Classification of Vascular Hotspots and Micro-Vessel Flow Velocity Waveforms in Low-Grade Squamous Intraepithelial Lesions and HPV Condyloma of the Cervix
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Population
2.2. Transvaginal Ultrasound with Power Doppler Angiography (TV-PDA)
2.3. Measurement of Blood Flow Velocity Waveforms within the Uterine Cervix
2.4. Statistical Analysis
3. Results
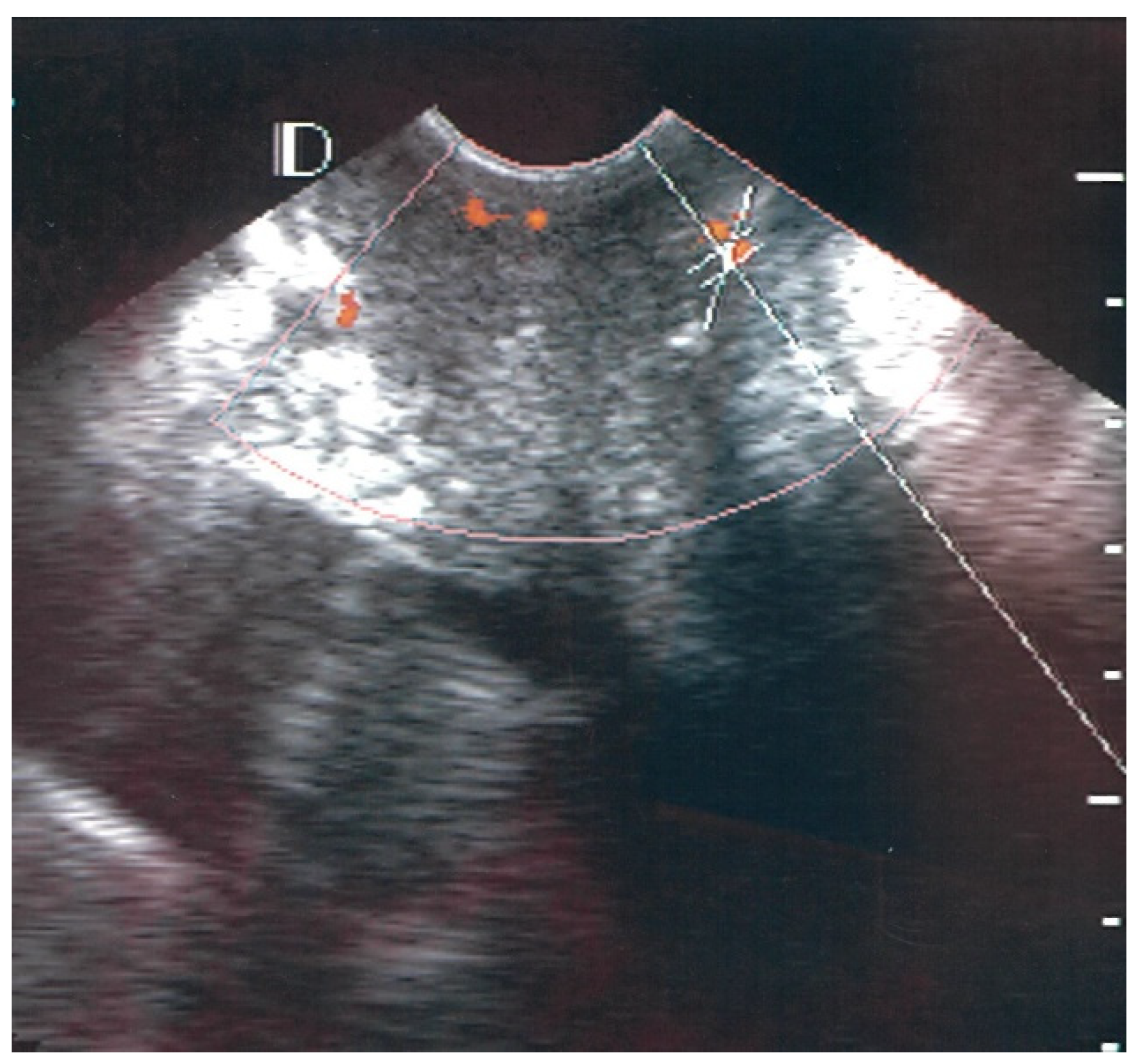
3.1. Visual Classification of Vascularity Findings on TV-PDU
3.2. Micro-Vessel Flow Velocity Waveform Findings from TV-PDU
3.3. Optimal Cutoff Values for the Six Sonographic Parameters for HPV Condyloma, LSIL (CIN I), and HPV Infection
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McBride, A.A. Human papillomaviruses: Diversity, infection and host interactions. Nat. Rev. Microbiol. 2022, 20, 95–108. [Google Scholar] [CrossRef] [PubMed]
- Haręża, D.A.; Wilczyński, J.R.; Paradowska, E. Human Papillomaviruses as Infectious Agents in Gynecological Cancers. Oncogenic Properties of Viral Proteins. Int. J. Mol. Sci. 2022, 23, 1818. [Google Scholar] [CrossRef] [PubMed]
- Luvero, D.; Lopez, S.; Bogani, G.; Raspagliesi, F.; Angioli, R. From the Infection to the Immunotherapy in Cervical Cancer: Can We Stop the Natural Course of the Disease? Vaccines 2020, 8, 597. [Google Scholar] [CrossRef] [PubMed]
- Warner, Z.C.; Reid, B.; Auguste, P.; Joseph, W.; Kepka, D.; Warner, E.L. Awareness and Knowledge of HPV, HPV Vaccination, and Cervical Cancer among an Indigenous Caribbean Community. Int. J. Environ. Res. Public. Health 2022, 19, 5694. [Google Scholar] [CrossRef]
- Jalilvand, S.; Saidi, M.; Shoja, Z.; Ghavami, N.; Hamkar, R. The prevalence of human papillomavirus infection in Iranian patients with sinonasal inverted papilloma. J. Chin. Med. Assoc. 2016, 79, 137–140. [Google Scholar] [CrossRef]
- Damkjær, M.; Laursen, J.B.; Petersen, L.K.; Schledermann, D.; Booth, B.B.; Dolleris, B.B.; Laursen, H.S.; Schroll, J. Endocervical sampling in women with suspected cervical neoplasia: A systematic review and meta-analysis of diagnostic test accuracy studies. Am. J. Obstet. Gynecol. 2022. Epub ahead of print. [Google Scholar] [CrossRef]
- Alrajjal, A.; Pansare, V.; Choudhury, M.S.R.; Khan, M.Y.A.; Shidham, V.B. Squamous intraepithelial lesions (SIL: LSIL, HSIL, ASCUS, ASC-H, LSIL-H) of Uterine Cervix and Bethesda System. Cytojournal 2021, 18, 16. [Google Scholar] [CrossRef]
