Histological Hallmarks of Mucosal Healing in Inflammatory Bowel Diseases in the Era of Monoclonal Antibodies Therapy: New Insights and Perspectives
Abstract
1. Introduction
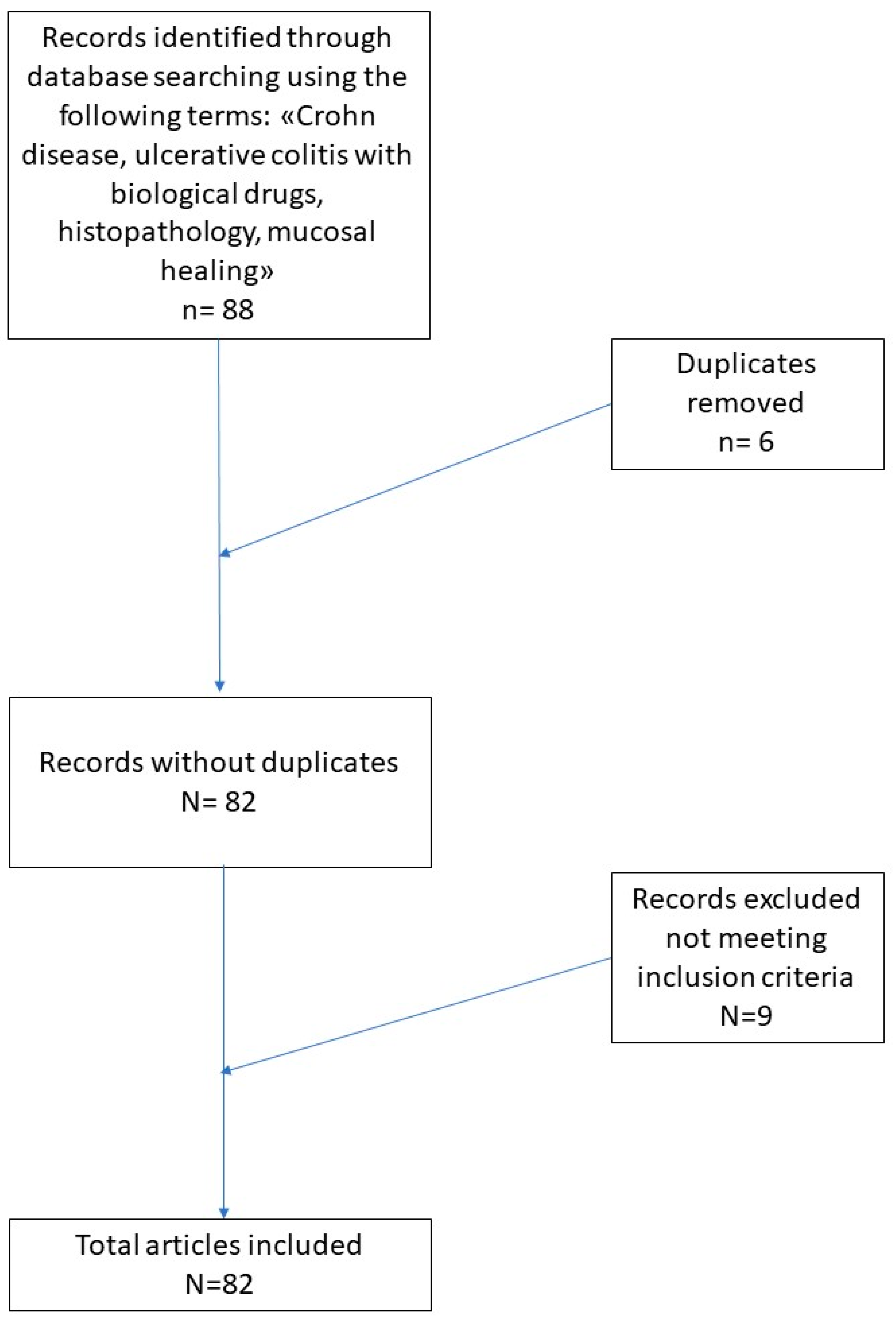
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Baumgart, D.C.; Carding, S.R. Inflammatory bowel disease: Cause and immunobiology. Lancet 2007, 369, 1627–1640. [Google Scholar] [CrossRef]
- Sairenji, T.; Collins, K.L.; Evans, D.V. An Update on Inflammatory Bowel Disease. Prim. Care 2017, 44, 673–692. [Google Scholar] [CrossRef]
- Mitchell, P.J.; Rabau, M.Y.; Haboubi, N.Y. Indeterminate colitis. Tech. Coloproctol. 2007, 11, 91–96. [Google Scholar] [CrossRef]
- Park, T.; Cave, D.; Marshall, C. Microscopic colitis: A review of etiology, treatment and refractory disease. World J. Gastroenterol. 2015, 21, 8804–8810. [Google Scholar] [CrossRef]
- Kaplan, G.G. The global burden of IBD: From 2015 to 2025. Nat. Rev. Gastroenterol. Hepatol. 2015, 12, 720–727. [Google Scholar] [CrossRef]
- Feakins, R.M. Ulcerative colitis or Crohn’s disease? Pitfalls and problems. Histopathology 2014, 64, 317–335. [Google Scholar] [CrossRef]
- Gajendran, M.; Loganathan, P.; Jimenez, G.; Catinella, A.P.; Ng, N.; Umapathy, C.; Ziade, N.; Hashash, J.G. A comprehensive review and update on ulcerative colitis. Dis. Mon. 2019, 65, 100851. [Google Scholar] [CrossRef]
- Feuerstein, J.D.; Moss, A.C.; Farraye, F.A. Ulcerative Colitis. Mayo Clin. Proc. 2019, 94, 1357–1373. [Google Scholar] [CrossRef]
- Boal Carvalho, P.; Cotter, J. Mucosal Healing in Ulcerative Colitis: A Comprehensive Review. Drugs 2017, 77, 159–173. [Google Scholar] [CrossRef]
- Shepherd, N.A.; Warren, B.F.; Williams, G.T.; Greenson, J.K.; Lauwers, G.Y.; Novelli, M.R. (Eds.) Morson and Dawson’s Gastrointestinal Pathology, 5th ed.; Wiley: Hoboken, NJ, USA, 2012. [Google Scholar]
- WHO Classification of Tumours Editorial Board. Digestive System Tumours: WHO Classification of Tumours; WHO: Geneva, Switzerland, 2019; Volume 1. [Google Scholar]
