A New Angle Measurement in Translabial Ultrasound as an Adjunct for the Diagnosis of Pelvic Organ Prolapse
Abstract
:1. Introduction
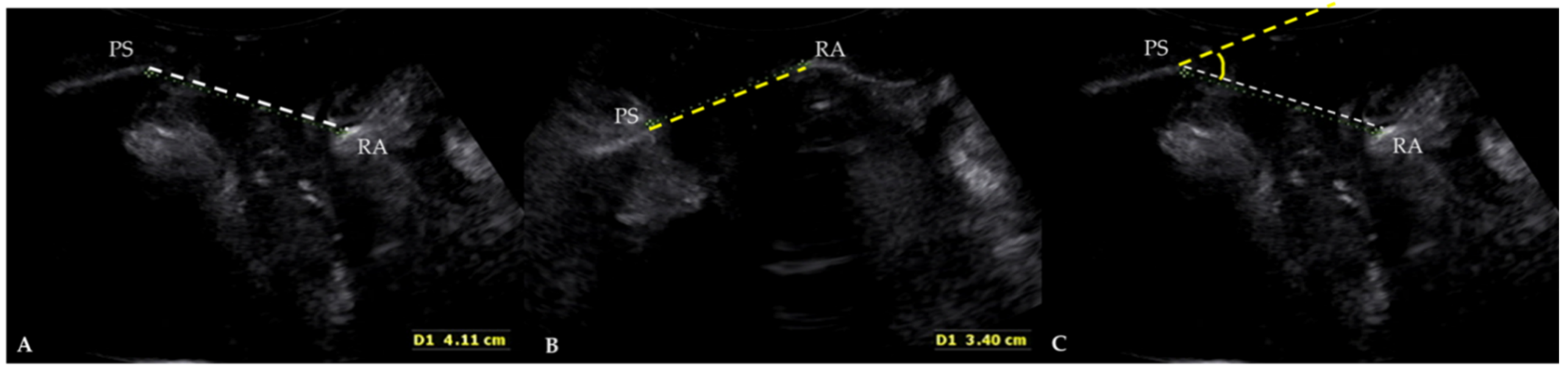
2. Materials and Methods
2.1. Study Design and Patients
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barber, M.D. Pelvic organ prolapse. BMJ 2016, 354, i3853. [Google Scholar] [CrossRef]
- Bump, R.C.; Mattiasson, A.; Bø, K.; Brubaker, L.P.; DeLancey, J.O.; Klarskov, P.; Shull, B.L.; Smith, A.R. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am. J. Obstet. Gynecol. 1996, 175, 10–17. [Google Scholar] [CrossRef]
- Nam, G.; Lee, S.-R.; Kim, S.-H.; Chae, H.-D. Importance of Translabial Ultrasound for the Diagnosis of Pelvic Organ Prolapse and Its Correlation with the POP-Q Examination: Analysis of 363 Cases. J. Clin. Med. 2021, 10, 4267. [Google Scholar] [CrossRef] [PubMed]
- Nam, G.; Lee, S.R.; Eum, H.R.; Kim, S.H.; Chae, H.D.; Kim, G.J. A Huge Hemorrhagic Epidermoid Cyst of the Perineum with Hypoechoic Semisolid Ultrasonographic Feature Mimicking Scar Endometriosis. Medicina 2021, 57, 276. [Google Scholar] [CrossRef] [PubMed]
- Nam, G.; Lee, S.R.; Choi, S. Clitoromegaly, Vulvovaginal Hemangioma Mimicking Pelvic Organ Prolapse, and Heavy Menstrual Bleeding: Gynecologic Manifestations of Klippel-Trénaunay Syndrome. Medicina 2021, 57, 366. [Google Scholar] [CrossRef]
- Lee, S.R.; Lim, Y.-M.; Jeon, J.H.; Park, M.H. Diagnosis of urethral diverticulum mimicking pelvic organ prolapse with translabial ultrasonography. Am. J. Obstet. Gynecol. 2017, 217, 482. [Google Scholar] [CrossRef]
- van Gruting, I.M.; Stankiewicz, A.; Kluivers, K.; De Bin, R.; Blake, H.; Sultan, A.H.; Thakar, R. Accuracy of four imaging techniques for diagnosis of posterior pelvic floor disorders. Obstet. Gynecol. 2017, 130, 1017–1024. [Google Scholar] [CrossRef] [PubMed]
- Mahieu, P.; Pringot, J.; Bodart, P. Defecography: I. Description of a new procedure and results in normal patients. Gastrointest. Radiol. 1984, 9, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Dvorkin, L.; Hetzer, F.; Scott, S.M.; Williams, N.; Gedroyc, W.; Lunniss, P. Open-magnet MR defaecography compared with evacuation proctography in the diagnosis and management of patients with rectal intussusception. Colorectal Dis. 2004, 6, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Perniola, G.; Shek, C.; Chong, C.; Chew, S.; Cartmill, J.; Dietz, H. Defecation proctography and translabial ultrasound in the investigation of defecatory disorders. Ultrasound Obstet. Gynecol. 2008, 31, 567–571. [Google Scholar] [CrossRef]
- Steensma, A.B.; Oom, D.M.; Burger, C.W.; Schouten, W.R. Assessment of posterior compartment prolapse: A comparison of evacuation proctography and 3D transperineal ultrasound. Colorectal Dis. 2010, 12, 533–539. [Google Scholar] [CrossRef] [PubMed]
- Martellucci, J.; Naldini, G. Clinical relevance of transperineal ultrasound compared with evacuation proctography for the evaluation of patients with obstructed defaecation. Colorectal Dis. 2011, 13, 1167–1172. [Google Scholar] [CrossRef] [PubMed]
