Masseter Muscle Thickness Measured by Ultrasound as a Possible Link with Sarcopenia, Malnutrition and Dependence in Nursing Homes
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Recruitment
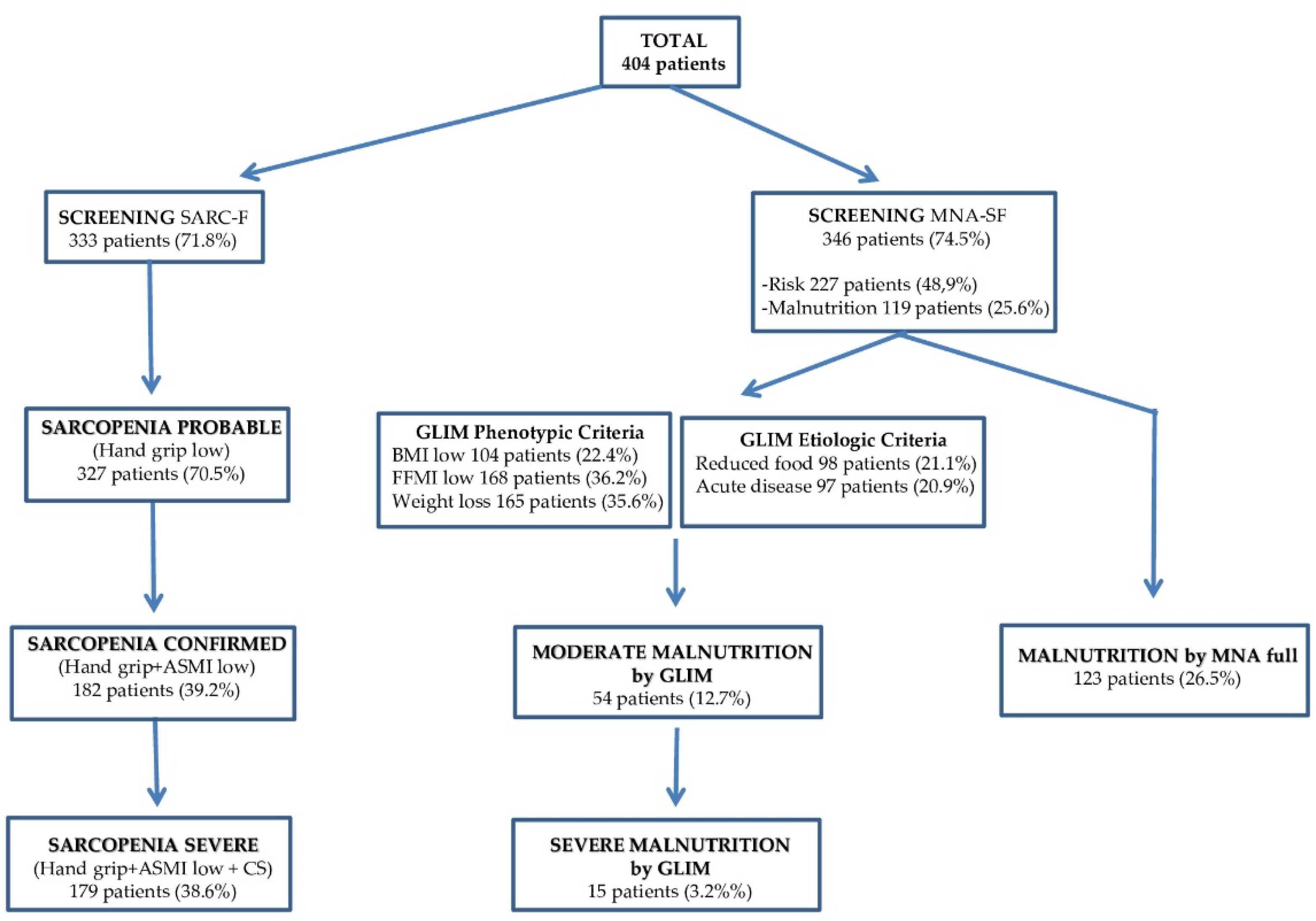
2.2. Sarcopenia Assessment
2.3. Nutritional Assessment
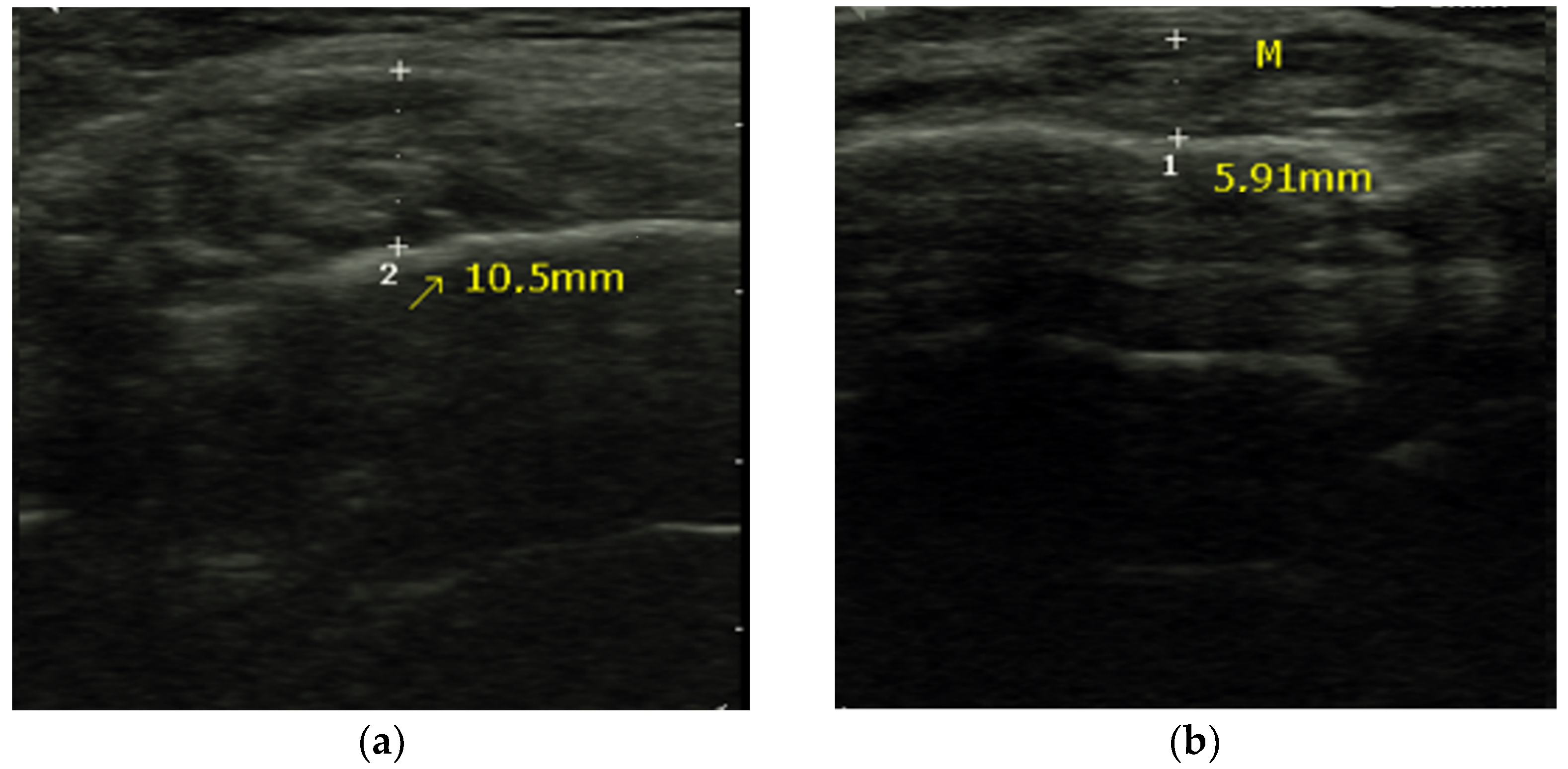
2.4. Masseter Muscle Thickness Measurement
2.5. Meal Forms Assessment
2.6. Functional Ability Assessment
2.7. Statistical Analysis
2.8. Ethical Aspects
3. Results
3.1. Basic Characteristics
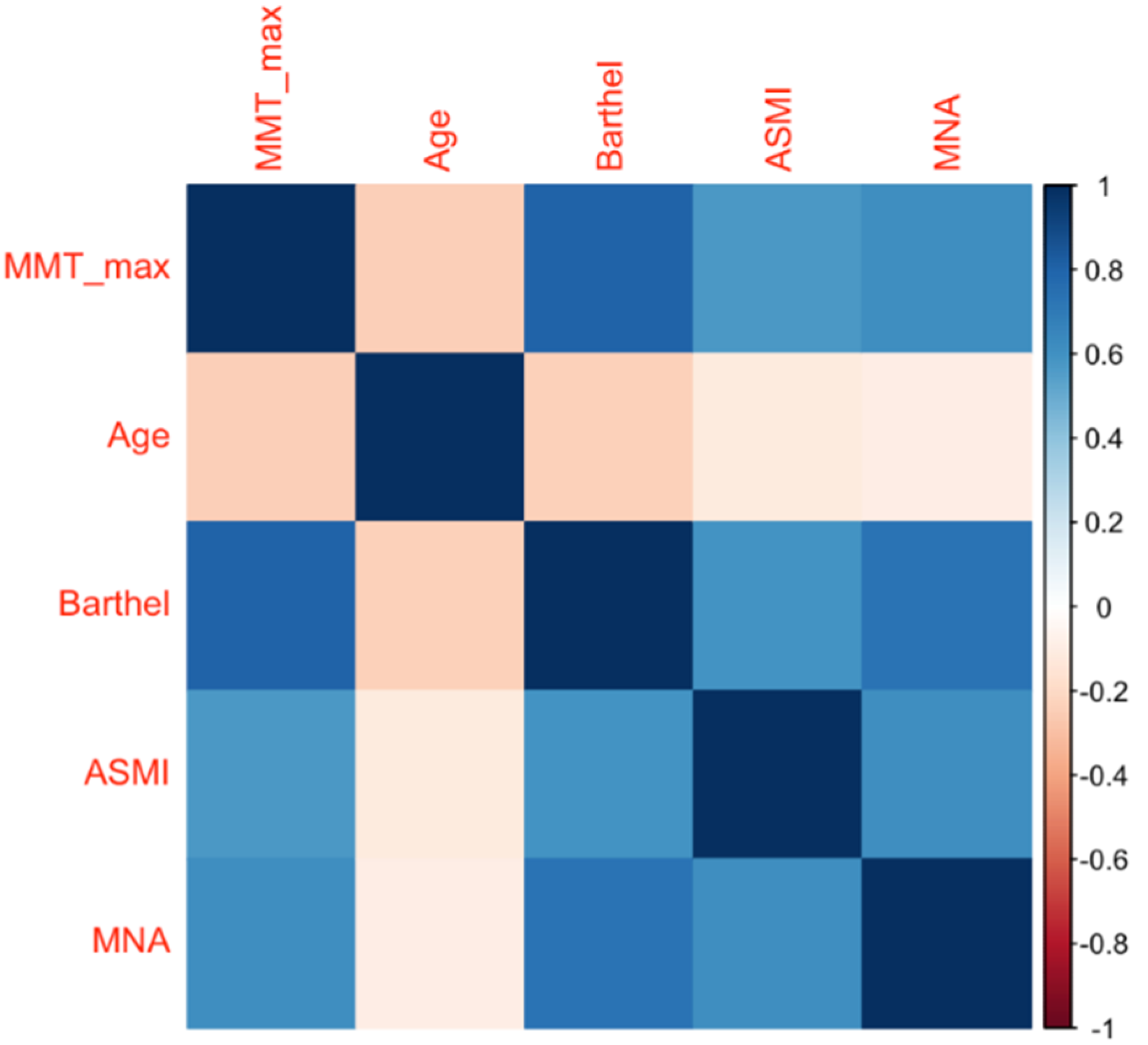
3.2. Factors Related to MMT
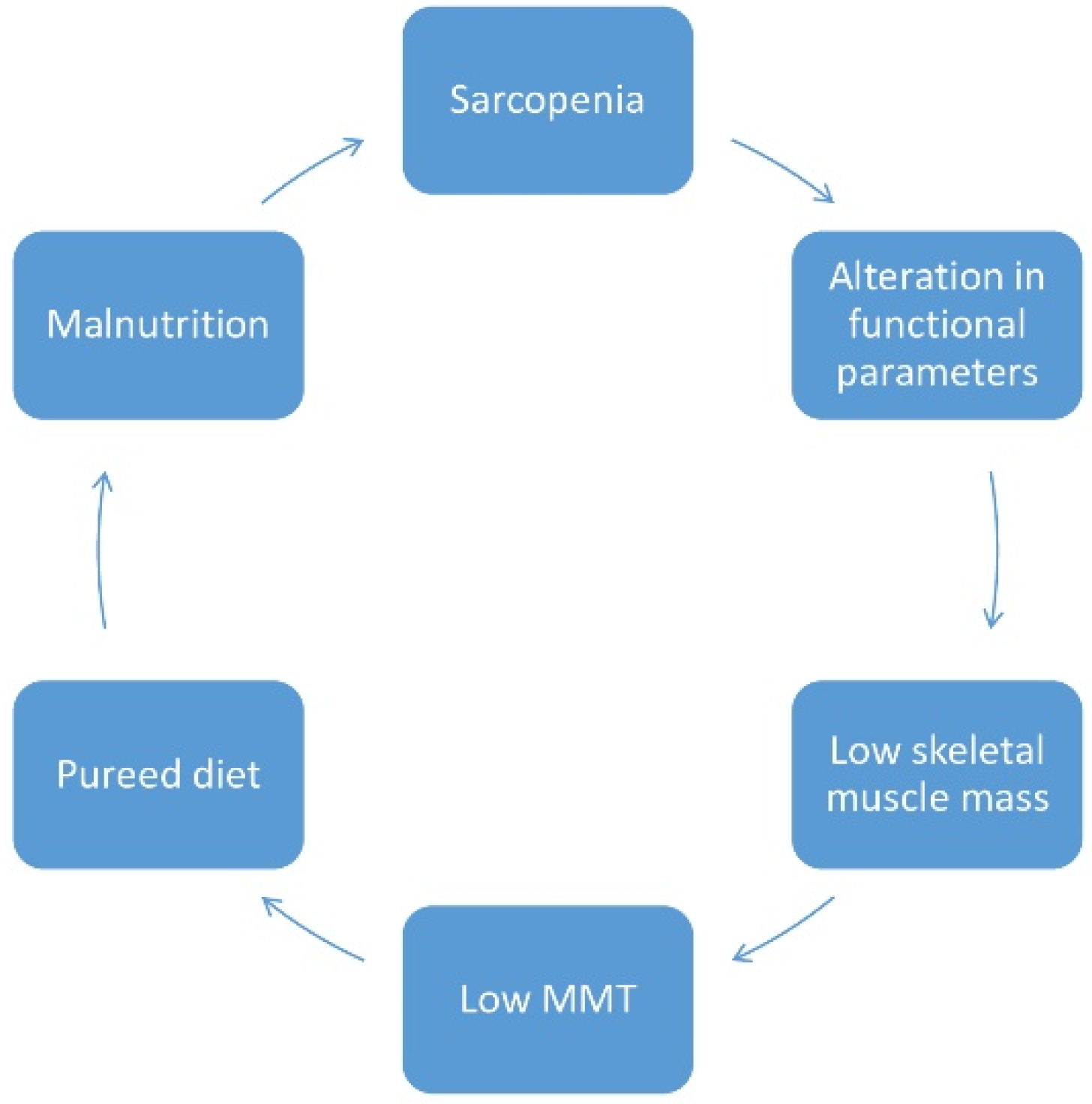
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Perkisas, S.; De Cock, A.M.; Vandewoude, M.; Verhoeven, V. Prevalence of sarcopenia and 9-year mortality in nursing home residents. Aging Clin. Exp. 2018, 31, 951–959. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.P.; Rolland, Y.; Schneider, S.M.; et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European working group on sarcopenia in older people. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Landi, F.; Liperoti, R.; Fusco, D.; Mastropaolo, S.; Quattrociocchi, D.; Proia, A.; Russo, A.; Bernabei, R.; Onder, G. Prevalence and risk factors of sarcopenia among nursing home older residents. J. Gerontol. Ser. A Biol. Sci. Med Sci. 2012, 67, 48–55. [Google Scholar] [CrossRef] [Green Version]
- Tasar, P.T.; Sahin, S.; Karaman, E.M.; Ulusoy, M.G.; Duman, S.O.; Berdeli, A.F.; Akcicek, F. Prevalence and risk factors of sarcopenia in elderly nursing home residents. Eur. Geriatr. Med. 2015, 6, 214–219. [Google Scholar] [CrossRef]
- Shen, Y.; Chen, J.; Chen, X.; Hou, L.; Lin, X.; Yang, M. Prevalence and Associated Factors of Sarcopenia in Nursing Home Residents: A Systematic Review and Meta-analysis. J. Am. Med. Dir. Assoc. 2019, 20, 5–13. [Google Scholar] [CrossRef]
- Salvà, A.; Serra-Rexach, J.A.; Artaza, I.; Formiga, F.; i Luque, X.R.; Cuesta, F.; López-Soto, A.; Masanés, F.; Ruiz, D.; Cruz-Jentoft, A.J. La prevalencia de sarcopenia en residencias de España: Comparación de los resultados del estudio multicéntrico ELLI con otras poblaciones. Rev. Esp. Geriatr. Gerontol. 2016, 51, 260–264. [Google Scholar] [CrossRef]
