Electromyographic Assessment of Anterior Cruciate Ligament Injury Risk in Male Tennis Players: Which Role for Visual Input? A Proof-of-Concept Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Electromyography
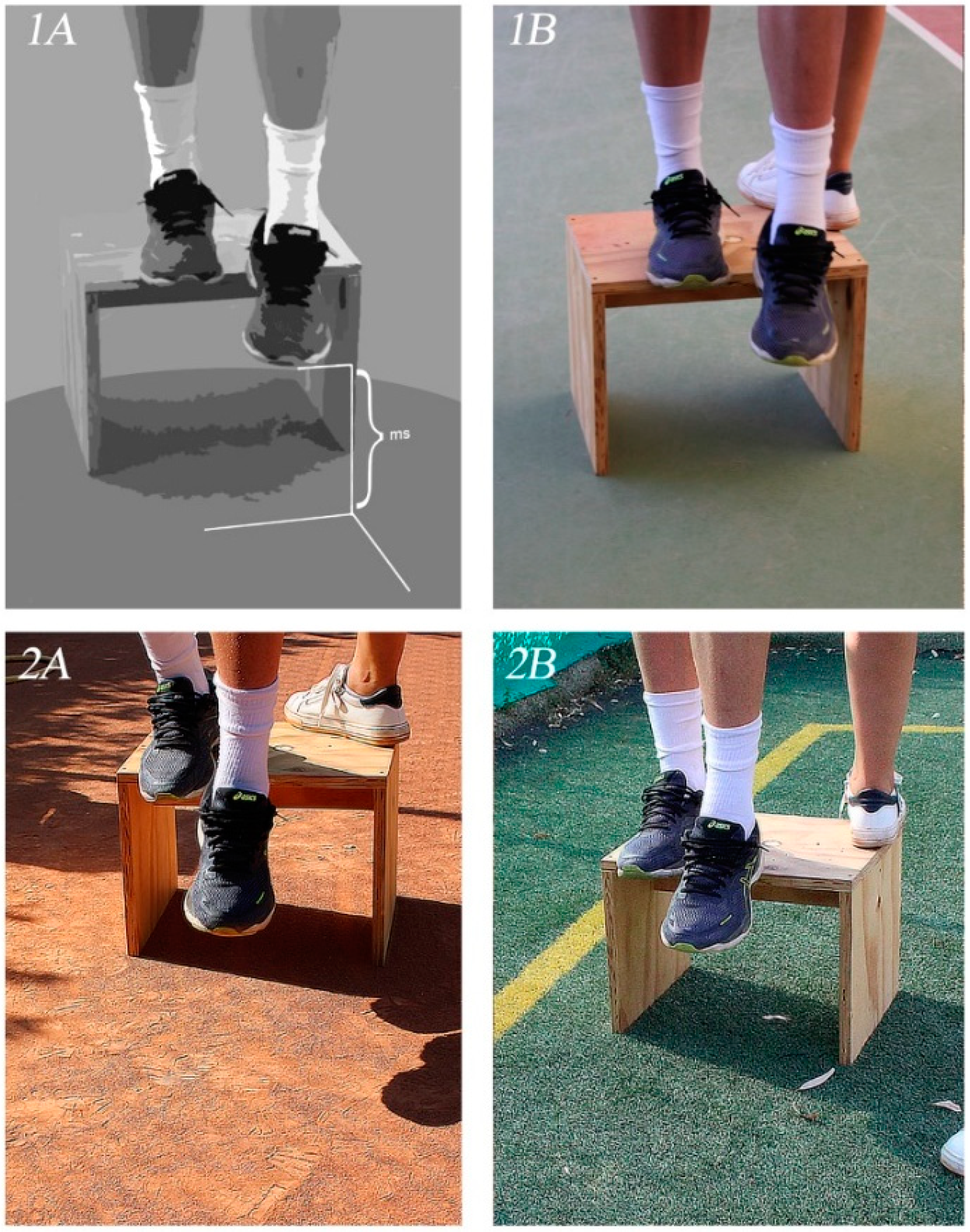
2.3. Drop Landing Test
2.4. Outcome Measures
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fu, M.C.; Ellenbecker, T.S.; Renstrom, P.A.; Windler, G.S.; Dines, D.M. Epidemiology of injuries in tennis players. Curr. Rev. Musculoskelet. Med. 2018, 11, 1–11. [Google Scholar] [CrossRef]
- Prieske, O.; Muehlbauer, T.; Krueger, T.; Kibele, A.; Behm, D.; Granacher, U. Sex-specific effects of surface instability on drop jump and landing biomechanics. Int. J. Sports Med. 2015, 36, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Moses, B.; Orchard, J.; Orchard, J. Systematic review: Annual incidence of ACL injury and surgery in various populations. Res. Sports Med. 2012, 20, 157–179. [Google Scholar] [CrossRef]
- Waldén, M.; Hägglund, M.; Magnusson, H.; Ekstrand, J. Anterior cruciate ligament injury in elite football: A prospective three-cohort study. Knee Surg. Sport. Traumatol. Arthrosc. 2011, 19, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Iolascon, G.; Gimigliano, F.; Moretti, A.; de Sire, A.; Migliore, A.; Brandi, M.L.; Piscitelli, P. Early osteoarthritis: How to define, diagnose, and manage. A systematic review. Eur. Geriatr. Med. 2017, 8, 383–396. [Google Scholar] [CrossRef]
- Gardinier, E.S.; Manal, K.; Buchanan, T.S.; Snyder-Mackler, L. Gait and neuromuscular asymmetries after acute anterior cruciate ligament rupture. Med. Sci. Sports Exerc. 2012, 44, 1490–1496. [Google Scholar] [CrossRef]
- Smeets, A.; Malfait, B.; Dingenen, B.; Robinson, M.A.; Vanrenterghem, J.; Peers, K.; Nijs, S.; Vereecken, S.; Staes, F.; Verschueren, S. Is knee neuromuscular activity related to anterior cruciate ligament injury risk? A pilot study. Knee 2019, 26, 40–51. [Google Scholar] [CrossRef] [PubMed]
- Medina, J.M.; Valovich McLeod, T.C.; Howell, S.K.; Kingma, J.J. Timing of neuromuscular activation of the quadriceps and hamstrings prior to landing in high school male athletes, female athletes, and female non-athletes. J. Electromyogr. Kinesiol. 2008, 18, 591–597. [Google Scholar] [CrossRef] [PubMed]
- Vigotsky, A.D.; Halperin, I.; Lehman, G.J.; Trajano, G.S.; Vieira, T.M. Interpreting signal amplitudes in surface electromyography studies in sport and rehabilitation sciences. Front. Physiol. 2018, 8, 985. [Google Scholar] [CrossRef] [PubMed]
