Mobile Health in Remote Patient Monitoring for Chronic Diseases: Principles, Trends, and Challenges
Abstract
1. Introduction
- (a)
- Studying 56 papers in the period of (2015–2019) that cover several features related to RPMS, including IoT, WBAN, cloud computing, fog computing, and CDSS.
- (b)
- Providing a comprehensive survey that summarizes the state of the art of RPM systems, tools, technologies, recent applications, and techniques.
- (c)
- Highlighting all the steps in building efficient and effective RPMs, in addition to the challenges and future directions at each stage.
- (d)
- Discussing the importance of artificial intelligence (AI) in building medically intuitive monitoring systems.
- (e)
- Providing a case study of remote patient monitoring for chronic diseases patients that tries to cover several limitations of the state-of-the-art architectures.
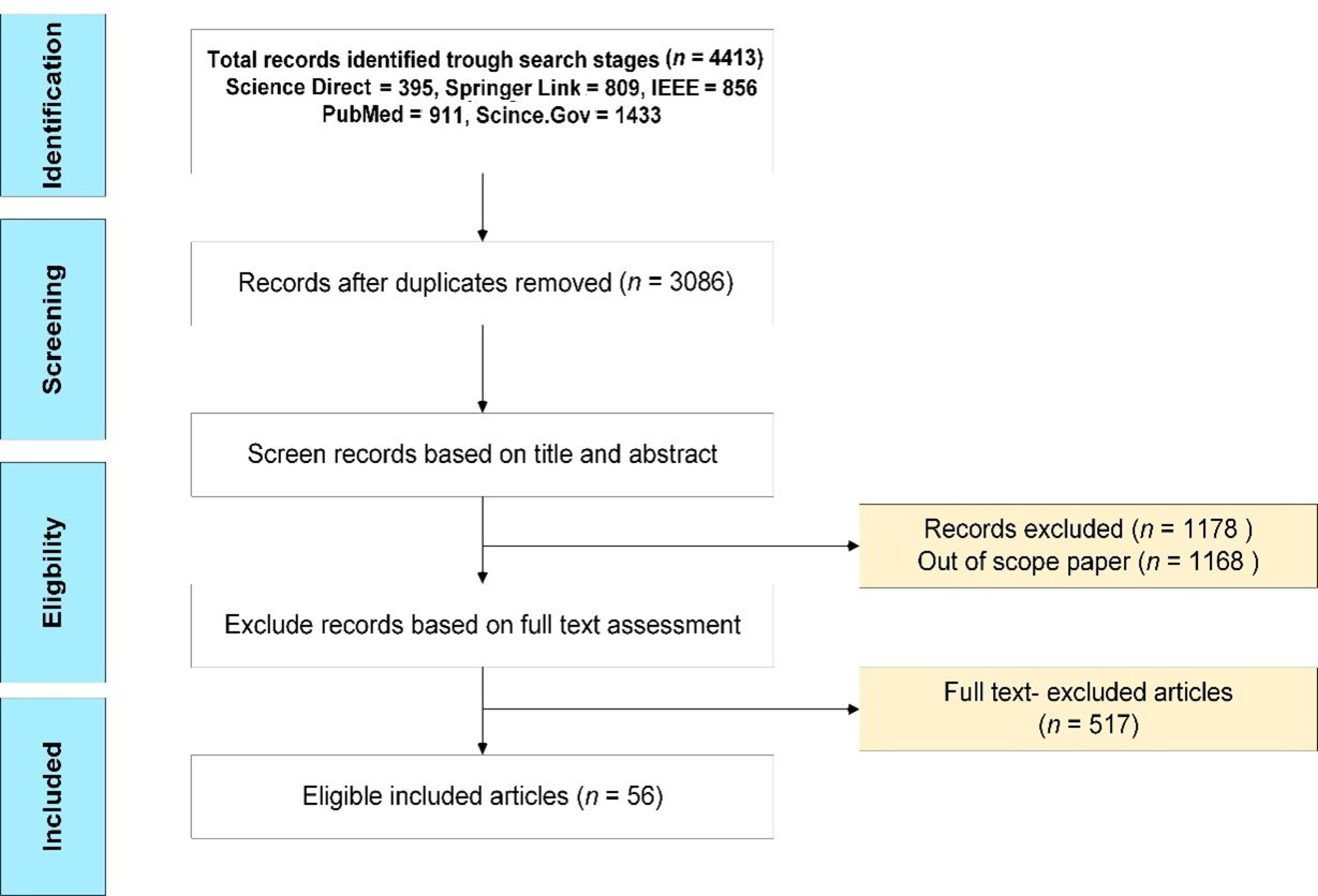
2. Materials and Methods
2.1. Selection Criteria
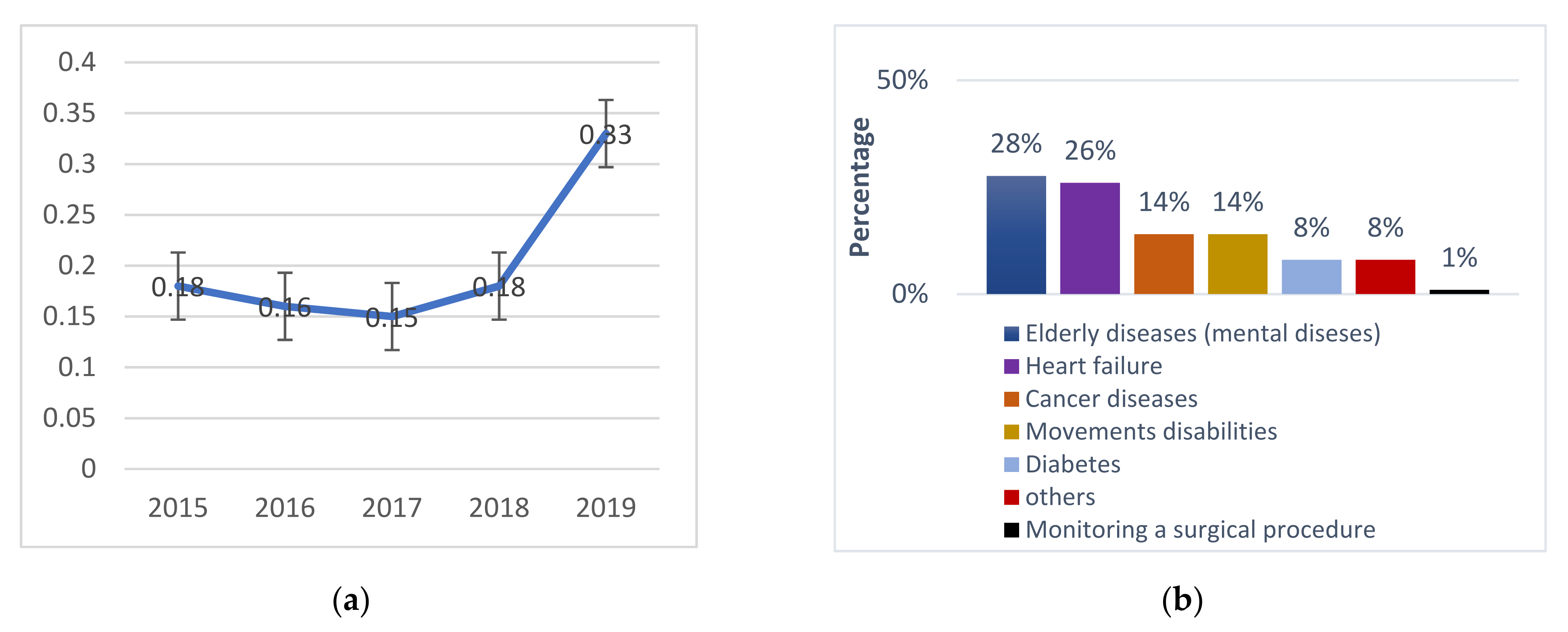
2.2. Results Statistical Analysis
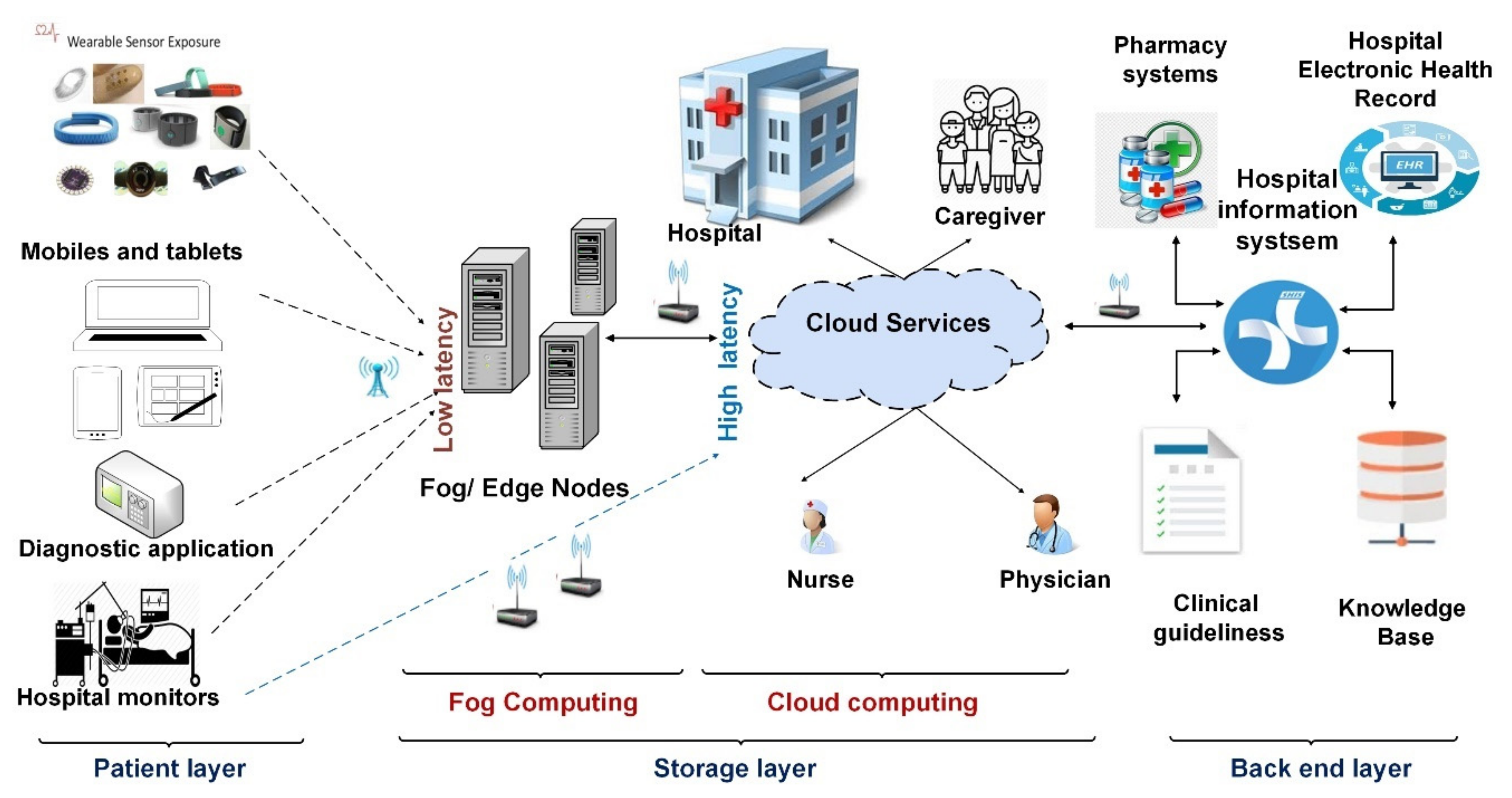
3. Main Components of the RPM System
- Provide patient assurance: RPMs could provide (24/7) care at home through wearable sensors, which are used to frequently measure patient vital signs, provide a real-time recommendation based on patient status.
- Increase patient awareness and responsibility: the continuous collecting of patient data increase patient awareness about his/her health status.
- Provision of low-cost solutions: depending on RPMs decreases the cost of hospitalization and admissions, consequently, saving on the total cost of healthcare services. Figure 3 shows the general form of the patient monitoring system.
3.1. Data Acquisition
- Implanted sensors: sensors that are implanted inside the patient’s body (under the patient’s skin).
- External sensors: sensors that attached directly to the patient’s skin or separated with about (2–5) CM.