- Chuai, Y.; Rizzuto, I.; Zhang, X.; Li, Y.; Dai, G.; Otter, S.J.; Bharathan, R.; Stewart, A.; Wang, A. Vascular endothelial growth factor (VEGF) targeting therapy for persistent, recurrent, or metastatic cervical cancer. Cochrane Database Syst. Rev. 2021, 3, CD013348. [Google Scholar]
- Fleischmann, M.; Chatzikonstantinou, G.; Fokas, E.; Wichmann, J.; Christiansen, H.; Strebhardt, K.; Rödel, C.; Tselis, N.; Rödel, F. Molecular Markers to Predict Prognosis and Treatment Response in Uterine Cervical Cancer. Cancers 2021, 13, 5748. [Google Scholar] [CrossRef]
- Dogan, O.; Pulatoglu, C.; Basbug, A.; Kaya, A.E.; Yassa, M. Discriminating performance of early uterine and cervical artery pulsatility and resistivity in pre-invasive cervical lesions. Med. Bull. Sisli. Etfal. Hosp. 2018, 52, 206–211. [Google Scholar]
- Alcazar, J.L. Transvaginal color Doppler in the assessment of cervical carcinoma. Cancer Ther. 2005, 3, 139–146. [Google Scholar]
- Jurado, M.; Galvan, R.; Martinez-Monge, R.; Mazaira, J.; Alcazar, J.L. Neoangiogenesis in early cervical cancer: Correlation between color Doppler findings and risk factors. A prospective observational study. World J. Surg. Oncol. 2008, 6, 126. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.C.; Yuan, C.C.; Hung, J.H.; Chao, K.C.; Yen, M.S.; Ng, H.T. Power Doppler angiographic appearance and blood flow velocity waveforms in invasive cervical carcinoma. Gynecol. Oncol. 2000, 79, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.C.; Yang, H.J.; Yuan, C.C.; Chao, K.C. Visual grading system, blood flow index, and tumor marker SCC antigen as prognostic factors in invasive cervical carcinoma. J. Med. Ultrasound 2006, 14, 25–31. [Google Scholar] [CrossRef]
- Liu, C.H.; Kung, Y.H.; Chien-Fu Lin, J.; Chuang, C.M.; Wu, H.H.; Jiang, L.Y.; Shih, Y.C.; Wang, P.H.; Chen, Y.J. Synergistic therapeutic effect of low-dose bevacizumab with cisplatin-based chemotherapy for advanced or recurrent cervical cancer. J. Chin. Med. Assoc. 2021, 84, 1139–1144. [Google Scholar] [CrossRef]
- Okunade, K.S. Human papillomavirus and cervical cancer. J. Obstet. Gynaecol. 2020, 40, 602–608. [Google Scholar] [CrossRef]
- Stuebs, F.A.; Koch, M.C.; Dietl, A.K.; Adler, W.; Geppert, C.; Hartmann, A.; Knöll, A.; Beckmann, M.W.; Mehlhorn, G.; Schulmeyer, C.E.; et al. Cytology and High-Risk Human Papillomavirus Test for Cervical Cancer Screening Assessment. Diagnostics 2022, 12, 1748. [Google Scholar] [CrossRef]