- Bravo-José, P.; Moreno, E.; Espert, M.; Romeu, M.; Martínez, P.; Navarro, C. Prevalence of sarcopenia and associated factors in institutionalised older adult patients. Clin. Nutr. ESPEN 2018, 27, 113–119. [Google Scholar] [CrossRef]
- Beaudart, C.; Sanchez-Rodriguez, D.; Locquet, M.; Reginster, J.Y.; Lengelé, L.; Bruyère, O. Malnutrition as a Strong Predictor of the Onset of Sarcopenia. Nutrients 2019, 12, 2883. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gingrich, A.; Volkert, D.; Kiesswetter, E.; Thomanek, M.; Bach, S.; Sieber, C.C.; Zopf, Y. Prevalence and overlap of sarcopenia, frailty, cachexia and malnutrition in older medical inpatients. BMC Geriatr. 2019, 19, 120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bauer, J.; Morley, J.E.; Schols, A.M.; Ferrucci, L.; Cruz-Jentoft, A.J.; Dent, E.; Baracos, V.E.; Crawford, J.A.; Doehner, W.; Heymsfield, S.B.; et al. Sarcopenia: A Time for Action. An SCWD Position Paper. J. Cachexia Sarcopenia Muscle 2019, 10, 956–961. [Google Scholar] [CrossRef]
- Perkisas, S.; Baudry, S.; Bauer, J.; Beckwee, D.; De Cock, A.M.; Hobbelen, H.; Jager-Wittenaar, H.; Kasiukiewicz, A.; Landi, F.; Marco, E.; et al. Application of ultrasound for muscle assessment in sarcopenia: Towards standardized measurements. Eur. Geriatr. Med. 2018, 9, 739–757. [Google Scholar] [CrossRef]
- Umeki, K.; Watanabe, Y.; Hirano, H.; Edahiro, A.; Ohara, Y.; Yoshida, H.; Obuchi, S.; Kawai, H.; Murakami, M.; Takagi, D.; et al. The relationship between masseter muscle thickness and appendicular skeletal muscle mass in Japanese community-dwelling elders: A cross-sectional study. Arch. Gerontol. Geriatr. 2018, 78, 18–22. [Google Scholar] [CrossRef]
- Moriya, S.; Ando, Y.; Miura, H. Trends and prospects of oral health conditions among Japanese: The achievement of 8020. J. Natl. Inst. Public Health 2011, 60, 379–386. [Google Scholar]
- Hernández Morante, J.J.; Gómez Martínez, C.; Morillas-Ruiz, J.M. Dietary Factors Associated with Frailty in Old Adults: A Review of Nutritional Interventions to Prevent Frailty Development. Nutrients 2019, 11, 102. [Google Scholar] [CrossRef] [Green Version]
- Education and Practical Standards Committee, European Federation of Societies for Ultrasound in Medicine and Biology. Minimum training recommendations for the practice of medical ultrasound. Ultraschall Med. 2006, 27, 79–105. [Google Scholar]
