Interpretation of Near-Infrared Imaging in Acute and Chronic Wound Care
Abstract
1. Introduction
- Effects of factors that are known to delay wound healing;
- Impact revascularization plays directly on the wound;
- Adequacy of wound debridement;
- Response to advanced wound-care modalities (i.e., hyperbaric oxygen therapy, negative pressure wound therapy);
- Proper timing of placement of biologics to aid in wound healing; and
2. Guide to Near Infra-Red (NIR) Image Interpretation
2.1. Factors Contributing to Delayed Wound Healing
2.1.1. Chronic Wound Stalling in the Inflammatory Phase of Wound Healing
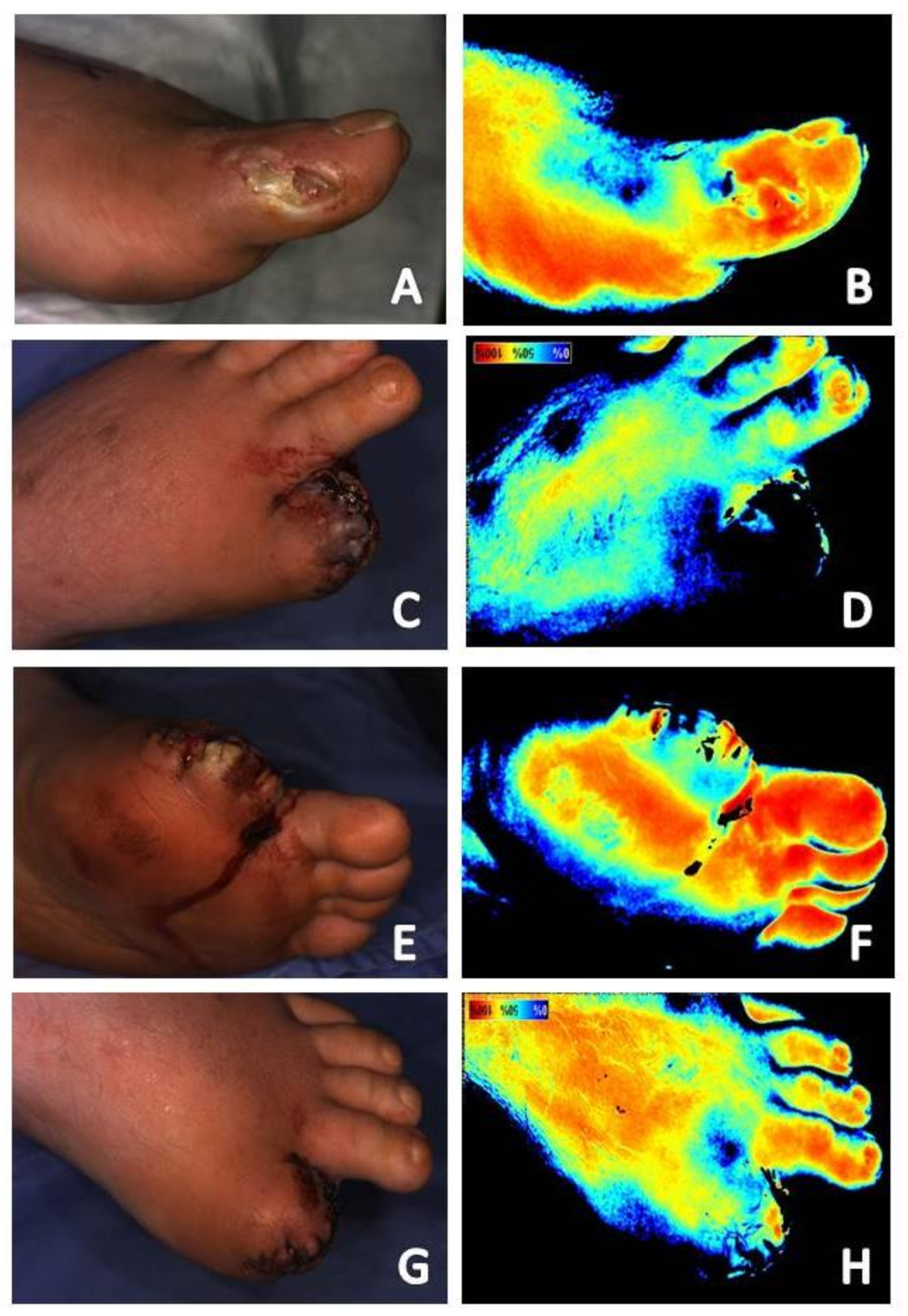
2.1.2. Local Ischemia
2.1.3. Infection
2.2. Factors Resulting in Variations in Tissue Thickness—Edema, Atrophic Tissue, Tissues, and Products within the Wound Bed
2.3. FactorsR in Variations in to Local Vasculature
2.3.1. Hyperbaric Oxygen Therapy
2.3.2. Use of Local Anesthetics with Epinephrine
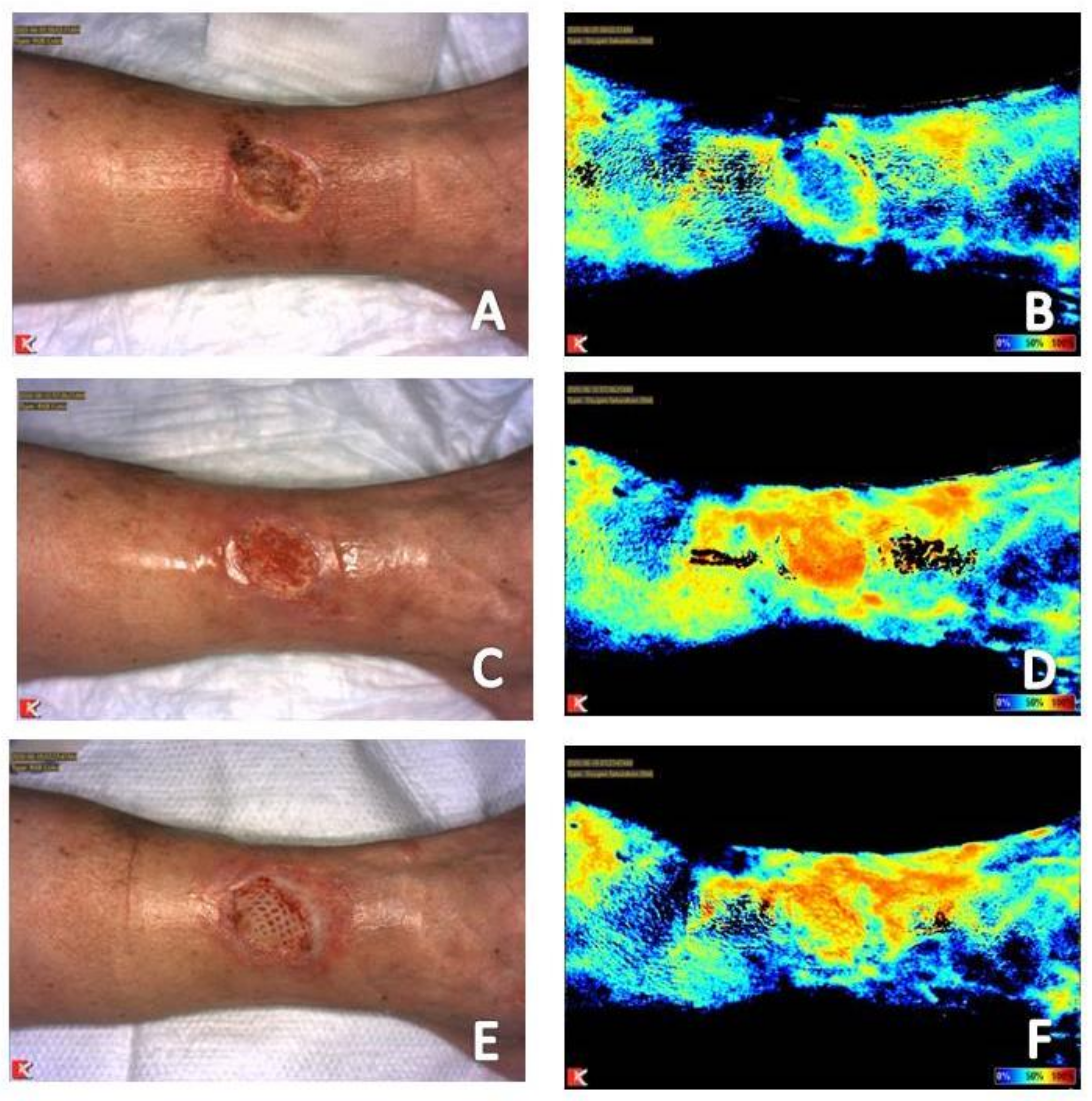
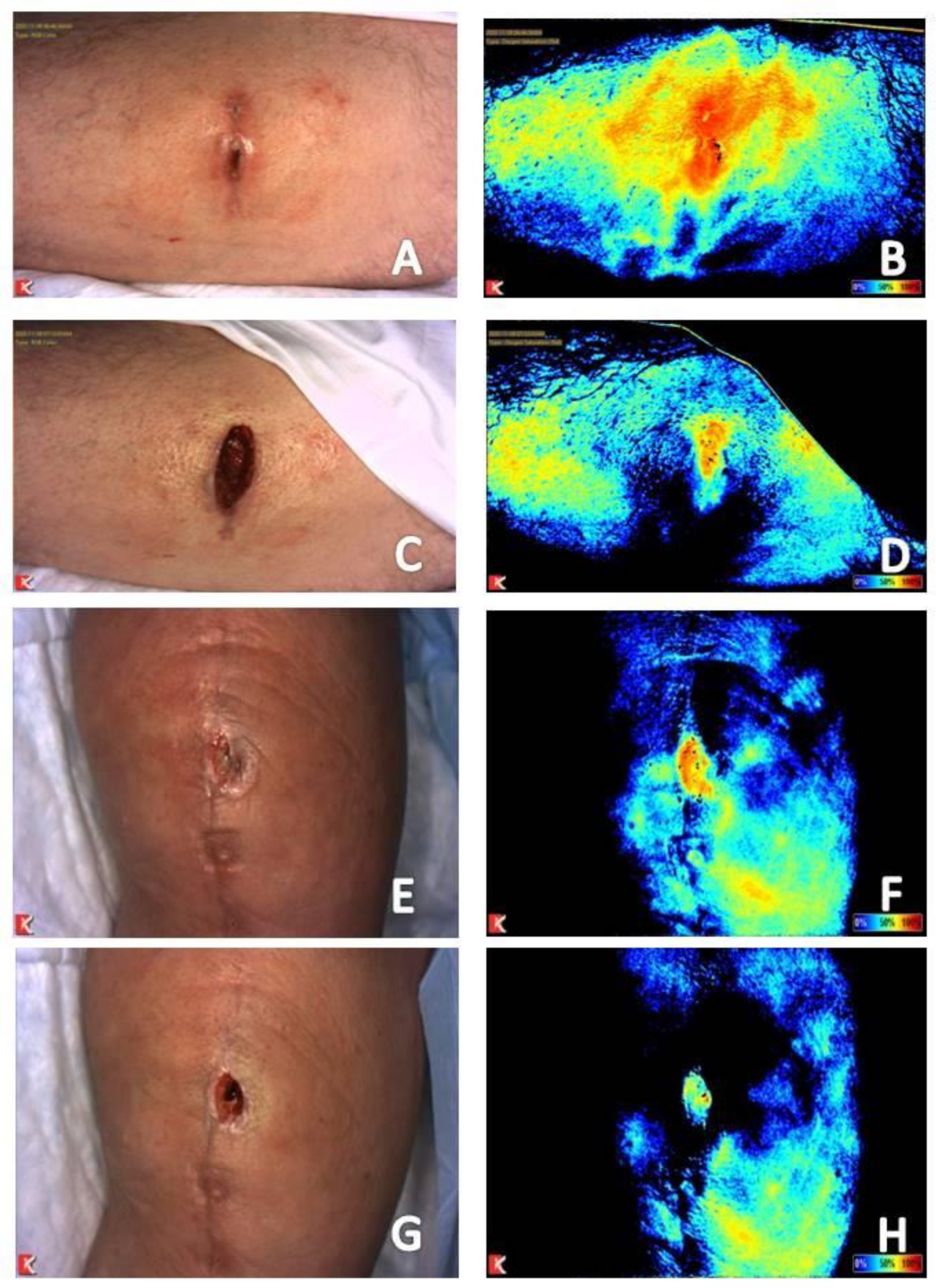
2.4. Imaging Analysis Consistent with a Wound Progressing toward Resolution
Progression from the Inflammatory to the Proliferative Phase of Wound Healing
3. Using NIR Image Interpretation to Guide Clinical Decision-Making for Expeditious and Optimal Patient Outcomes
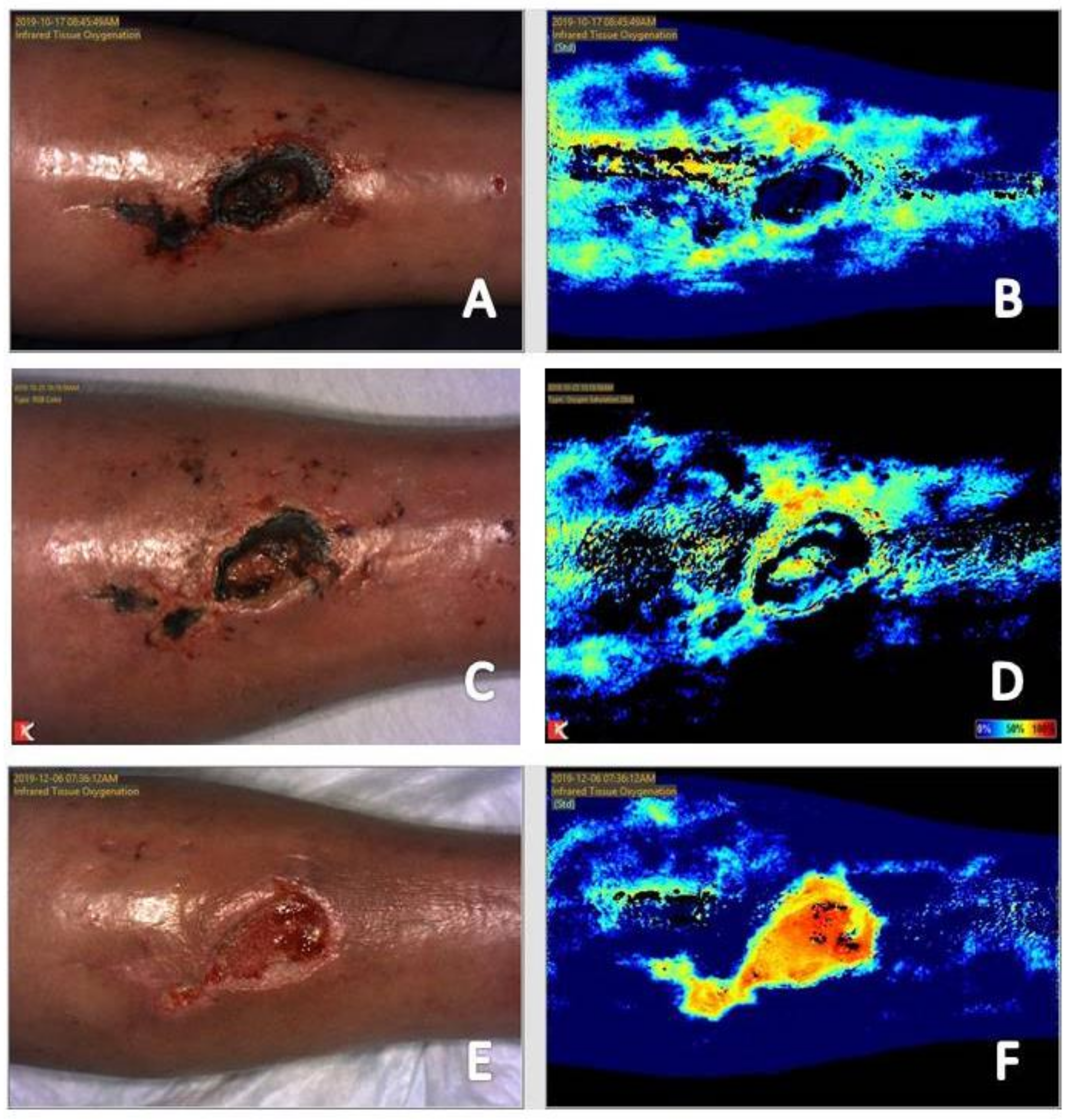
3.1. Wound Bed Preparation and Preoperative Planning
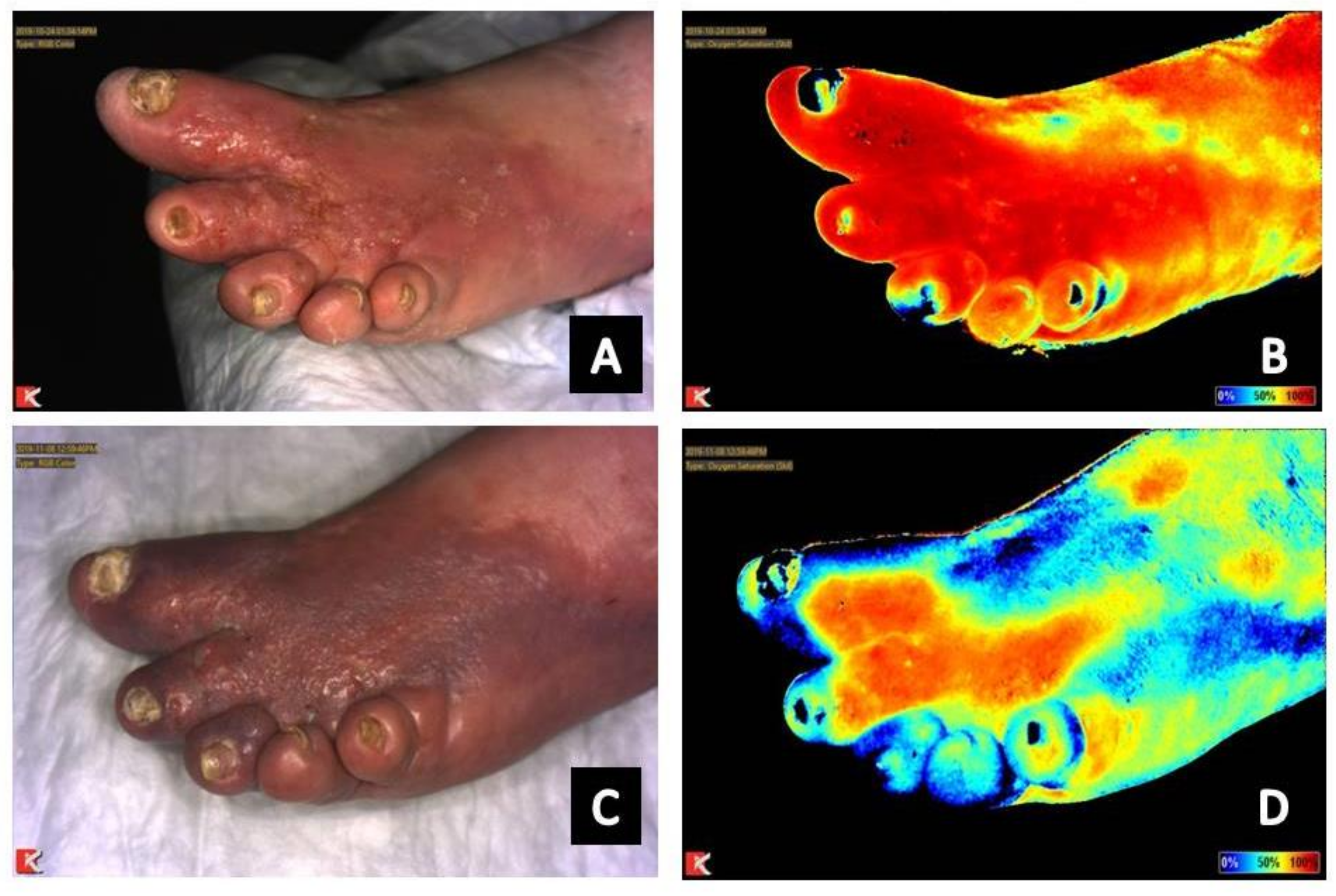
3.2. Supporting Information for Vascular Intervention When Routine Noninvasive Vascular Study Results Are Inconclusive or Unreliable
3.3. Response to Treatment
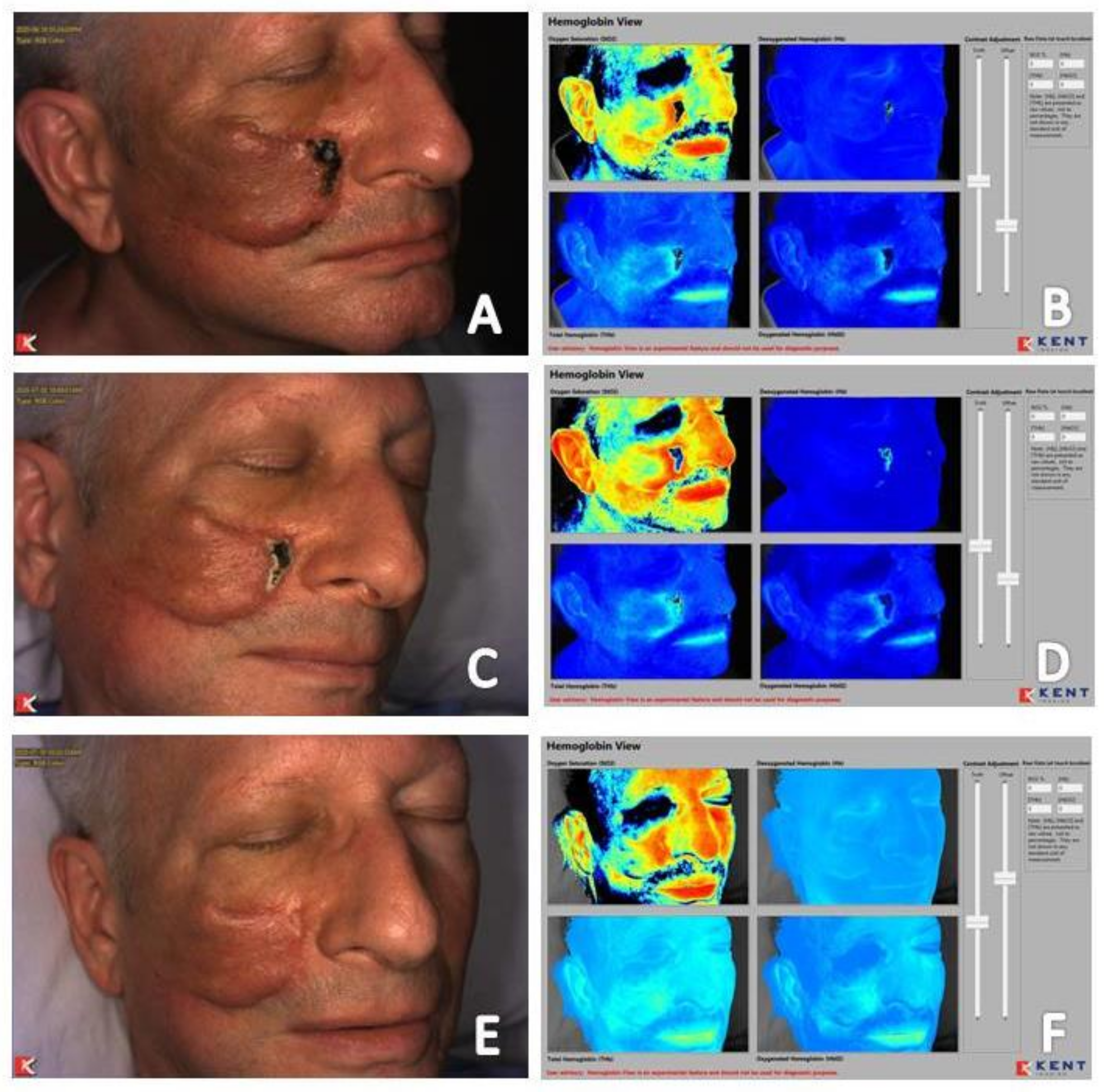
3.3.1. Resolving Infection
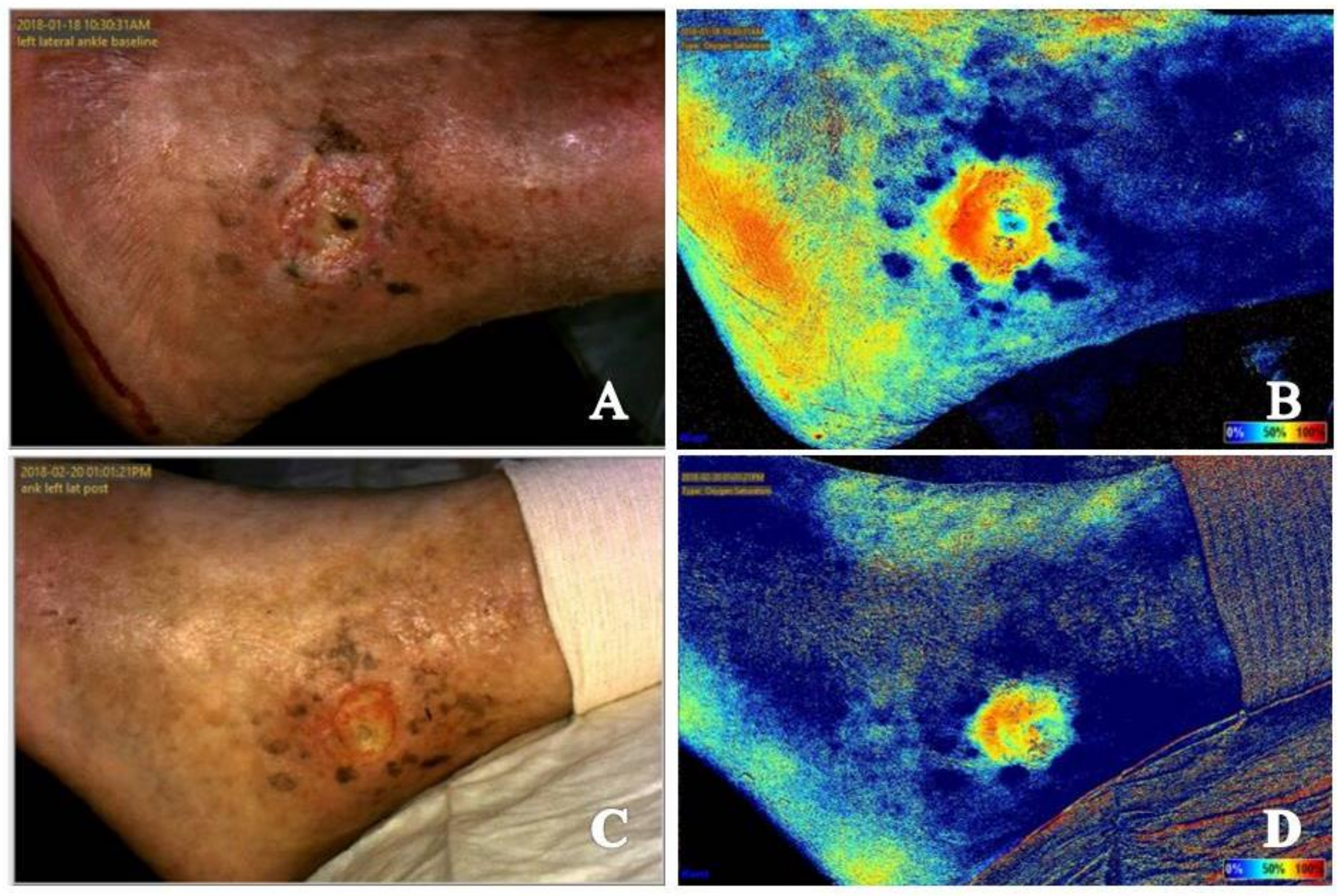