- Zebis, M.K.; Andersen, L.L.; Bencke, J.; Kjær, M.; Aagaard, P. Identification of athletes at future risk of anterior cruciate ligament ruptures by neuromuscular screening. Am. J. Sports Med. 2009, 37, 1967–1973. [Google Scholar] [CrossRef]
- Marotta, N.; Demeco, A.; de Scorpio, G.; Indino, A.; Iona, T.; Ammendolia, A. Late activation of the vastus medialis in determining the risk of anterior cruciate ligament injury in soccer players. J. Sports Rehabil. 2020, 29, 952–955. [Google Scholar] [CrossRef] [PubMed]
- Youdas, J.W.; Hollman, J.H.; Hitchcock, J.R.; Hoyme, G.J.; Johnsen, J.J. Comparison of hamstring and quadriceps femoris electromyographic activity between men and women during a single-limb squat on both a stable and labile surface. J. Strength Cond. Res. 2007, 21, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Girard, O.; Micallef, J.P.; Millet, G.P. Effects of the playing surface on plantar pressures during the first serve in tennis. Int. J. Sports Physiol. Perform. 2010, 5, 384–393. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Serpell, B.G.; Scarvell, J.M.; Pickering, M.R.; Ball, N.B.; Newman, P.; Perriman, D.; Warmenhoven, J.; Smith, P.N. Medial and lateral hamstrings and quadriceps co-activation affects knee joint kinematics and ACL elongation: A pilot study. BMC Musculoskelet. Disord. 2015, 16, 1–11. [Google Scholar] [CrossRef]
- de Sire, A.; Demeco, A.; Marotta, N.; Moggio, L.; Palumbo, A.; Iona, T.; Ammendolia, A. Anterior Cruciate Ligament Injury Prevention Exercises: Could a Neuromuscular Warm-Up Improve Muscle Pre-Activation before a Soccer Game? A Proof-of-Principle Study on Professional Football Players. Appl. Sci. 2021, 11, 4958. [Google Scholar] [CrossRef]
- Gibson, J.J. The Ecological Approach to Visual Perception: Classic Edition; Psychology Press & Routledge Classic Editions; Psychology Press: Hove, UK, 1979; ISBN 9781848725775. [Google Scholar]
- Badcock, P.B.; Friston, K.J.; Ramstead, M.J.D.; Ploeger, A.; Hohwy, J. The hierarchically mechanistic mind: An evolutionary systems theory of the human brain, cognition, and behavior. Cogn. Affect. Behav. Neurosci. 2019, 19, 1319–1351. [Google Scholar] [CrossRef]
- Negrini, F.; de Sire, A.; Lazzarini, S.G.; Pennestrì, F.; Sorce, S.; Arienti, C.; Vitale, J.A. Reliability of activity monitors for physical activity assessment in patients with musculoskeletal disorders: A systematic review. J. Back Musculoskelet. Rehabil. 2021, 1–9. [Google Scholar] [CrossRef]