- Dupont, A.C.; Sauerbrei, E.E.; Fenton, P.V.; Shragge, P.C.; Loeb, G.E.; Richmond, F.J. Real-time sonography to estimate muscle thickness: Comparison with MRI and CT. J. Clin. Ultrasound 2001, 29, 230–236. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [Green Version]
- Malmstrom, T.K.; Miller, D.K.; Simonsick, E.M.; Ferrucci, L.; Morley, J.E. SARC-F: A symptom score to predict persons with sarcopenia at risk for poor functional outcomes. J. Cachexia Sarcopenia Muscle 2016, 7, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Parra-Rodríguez, L.; Szlejf, C.; García-González, A.I.; Malmstrom, T.K.; Cruz-Arenas, E.; Rosas-Carrasco, O. Cross-Cultural Adaptation and Validation of the Spanish-Language Version of the SARC-F to Assess Sarcopenia in Mexican Community-Dwelling Older Adults. J. Am. Med. Dir. Assoc. 2016, 17, 1142–1146. [Google Scholar] [CrossRef] [PubMed]
- Roberts, H.C.; Denison, H.J.; Martin, H.J.; Patel, H.P.; Syddall, H.; Cooper, C.; Sayer, A.A. A review of the measurement of grip strength in clinical and epidemiological studies: Towards a standardised approach. Age Ageing 2011, 40, 423–429. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dodds, R.M.; Syddall, H.E.; Cooper, R.; Benzeval, M.; Deary, I.J.; Dennison, E.M.; Der, G.; Gale, C.R.; Inskip, H.M.; Jagger, C.; et al. Grip strength across the life course: Normative data from twelve British studies. PLoS ONE 2014, 9, e113637. [Google Scholar]
- Sergi, G.; De Rui, M.; Veronese, N.; Bolzetta, F.; Berton, L.; Carraro, S.; Bano, G.; Coin, A.; Manzato, E.; Perissinotto, E. Assessing appendicular skeletal muscle mass with bioelectrical impedance analysis in free-living Caucasian older adults. Clin. Nutr. 2015, 34, 667–673. [Google Scholar] [CrossRef] [PubMed]
- Gould, H.; Brennan, S.L.; Kotowicz, M.A.; Nicholson, G.C.; Pasco, J.A. Total and appendicular lean mass reference ranges for Australian men and women: The Geelong osteoporosis study. Calcif. Tissue Int. 2014, 94, 363–372. [Google Scholar] [CrossRef] [PubMed]
- Rydwik, E.; Bergland, A.; Forsen, L.; Frändin, K. Investigation into the reliability and validity of the measurement of elderly people’s clinical walking speed: A systematic review. Physiother. Theory Pract. 2012, 28, 238–256. [Google Scholar] [CrossRef]