WBAN Challenges in RMS
3.2. Storage Server
3.2.1. Cloud Computing
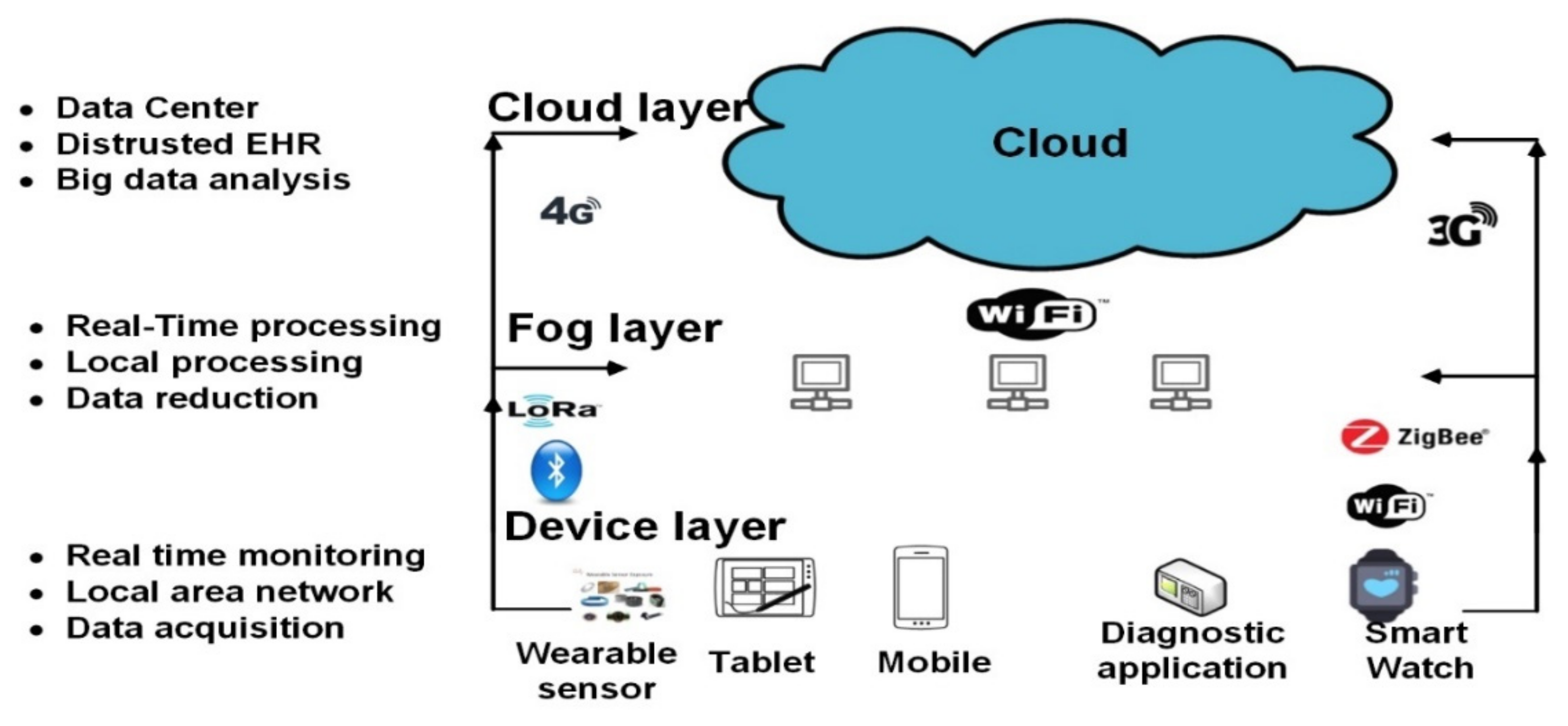
3.2.2. Fog Computing in RPMs
3.3. Back-End System
Knowledge Base
4. Disease-Specific Remote Patient Monitoring Systems
4.1. Heart Disease Monitoring Systems
4.2. Fall Detection Monitoring Systems
4.3. Mental Health Systems
4.4. Diabetes Monitoring System
4.5. Vital Sign Monitoring and Health Assessment Systems
4.6. Other Diseases Monitoring Systems
5. The Role of Artificial Intelligence in RPMs
5.1. Rule-Based Systems (Expert Systems)
5.2. Machine Learning Techniques
- (1)
- Supervised and non-supervised algorithms: Several types of supervised machine learning algorithms are used in RPMs, analyzing medical data in order to predict patient future events. For example, El-Rashidy et al. [80] used supervised ML algorithms (i.e., rule-based classifier, non-linear classifier, instance-based classifier, tree-based classifier, etc.) to analyze patient’s medical records and predict mortality among them. Each classifier used a different learning algorithm to build a model that best fit between input and output with a good generalization capability. Shamer et al. [128] developed a quality assessment model that was used to predict readmission, several ML algorithms were integrated to build an ensemble model to make predictions. The same model was used for predicting complications in ICU units [125], cardiovascular [129,130] Diabetes [131,132,133,134], sepsis [135,136], and COVID-19 [136,137,138]. ML is also used to provide timely medical services to patients. One such example is called Home Smart Health (HSH) [139]. HSH used a body sensor network and a personal sensor network for building a smart environment that has the capability to meet patient’s needs. ML (supervised and non-supervised) is used to analyze patients’ data (sensor data) to understand patient behavior and provide specific services for each patient.