- Ozbay, K.; Deveci, S. Relationships between transvaginal color Doppler findings, infectious parameters analogue scale scores in patients with mild acute pelvic inflammatory disease. Eur. J. Obstet. Gynecol. Reprod. Biol. 2010, 156, 105–108. [Google Scholar] [CrossRef]
- Alatas, C.; Aksoy, E.; Akarsu, C.; Yakin, K.; Bahceci, M. Hemodynamic assessment in pelvic inflammatory disease by transvaginal color Doppler ultrasonography. Eur. J. Obstet. Gynecol. Reprod. Biol. 1996, 70, 75–78. [Google Scholar] [CrossRef]
- Tinkanen, H. Doppler ultrasound findings in female infertility. With special reference to pelvic inflammatory disease and endocrinological factors. Acta Obstet. Gynecol. Scand. 1995, 74, 762–763. [Google Scholar] [CrossRef]
- Belitsos, P.; Papoutsis, D.; Rodolakis, A.; Mesogitis, S.; Antsaklis, A. Three-dimensional power Doppler ultrasound for the study of cervical cancer and precancerous lesions. Ultrasound Obstet. Gynecol. 2012, 40, 576–581. [Google Scholar] [CrossRef]
- Testa, A.C.; Ferrandina, G.; Distefano, M.; Fruscella, E.; Mansueto, D.; Basso, D.; Salutari, V.; Scambia, G. Color Doppler velocimetry and three-dimensional color power angiography of cervical carcinoma. Ultrasound Obstet. Gynecol. 2004, 24, 445–452. [Google Scholar] [CrossRef] [PubMed]
- Alcazar, J.L. Three-dimensional power Doppler-derived vascular indices: What are we measuring, and how are we doing it? Ultrasound Obstet. Gynecol. 2008, 32, 485–487. [Google Scholar] [CrossRef] [PubMed]
- Raine-Fenning, N.J.; Campbell, B.K.; Clewes, J.S.; Kendall, N.R.; Johnson, I.R. The reliability of virtual organ computer-aided analysis (VOCAL) for the semi-quantification of ovarian, endometrial, and sub-endometrial perfusion. Ultrasound Obstet. Gynecol. 2003, 22, 633–639. [Google Scholar] [CrossRef]
- Hsu, K.F.; Su, J.M.; Huang, S.C.; Cheng, Y.M.; Kang, C.Y.; Shen, M.R.; Chang, F.M.; Chou, C.Y. Three-dimensional power Doppler imaging of early-stage cervical cancer. Ultrasound Obstet. Gynecol. 2004, 24, 664–671. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, K.; Umesaki, N. Impact of three-dimensional (3D) ultrasonography and power Doppler angiography in the management of cervical cancer. Eur. J. Gynaecol. Oncol. 2010, 31, 10–17. [Google Scholar]