- Piacentini, M.F.; Minganti, C.; Ferragina, A.; Ammendolia, A.; Capranica, L.; Cibelli, G. Stress related changes during a half marathon in master endurance athletes. J. Sports Med. Phys. Fit. 2015, 55, 329–336. [Google Scholar]
- Segura-García, C.; Papaianni, M.C.; Caglioti, F.; Procopio, L.; Nisticò, C.G.; Bombardiere, L.; Ammendolia, A.; Rizza, P.; De Fazio, P.; Capranica, L. Orthorexia nervosa: A frequent eating disordered behavior in athletes. Eat. Weight Disord. 2012, 17. [Google Scholar] [CrossRef]
- Sherman, D.A.; Glaviano, N.R.; Norte, G.E. Hamstrings Neuromuscular Function After Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-Analysis. Sports Med. 2021, 1–19. [Google Scholar] [CrossRef]
- Sacco, I.C.N.; Gomes, A.A.; Otuzi, M.E.; Pripas, D.; Onodera, A.N. A method for better positioning bipolar electrodes for lower limb EMG recordings during dynamic contractions. J. Neurosci. Methods 2009, 180, 133–137. [Google Scholar] [CrossRef]
- Miljković, N.; Malešević, N.; Kojić, V.; Bijelić, G.; Keller, T.; Popović, D.B. Recording and assessment of evoked potentials with electrode arrays. Med. Biol. Eng. Comput. 2015, 53, 857–867. [Google Scholar] [CrossRef] [PubMed]
- Demeco, A.; Marotta, N.; Moggio, L.; Pino, I.; Marinaro, C.; Barletta, M.; Petraroli, A.; Palumbo, A.; Ammendolia, A. Quantitative analysis of movements in facial nerve palsy with surface electromyography and kinematic analysis. J. Electromyogr. Kinesiol. 2021, 56, 102485. [Google Scholar] [CrossRef]
- Hermens, H.J.; Freriks, B.; Disselhorst-Klug, C.; Rau, G. Development of recommendations for SEMG sensors and sensor placement procedures. J. Electromyogr. Kinesiol. 2000, 10, 361–374. [Google Scholar] [CrossRef]
- Marotta, N.; Demeco, A.; Moggio, L.; Isabello, L.; Iona, T.; Ammendolia, A. Correlation between dynamic knee valgus and quadriceps activation time in female athletes. J. Phys. Educ. Sport 2020, 20, 2508–2512. [Google Scholar] [CrossRef]
- Seifert, L.; Button, C.; Davids, K. Key properties of expert movement systems in sport: An ecological dynamics perspective. Sports Med. 2013, 43, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Araújo, D.; Davids, K.; Renshaw, I. Cognition, Emotion and Action in Sport. In Handbook of Sport Psychology; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2020. [Google Scholar]
- Myer, G.D.; Ford, K.R.; Brent, J.L.; Hewett, T.E. Differential neuromuscular training effects onACL injury risk factors in “high-risk” versus “low-risk” athletes. BMC Musculoskelet. Disord. 2007, 8, 39. [Google Scholar] [CrossRef] [PubMed]
