Percutaneous C-Arm Free O-Arm Navigated Biopsy for Spinal Pathologies: A Technical Note
Abstract
1. Introduction
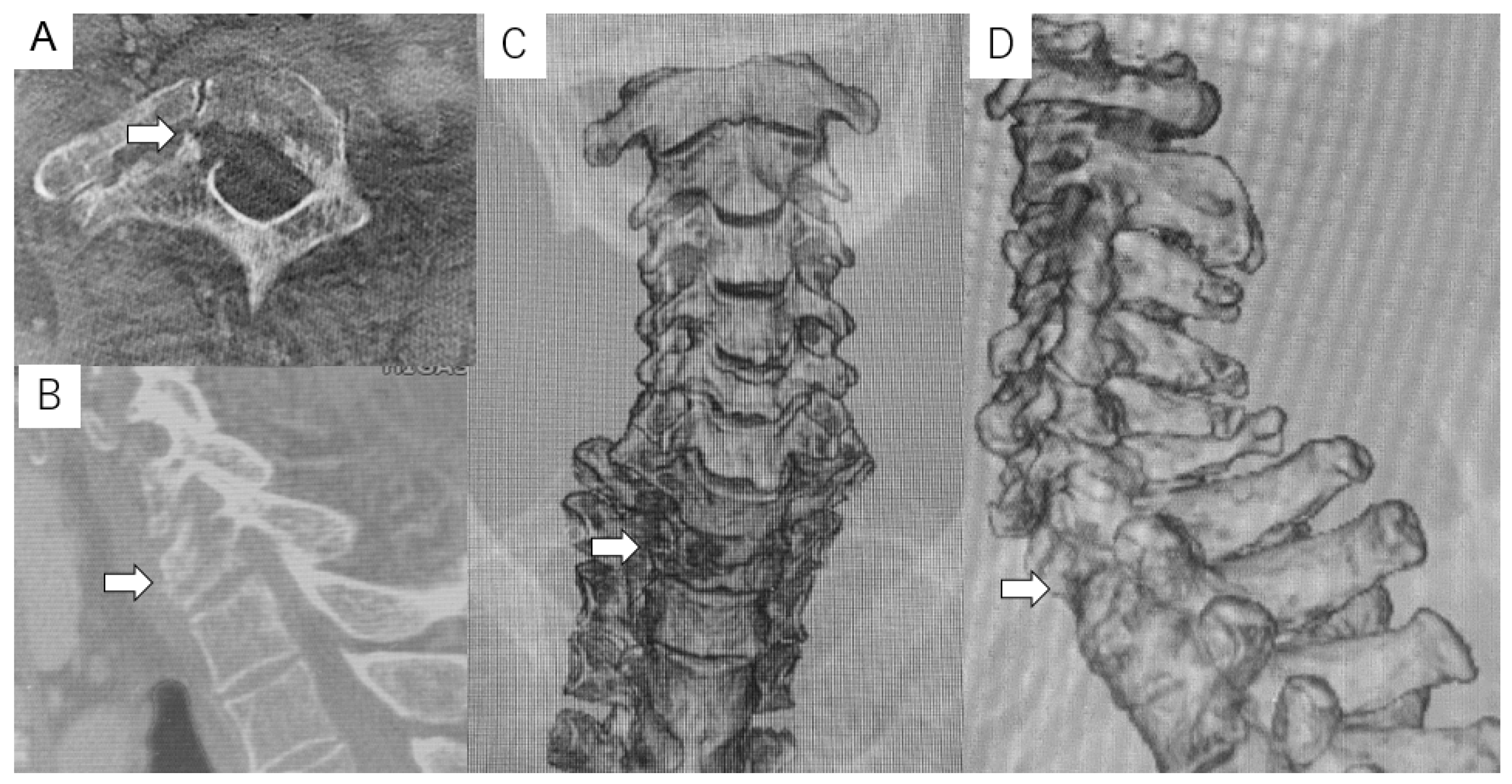
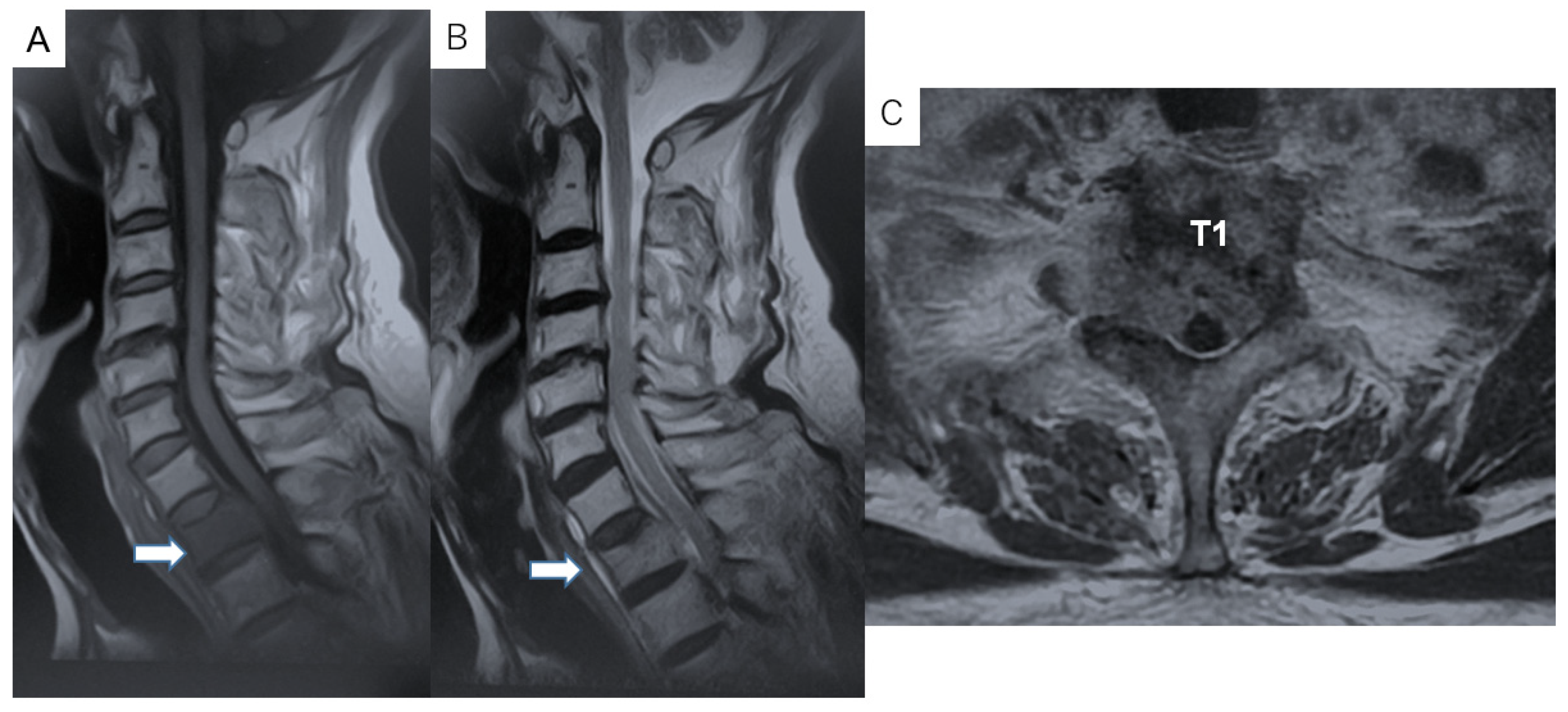
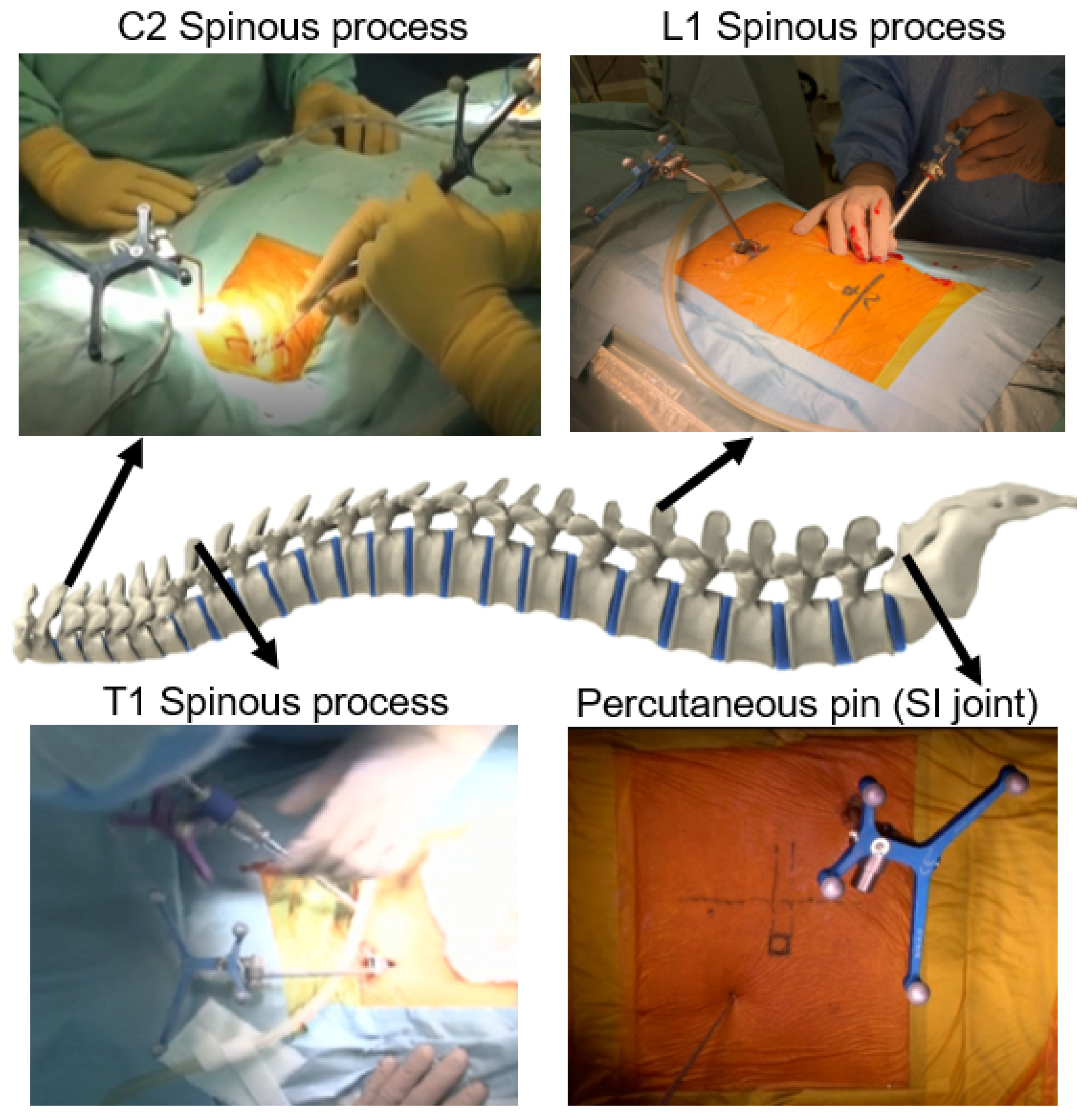
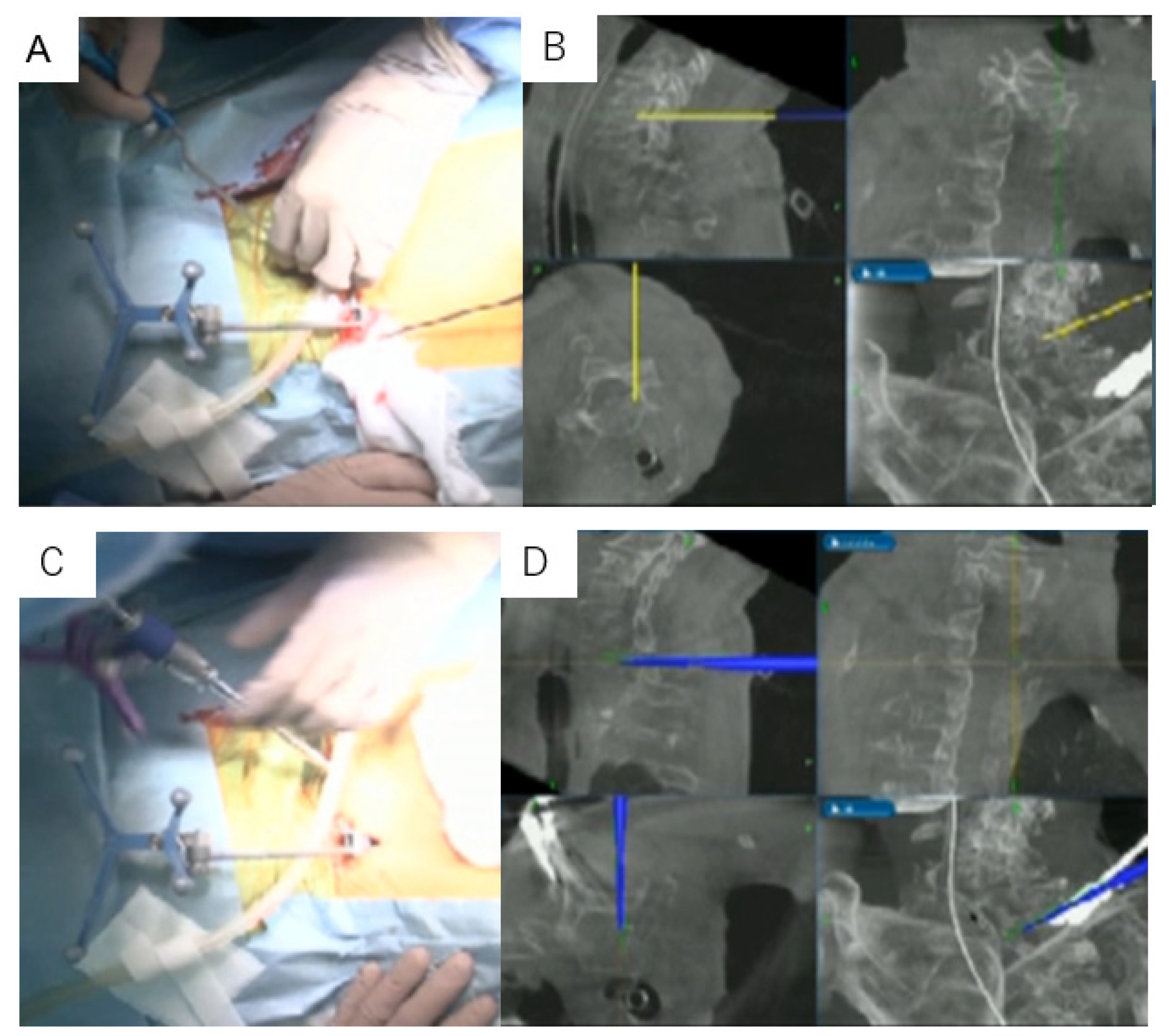
2. Methods
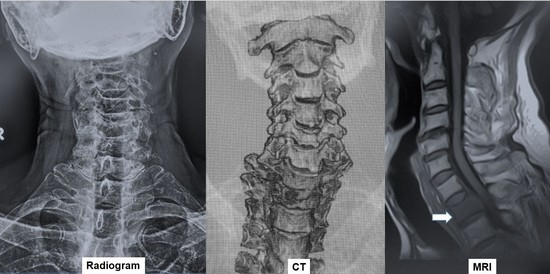
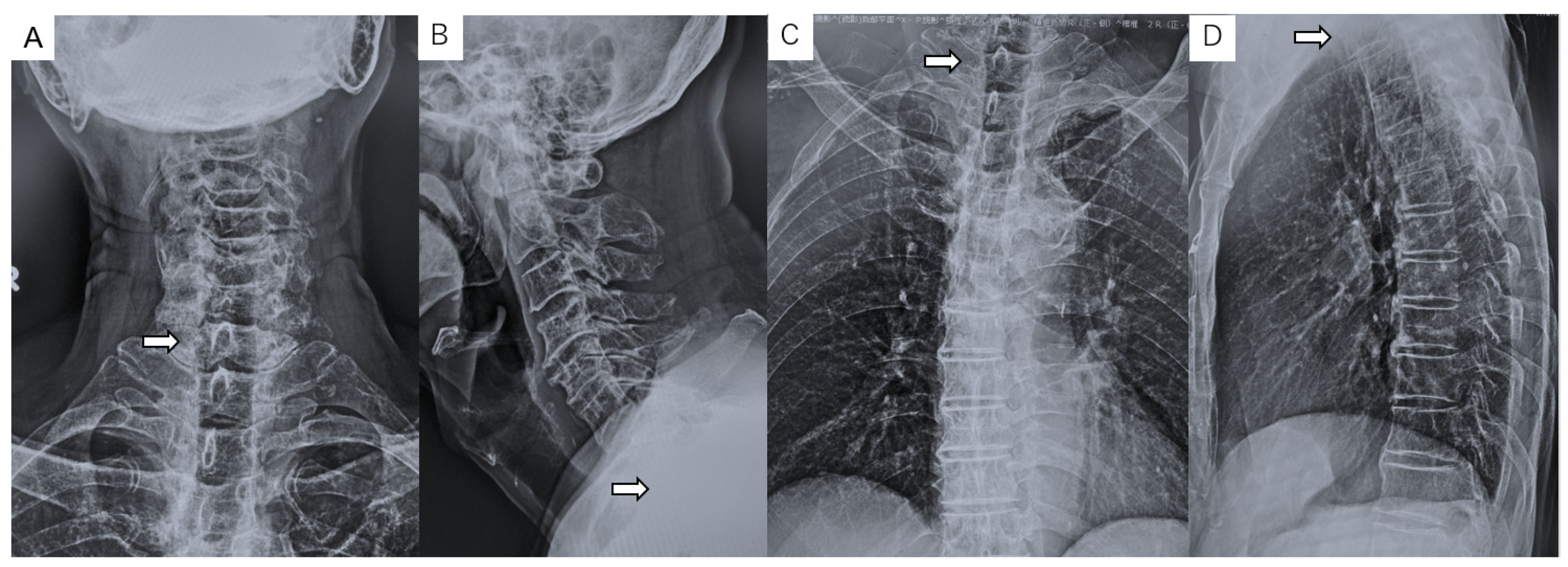
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hosono, N.; Yonenobu, K.; Fuji, T.; Ebara, S.; Yamashita, K.; Ono, K. Orthopaedic management of spinal metastases. Clin. Orthop. Relat. Res. 1995, 312, 148–159. [Google Scholar]
- Harrington, K.D. Orthopedic surgical management of skeletal complications of malignancy. Cancer 1997, 80 (Suppl. S8), S1614–S1627. [Google Scholar] [CrossRef]
- Gokaslan, Z.L.; York, J.E.; Walsh, G.L.; McCutcheon, I.E.; Lang, F.F.; Putnam, J.B., Jr.; Sawaya, R. Transthoracic vertebrectomy for metastatic spinal tumors. J. Neurosurg. 1998, 89, 599–609. [Google Scholar] [CrossRef] [PubMed]