- (2)
- Reinforcement learning (RL): ML models that learn by the trial-and-error concept, the learning process is repeated until the optimal solution is reached. RL is used in various monitoring systems. For example, Nuayto et al. [140] built RPMs for continuous monitoring of bio signs through a heterogeneous sensor transceiver. The proposed architecture used reinforcement learning (constrained Markov decision process (CMDP)) to minimize cost while maintaining the optimal quality of service (QoS). Wipawee et al. [141] used Q-learning (reinforcement learning) to provide a monitoring system. They used a distributed routing mechanism to route information to the nearest sink. Others use reinforcement learning to find the optimal treatment for a patient with anemia.
- (3)
- Deep learning (DL): This is a new area of ML that simulates the human thinking process. DL provides healthcare applications the ability to analyze huge data at exceptional speed with promising accuracy. For example, El-Sappagh et al. [115] used the DL model to predict patients with Alzheimer’s based on patient vital signs and X-ray images. Other common applications use DL models to specify the most critical features in patients’ imaging data, it is considered a promising solution in oncology image analysis. DL also has an increasing impact on natural language processing (NLP) [142]. In RPMs, NLP contributes to understanding the clinical notes on patients to provide efficient monitoring, transcribe interactions from patients, and provide conversational AI supportive tools such as chatbots [143]. For more details, [21,141,144] provide comprehensive surveys about using ML in RPMs.
5.3. Human-Computer Interaction
5.4. Physical and Processing Robots
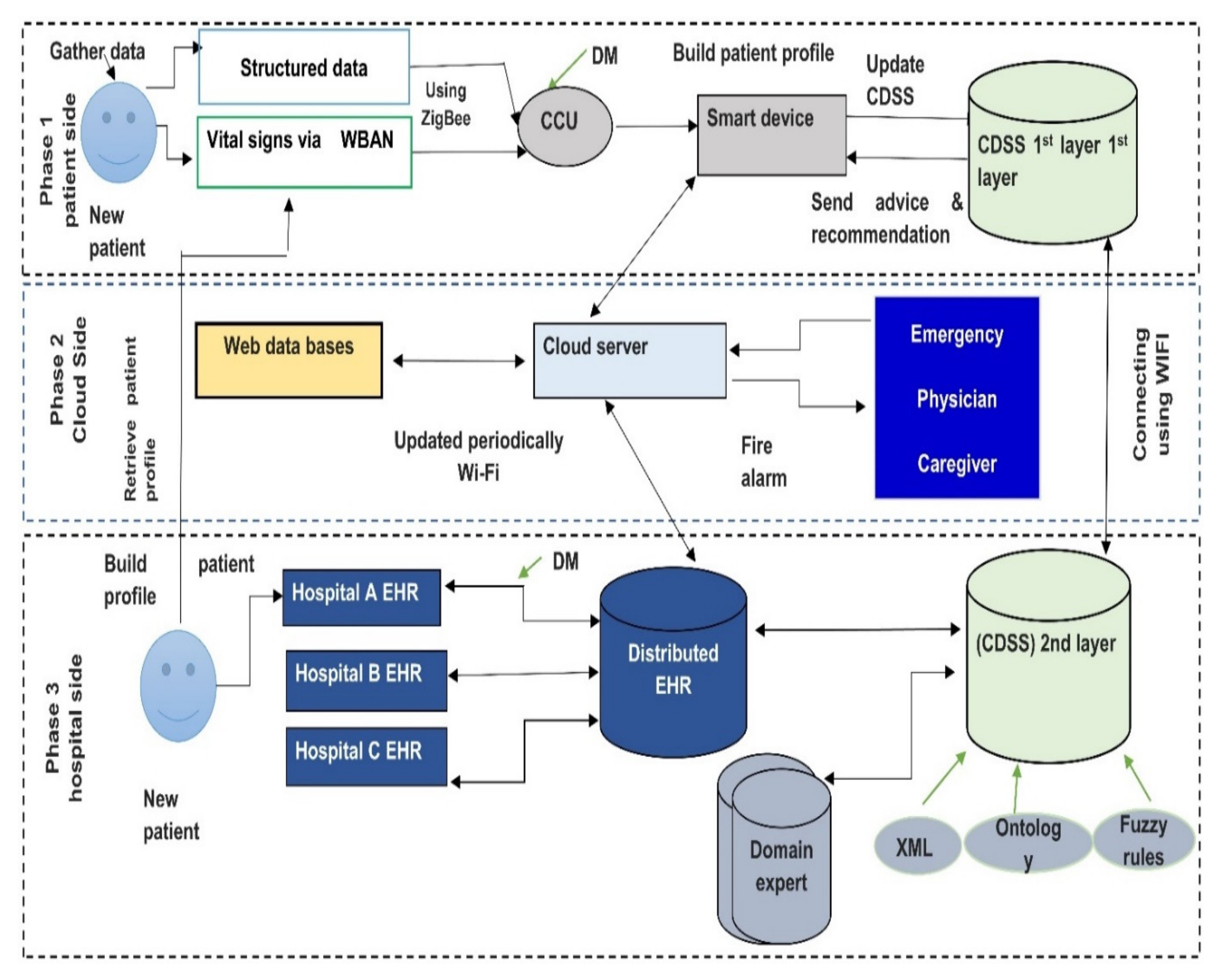
6. Case Study: Chronic Diseases Monitoring System
- (1)
- Lightweight biosensors are attached to a patient body. They continuously monitors patient vital signs like glucose level, vision level, fatigue level (EEG), activity level, blood pressure, body temperature, etc. Then all vital signs are gathered and sent to the central control unit. Note that ZigBee is used to deliver vital signs from sensors to central devices. If mobile applications notice that there is no patient record, the system will send a message to the patient via text or call to check the sensor or batteries. In case of no response after a short time system will automatically call the caregiver to check the patient’s state.