- Ko, J.K.; Auyeung, K.K. Inflammatory bowel disease: Etiology, pathogenesis and current therapy. Curr. Pharm Des. 2014, 20, 1082–1096. [Google Scholar] [CrossRef]
- Koelink, P.J.; Bloemendaal, F.M.; Li, B.; Westera, L.; Vogels, E.W.M.; van Roest, M.; Gloudemans, A.K.; van ‘t Wout, A.B.; Korf, H.; Vermeire, S.; et al. Anti-TNF therapy in IBD exerts its therapeutic effect through macrophage IL-10 signalling. Gut 2020, 69, 1053–1063. [Google Scholar] [CrossRef] [PubMed]
- Mao, R.; Hu, P.J. The Future of IBD Therapy: Where Are We and Where Should We Go Next? Dig. Dis. 2016, 34, 175–179. [Google Scholar] [CrossRef]
- Geboes, K.; Riddell, R.; Öst, A.; Jensfelt, B.; Persson, T.; Löfberg, R. A reproducible grading scale for histological assessment of inflammation in ulcerative colitis. Gut 2000, 47, 404–409. [Google Scholar] [CrossRef]
- Marchal-Bressenot, A.; Salleron, J.; Boulagnon-Rombi, C.; Bastien, C.; Cahn, V.; Cadiot, G.; Diebold, M.D.; Danese, S.; Reinisch, W.; Schreiber, S.; et al. Development and validation of the Nancy histological index for UC. Gut 2017, 66, 43–49. [Google Scholar] [CrossRef]
- Khanna, R.; Ma, C.; Jairath, V.; Vande Casteele, N.; Zou, G.; Feagan, B.G. Endoscopic Assessment of Inflammatory Bowel Disease Activity in Clinical Trials. Clin. Gastroenterol. Hepatol. 2020. [Google Scholar] [CrossRef]
- Arijs, I.; De Hertogh, G.; Lemmens, B.; Van Lommel, L.; de Bruyn, M.; Vanhove, W.; Cleynen, I.; Machiels, K.; Ferrante, M.; Schuit, F.; et al. Effect of vedolizumab (anti-α4β7-integrin) therapy on histological healing and mucosal gene expression in patients with UC. Gut 2018, 67, 43–52. [Google Scholar] [CrossRef]
- Dai, C.; Liu, W.X.; Jiang, M.; Sun, M.J. Mucosal healing did not predict sustained clinical remission in patients with IBD after discontinuation of one-year infliximab therapy. PLoS ONE 2014, 9, e110797. [Google Scholar] [CrossRef]
- Oxford Centre for Evidence-Based Medicine 2011 Levels of Evidence. Available online: http://www.cebm.net/wp-content/uploads/2014/06/CEBM-Levels-of-Evidence-2.1.pdf (accessed on 26 July 2021).