- Weemhoff, M.; Kluivers, K.; Govaert, B.; Evers, J.; Kessels, A.; Baeten, C. Transperineal ultrasound compared to evacuation proctography for diagnosing enteroceles and intussusceptions. Int. J. Colorectal Dis. 2013, 28, 359–363. [Google Scholar] [CrossRef] [PubMed]
- Beer-Gabel, M.; Carter, D. Comparison of dynamic transperineal ultrasound and defecography for the evaluation of pelvic floor disorders. Int. J. Colorectal Dis. 2015, 30, 835–841. [Google Scholar] [CrossRef] [PubMed]
- Foti, P.; Farina, R.; Riva, G.; Coronella, M.; Fisichella, E.; Palmucci, S.; Racalbuto, A.; Politi, G.; Ettorre, G. Pelvic floor imaging: Comparison between magnetic resonance imaging and conventional defecography in studying outlet obstruction syndrome. La Radiol. Med. 2013, 118, 23–39. [Google Scholar] [CrossRef]
- Shorvon, P.; McHugh, S.; Diamant, N.; Somers, S.; Stevenson, G. Defecography in normal volunteers: Results and implications. Gut 1989, 30, 1737–1749. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Freimanis, M.G.; Wald, A.; Caruana, B.; Bauman, D.H. Evacuation proctography in normal volunteers. Investig. Radiol. 1991, 26, 581–585. [Google Scholar] [CrossRef] [PubMed]
- Müller-Lissner, S.; Bartolo, D.; Christiansen, J.; Ekberg, O.; Goei, R.; Höpfner, W.; Infantino, A.; Kuijpers, H.; Selvaggi, F.; Wald, A. Interobserver agreement in defecography—An international study. Z. Fur Gastroenterol. 1998, 36, 273–279. [Google Scholar]
- Dietz, H.; Haylen, B.; Broome, J. Ultrasound in the quantification of female pelvic organ prolapse. Ultrasound Obstet. Gynecol. Off. J. Int. Soc. Ultrasound Obstet. Gynecol. 2001, 18, 511–514. [Google Scholar] [CrossRef]
- Dietz, H.P.; Steensma, A.B. Posterior compartment prolapse on two-dimensional and three-dimensional pelvic floor ultrasound: The distinction between true rectocele, perineal hypermobility and enterocele. Ultrasound Obstet. Gynecol. 2005, 26, 73–77. [Google Scholar] [CrossRef]
- Dietz, H. Ultrasound imaging of the pelvic floor. Part I: Two-dimensional aspects. Ultrasound Obstet. Gynecol. 2004, 23, 80–92. [Google Scholar] [CrossRef]
- Beer-Gabel, M.; Teshler, M.; Schechtman, E.; Zbar, A. Dynamic transperineal ultrasound vs. defecography in patients with evacuatory difficulty: A pilot study. Int. J. Colorectal Dis. 2004, 19, 60–67. [Google Scholar] [CrossRef] [PubMed]
- van Gruting, I.M.; Stankiewicz, A.; Thakar, R.; Santoro, G.A.; IntHout, J.; Sultan, A.H. Imaging modalities for the detection of posterior pelvic floor disorders in women with obstructed defaecation syndrome. Cochrane Database Syst. Rev. 2021, 9, CD011482. [Google Scholar] [PubMed]
- Dietz, H.; Brown, B.; Friedman, T.; Subramaniam, N. Does the presence of a true radiological rectocele increase the likelihood of symptoms of prolapse? Int. Urogynecol. J. 2020, 32, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Dietz, H.; Beer-Gabel, M. Ultrasound in the investigation of posterior compartment vaginal prolapse and obstructed defecation. Ultrasound Obstet. Gynecol. 2012, 40, 14–27. [Google Scholar] [CrossRef] [PubMed]