- Alcazar, J.L.; Jurado, M.; Lopez-Garcia, G. Tumor vascularization in cervical cancer by 3-dimensional power Doppler angiography: Correlation with tumor characteristics. Int. J. Gynecol. Cancer 2010, 20, 393–397. [Google Scholar] [CrossRef]
- Dubiel, M.; Hammid, A.; Breborowicz, A.; Pietryga, M.; Sladkevicius, P.; Olofsson, P.A.; Breborowicz, G.H.; Gudmundsson, S. Flow index evaluation of 3-D volume flow images: An in vivo and in vitro study. Ultrasound. Med. Biol. 2006, 32, 665–671. [Google Scholar] [CrossRef]
- Hsieh, C.Y.; Wu, C.C.; Chen, T.M.; Chen, C.A.; Chen, C.L.; Wang, J.F.; Chang, C.F.; Hsieh, F.J. Clinical significance of intratumoral blood flow in cervical carcinoma assessed by color Doppler ultrasound. Cancer 1995, 75, 2518–2522. [Google Scholar] [CrossRef]
- Schulten-Wijman, M.J.; Struijk, P.C.; Brezinka, C.; De Jong, N.; Steegers, E.A. Evaluation of volume vascularization index and flow index: A phantom study. Ultrasound Obstet. Gynecol. 2008, 32, 560–564. [Google Scholar] [CrossRef]
- Wu, Y.C.; Chen, C.H.; Ko, Y.L.; Huang, J.Y.; Yuan, C.C.; Wang, P.H.; Hsiao, C.H.; Chu, W.C. Cervical Power Doppler Angiography with Micro Vessel Blood Flow Indices in the Auxiliary Diagnosis of Acute Cervicitis. Diagnostics 2022, 12, 1131. [Google Scholar] [CrossRef] [PubMed]
- Feltovich, H.; Carlson, L. New techniques in evaluation of the cervix. Semin. Perinatol. 2017, 41, 477–484. [Google Scholar] [CrossRef] [PubMed]





| Vascular Classification | |||||
|---|---|---|---|---|---|
| Number | Class 0 | Class I | Class II | Class III | |
| LSIL | 26 | 0 | 18 | 7 | 1 |
| HPV condyloma | 13 | 0 | 12 | 1 | 0 |
| Normal | 40 | 29 | 10 | 1 | 0 |
| Classification | Numbers of Visualize Vascular Hotspots within Cervix (One Spot: 1 × 1 mm) |
|---|---|
| Class 0 | 0 |
| Class I | 1 to 5 |
| Class II | 5 to 10 |
| Class III | >10 |
| (A) HPV Condyloma (n = 13) vs. Control Group (n = 40) | ||||||||
| Variable | Area | Optimal | Sensitivity | 95%LCL | 95%UCL | Specificity | 95%LCL | 95%UCL |
| PI | 0.89 | 1.07 | 84.6 | 54.6 | 98.1 | 85 | 70.2 | 94.3 |
| RI | 0.79 | 0.62 | 69.2 | 38.6 | 90.9 | 85 | 70.2 | 94.3 |
| PS | 0.73 | 7.68 | 69.2 | 38.6 | 90.9 | 80 | 64.4 | 90.9 |
| ED | 0.55 | 3.52 | 84.6 | 54.6 | 98.1 | 32.5 | 18.6 | 49.1 |
| TAMV | 0.65 | 5.34 | 76.9 | 46.2 | 94.9 | 52.5 | 36.1 | 68.4 |
| VI | 0.76 | 2.57 | 69.2 | 38.6 | 90.9 | 85 | 70.2 | 94.3 |