- Pigneur, B.; Lepage, P.; Mondot, S.; Schmitz, J.; Goulet, O.; Doré, J.; Ruemmele, F.M. Mucosal Healing and Bacterial Composition in Response to Enteral Nutrition Vs Steroid-based Induction Therapy-A Randomised Prospective Clinical Trial in Children With Crohn’s Disease. J. Crohns Colitis. 2019, 13, 846–855. [Google Scholar] [CrossRef]
- Li, K.; Friedman, J.R.; Chan, D.; Pollack, P.; Yang, F.; Jacobstein, D.; Brodmerkel, C.; Gasink, C.; Feagan, B.G.; Sandborn, W.J.; et al. Effects of Ustekinumab on Histologic Disease Activity in Patients with Crohn’s Disease. Gastroenterology 2019, 157, 1019.e7–1031.e7. [Google Scholar] [CrossRef]
- Nardone, O.M.; Shivaji, U.N.; Ferruzza, V.; Ghosh, S.; Iacucci, M. Soluble Blood Markers of Mucosal Healing in Inflammatory Bowel Disease: The Future of Noninvasive Monitoring. Inflamm. Bowel Dis. 2020, 26, 961–969. [Google Scholar] [CrossRef]
- Mazzuoli, S.; Guglielmi, F.W.; Antonelli, E.; Salemme, M.; Bassotti, G.; Villanacci, V. Definition and evaluation of mucosal healing in clinical practice. Dig. Liver Dis. 2013, 45, 969–977. [Google Scholar] [CrossRef]
- Leung, C.M.; Tang, W.; Kyaw, M.; Niamul, G.; Aniwan, S.; Limsrivilai, J.; Wang, Y.F.; Ouyang, Q.; Simadibrata, M.; Abdul-lah, M.; et al. Endoscopic and Histological Mucosal Healing in Ulcerative Colitis in the First Year of Diagnosis: Results from a Population-based Inception Cohort from Six Countries in Asia. J. Crohns Colitis 2017, 11, 1440–1448. [Google Scholar] [CrossRef] [PubMed]
- Bitton, A.; Peppercorn, M.A.; Antonioli, D.A.; Niles, J.L.; Shah, S.; Bousvaros, A.; Ransil, B.; Wild, G.; Cohen, A.; Edwardes, M.D.D.; et al. Clinical, biological, and histologic parameters as predictors of relapse in ulcerative colitis. Gastroenterology 2001, 120, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Af Björkesten, C.G.; Nieminen, U.; Turunen, U.; Arkkila, P.E.; Sipponen, T.; Färkkilä, M.A. Endoscopic monitoring of infliximab therapy in Crohn’s disease. Inflamm. Bowel Dis. 2011, 17, 947–953. [Google Scholar] [CrossRef]
- Fiorino, G.; Cesarini, M.; Indriolo, A.; Malesci, A. Mucosal healing in ulcerative colitis: Where do we stand? Curr. Drug Targets 2011, 12, 1417–1423. [Google Scholar] [CrossRef] [PubMed]
- Dave, M.; Loftus, E.V. Mucosal healing in inflammatory bowel disease-a true paradigm of success? Gastroenterol. Hepatol. 2012, 8, 29–38. [Google Scholar]
- D’haens, G.; Van Deventer, S.; Van Hogezand, R.; Chalmers, D.; Kothe, C.; Baert, F.; Braakman, T.; Schaible, T.; Geboes, K.; Rutgeerts, P. Endoscopic and histological healing with infliximab anti-tumor necrosis factor antibodies in Crohn’s disease: A European multicenter trial. Gastroenterology 1999, 116, 1029–1034. [Google Scholar] [CrossRef]
- Schnitzler, F.; Fidder, H.; Ferrante, M.; Noman, M.; Arijs, I.; Van Assche, G.; Hoffman, I.; Van Steen, K.; Vermeire, S.; Rutgeerts, P. Mucosal healing predicts long-term outcome of maintenance therapy with infliximab in Crohn’s disease. Inflamm. Bowel Dis. 2009, 15, 1295–1301. [Google Scholar] [CrossRef]
- Frøslie, K.F.; Jahnsen, J.; Moum, B.A.; Vatn, M.H.; IBSEN Group. Mucosal healing in inflammatory bowel disease: Results from a Norwegian population-based cohort. Gastroenterology 2007, 133, 412–422. [Google Scholar] [CrossRef]
- Neurath, M.F.; Travis, S.P. Mucosal healing in inflammatory bowel diseases: A systematic review. Gut 2012, 61, 1619–1635. [Google Scholar] [CrossRef]
- Ferrante, M.; Van Assche, G. Medical therapy and mucosal healing. Curr. Drug Targets 2012, 13, 1294–1299. [Google Scholar] [CrossRef] [PubMed]
- Rogler, G.; Vavricka, S.; Schoepfer, A.; Lakatos, P.L. Mucosal healing and deep remission: What does it mean? World J. Gastroenterol. 2013, 19, 7552–7560. [Google Scholar] [CrossRef]