3.3.2. Compression Therapy
3.3.3. Hyperbaric Oxygen Therapy
3.4. Timing of Placement and Monitoring of Response to Use of Advanced Tissue Products
4. Summary
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gerhard-Herman, M.D.; Gornik, H.L.; Barrett, C.; Barshes, N.R.; Corriere, M.A.; Drachman, D.E.; Fleisher, L.A.; Fowkes, F.G.R.; Hamburg, N.M.; Kinlay, S.; et al. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: Executive summary. Vasc. Med. 2017, 22, NP1–NP43. [Google Scholar] [CrossRef]
- Londero, L.S.; Lindholt, J.S.; Thomsen, M.D.; Hoegh, A. Pulse palpation is an effective method for population-based screening to exclude peripheral arterial disease. J. Vasc. Surg. 2016, 63, 1305–1310. [Google Scholar] [CrossRef]
- Arnold, J.F. Vascular assessment of the lower extremity with a chronic wound. Surg. Clin. N. Am. 2020, 100, 807–822. [Google Scholar] [CrossRef]
- Schaper, N.C.; Andros, G.; Apelqvist, J.; Bakker, K.; Lammer, J.; Lepantalo, M.; Mills, J.L.; Reekers, J.; Shearman, C.P.; Zierler, R.E.; et al. Diagnosis and treatment of peripheral arterial disease in diabetic patients with a foot ulcer. A progress report of the International Working Group on the Diabetic Foot. Diabetes Metab. Res. Rev. 2012, 28, 218–224. [Google Scholar] [CrossRef]
- Aubert, C.E.; Cluzel, P.; Kemel, S.; Michel, P.-L.; Lajat-Kiss, F.; Dadon, M.; Hartemann, A.; Bourron, O. Influence of peripheral vascular calcification on efficiency of screening tests for peripheral arterial occlusive disease in diabetes—A cross-sectional study. Diabet Med. 2014, 31, 192–199. [Google Scholar] [CrossRef]