- Heinrich, D.; van den Bogert, A.J.; Csapo, R.; Nachbauer, W. A model-based approach to predict neuromuscular control patterns that minimize ACL forces during jump landing. Comput. Methods Biomech. Biomed. Engin. 2020, 1–11. [Google Scholar] [CrossRef]
- Smeets, A.; Verschueren, S.; Staes, F.; Vandenneucker, H.; Claes, S.; Vanrenterghem, J. Athletes with an ACL reconstruction show a different neuromuscular response to environmental challenges compared to uninjured athletes. Gait Posture 2021, 83, 44–51. [Google Scholar] [CrossRef]
- Badiola-Zabala, A.; Massó-Ortigosa, N.; Cabedo-Sanromà, J.; Rey-Abella, F.; Milà, R.; Oviedo, G.R. Observational study with the objective of determining possible correlations between GRF and muscle activation at reception after a jump in an ACL injury. Apunt. Sports Med. 2020, 55, 63–70. [Google Scholar] [CrossRef]
- Nedergaard, N.J.; Dalbø, S.; Petersen, S.V.; Zebis, M.K.; Bencke, J. Biomechanical and neuromuscular comparison of single- and multi-planar jump tests and a side-cutting maneuver: Implications for ACL injury risk assessment. Knee 2020, 27, 324–333. [Google Scholar] [CrossRef] [PubMed]
- Minghelli, B.; Cadete, J. Epidemiology of musculoskeletal injuries in tennis players: Risk factors. J. Sports Med. Phys. Fitness. 2019, 59, 2045–2052. [Google Scholar] [CrossRef] [PubMed]
- Majewski, M.; Susanne, H.; Klaus, S. Epidemiology of athletic knee injuries: A 10-year study. Knee 2006, 13, 184–188. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.; Sorel, A.; Touzard, P.; Bideau, B.; Gaborit, R.; DeGroot, H.; Kulpa, R. Influence of the forehand stance on knee biomechanics: Implications for potential injury risks in tennis players. J. Sports Sci. 2020, 39, 992–1000. [Google Scholar] [CrossRef] [PubMed]
- Girard, O.; Eicher, F.; Fourchet, F.; Micallef, J.P.; Millet, G.P. Effects of the playing surface on plantar pressures and potential injuries in tennis. Br. J. Sports Med. 2007, 41, 733–738. [Google Scholar] [CrossRef]
- Clarke, J.; Carré, M.; Damm, L.; Dixon, S. The influence of surface characteristics on the tribological interactions at the shoe-surface interface in tennis. Procedia Eng. 2012, 34, 866–871. [Google Scholar] [CrossRef][Green Version]
- Barnett, T.; Pollard, G. How the tennis court surface affects player performance and injuries. Med. Sci. Tennis 2007, 12, 34–37. [Google Scholar]
- Breznik, K.; Batagelj, V. Retired matches among male professional tennis players. J. Sports Sci. Med. 2012, 11, 270–278. [Google Scholar]