| (B) LSIL (CIN I) of the Cervix (n = 26) vs. Control Group (n = 40) | ||||||||
| Variable | Area | Optimal | Sensitivity | 95%LCL | 95%UCL | Specificity | 95%LCL | 95%UCL |
| PI | 0.94 | 1.08 | 100 | 86.7 | 100 | 85 | 70.2 | 94.3 |
| RI | 0.84 | 0.65 | 88.5 | 69.8 | 97.6 | 72.5 | 58.8 | 87.3 |
| PS | 0.67 | 7.1 | 42.3 | 23.4 | 63.1 | 90 | 76.3 | 97.2 |
| ED | 0.52 | 2.3 | 23.1 | 8.9 | 43.6 | 87.5 | 73.2 | 95.8 |
| TAMV | 0.6 | 4.48 | 42.3 | 23.4 | 63.1 | 82.5 | 67.2 | 92.7 |
| VI | 0.83 | 2.86 | 92.3 | 74.9 | 99.1 | 67.5 | 50.9 | 81.4 |
| (C) HPV Infection (n = 39) vs. Control Group (n = 40) | ||||||||
| Variables | Area | Optimal | Sensitivity | 95%LCL | 95%UCL | Specificity | 95%LCL | 95%UCL |
| PI | 0.92 | 1.08 | 94.9 | 82.7 | 99.4 | 85 | 70.2 | 94.3 |
| RI | 0.81 | 0.65 | 84.6 | 69.5 | 94.1 | 72.5 | 58.8 | 87.3 |
| PS | 0.68 | 7.68 | 51.3 | 34.8 | 67.6 | 80 | 64.4 | 90.9 |
| ED | 0.52 | 2.33 | 23.1 | 11.1 | 39.3 | 87.5 | 73.2 | 95.8 |
| TAMV | 0.6 | 4.5 | 43.6 | 27.8 | 60.4 | 80 | 64.4 | 90.9 |
| VI | 0.79 | 2.82 | 84.6 | 69.5 | 94.1 | 70 | 63.5 | 83.4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, Y.-C.; Chen, C.-H.; Ko, Y.-L.; Yuan, C.-C.; Wang, P.-H.; Chu, W.-C. Classification of Vascular Hotspots and Micro-Vessel Flow Velocity Waveforms in Low-Grade Squamous Intraepithelial Lesions and HPV Condyloma of the Cervix. Diagnostics 2022, 12, 2390. https://doi.org/10.3390/diagnostics12102390
Wu Y-C, Chen C-H, Ko Y-L, Yuan C-C, Wang P-H, Chu W-C. Classification of Vascular Hotspots and Micro-Vessel Flow Velocity Waveforms in Low-Grade Squamous Intraepithelial Lesions and HPV Condyloma of the Cervix. Diagnostics. 2022; 12(10):2390. https://doi.org/10.3390/diagnostics12102390
Chicago/Turabian StyleWu, Yi-Cheng, Ching-Hsuan Chen, Yi-Li Ko, Chiou-Chung Yuan, Peng-Hui Wang, and Woei-Chyn Chu. 2022. "Classification of Vascular Hotspots and Micro-Vessel Flow Velocity Waveforms in Low-Grade Squamous Intraepithelial Lesions and HPV Condyloma of the Cervix" Diagnostics 12, no. 10: 2390. https://doi.org/10.3390/diagnostics12102390
APA StyleWu, Y.-C., Chen, C.-H., Ko, Y.-L., Yuan, C.-C., Wang, P.-H., & Chu, W.-C. (2022). Classification of Vascular Hotspots and Micro-Vessel Flow Velocity Waveforms in Low-Grade Squamous Intraepithelial Lesions and HPV Condyloma of the Cervix. Diagnostics, 12(10), 2390. https://doi.org/10.3390/diagnostics12102390








