, Vinícius C. Oliveira, and et al. 2022. "Efficacy of Hip Strengthening on Pain Intensity, Disability, and Strength in Musculoskeletal Conditions of the Trunk and Lower Limbs: A Systematic Review with Meta-Analysis and Grade Recommendations" Diagnostics 12, no. 12: 2910. https://doi.org/10.3390/diagnostics12122910
APA Stylede F. Silva, A., Maia, L. B., Mendonça, V. A., dos Santos, J. M., Coelho-Oliveira, A. C., Santos, J. N. V., Moreira, L. L. V., Mascarenhas, R. d. O., Gonçalves, G. T., Oliveira, V. C., Teixeira, L. A. C., Rapin, A., Lacerda, A. C. R., & Taiar, R. (2022). Efficacy of Hip Strengthening on Pain Intensity, Disability, and Strength in Musculoskeletal Conditions of the Trunk and Lower Limbs: A Systematic Review with Meta-Analysis and Grade Recommendations. Diagnostics, 12(12), 2910. https://doi.org/10.3390/diagnostics12122910