- Cederholm, T.; Bosaeus, I.; Barazzoni, R.; Bauer, J.; Van Gossum, A.; Klek, S.; Muscaritoli, M.; Nyulasi, I.; Ockenga, J.; Schneider, S.M.; et al. Diagnostic criteria for malnutrition—An ESPEN Consensus Statement. Clin. Nutr. 2015, 34, 335–340. [Google Scholar] [CrossRef]
- Guigoz, Y.; Vellas, B.; Garry, P.J. Mini Nutritional Assessment: A practical assessment tool for grading the nutritional state of elderly patients. Facts Res. Gerontol. 1994, 2, 15–59. [Google Scholar]
- Alastrué, A.; Sena, A.; Jaurrieta, E.; Sitges Creus, A. Anthropometric parameters for a Spanish population. Med. Clin. 1982, 78, 407–415. [Google Scholar]
- Stoudt, H.W. The anthropometry of the elderly. Hum. Factors 1981, 23, 29–37. [Google Scholar] [CrossRef]
- Chumlea, W.C.; Roche, A.F.; Steinbaugh, M.L. Estimating stature from knee height for persons 60 to 90 years of age. J. Am. Geriatr. Soc. 1985, 33, 116–120. [Google Scholar] [CrossRef]
- González-Fernández, M.; Arbones-Mainar, J.M.; Ferrer-Lahuerta, E.; Perez-Nogueras, J.; Serrano-Oliver, A.; Torres-Anoro, E.; Sanz-Paris, A. Ultrasonographic Measurement of Masseter Muscle Thickness Associates with Oral Phase Dysphagia in Institutionalized Elderly Individuals. Dysphagia 2021. [Google Scholar] [CrossRef]
- Cichero, J.A.; Lam, P.; Steele, C.M.; Hanson, B.; Chen, J.; Dantas, R.O.; Duivestein, J.; Kayashita, J.; Lecko, C.; Murray, J.; et al. Development of International Terminology and Definitions for Texture-Modified Foods and Thickened Fluids Used in Dysphagia Management: The IDDSI Framework. Dysphagia 2017, 32, 293–314. [Google Scholar] [CrossRef] [Green Version]
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The Barthel Index. Md. State Med. 1965, 14, 61–65. [Google Scholar]
- Cid-Ruzafa, J.; Damián-Moreno, J. Disability evaluation: Barthel´s index. Rev. Esp. Salud. Pública 1997, 71, 127–137. [Google Scholar] [CrossRef]
- Dodds, R.M.; Granic, A.; Davies, K.; Kirkwood, T.B.; Jagger, C.; Sayer, A.A. Prevalence and incidence of sarcopenia in the very old: Findings from the Newcastle 85+ Study. J. Cachexia Sarcopenia Muscle 2017, 8, 229–237. [Google Scholar] [CrossRef] [PubMed]
- Legrand, D.; Vaes, B.; Matheï, C.; Swine, C.; Degryse, J.M. The prevalence of sarcopenia in very old individuals according to the European consensus definition: Insights from the BELFRAIL study. Age Ageing 2013, 42, 727–734. [Google Scholar] [CrossRef] [Green Version]