- Wang, Z.; Hasan, R.; Firwana, B.; Elraiyah, T.; Tsapas, A.; Prokop, L.; Mills, J.L.; Murad, M.H. A systematic review and meta-analysis of tests to predict wound healing in diabetic foot. J. Vasc. Surg. 2016, 63, 29S–36S. [Google Scholar] [CrossRef] [PubMed]
- Arnold, J.F. Is there adequate perfusion for healing? What routine noninvasive vascular studies are missing? Wounds 2018, 30, E89–E92. [Google Scholar] [PubMed]
- Braun, J.D.; Trinidad-Hernandez, M.; Perry, D.; Armstrong, D.G.; Mills, J.L. Early quantitative evaluation of indocyanine green angiography in patients with critical limb ischemia. J. Vasc. Surg. 2013, 57, 1213–1218. [Google Scholar] [CrossRef]
- Dooley, J.; Schirmer, J.; Slade, B.; Folden, B. Use of transcutaneous pressure of oxygen in the evaluation of edematous wounds. Undersea. Hyperb. Med. 1996, 23, 167–174. [Google Scholar] [PubMed]
- Tehan, P.E.; Bray, A.; Chuter, V.H. Noninvasive vascular assessment in the foot with diabetes: Sensitivity and specificity of the ankle brachial index, toe brachial index and continuous wave Doppler for detecting peripheral arterial disease. J. Diabetes Complicat. 2016, 30, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Xu, D.; Zou, L.; Xing, Y.; Hou, L.; Wei, Y.; Zhang, J.; Qiao, Y.; Hu, D.; Xu, Y.; Li, J.; et al. Diagnostic value of ankle-brachial index in peripheral arterial disease: A meta-analysis. Can. J. Cardiol. 2013, 29, 492–498. [Google Scholar] [CrossRef] [PubMed]
- Yip, W.L. Influence of oxygen on wound healing. Int. Wound J. 2015, 12, 620–624. [Google Scholar] [CrossRef]
- Sheffield, P.J. Tissue oxygen measurements with respect to soft tissue wound healing with normobaric and hyperbaric oxygen. HBO Rev. 1985, 6, 18–46. [Google Scholar]