- Rafols Parellada, L.; Linde, X.; Solà, J.; Fort, A.; Brau, J. Muscle activation during rehabilitation on artificial turf vs. sand after cruciate ligament surgery: A case series. Apunt. Sports Med. 2020, 55, 111–114. [Google Scholar] [CrossRef]
- Jacunski, M.; Rafferty, G.F. The effects of hypoxia and fatigue on skeletal muscle electromechanical delay. Exp. Physiol. 2020, 105, 842–851. [Google Scholar] [CrossRef]


| Presence or Absence of Visual Input | Different Tennis Court Surfaces | |||||
|---|---|---|---|---|---|---|
| Blindfolded | Not Blindfolded | p Value | Clay | Grass | p Value | |
| RF (ms) | 598.2 ± 62.9 | 552.5 ± 57.6 | p < 0.01 * | 552.4 ± 58.7 | 513.4 ± 74.3 | p < 0.01 * |
| VM (ms) | 204.9 ± 11.6 | 190.6 ± 12.2 | p < 0.01 * | 190.6 ± 12.2 | 137.3 ± 12.3 | p < 0.01 * |
| BF (ms) | 145.1 ± 9.1 | 127.9 ± 7.6 | p < 0.01 * | 125.9 ± 9.1 | 83.2 ± 12.3 | p < 0.01 * |
| MH (ms) | 129.9 ± 11.0 | 96.9 ± 7.1 | p < 0.01 * | 93.5 ± 9.1 | 72.4 ± 12.1 | p < 0.01 * |
| MH/RF | 0.22 ± 0.02 | 0.177 ± 0.02 | p < 0.01 * | 0.17 ± 0.02 | 0.14 ± 0.03 | p < 0.01 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Sire, A.; Marotta, N.; Demeco, A.; Moggio, L.; Paola, P.; Marotta, M.; Iona, T.; Invernizzi, M.; Leigheb, M.; Ammendolia, A. Electromyographic Assessment of Anterior Cruciate Ligament Injury Risk in Male Tennis Players: Which Role for Visual Input? A Proof-of-Concept Study. Diagnostics 2021, 11, 997. https://doi.org/10.3390/diagnostics11060997
de Sire A, Marotta N, Demeco A, Moggio L, Paola P, Marotta M, Iona T, Invernizzi M, Leigheb M, Ammendolia A. Electromyographic Assessment of Anterior Cruciate Ligament Injury Risk in Male Tennis Players: Which Role for Visual Input? A Proof-of-Concept Study. Diagnostics. 2021; 11(6):997. https://doi.org/10.3390/diagnostics11060997
Chicago/Turabian Stylede Sire, Alessandro, Nicola Marotta, Andrea Demeco, Lucrezia Moggio, Pasquale Paola, Marcello Marotta, Teresa Iona, Marco Invernizzi, Massimiliano Leigheb, and Antonio Ammendolia. 2021. "Electromyographic Assessment of Anterior Cruciate Ligament Injury Risk in Male Tennis Players: Which Role for Visual Input? A Proof-of-Concept Study" Diagnostics 11, no. 6: 997. https://doi.org/10.3390/diagnostics11060997
APA Stylede Sire, A., Marotta, N., Demeco, A., Moggio, L., Paola, P., Marotta, M., Iona, T., Invernizzi, M., Leigheb, M., & Ammendolia, A. (2021). Electromyographic Assessment of Anterior Cruciate Ligament Injury Risk in Male Tennis Players: Which Role for Visual Input? A Proof-of-Concept Study. Diagnostics, 11(6), 997. https://doi.org/10.3390/diagnostics11060997












