Synchronous Thyrolipoma and Papillary Thyroid Carcinoma: A Rare but Significant Event
Abstract
:1. Introduction
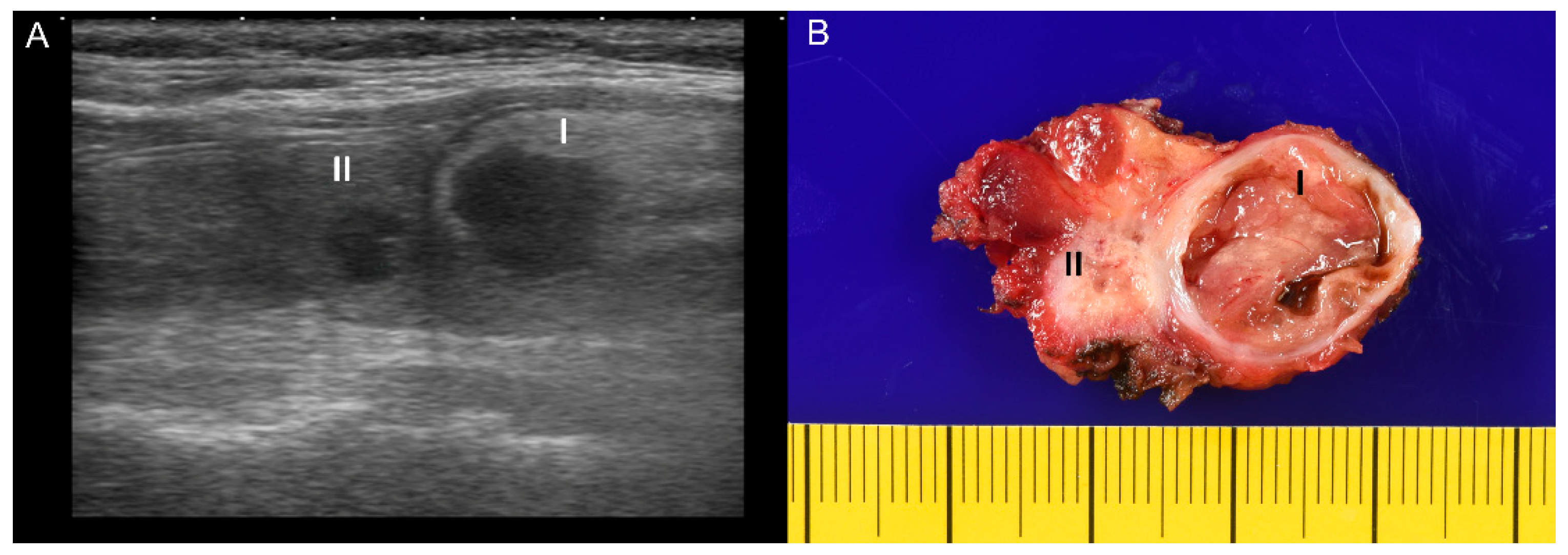
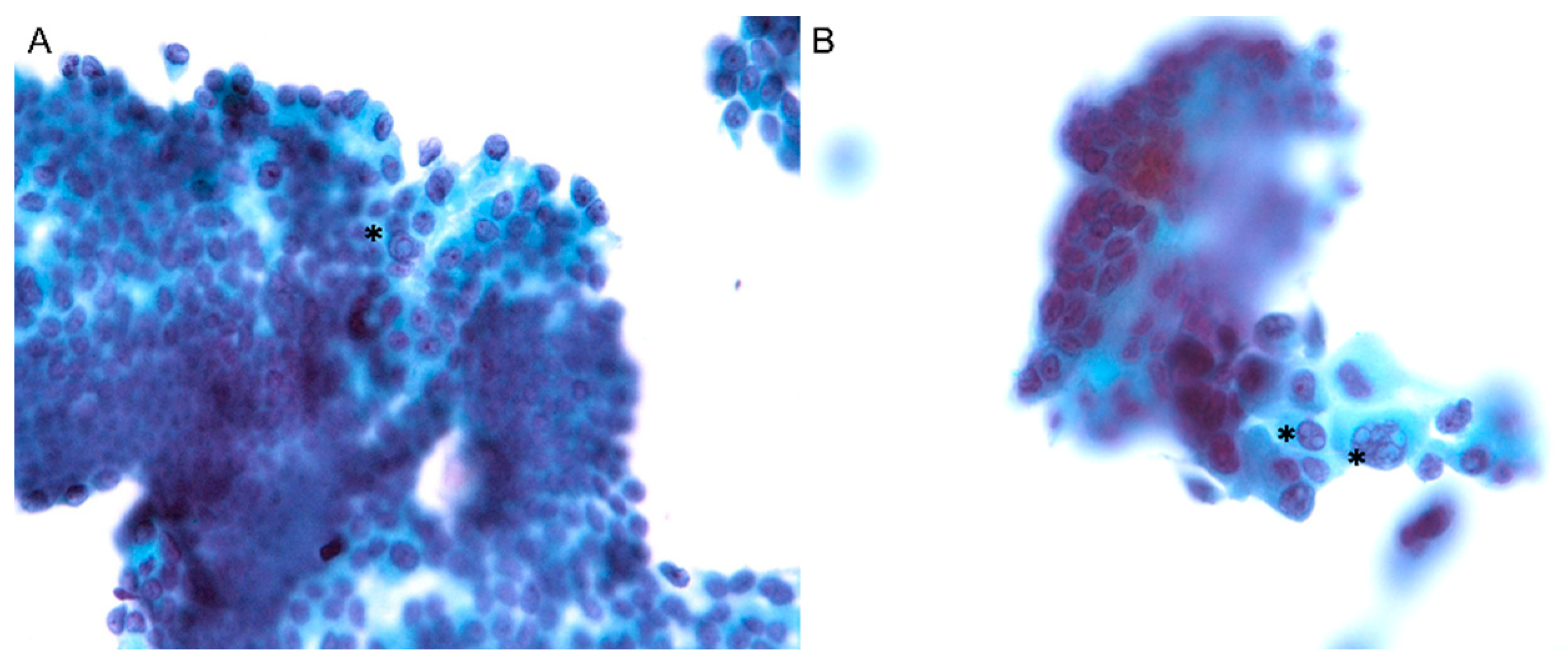
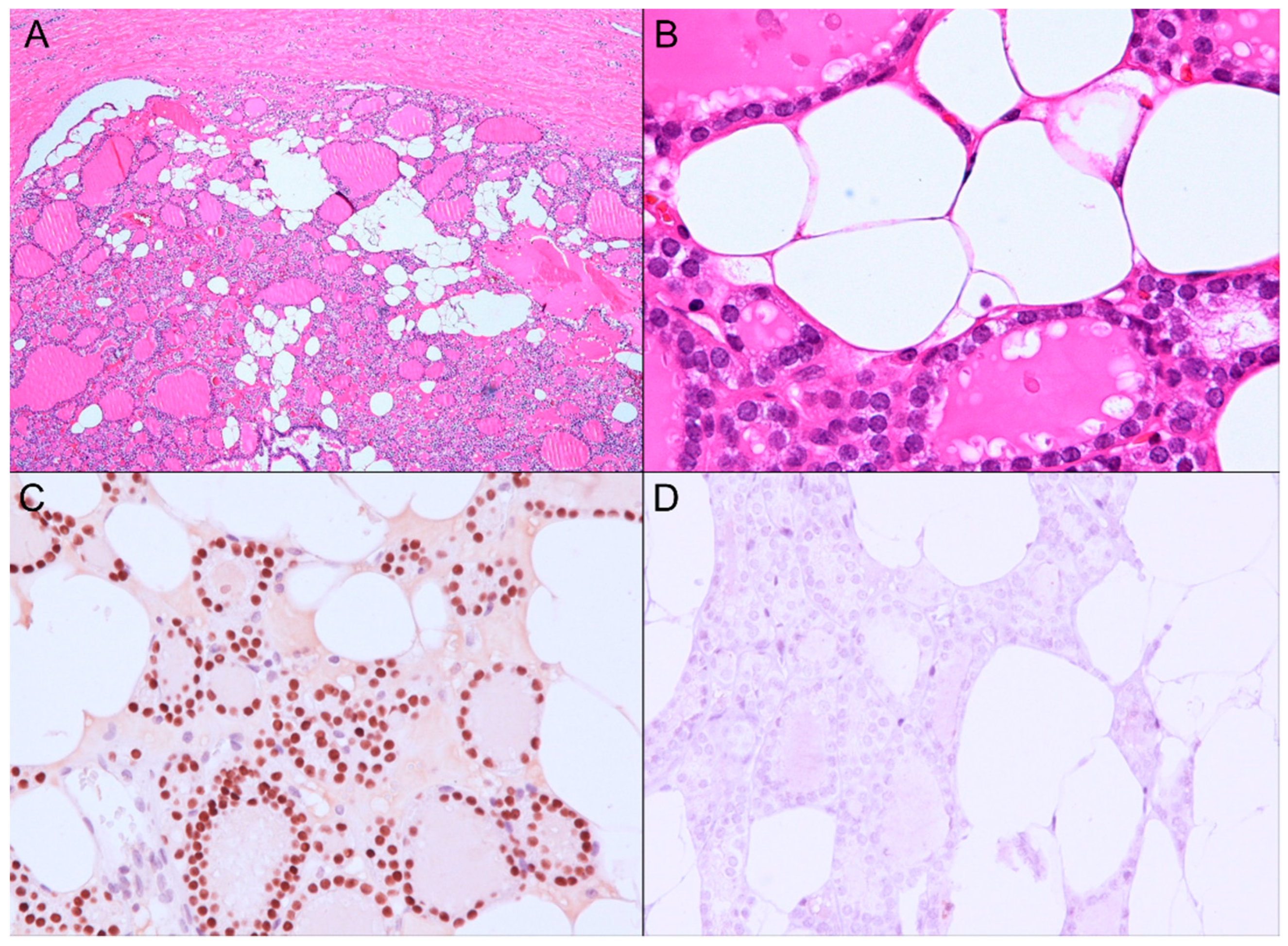
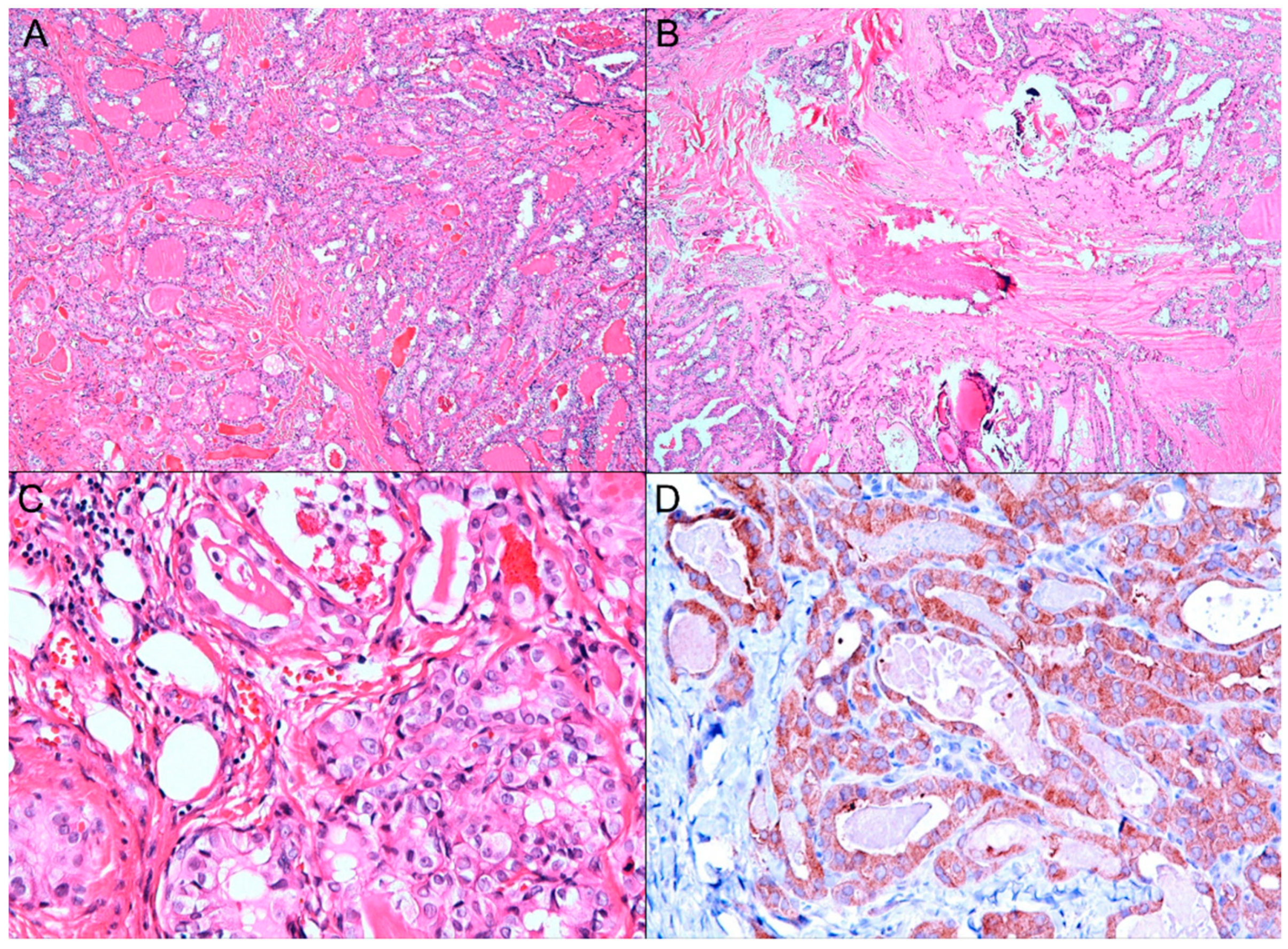
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nandyala, H.S.; Madapuram, S.; Yadav, M.; Katamala, S.K. Diffuse lipomatosis of the thyroid gland with papillary microcarcinoma: Report of a rare entity. Indian J. Pathol. Microbiol. 2015, 58, 348–350. [Google Scholar] [CrossRef]
- Steiner, T.; Péter, I.; Pogány, P.; Lantos, A.; Sándor, Z.; Téglás, M.; Koltai, P. Az autoimmun thyreoiditis, a kétoldali papillaris pajzsmirigy-carcinoma, a nyaki thyreolipoma és a diabetes mellitus együttes előfordulása. Orvosi. Hetilap. 2018, 159, 1024–1032. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cameselle-Teijeiro, J.; Fachal, C.; Cabezas-Agrícola, J.M.; Alfonsín-Barreiro, N.; Abdulkader, I.; Vega-Gliemmo, A.; Hermo, J.A. Thyroid