- Findlay, J.M.; Bernstein, M.; Vanderlinden, R.G.; Resch, L. Microsurgical resection of solitary intramedullary spinal cord metastases. Neurosurgery 1987, 21, 911–915. [Google Scholar] [CrossRef] [PubMed]
- Buyukbebeci, O.; Karakurum, G.; Tutar, E.; Gulec, A.; Arpacioglu, O. Biopsy of vertebral tumour metastasis for diagnosing unknown primaries. J. Orthop. Surg. 2010, 18, 361–363. [Google Scholar] [CrossRef]
- Destombe, C.; Botton, E.; Le Gal, G.; Roudaut, A.; Jousse-Joulin, S.; Devauchelle-Pensec, V.; Saraux, A. Investigations for bone metastasis from an unknown primary. Jt. Bone Spine 2007, 74, 85–89. [Google Scholar] [CrossRef] [PubMed]
- Dupuy, D.E.; Rosenberg, A.E.; Punyaratabandhu, T.; Tan, M.H.; Mankin, H.J. Accuracy of CT-guided needle biopsy of musculoskeletal neoplasms. AJR Am. J. Roentgenol. 1998, 171, 759–762. [Google Scholar] [CrossRef] [PubMed]
- Schweitzer, M.E.; Gannon, F.H.; Deely, D.M.; O’Hara, B.J.; Juneja, V. Percutaneous skeletal aspiration and core biopsy: Complementary techniques. AJR Am. J. Roentgenol. 1996, 166, 415–418. [Google Scholar] [CrossRef] [PubMed]