- Seidelin, J.B.; Coskun, M.; Nielsen, O.H. Mucosal healing in ulcerative colitis: Pathophysiology and pharmacology. Adv. Clin. Chem. 2013, 59, 101–123. [Google Scholar]
- Osterman, M.T. Mucosal healing in inflammatory bowel disease. J. Clin. Gastroenterol. 2013, 47, 212–221. [Google Scholar] [CrossRef]
- Dulai, P.S.; Levesque, B.G.; Feagan, B.G.; D’Haens, G.; Sandborn, W.J. Assessment of mucosal healing in inflammatory bowel disease: Review. Gastrointest. Endosc. 2015, 82, 246–255. [Google Scholar] [CrossRef] [PubMed]
- Florholmen, J. Mucosal healing in the era of biologic agents in treatment of inflammatory bowel disease. Scand. J. Gastroenterol. 2015, 50, 43–52. [Google Scholar] [CrossRef]
- Yu, L.; Yang, X.; Xia, L.; Zhong, J.; Ge, W.; Wu, J.; Liu, H.; Liu, F.; Liu, Z. Infliximab preferentially induces clinical remission and mucosal healing in short course Crohn’s disease with luminal lesions through balancing abnormal immune response in gut mucosa. Mediat. Inflamm. 2015, 2015, 793764. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.C.; Colombel, J.F.; Sands, B.E.; Narula, N. Systematic review with meta-analysis: Mucosal healing is associated with improved long-term outcomes in Crohn’s disease. Aliment. Pharmacol. Ther. 2016, 43, 317–333. [Google Scholar] [CrossRef]
- Vickers, A.D.; Ainsworth, C.; Mody, R.; Bergman, A.; Ling, C.S.; Medjedovic, J.; Smyth, M. Systematic Review with Network Meta-Analysis: Comparative Efficacy of Biologics in the Treatment of Moderately to Severely Active Ulcerative Colitis. PLoS ONE 2016, 11, e0165435. [Google Scholar] [CrossRef] [PubMed]
- Reinink, A.R.; Lee, T.C.; Higgins, P.D. Endoscopic Mucosal Healing Predicts Favorable Clinical Outcomes in Inflammatory Bowel Disease: A Meta-analysis. Inflamm. Bowel Dis. 2016, 22, 1859–1869. [Google Scholar] [CrossRef]
- Eder, P.; Lykowska-Szuber, L.; Iwanik, K.; Krela-Kazmierczak, I.; Stawczyk-Eder, K.; Majewski, P.; Linke, K.; Kay, E.W.; Wozniak, A. The influence of anti-TNF therapy on CD31 and VEGF expression in colonic mucosa of Crohn’s disease patients in relation to mucosal healing. Folia Histochem Cytobiol. 2016, 54, 75–80. [Google Scholar] [CrossRef][Green Version]
- Cholapranee, A.; Hazlewood, G.S.; Kaplan, G.G.; Peyrin-Biroulet, L.; Ananthakrishnan, A.N. Systematic review with meta-analysis: Comparative efficacy of biologics for induction and maintenance of mucosal healing in Crohn’s disease and ulcerative colitis controlled trials. Aliment. Pharmacol. Ther. 2017, 45, 1291–1302. [Google Scholar] [CrossRef]
- Kurashima, Y.; Kiyono, H. Mucosal Ecological Network of Epithelium and Immune Cells for Gut Homeostasis and Tissue Healing. Annu. Rev. Immunol. 2017, 35, 119–147. [Google Scholar] [CrossRef] [PubMed]
- Pantavou, K.; Yiallourou, A.I.; Piovani, D.; Evripidou, D.; Danese, S.; Peyrin-Biroulet, L.; Bonovas, S.; Nikolopoulos, G.K. Efficacy and safety of biologic agents and tofacitinib in moderate-to-severe ulcerative colitis: A systematic overview of meta-analyses. United Eur. Gastroenterol. J. 2019, 7, 1285–1303. [Google Scholar] [CrossRef]
- Singh, S.; Fumery, M.; Sandborn, W.J.; Murad, M.H. Systematic review with network meta-analysis: First- and second-line pharmacotherapy for moderate-severe ulcerative colitis. Aliment. Pharmacol. Ther. 2018, 47, 162–175. [Google Scholar] [CrossRef]
- Leppkes, M.; Siegmund, B.; Becker, C. Editorial: Immune-Epithelial Crosstalk in Inflammatory Bowel Diseases and Mucosal Wound Healing. Front. Immunol. 2018, 9, 1171. [Google Scholar] [CrossRef]
- Antonelli, E.; Villanacci, V.; Bassotti, G. Novel oral-targeted therapies for mucosal healing in ulcerative colitis. World J. Gastroenterol. 2018, 24, 5322–5330. [Google Scholar] [CrossRef]