Pathology Findings in Cowden Syndrome: A Clue for the Diagnosis of the PTEN Hamartoma Tumor Syndrome. Am. J. Clin. Pathol. 2015, 144, 322–328. [Google Scholar] [CrossRef] [Green Version]
- Butler, S.L.; Oertel, Y.C. Lipomas of anterior neck simulating thyroid nodules: Diagnosis by fine-needle aspiration. Diagn. Cytopathol. 1992, 8, 528–531. [Google Scholar] [CrossRef] [PubMed]
- Laforga, J.B.; Vierna, J. Adenoma of thyroid gland containing fat (thyrolipoma). Report of a case. J. Laryngol. Otol. 1996, 110, 1088–1089. [Google Scholar] [CrossRef] [PubMed]
- Rollins, S.D.; Flinner, R.L. Thyrolipoma: Diagnostic pitfalls in the cytologic diagnosis and review of the literature. Diagn. Cytopathol. 1991, 7, 150–154. [Google Scholar] [CrossRef] [PubMed]
- Cibas, E.S.; Ali, S.Z. The 2017 Bethesda System for Reporting Thyroid Cytopathology. Thyroid 2017, 27, 1341–1346. [Google Scholar] [CrossRef] [PubMed]
- Cherella, C.E.; Angell, T.E.; Richman, D.M.; Frates, M.C.; Benson, C.B.; Moore, F.D.; Barletta, J.A.; Hollowell, M.; Smith, J.R.; Alexander, E.K.; et al. Differences in Thyroid Nodule Cytology and Malignancy Risk Between Children and Adults. Thyroid 2019, 29, 1097–1104. [Google Scholar] [CrossRef] [PubMed]
| Cases [Reference] | Age, Sex | Size (cm) | Diagnosis | Other Findings |
|---|---|---|---|---|
| Nandyala et al. [1] | 37, M | 15 × 11 × 5 | Diffuse lipomatosis | PTC, nodular goiter, adenocarcinoma of ascending colon. |
| Steiner et al. [2] | 52, F | 4.0 × 3.5 × 2.2 | Thyrolipoma | Autoimmune thyroiditis, bilateral PTC, diabetes mellitus, hypertension, hypothyroidism, mass neck compression. |
| Cameselle-Teijeiro et al. [3] | 28, F | Multiple small nodules. | Thyrolipoma | Lymphocytic thyroiditis, multinodular goiter, PTC (follicular variant), lipoma of neck, Cowden syndrome. |
| Laforga et al. [5] | 58, F | 3.8 | Thyrolipoma | PTC |