- (2)
- Social media patient’s activities (Facebook comments and tweets) are also tracked continuously and analyzed using components for handling unstructured data. All gathered raw data are then transported to the central control unit (CCU). In some cases, a smartphone may be used as a central control unit.
- (3)
- Our proposed framework provides two monitoring modes, the online and offline monitoring systems. The offline mode runs via the first layer CDSS that is installed on a personal server (discussed in the next step), and online via a cloud server (discussed in step 4), distributed her, and second layer CDSS. In the personal server, each patient transmits his/her vital signs, then all patient’s data are transmitted to the cloud hospital server.
- (4)
- In case the internet connection is interrupted or unplugged, the system will not work properly, and the patient will not be able to connect with the system. To overcome this challenge, a light CDSS was added to the patient side to monitor the patient until the internet problem was fixed. The CDSS’s first layer helps patients with advice and recommendations based on the patient profile (i.e., EHR) and a small knowledge base. The knowledge base will continually update by discovering and extracting knowledge from the EHR. CDSS in the first layer resolves the human-computer interaction issues and provides a simple and user-friendly GUI that does not require experience in dealing with computers or smart apps.
- (5)
- Periodically, patient data is transmitted to a stand-alone device where a wireless area network is created between it and another system component (Caregiver provider, family, emergency system), which permits them to access and check the patient status and retrieve patient information during monitoring system. In case the system detects abnormal signs, it will fire the alarm and send an alarm message to the network. Note that Wi-Fi IEEE 802 is used to transmit data between CCU, cloud server, and the CDSS second layer.