- Sobestiansky, S.; Michaelsson, K.; Cederholm, T. Sarcopenia prevalence and associations with mortality and hospitalisation by various sarcopenia definitions in 85–89 year old community-dwelling men: A report from the ULSAM study. BMC Geriatr. 2019, 19, 318. [Google Scholar] [CrossRef]
- Kim, J.; Wang, Z.; Heymsfield, S.B.; Baumgartner, R.N.; Gallagher, D. Total body skeletal muscle mass: Estimation by a new dual-energy X-ray absorptiometry method. Am. J. Clin. Nutr. 2002, 76, 378–383. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cichero, J.A.; Lam, P.; Steele, C.M.; Hanson, B.; Chen, J.; Dantas, R.O.; Duivestein, J.; Kayashita, J.; Lecko, C.; Murray, J.; et al. Sarcopenia as a predictor of mortality in elderly blunt trauma patients: Comparing the masseter to the psoas using computed tomography. J. Trauma Acute Care Surg. 2017, 82, 65–72. [Google Scholar]
- Raadsheer, M.C.; Van Eijden, T.M.G.J.; Van Ginkel, F.C.; Prahl-Andersen, B. Human jaw muscle strength and size in relation to limb muscle strength and size. Eur. J. Oral Sci. 2004, 112, 398–405. [Google Scholar] [CrossRef]
- Yamaguchi, K.; Tohara, H.; Hara, K.; Nakane, A.; Kajisa, E.; Yoshimi, K.; Minakuchi, S. Relationship of aging, skeletal muscle mass, and tooth loss with masseter muscle thickness. BMC Geriatr. 2018, 18, 67. [Google Scholar] [CrossRef]
- N’gom, P.I.; Woda, A. Influence of impaired mastication on nutrition. J. Prosthet. Dent. 2002, 87, 667–673. [Google Scholar] [CrossRef]
- Hwang, Y.; Lee, Y.H.; Cho, D.H.; Kim, M.; Lee, D.S.; Cho, H.J. Applicability of the masseter muscle as a nutritional biomarker. Medicine 2020, 99, e19069. [Google Scholar] [CrossRef] [PubMed]
- Iinuma, T.; Arai, Y.; Fukumoto, M.; Takayama, M.; Abe, Y.; Asakura, K.; Nishiwaki, Y.; Takebayashi, T.; Iwase, T.; Komiyama, K.; et al. Maximum occlusal force and physical performance in the oldest old: The Tokyo oldest old survey on total health. J. Am. Geriatr. Soc. 2012, 60, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, K.; Tohara, H.; Hara, K.; Nakane, A.; Yoshimi, K.; Nakagawa, K.; Minakuchi, S. Factors associated with masseter muscle quality assessed from ultrasonography in community-dwelling elderly individuals: A cross-sectional study. Arch. Gerontol. Geriatr. 2019, 82, 128–132. [Google Scholar] [CrossRef] [PubMed]