- Castiglione, F.; Imperatore, N.; Testa, A.; De Palma, G.D.; Nardone, O.M.; Pellegrini, L.; Caporaso, N.; Rispo, A. One-year clinical outcomes with biologics in Crohn’s disease: Transmural healing compared with mucosal or no healing. Aliment. Pharmacol Ther. 2019, 49, 1026–1039. [Google Scholar] [CrossRef]
- Park, S.H.; Hong, M.; Lee, H.S.; Ye, B.D.; Hwang, S.W.; Jung, S.; Baek, J.; Moon, J.W.; Kim, B.M.; Oh, S.H.; et al. Association of TRAP1 with infliximab-induced mucosal healing in Crohn’s disease. J. Gastroenterol. Hepatol. 2019, 34, 2118–2125. [Google Scholar] [CrossRef]
- Samaan, M.; Campbell, S.; Cunningham, G.; Tamilarasan, A.G.; Irving, P.M.; McCartney, S. Biologic therapies for Crohn’s disease: Optimising the old and maximising the new. F1000Research 2019, 8, 1210. [Google Scholar] [CrossRef]
- Löwenberg, M.; Vermeire, S.; Mostafavi, N.; Hoentjen, F.; Franchimont, D.; Bossuyt, P.; Hindryckx, P.; Rispens, T.; de Vries, A.; van der Woude, C.J.; et al. Vedolizumab Induces Endoscopic and Histologic Remission in Patients with Crohn’s Disease. Gastroenterology 2019, 157, 997.e6–1006.e6. [Google Scholar] [CrossRef] [PubMed]
- Pouillon, L.; Rousseau, H.; Busby-Venner, H.; De Carvalho Bittencourt, M.; Choukour, M.; Gauchotte, G.; Zallot, C.; Danese, S.; Baumann, C.; Peyrin-Biroulet, L. Vedolizumab Trough Levels and Histological Healing During Maintenance Therapy in Ulcerative Colitis. J. Crohns Colitis 2019, 13, 970–975. [Google Scholar] [CrossRef] [PubMed]
- Cucchiara, S.; D’Arcangelo, G.; Isoldi, S.; Aloi, M.; Stronati, L. Mucosal healing in Crohn’s disease: New insights. Expert Rev. Gastroenterol. Hepatol. 2020, 14, 335–345. [Google Scholar] [CrossRef]
- Petryszyn, P.; Ekk-Cierniakowski, P.; Zurakowski, G. Infliximab, adalimumab, golimumab, vedolizumab and tofacitinib in moderate to severe ulcerative colitis: Comparative cost-effectiveness study in Poland. Ther. Adv. Gastroenterol. 2020, 25, 13–17. [Google Scholar] [CrossRef]
- Kucharzik, T.; Koletzko, S.; Kannengiesser, K.; Dignass, A. Ulcerative Colitis-Diagnostic and Therapeutic Algorithms. Dtsch. Ärzteblatt Int. 2020, 117, 564–574. [Google Scholar] [CrossRef]
- Sagami, S.; Kobayashi, T.; Aihara, K.; Umeda, M.; Morikubo, H.; Matsubayashi, M.; Kiyohara, H.; Nakano, M.; Ohbu, M.; Hibi, T. Transperineal ultrasound predicts endoscopic and histological healing in ulcerative colitis. Aliment. Pharmacol. Ther. 2020, 51, 1373–1383. [Google Scholar] [CrossRef]
- Li, K.; Marano, C.; Zhang, H.; Yang, F.; Sandborn, W.J.; Sands, B.E.; Feagan, B.G.; Rubin, D.T.; Peyrin-Biroulet, L.; Friedman, J.R.; et al. Relationship Between Combined Histologic and Endoscopic Endpoints and Efficacy of Ustekinumab Treatment in Patients with Ulcerative Colitis. Gastroenterology 2020, 159, 2052–2064. [Google Scholar] [CrossRef] [PubMed]
- Schumacher, G.; Kollberg, B.; Sandstedt, B. A prospective study of first attacks of inflammatory bowel disease and infectious colitis. Histologic course during the 1st year after presentation. Scand. J. Gastroenterol. 1994, 29, 318–332. [Google Scholar] [CrossRef]
- Phillipson, M.; Kubes, P. The Healing Power of Neutrophils. Trends Immunol. 2019, 40, 635–647. [Google Scholar] [CrossRef] [PubMed]
- Iai, M.; Ghosh, S. Mucosal Healing—How Deep Is Enough? Dig. Dis. 2016, 34, 160–164. [Google Scholar]
- Scott, B.B.; Goodall, A.; Stephenson, P.; Jenkins, D. Rectal mucosal plasma cells in inflammatory bowel disease. Gut 1983, 24, 519–524. [Google Scholar] [CrossRef]
- Seldenrijk, C.A.; Morson, B.C.; Meuwissen, S.G.; Schipper, N.W.; Lindeman, J.; Meijer, C.J. Histopathological evaluation of colonic mucosal biopsy specimens in chronic inflammatory bowel disease: Diagnostic implications. Gut 1991, 32, 1514–1520. [Google Scholar] [CrossRef]