| Current case | 51, F | 2.0 × 1.5 × 1.3 | Thyrolipoma | PTC, diabetes mellitus, hypertension. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuk, M.; Kuo, C.-J.; Nguyen, V.-H.; Chen, C.-C. Synchronous Thyrolipoma and Papillary Thyroid Carcinoma: A Rare but Significant Event. Diagnostics 2021, 11, 1334. https://doi.org/10.3390/diagnostics11081334
Kuk M, Kuo C-J, Nguyen V-H, Chen C-C. Synchronous Thyrolipoma and Papillary Thyroid Carcinoma: A Rare but Significant Event. Diagnostics. 2021; 11(8):1334. https://doi.org/10.3390/diagnostics11081334
Chicago/Turabian StyleKuk, Mariya, Chu-Jen Kuo, Van-Hung Nguyen, and Chien-Chin Chen. 2021. "Synchronous Thyrolipoma and Papillary Thyroid Carcinoma: A Rare but Significant Event" Diagnostics 11, no. 8: 1334. https://doi.org/10.3390/diagnostics11081334
APA StyleKuk, M., Kuo, C.-J., Nguyen, V.-H., & Chen, C.-C. (2021). Synchronous Thyrolipoma and Papillary Thyroid Carcinoma: A Rare but Significant Event. Diagnostics, 11(8), 1334. https://doi.org/10.3390/diagnostics11081334