- Gaszynska, E.; Godala, M.; Szatko, F.; Gaszynski, T. Masseter muscle tension, chewing ability, and selected parameters of physical fitness in elderly care home residents in Lodz, Poland. Clin. Interv. Aging 2014, 9, 1197–1203. [Google Scholar] [CrossRef] [Green Version]
- Watanabe, Y.; Hirano, H.; Arai, H.; Morishita, S.; Ohara, Y.; Edahiro, A.; Murakami, M.; Shimada, H.; Kikutani, T.; Suzuki, T. Relationship Between Frailty and Oral Function in Community-Dwelling Elderly Adults. J. Am. Geriatr. Soc. 2017, 65, 66–76. [Google Scholar] [CrossRef]
- Faxén-Irving, G.; Luiking, Y.; Grönstedt, H.; Franzén, E.; Seiger, Å.; Vikström, S.; Wimo, A.; Boström, A.M.; Cederholm, T. Do Malnutrition, Sarcopenia and Frailty Overlap in Nursing-Home Residents? J. Frailty Aging 2021, 10, 17–21. [Google Scholar]
- Keller, H.H.; Carrier, N.; Slaughter, S.E.; Lengyel, C.; Steele, C.M.; Duizer, L.; Morrison, J.; Brown, K.S.; Chaudhury, H.; Yoon, M.N.; et al. Prevalence and Determinants of Poor Food Intake of Residents Living in Long-Term Care. J. Am. Med. Dir. Assoc. 2017, 18, 941–947. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dahl, W.J.; Whiting, S.J.; Tyler, R.T. Protein content of pureed diets: Implications for planning. Can. J. Diet. Pract. Res. 2007, 68, 99–102. [Google Scholar] [CrossRef] [PubMed]
- Vucea, V.; Keller, H.H.; Ducak, K. Interventions for Improving Mealtime Experiences in Long-Term Care. J. Nutr. Gerontol. Geriatr. 2014, 33, 249–324. [Google Scholar] [CrossRef] [PubMed]
- De Luis, D.; Aller, R.; Izaola, O. Modified texture diet and useful in patients with nutritional risk. Nutr. Hosp. 2014, 29, 751–759. [Google Scholar] [PubMed]
- Rodríguez-Rejón, A.I.; Ruiz-López, M.D.; Artacho, R. Dietary Intake and Associated Factors in Long-Term Care Homes in Southeast Spain. Nutrients 2019, 11, 266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Minetto, M.A.; Caresio, C.; Menapace, T.; Hajdarevic, A.; Marchini, A.; Molinari, F.; Maffiuletti, N.A. Ultrasound-Based Detection of Low Muscle Mass for Diagnosis of Sarcopenia in Older Adults. PMR 2016, 8, 453–462. [Google Scholar] [CrossRef] [PubMed]
- Fukumoto, Y.; Ikezoe, T.; Taniguchi, M.; Yamada, Y.; Sawano, S.; Minani, S.; Asai, T.; Kimura, M.; Ichihashi, N. Cut-off Values for Lower Limb Muscle Thickness to Detect Low Muscle Mass for Sarcopenia in Older Adults. Clin. Interv. Aging 2021, 25, 1215–1222. [Google Scholar] [CrossRef] [PubMed]