- Schepper, E.; Koes, B.; Veldhuizen, E.; Oei, E.; Bierma-Zeinstra, S.; Luijsterburg, P. Prevalence of spinal pathology in patients presenting for lumbar MRI as referred from general practice. Fam. Pract. 2016, 33, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Cortet, B.; Coquerelle, P.; Cotton, A.; Delambre, C. Diagnostic value of spinal puncture biopsy in non infectious spinal disease. Rev. Rhum. 1994, 61, 505–511. [Google Scholar]
- Mankin, H.J.; Lange, T.A.; Spanier, S.S. The hazards of biopsy in patients with malignant primary bone and soft-tissue tumors. J. Bone Jt. Surg. Am. 1982, 64, 1121–1127. [Google Scholar] [CrossRef]
- Laredo, J.D.; Bard, M. Thoracic spine: Percutaneous trephine biopsy. Radiology 1986, 160, 485–489. [Google Scholar] [CrossRef] [PubMed]
- Olscamp, A.; Rollins, J.; Tao, S.S.; Ebraheim, N.A. Complications of CT-guided biopsy of the spine and sacrum. Orthopedics 1997, 20, 1149–1152. [Google Scholar] [PubMed]
- Kaltsikis, I.; Chourmouzi, D.; Drevelegas, K.; Potsi, S.; Moumtzouoglou, A.; Drevelegas, A. Core needle biopsy of spinal lesions under CT guidance: Review of 79 cases. J. Neurol. Surg. A Cent. Eur. Neurosurg. 2012, 73, 199–203. [Google Scholar] [CrossRef] [PubMed]
- Kornblum, M.B.; Wesolowski, D.P.; Fischgrund, J.S.; Herkowitz, H.N. Computed tomography-guided biopsy of the spine. A review of 103 patients. Spine 1998, 23, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Czuczman, G.J.; Marrero, D.E.; Huang, A.J.; Mandell, J.C.; Ghazikhanian, V.; Simeone, F.J. Diagnostic yield of repeat CT-guided biopsy for suspected infectious spondylodiscitis. Skelet. Radiol. 2018, 47, 1403–1410. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.S.; McMahon, C.J.; Lozano-Calderon, S.; Kung, J.W. Utility of repeat core needle biopsy of musculoskeletal lesions with initially nondiagnostic findings. AJR Am. J. Roentgenol. 2017, 208, 609–616. [Google Scholar] [CrossRef] [PubMed]