- Arsenault, K.A.; Al-Otaibi, A.; Devereaux, P.J.; Thorlund, K.; Tittley, J.G.; Whitlock, R.P. The use of transcutaneous oximetry to predict healing complications of lower limb amputations: A systematic review and meta-analysis. Eur. J. Vasc. Endovasc. Surg. 2012, 43, 329–336. [Google Scholar] [CrossRef]
- Mukherjee, R.; Tewary, S.; Routray, A. Diagnostic and prognostic utility of non-invasive multimodal imaging in chronic wound monitoring: A systematic review. J. Med. Syst. 2017, 41, 46. [Google Scholar] [CrossRef]
- Mothes, H.; Dönicke, T.; Friedel, R.; Simon, M.; Markgraf, E.; Bach, O. Indocyanine-green fluorescence video angiography used clinically to evaluate tissue perfusion in microsurgery. J. Trauma Acute Care Surg. 2004, 57, 1018–1024. [Google Scholar] [CrossRef]
- Zimmerman, A.; Roenneberg, C.; Reeps, C.; Wendorff, H.; Holzbach, T.; Eckstein, H.H. The determination of tissue perfusion and collateralization in peripheral arterial disease with indocyanine green fluorescence angiography. Clin. Hem. Micro. 2012, 50, 157–166. [Google Scholar] [CrossRef]
- Li, W.W.; Arnold, J. Imaging of the chronic wound and the emerging role of fluorescence mircoangiography. Today’s Wound Clinic 2014, 8, S1–S4. [Google Scholar]
- Arnold, J.F.; Roscum, M. The explore trial: A feasibility study using fluorescence angiography to evaluate perfusion in the oxygen-rich environment. Surg. Technol. Int. 2016, 29, 61–79. [Google Scholar] [PubMed]
- Landsman, A. Visualization of wound healing progression with near infrared spectroscopy: A retrospective study. Wounds 2020, 32, 265–271. [Google Scholar] [PubMed]
- Kang, Y.; Lee, J.; Kwon, K.; Choi, C. Dynamic fluorescence imaging of indocyanine green for reliable and sensitive diagnosis of peripheral vascular insufficiency. Microvasc. Res. 2010, 80, 552–555. [Google Scholar] [CrossRef]