7. Study Results
Challenges and Future Directions
- Not all smart devices support the automatic transmission of patient data to the cloud or the fog nodes without patient intervention. Therefore, a new generation of mobiles should work on providing the automatic and accurate transfer of data [166]. For example, in 2016 Android worked on improving the sampling rate constraints and permitting third-party applications to sample from various sensors.
- The accuracy of sensing devices (i.e., sensors) has still not reached a stable state; therefore, various challenges include working on enhancing signal processing and transmission. For example, Kim et al. [167] introduced a group of analog-front-end solutions that address the tradeoff between the quality of transmission and power consumption.
- The RPM systems are developed to solve the problem of patient monitoring regardless of time and place. Therefore, the design of WSN should maintain the mobility, transmission rate, data rate, and network coverage issues [168]. For example, building monitoring systems that utilize both fog computing and cloud computing may provide various capabilities such as mobility, low latency, and low bandwidth consumption.
- Managing and integrating the massive data extracted during patient monitoring are considered a daunting task. To take full advantage of the extracted data, various data mining and knowledge extraction tools should be developed to have deep insights into these data to improve knowledge outcomes and decrease costs [76].
- The internet is considered the primary medium for data transmission in any RPMs. This raises the need for ironclad privacy and security protocols to protect data from different attacks such as data eavesdropping modification and impersonations. The problem worsens due to the fact that most wireless body area network devices used in patient monitoring are limited in memory, processing, and energy capabilities [169]. Therefore, it is considered impossible to provide full monitoring systems based on them. Accordingly, privacy and security issues need additional work, to provide an acceptable solution in the different layers of monitoring [170,171]. A comprehensive survey of security and privacy in patient monitoring can be found in [172].
- Encryption could be used to prevent data eavesdropping. Therefore, working on symmetric and asymmetric key encryption algorithms could help to provide a high level of security for patient’s data [173].
- Managing large networks is also a complex challenge. Therefore, working on developing role-based access control systems may help in reducing the complexity in administration, especially with large healthcare systems.
- Monitoring systems could be used for a small number of patients in clinics or may be scaled up to be used by a large number of users in hospitals. This results in the rapid growth of demands for physicians as well as healthcare organizations. Accordingly, RPMs should be scalable in terms of applications, networks, and services [8].
- RPM systems are very time-sensitive and require the guarantee of several QoS criteria such as maintainability, reliability, and availability. This is due to the fact that such systems put patient’s lives in danger in critical health problems [174].
- The power consumption of WBAN sensors is a big challenge for RPMs. Usually, the capacity of batteries is consumed in sensing, processing, and transmitting of data, so that it requires frequent recharging. It may be considered the weakest point in RPMs as frequent charging for batteries is considered a big burden for patients. Therefore, the optimization of power consumption is considered one of the main points in various studies. Some studies working on improving the current protocols such as Zigbee and Bluetooth are [11,132,175]. Others work on extending the lifetime of the sensor battery by utilizing medium access control (MAC) protocols with low power consumption [176].
- Providing continuous monitoring in the healthcare sector requires the use of various sensors that are mostly manufactured by different manufacturers. The lack of standardization techniques hinders the ability of devices to communicate and transmit data among them effectively. Therefore, working on standards and data integration protocols is considered a pressing need to provide data and device interoperability. From the application side, some monitoring applications require approval for use from some bodies such as the FDA. To overcome this delay, participants must come up with medical guidelines that work on speeding up the deployment of medical applications.
- The development of complete RPMs that allow patients to integrate with various hardware and software service providers and different sources of data (heterogeneous sources with different standards and formats) is a challenge that needs to be addressed in future studies.
- The patient’s EHR system may include various components such as laboratory systems, hospital information systems, etc. Each component may have different standards (i.e., HL7, OpenEHR, and ISO/IEEE) and different terminologies (i.e., LONIC, SNOMED CT, and CPT4). Therefore, working on a unified standard is essential to maintaining syntax and semantic interoperability [177].
- CDSS should work based on a patient’s EHR data, in addition to vital signs data sensed from wearable sensors. Therefore, CDSSs should provide specific services based on each patient’s data. On the other hand, CDSSs interfaces should maintain a brain-computer interface (BCI) and human-computer interaction (HCI) in order to support the dynamic creation of an application interface according to patient’s moods [178].