- Fyfe, I.S.; Henry, A.P.; Mulholland, R.C. Closed vertebral biopsy. J. Bone Jt. Surg. Br. 1983, 65, 140–143. [Google Scholar] [CrossRef] [PubMed]
- Nam, K.H.; Song, G.S.; Han, I.H.; Choi, B.K.; Cha, S.H. Diagnostic Value of Biopsy Techniques in Lumbar Spondylodiscitis: Percutaneous Needle Biopsy and Open Biopsy. Korean J. Spine 2011, 8, 267–271. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, M.; Fujiwara, Y.; Uotani, K.; Maste, P.; Yamauchi, T. C-Arm-Free Circumferential Minimally Invasive Surgery for Adult Spinal Deformity: Technical Note. World Neurosurg. 2020, 143, 235–246. [Google Scholar] [CrossRef] [PubMed]

| Category | |
|---|---|
| Primary lesion | Unknown |
| Tumor location | Lamina, pedicle, vertebral body, paravertebral mass |
| Core needle biopsy | Failure or impossible |
| Extra-spinal lesion | None or no suitable lesion for biopsy |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tanaka, M.; Sonawane, S.; Uotani, K.; Fujiwara, Y.; Sessumpun, K.; Yamauchi, T.; Sugihara, S. Percutaneous