- Casellas, F.; Barreiro de Acosta, M.; Iglesias, M.; Robles, V.; Nos, P.; Aguas, M.; Riestra, S.; de Francisco, R.; Papo, M.; Borruel, N. Mucosal healing restores normal health and quality of life in patients with inflammatory bowel disease. Eur. J. Gastroenterol. Hepatol. 2012, 24, 762–769. [Google Scholar] [CrossRef] [PubMed]
- Sumagin, R.; Robin, A.Z.; Nusrat, A.; Parkos, C.A. Transmigrated neutrophils in the intestinal lumen engage ICAM-1 to regulate the epithelial barrier and neutrophil recruitment. Mucosal Immunol. 2014, 7, 905–915. [Google Scholar] [CrossRef]
- Schmitt, H.; Ulmschneider, J.; Billmeier, U.; Vieth, M.; Scarozza, P.; Sonnewald, S.; Reid, S.; Atreya, I.; Rath, T.; Zundler, S.; et al. The TLR9 Agonist Cobitolimod Induces IL10-Producing Wound Healing Macrophages and Regulatory T Cells in Ulcerative Colitis. J. Crohns Colitis 2020, 14, 508–524. [Google Scholar] [CrossRef] [PubMed]
- Di Ruscio, M.; Variola, A.; Vernia, F.; Lunardi, G.; Castelli, P.; Bocus, P.; Geccherle, A. Role of Ulcerative Colitis Endoscopic Index of Severity (UCEIS) versus Mayo Endoscopic Subscore (MES) in Predicting Patients’ Response to Biological Therapy and the Need for Colectomy. Digestion 2021, 102, 534–545. [Google Scholar] [CrossRef]
- Castro-Dopico, T.; Fleming, A.; Dennison, T.W.; Ferdinand, J.R.; Harcourt, K.; Stewart, B.J.; Cader, Z.; Tuong, Z.K.; Jing, C.; Lok, L.S.C.; et al. GM-CSF Calibrates Macrophage Defense and Wound Healing Programs during Intestinal Infection and Inflammation. Cell Rep. 2020, 32, 107857. [Google Scholar] [CrossRef] [PubMed]
- Danese, S.; Sandborn, W.J.; Colombel, J.F.; Vermeire, S.; Gloverm, S.C.; Rimola, J.; Siegelman, J.; Jones, S.; Bornstein, J.D.; Feagan, B.G. Endoscopic, Radiologic, and Histologic Healing With Vedolizumab in Patients With Active Crohn’s Disease. Gastroenterology 2019, 157, 1007–1018.e7. [Google Scholar] [CrossRef] [PubMed]
- Baert, F.J.; D’Haens, G.R.; Peeters, M.; Hiele, M.I.; Schaible, T.F.; Shealy, D.; Geboes, K.; Rutgeerts, P.J. Tumor necrosis factor alpha antibody (infliximab) therapy profoundly down-regulates the inflammation in Crohn’s ileocolitis. Gastroenterology 1999, 116, 22–28. [Google Scholar] [CrossRef]
- Katsanos, K.H.; Papadakis, K.A. Inflammatory Bowel Disease: Updates on Molecular Targets for Biologics. Gut Liver 2017, 11, 455–463. [Google Scholar] [CrossRef]
- Pizarro, T.T.; Stappenbeck, T.S.; Rieder, F.; Rosen, M.J.; Colombel, J.F.; Donowitz, M.; Towne, J.; Mazmanian, S.K.; Faith, J.J.; Hodin, R.A.; et al. Challenges in IBD Research: Preclinical Human IBD Mechanisms. Inflamm. Bowel Dis. 2019, 25 (Suppl. 2), S5–S12. [Google Scholar] [CrossRef]
- Hassan, C.; Ierardi, E.; Burattini, O.; De Francesco, V.; Zullo, A.; Stoppino, G.; Panella, C.; Morini, S. Tumour necrosis factor alpha down-regulation parallels inflammatory regression in ulcerative colitis patients treated with infliximab. Dig. Liver Dis. 2007, 39, 811–817. [Google Scholar] [CrossRef] [PubMed]
- Fratila, O.C.; Craciun, C. Ultrastructural evidence of mucosal healing after infliximab in patients with ulcerative colitis. J. Gastrointestin. Liver Dis. 2010, 19, 147–153. [Google Scholar] [PubMed]
- Biancone, L.; Ardizzone, S.; Armuzzi, A.; Castiglione, F.; D’Incà, R.; Danese, S.; Daperno, M.; Gionchetti, P.; Rizzello, F.; Scribano, M.L.; et al. Ustekinumab for treating ulcerative colitis: An expert opinion. Expert Opin. Biol. Ther. 2020, 20, 1321–1329. [Google Scholar] [CrossRef] [PubMed]
- Levin, A.D.; Wildenberg, M.E.; van den Brink, G.R. Mechanism of Action of Anti-TNF Therapy in Inflammatory Bowel Disease. J. Crohns Colitis 2016, 10, 989–997. [Google Scholar] [CrossRef]
| PICO Facets | Considerations |
|---|---|
| Patient (P) | Persons with histological diagnosis of IBD (CD e/o UC) |
| Intervention (I) | Therapy with monoclonal antibody |
| Comparison (C) | Therapy without monoclonal antibody |
| Outcome (O) | Histological difference in remission induced by Ab-monoclonal therapy compared to other therapies |