| All (n = 464) | Women (n = 325) | Men (n = 139) | p | |
|---|---|---|---|---|
| Age (years) | 84.7 (7.7) | 85.1 (7.6) | 83.7 (7.6) | 0.06 |
| BMI (Kg/m2) | 24.4 (5.8) | 24.7 (6.3) | 23.8 (4.3) | 0.07 |
| MMT (mm) | 6.5 (1.5) | 6.2 (1.5) | 7.0 (1.6) | 0.0001 |
| MNA score | 19.6 (5.0) | 18.9 (4.9) | 20.9 (4.9) | 0.0001 |
| MNA normal (%) | 25.6 | 20.0 | 38.2 | 0.0001 |
| MNA risk (%) | 47.8 | 49.7 | 43.8 | |
| MNA malnutrition (%) | 26.5 | 30.3 | 18.1 | |
| GLIM normal (%) | 88.8 | 89.7 | 86.8 | 0.2 |
| GLIM malnutrition (%) | 11.2 | 10.3 | 13.2 | |
| Total dependence (%) | 37.9 | 43.7 | 24.5 | 0.0001 |
| Severe dependence (%) | 13.4 | 15.1 | 9.4 | |
| Moderate dependence (%) | 15.7 | 16.3 | 14.4 | |
| Light dependence (%) | 30.6 | 24.0 | 46.0 | |
| Independent (%) | 2.4 | 0.9 | 5.8 | |
| Regular diet (%) | 55.4 | 51.4 | 64.4 | 0.043 |
| Soft diet (%) | 14.9 | 16.6 | 10.8 | |
| Smooth puréed diet (%) | 29.7 | 31.7 | 25.2 | |
| Sarcopenia risk (%) | 71.8 | 79.7 | 54.2 | 0.0001 |
| Probable sarcopenia (%) | 70.5 | 78.1 | 53.5 | 0.0001 |
| Confirmed sarcopenia (%) | 39.2 | 40.0 | 37.5 | 0.6 |
| Severe sarcopenia (%) | 38.6 | 39.1 | 37.5 | 0.7 |
| Factors | MMT (mm) | Differences |
|---|---|---|
| Diet Texture | ||
| Regular | 7.0 (1.4) | p: 0.0001 |
| Soft | 6.3 (1.5) | |
| Puréed | 5.5 (1.3) | |
| Malnutrition (MNA) | ||
| Normal | 7.6 (1.3) | p: 0.0001 |
| Risk | 6.6 (1.4) | |
| Confirmed malnutrition | 5.1 (1.1) | |
| Malnutrition (GLIM) | ||
| Normal | 6.6 (1.5) | p: 0.0001 |
| Confirmed malnutrition | 5.5 (1.3) | |
| Sarcopenia | ||
| Normal | 7.3 (1.4) | p: 0.0001 |
| Confirmed sarcopenia | 5.5 (1.3) | |
| Barthel Index | ||
| Independent | 8.8 (1.5) | p: 0.0001 |
| Mild | 7.7 (1.3) | |
| Moderate | 6.9 (0.8) | |
| Severe | 6.7 (0.9) | |
| Total | 5.1 (0.9) | |
| OR (RAW) | OR (Model 1) | OR (Model 2) | OR (Model 3) | |
|---|---|---|---|---|
| Sarcopenia | 0.37 (0.30–0.45, p < 0.001) | 0.34 (0.28–0.42, p < 0.001) | 0.42 (0.33–0.52, p < 0.001) | 0.43 (0.34–0.54, p < 0.001) |
| Malnutrition (MNA) | 0.31 (0.25–0.40, p < 0.001) | 0.30 (0.23–0.33, p < 0.001) | 0.34 (0.27–0.45, p < 0.001) | 0.37 (0.29–0.49, p < 0.001) |
| Malnutrition (GLIM) | 0.6 (0.48–0.75, p < 0.001) | 0.57 (0.45–0.72, p < 0.001) | 0.65 (0.50–0.85, p < 0.001) | 0.66 (0.51–0.87, p < 0.003) |