C-Arm Free O-Arm Navigated Biopsy for Spinal Pathologies: A Technical Note. Diagnostics 2021, 11, 636. https://doi.org/10.3390/diagnostics11040636
Tanaka M, Sonawane S, Uotani K, Fujiwara Y, Sessumpun K, Yamauchi T, Sugihara S. Percutaneous C-Arm Free O-Arm Navigated Biopsy for Spinal Pathologies: A Technical Note. Diagnostics. 2021; 11(4):636. https://doi.org/10.3390/diagnostics11040636
Chicago/Turabian StyleTanaka, Masato, Sumeet Sonawane, Koji Uotani, Yoshihiro Fujiwara, Kittipong Sessumpun, Taro Yamauchi, and Shinsuke Sugihara. 2021. "Percutaneous C-Arm Free O-Arm Navigated Biopsy for Spinal Pathologies: A Technical Note" Diagnostics 11, no. 4: 636. https://doi.org/10.3390/diagnostics11040636
APA StyleTanaka, M., Sonawane, S., Uotani, K., Fujiwara, Y., Sessumpun, K., Yamauchi, T., & Sugihara, S. (2021). Percutaneous C-Arm Free O-Arm Navigated Biopsy for Spinal Pathologies: A Technical Note. Diagnostics, 11(4), 636. https://doi.org/10.3390/diagnostics11040636