- van Gruting, I.; Kluivers, K.; Sultan, A.; De Bin, R.; Stankiewicz, A.; Blake, H.; Thakar, R. Does 4D transperineal ultrasound have additional value over 2D transperineal ultrasound for diagnosing posterior pelvic floor disorders in women with obstructed defecation syndrome? Ultrasound Obstet. Gynecol. 2018, 52, 784–791. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tan, C.; Geng, J.; Tang, J.; Yang, X. The relationship between obstructed defecation and true rectocele in patients with pelvic organ prolapse. Sci. Rep. 2020, 10, 1–6. [Google Scholar] [CrossRef]
- Hainsworth, A.; Solanki, D.; Hamad, A.; Morris, S.; Schizas, A.; Williams, A. Integrated total pelvic floor ultrasound in pelvic floor defaecatory dysfunction. Colorectal Dis. 2017, 19, O54–O65. [Google Scholar] [CrossRef] [PubMed]
- Samantray, S.R.; Mohapatra, I. Study of the Relationship Between Pelvic Organ Prolapse Quantification (POP-Q) Staging and Decubitus Ulcer in Pelvic Organ Prolapse. Cureus 2021, 13, e12443. [Google Scholar] [CrossRef]
- Braga, A.; Soave, I.; Caccia, G.; Regusci, L.; Ruggeri, G.; Pitaku, I.; Bassi, V.; Papadia, A.; Serati, M. What is this vaginal bulge? An atypical case of vaginal paraurethral leiomyoma. A case report and literature systematic review. J. Gynecol. Obstet. Hum. Reprod. 2020, 50, 101822. [Google Scholar] [CrossRef]
- Vitale, S.G.; Lagana, A.S.; Gulino, F.A.; Tropea, A.; Tarda, S. Prosthetic surgery versus native tissue repair of cystocele: Literature review. Updates Surg. 2016, 68, 325–329. [Google Scholar] [CrossRef] [PubMed]
- Altman, D.; Väyrynen, T.; Engh, M.E.; Axelsen, S.; Falconer, C. Anterior colporrhaphy versus transvaginal mesh for pelvic-organ prolapse. N. Engl. J. Med. 2011, 364, 1826–1836. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| POP-Q Points (n = 452) | Mean ± SD | Range |
|---|---|---|
| Aa | 0.94 ± 2.04 | −3 to 3 |
| Ba | 2.86 ± 2.52 | −3 to 10 |
| C | 0.41 ± 4.07 | −9 to 10 |
| Ap | −1.51 ± 2.65 | −3 to 3 |
| Bp | 0.15 ± 3.02 | −3 to 10 |
| Gh | 5.15 ± 1.38 | 3.5 to 8 |
| Pb | 3.46 ± 1.20 | 3 to 9 |
| Parameter (n = 452) | Mean ± SD | Range |
|---|---|---|
| Angle difference (°) † | 17.56 ± 10.70 | −18.14 to 74.79 |
| POP-Q Coordinate | Correlation Coefficient for Angle | p-Value |
|---|---|---|
| Aa | −0.11 † | 0.02 |
| Ba | −0.18 † | 0.00 |
| C | −0.14 † | 0.00 |
| Ap | 0.17 † | 0.00 |
| Bp | −0.001 † | 0.98 |
| Gh | −0.02 † | 0.68 |
| Pb | −0.07 † | 0.12 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nam, G.; Song, J.-Y.; Lee, S.-R. A New Angle Measurement in Translabial Ultrasound as an Adjunct for the Diagnosis of Pelvic Organ Prolapse. Diagnostics 2022, 12, 98. https://doi.org/10.3390/diagnostics12010098
Nam G, Song J-Y, Lee S-R. A New Angle Measurement in Translabial Ultrasound as an Adjunct for the Diagnosis of Pelvic Organ Prolapse. Diagnostics. 2022; 12(1):98. https://doi.org/10.3390/diagnostics12010098
Chicago/Turabian StyleNam, Gina, Jae-Yen Song, and Sa-Ra Lee. 2022. "A New Angle Measurement in Translabial Ultrasound as an Adjunct for the Diagnosis of Pelvic Organ Prolapse" Diagnostics 12, no. 1: 98. https://doi.org/10.3390/diagnostics12010098
APA StyleNam, G., Song, J.-Y., & Lee, S.-R. (2022). A New Angle Measurement in Translabial Ultrasound as an Adjunct for the Diagnosis of Pelvic Organ Prolapse. Diagnostics, 12(1), 98. https://doi.org/10.3390/diagnostics12010098