- Igari, K.; Kudo, T.; Toyofuku, T.; Jibiki, M.; Inoue, Y.; Kawano, T. Quantitative evaluation of the outcomes of revascularization procedures for peripheral arterial disease using indocyanine green angiography. Eur. J. Vasc. Endovasc. Surg. 2013, 46, 460–465. [Google Scholar] [CrossRef]
- Zimmerman, A.; Roenneberg, C.; Wendorff, H.; Holzbach, T.; Giunta, R.E.; Eckstein, H.H. Early postoperative detection of tissue necrosis in amputation stumps with indocyanine green fluorescence angiography. Vas. Endovas. Surg. 2010, 44, 269–273. [Google Scholar] [CrossRef]
- Igari, K.; Kudo, T.; Uchiyama, H.; Toyofuku, T.; Inoue, Y. Indocyanine green angiography for the diagnosis of peripheral arterial disease with isolated infrapopliteal lesions. Ann. Vasc. Surg. 2014, 28, 1479–1484. [Google Scholar] [CrossRef]
- Igari, K.; Kudo, T.; Uchiyama, H.; Toyofuku, T.; Inoue, Y. Intraarterial injection of indocyanine green for evaluation of peripheral blood circulation in patients with peripheral arterial disease. Ann. Vasc. Surg. 2014, 28, 1280–1285. [Google Scholar] [CrossRef] [PubMed]
- Arnold, J.F.; Marmolejo, V. Visualization of angiogenesis and vasculogenesis in a late tissue radiation injury of the chest wall treated with adjuvant hyperbaric oxygen therapy using fluorescence angiography. Undersea Hyperb. Med. 2019, 46, 69–73. [Google Scholar] [CrossRef]
- Marmolejo, V.S.; Arnold, J.F. The Ability of fluorescence angiography to detect local ischemia in patients with heel ulceration. Foot Ankle Spec. 2018, 11, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, M.; Cettolo, V.; Quaresima, V. Light source-detector spacing of near-infrared-based tissue oximeters and the influence of skin blood flow. J. Appl. Physiol. 2006, 100, 1426, author reply 1427. [Google Scholar] [CrossRef]