| Cutoff Point | Area | Significance | 95% IC | Sensitivity | Specificity | ||
|---|---|---|---|---|---|---|---|
| Lower Limit | Upper Limit | ||||||
| Malnutrition (GLIM) | 7.21 mm | 0.749 | 0.0001 | 0.659 | 0.840 | 0.536 | 0.947 |
| Malnutrition (MNA) | 6.59 mm | 0.965 | 0.0001 | 0.923 | 1.000 | 0.891 | 0.962 |
| Sarcopenia | 6.59 mm | 0.843 | 0.0001 | 0.774 | 0.912 | 0.844 | 0.722 |
| Cutoff Point | Area | Significance | 95% CI | Sensitivity | Specificity | ||
|---|---|---|---|---|---|---|---|
| Lower Limit | Upper Limit | ||||||
| Malnutrition (GLIM) | 5.78 mm | 0.707 | 0.0001 | 0.607 | 0.808 | 0.662 | 0.727 |
| Malnutrition (MNA) | 6.27 mm | 0.897 | 0.0001 | 0.844 | 0.950 | 0.862 | 0.867 |
| Sarcopenia | 6.00 mm | 0.822 | 0.0001 | 0.775 | 0.869 | 0.776 | 0.766 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
González-Fernández, M.; Perez-Nogueras, J.; Serrano-Oliver, A.; Torres-Anoro, E.; Sanz-Arque, A.; Arbones-Mainar, J.M.; Sanz-Paris, A. Masseter Muscle Thickness Measured by Ultrasound as a Possible Link with Sarcopenia, Malnutrition and Dependence in Nursing Homes. Diagnostics 2021, 11, 1587. https://doi.org/10.3390/diagnostics11091587
González-Fernández M, Perez-Nogueras J, Serrano-Oliver A, Torres-Anoro E, Sanz-Arque A, Arbones-Mainar JM, Sanz-Paris A. Masseter Muscle Thickness Measured by Ultrasound as a Possible Link with Sarcopenia, Malnutrition and Dependence in Nursing Homes. Diagnostics. 2021; 11(9):1587. https://doi.org/10.3390/diagnostics11091587
Chicago/Turabian StyleGonzález-Fernández, Mikel, Javier Perez-Nogueras, Antonio Serrano-Oliver, Elena Torres-Anoro, Alejandro Sanz-Arque, Jose M. Arbones-Mainar, and Alejandro Sanz-Paris. 2021. "Masseter Muscle Thickness Measured by Ultrasound as a Possible Link with Sarcopenia, Malnutrition and Dependence in Nursing Homes" Diagnostics 11, no. 9: 1587. https://doi.org/10.3390/diagnostics11091587
APA StyleGonzález-Fernández, M., Perez-Nogueras, J., Serrano-Oliver, A., Torres-Anoro, E., Sanz-Arque, A., Arbones-Mainar, J. M., & Sanz-Paris, A. (2021). Masseter Muscle Thickness Measured by Ultrasound as a Possible Link with Sarcopenia, Malnutrition and Dependence in Nursing Homes. Diagnostics, 11(9), 1587. https://doi.org/10.3390/diagnostics11091587