| Number of Reference | Author(s) | Year(s) | Type of Paper | Therapeutic Treatment | Endpoint of MH (Y/N) | Modification of MH |
|---|---|---|---|---|---|---|
| [1] | Baumgart et al. | 2007 | Review | Not applicable | Not applicable | Not applicable |
| [2] | Sairenji et al. | 2017 | Review | Not applicable | Not applicable | Not applicable |
| [9] | Boal Carvalho et al. | 2017 | Review | Not applicable | Not applicable | Not applicable |
| [18] | Arijs et al. | 2018 | Clinical Trial | Vedolizumab | Yes | 55% responders |
| [19] | Dai et al. | 2014 | Clinical Trial | Infliximab | No | Not applicable |
| [28] | Fiorino et al. | 2011 | Review | Not applicable | Not applicable | Not applicable |
| [33] | Neurath et al. | 2012 | Review | Not applicable | No | Not applicable |
| [34] | Ferrante et al. | 2012 | Review | Monoclonal Ab | Yes | Yes |
| [35] | Rogler et al. | 2012 | Review | Monoclonal Ab | Yes | Yes |
| [36] | Seidelin et al. | 2013 | Review | Monoclonal Ab | Yes | Yes |
| [37] | Osterman | 2013 | Review | Various therapy | Yes | Not applicable |
| [38] | Dulai et al. | 2015 | Review | Monoclonal Ab | No, but desirable | Not applicable |
| [39] | Florholmen | 2015 | Review | Monoclonal Ab | Yes | Yes |
| [40] | Yu et al. | 2015 | Original article | Infliximab (only CD) | Not, but desirable | Not applicable |
| [41] | Shah et al. | 2016 | Review with meta-analysis | Infliximab, Adalimumab Vedolizumab | Yes | Yes |
| [42] | Vickers et al. | 2016 | Review | Monoclonal Ab (only UC) | Yes | Not applicable |
| [43] | Reinink et al. | 2016 | Review | Various therapies | No | Not applicable |
| [44] | Eder et al. | 2016 | Original article | Monoclonal Ab | Yes | Yes |
| [45] | Cholapranee et al. | 2017 | Review | Monoclonal Ab | Yes | Yes |
| [46] | Kurashima et al. | 2017 | Review | Various therapies | Not applicable | Not applicable |
| [47] | Pantavou et al. | 2019 | Meta-analysis | Monoclonal Ab and Tofacinib (only UC) | Yes | Yes |
| [48] | Singh et al. | 2018 | Review | Monoclonal Ab | Yes | Yes |
| [49] | Leppkes et al. | 2018 | Editorial | Various therapies | No | Not applicable |
| [50] | Antonelli et al. | 2018 | Review | Monoclonal Ab and others oral therapies | Yes | Not applicable |
| [51] | Castiglione et al. | 2019 | Original article | Monoclonal Ab (only CD) | No | Not applicable |
| [52] | Park et al. | 2019 | Original article | Monoclonal Ab | No | Not applicable |
| [53] | Samaan et al. | 2019 | Review | Monoclonal Ab | Yes, deep histological remission | Yes |
| [21] | Pigneur et al. | 2019 | Randomized controlled trial | Monoclonal Ab (only childrens with CD) | Yes | Yes |
| [54] | Löwenberg et al. | 2019 | Original article | Vedolizumab (only CD) | Yes | Yes, 64% of patients |
| [22] | Li K et al. | 2019 | Clinical trial | Ustekinumab (only CD) | Yes | Yes |
| [55] | Pouillon et al. | 2019 | Review | Vedolizumab (only UC) | Yes | Yes |
| [56] | Cucchiara et al. | 2020 | Review | Monoclonal Ab | Yes | Not applicable |
| [23] | Nardone et al. | 2020 | Review | Monoclonal Ab | Yes | Not applicable |
| [57] | Petryszyn et al. | 2020 | Review | Infliximab Adalimumab Vedolizumab Tofacitinib (only UC) | Yes | Yes |
| [58] | Kucharzik et al. | 2020 | Review | Monoclonal Ab | Not applicable | Not applicable |
| [59] | Sagami et al. | 2020 | Comparative study | Monoclonal Ab | Yes | Not applicable |
| [60] | Li et al. | 2020 | Review | Ustekinumab (only UC) | Yes | Not applicable |
| Clinical Findings | Histological Findings | |
|---|---|---|
| Crohn disease (CD) | Perianal lesion common; frank bleeding less frequent than in UC | Transmural discontinous inflammation with fissuring, submucosal involvement, granuloma (25–28%), pseudopiloric metaplasia, globet cells preservation |