- Matsushita, K.; Homma, S.; Okada, E. Influence of adipose tissue on muscle oxygenation measurement with NIRS instrument. In Photon Propagation in Tissue. III. Proceedings of the SPIE; Benaron, D.A., Chance, B., Ferrari, M., Bellingham, W.A., Eds.; International Society for Optical Engineering: Bellingham, WA, USA, 1998; Volume 3194, pp. 151–165. [Google Scholar]
- Niwayama, M.; Lin, L.; Shao, J.; Kudo, N.; Yamamoto, K. Quantitative measurement of muscle hemoglobin oxygenation using near-infrared spectroscopy with correction for the influence of a subcutaneous fat layer. Rev. Sci. Instr. 2000, 71, 4571–4575. [Google Scholar] [CrossRef]
- O’Meara, S.; Cullum, N.; Nelson, E.A.; Dumville, J.C. Compression for venous leg ulcers. Cochrane Database Syst. Rev. 2012, 14, 11. [Google Scholar] [CrossRef] [PubMed]
- Thom, S.R. Hyperbaric oxygen: Its mechanisms and efficacy. Plast. Reconstr. Surg. 2011, 127, 131S–141S. [Google Scholar] [CrossRef]
- Munabi, N.C.O.; Olorunnipa, O.B.; Goltsman, D.; Rohde, C.H.; Ascherman, J.A. The ability of intra-operative perfusion mapping with laser-assisted indocyanine green angiography to predict mastectomy flap necrosis in breast reconstruction: A prospective trial. J. Plast. Reconstr. Aesthet. Surg. 2014, 67, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, G.S.; Cooper, D.M.; Knighton, D.R.; Margolis, D.J.; Pecoraro, R.E.; Rodeheaver, G.; Robson, M.C. Definitions and guidelines for assessment of wounds and evaluation of healing. Arch. Dermatol. 1994, 130, 489–493. [Google Scholar] [CrossRef]
- Pérez-Panero, A.J.; Ruiz-Muñoz, M.; Cuesta-Vargas, A.I.; Gónzalez-Sánchez, M. Prevention, assessment, diagnosis and management of diabetic foot based on clinical practice guidelines: A systematic review. Medicine 2019, 98, e16877. [Google Scholar] [CrossRef]
- Tyrell, R.; Kilmartin, C.; Acevedo, E.; Keshavamurthy, S.; Gassman, A. Is non-invasive indocyanine-green angiography a useful adjunct for the debridement of infected sternal wounds? JPRAS Open 2018, 16, 117–120. [Google Scholar] [CrossRef]
- Johnson-Arbor, K.; Falola, R.; Kelty, J.; Barbour, J.; Attinger, C. Use of indocyanine green fluorescent angiography in a hyperbaric patient with soft tissue radiation necrosis: A case report. Undersea. Hyperb. Med. 2017, 44, 273–278. [Google Scholar] [CrossRef]
- Rammos, C.K.; Jones, G.E.; Taege, S.M.; Lemaster, C.M. The use of multispectral imaging in diep free flap perforator selection: A case study. Plast. Reconstr. Surg. Glob. Open 2020, 8, e3245. [Google Scholar] [CrossRef]
- Willenberg, T.; Lun, B.; Amsler, F.; Baumgartner, I. Ease of application of medical compression-stocking systems for the treatment of venous ulcers. Eur. J. Vasc. Endovasc. Surg. 2010, 40, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Zeng-Treitler, Q.; Perri, S.; Nakamura, C.; Kuang, J.; Hill, B.; Bui, D.D.; Stoddard, G.J.; Bray, B.E. Evaluation of a pictograph enhancement system for patient instruction: A recall study. J. Am. Med. Inform. Assoc. 2014, 21, 1026–1031. [Google Scholar] [CrossRef]
- Meppelink, C.S.; van Weert, J.C.; Haven, C.J.; Smit, E.G. The effectiveness of health animations in audiences with different health literacy levels: An experimental study. J. Med. Internet Res. 2015, 17, e11. [Google Scholar] [CrossRef]