| Ulcerative colitis (UC) | Bloody diarrhea | Acute and chronic diffuse inflammatory infiltrate, depletion of globet cells, crypt abscesses, lymphoid aggregates, distorsion of crypts, basal plasmacytosis |
| Crohn Disease | Clinical MH Features | Histological MH Features |
|---|---|---|
| Infliximab | Reduction of Crohn Disease index of severity (CDEIS) and simple endoscopic score for Crohn disease (SES-CD) | Reduction of inflammatory infiltrate at normal levels. Reduction of epithelial damage. Persistence of crypt architecture. |
| Adalimumab | Reduction of Crohn’s disease activity index (PCDAI) and simple endoscopic score for Crohn disease (SES-CD) | Reduction of inflammatory infiltrate at normal levels. Reduction of epithelial damage. |
| Vedolizumab | Reduction of Crohn Di-sease index of severity (CDEIS) and simple endoscopic score for Crohn disease (SES-CD) | Reduction of inflammatory infiltrate with reduction of neutrophils. Reduction of epithelial damage. Persistence of crypt architecture. |
| Ustekinumab | Reduction of simple endoscopic score for Crohn disease (SES-CD) | Reduction of global histology activity scores (GHASs). |
| Ulcerative Colitis | ||
| Infliximab | Reduction of Mayo Endoscopic Score (MES) | Reduction of alterations of the intestinal epithelium, such as depletion of microvilli, crushing of epithelial junctions, cytoplasmic vacuolization. Restoration of the function of intracellular organelles. Reduction of pycnotic nuclei. Restoration of muciparous goblet cells with regular mucus formation and secretion. |
| Adalimumab Golimumab | Reduction of Ulcerative Colitis Endoscopic Index of Severity (UCEIS) | Restricting the inflammatory infiltrate and T-cell proliferation within the lamina propria. Downregulation of the expression of metalloproteinases and proinflammatory molecules. Restore the protective capabilities of the mucosa by reinforcing intestinal permeability and mucosal secretion, activating fibroblasts, and maintaining epithelial regeneration. |
| Vedolizumab | Ulcerative Colitis Endoscopic Index of Severity (UCEIS) | Limits both B- and T-cell lymphocyte fixation on the intestinal vascular endothelial cells and consequent migration to the lamina propria and tissue cells. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cazzato, G.; Colagrande, A.; Andriola, V.; Lettini, T.; Cicco, S.; Candance, P.M.V.; Resta, L.; Vincenti, L.; Ingravallo, G. Histological Hallmarks of Mucosal Healing in Inflammatory Bowel Diseases in the Era of Monoclonal Antibodies Therapy: New Insights and Perspectives. Diagnostics 2021, 11, 1570. https://doi.org/10.3390/diagnostics11091570
Cazzato G, Colagrande A, Andriola V, Lettini T, Cicco S, Candance PMV, Resta L, Vincenti L, Ingravallo G. Histological Hallmarks of Mucosal Healing in Inflammatory Bowel Diseases in the Era of Monoclonal Antibodies Therapy: New Insights and Perspectives. Diagnostics. 2021; 11(9):1570. https://doi.org/10.3390/diagnostics11091570
Chicago/Turabian StyleCazzato, Gerardo, Anna Colagrande, Valeria Andriola, Teresa Lettini, Sebastiano Cicco, Pragnell Mary Victoria Candance, Leonardo Resta, Leonardo Vincenti, and Giuseppe Ingravallo. 2021. "Histological Hallmarks of Mucosal Healing in Inflammatory Bowel Diseases in the Era of Monoclonal Antibodies Therapy: New Insights and Perspectives" Diagnostics 11, no. 9: 1570. https://doi.org/10.3390/diagnostics11091570
APA StyleCazzato, G., Colagrande, A., Andriola, V., Lettini, T., Cicco, S., Candance, P. M. V., Resta, L., Vincenti, L., & Ingravallo, G. (2021). Histological Hallmarks of Mucosal Healing in Inflammatory Bowel Diseases in the Era of Monoclonal Antibodies Therapy: New Insights and Perspectives. Diagnostics, 11(9), 1570. https://doi.org/10.3390/diagnostics11091570