- Schillinger, D.; Piette, J.; Grumbach, K.; Wang, F.; Wilson, C.; Daher, C.; Leong-Grotz, K.; Castro, C.; Bindman, A.B. Closing the loop: Physician communication with diabetic patients who have low health literacy. Arch. Intern. Med. 2003, 163, 83–90. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, D.M.; Waite, K.R.; Curtis, L.M.; Engel, K.G.; Baker, D.W.; Wolf, M.S. What did the doctor say? Health literacy and recall of medical instructions. Med. Care 2012, 50, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Nauta, T. Hypoxic signaling during tissue repair and regenerative medicine. Int. J. Mol. Sci. 2014, 15, 19791–19815. [Google Scholar] [CrossRef]
- Laschke, M.W.; Menger, M.D. Adipose tissue-derived microvascular fragments: Natural vascularization units for regenerative medicine. Trends Biotechnol. 2015, 33, 442–448. [Google Scholar] [CrossRef] [PubMed]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arnold, J.; Marmolejo, V.L. Interpretation of Near-Infrared Imaging in Acute and Chronic Wound Care. Diagnostics 2021, 11, 778. https://doi.org/10.3390/diagnostics11050778
Arnold J, Marmolejo VL. Interpretation of Near-Infrared Imaging in Acute and Chronic Wound Care. Diagnostics. 2021; 11(5):778. https://doi.org/10.3390/diagnostics11050778
Chicago/Turabian StyleArnold, Jonathan, and Valerie L. Marmolejo. 2021. "Interpretation of Near-Infrared Imaging in Acute and Chronic Wound Care" Diagnostics 11, no. 5: 778. https://doi.org/10.3390/diagnostics11050778
APA StyleArnold, J., & Marmolejo, V. L. (2021). Interpretation of Near-Infrared Imaging in Acute and Chronic Wound Care. Diagnostics, 11(5), 778. https://doi.org/10.3390/diagnostics11050778