- Based on the surveyed literature presented in this paper, we could not categorize whether the existing RPM solutions are easily compatible with security and privacy legislation. Nonetheless, as healthcare solutions undergo a digital transformation, the paradigm needs to be implemented with the compliance of different legislative frameworks such as the general data protection regulation (GDPR) and network and information security (NIS) directive (NISD) requirements [82]. While the GDPR is a privacy directive that instructs how organizations should handle personal data, the NISD emphasizes strengthening organizations’ security capability from the service infrastructure viewpoints. The work in [83] identified a set of different measures that can be integrated with m-health systems to adopt GDPR-compliant security and privacy schemes. Recently, the work in [179] provides a case study of the “WELCOME” research project, an integrated system for chronic patients’ monitoring, diagnosis, detection, and treatment. In the study, the authors propose a framework for the security and privacy of m-health applications adhering to the GDPR guidelines. Policy enforcement is necessary to monitor and guarantee that the digital information systems strictly follow specific policies in dealing with medical information.
- The advanced message queuing protocol (AMQP) and message queuing telemetry transport (MQTT) are the two most common data transfer protocols used to exchange data between IoT systems and edge or cloud servers. Although both of these schemes are non-healthcare-specific protocols, they can be integrated with HL7, which is here and now the most widely adopted data interaction standard in medical applications [180]. In MQTT, a broker receives messages from the publishers then routes the messages to the respective subscribers. While AMQP provides similar functionality as MQTT, it also facilitates queues in the broker to store the message when the consumer does not access the messages. Large organizations that include many IoT devices require a higher level of data integrity. Therein, both AMQP and MQTT can simultaneously be deployed for different clusters and regions [181,182]. As such, the coexistence of AMQP and MQTT protocols is conceivable in HL7-facilitated organizations. However, to determine the suitability for the HL7 framework, more research on lightweight publish-subscribe network protocols is required from practical and implementation contexts.
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| AHP | Analytical hierarchy process |
| CBR | Case-based reasoning |
| CC | Cloud computing |
| CDSS | Clinical decision support system |
| CHMS | Cloud health monitoring system |
| COPD | Chronic obstructive pulmonary diseases |
| ECG | Electrocardiogram |
| EEG | Electroencephalogram |
| EHR | Electronic health record |
| EMG | Electromyogram |
| HL7 | Health Level Seven |
| IoT | Internet of Things |
| KB | Knowledge bases |
| MAC | Medium Access Control |
| PMS | Patient monitoring systems |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| QoS | Quality of service |
| SCI | Spinal cord injury |
| SNOMED-CD | Systematized nomenclature of medicine-clinical terms |
| TDMA | Flexible time division multiple access |
| Term | Abbreviation |
| UMLS | Unified Medical Language System |
| WBAN | Wireless body area network |
| XML | Extensible Markup Language |
References
- Raghupathi, W.; Raghupathi, V. An Empirical Study of Chronic Diseases in the United States: A Visual Analytics Approach to Public Health. Int. J. Environ. Res. Public Health 2018, 15, 431. [Google Scholar] [CrossRef] [PubMed]
- Waqialla, M.; Alshammari, R.; Razzak, M.I. An ontology for remote monitoring of cardiac implantable electronic devices. In Proceedings of the 2015 3rd International Conference on Computer, Communication, Control and Information Technology, Hooghly, India, 7–8 February 2015; pp. 520–523. [Google Scholar]
- Rahim, A.; Forkan, M.; Khalil, I. A Probabilistic model for early prediction of abnormal clinical events using vital sign correlations in home-based monitoring. In Proceedings of the 2016 IEEE International Conference on Pervasive Computing and Communications, Sydney, NSW, Australia, 14–19 March 2016. [Google Scholar]
- Zhanwei, D.; Yongjian, Y. Semi-automatic remote medicine monitoring system of mobile users. China Commun. 2015, 12, 134–142. [Google Scholar] [CrossRef]
- Jackson Healthcare. Physician Trends 2016 Report; Jackson Healthcare: Alpharetta, GA, USA, 2016; pp. 1–60. [Google Scholar]
- Mazboori, N.; Javidan, A.N.; Bahmani, P. The Effect of Remote Patient Monitoring on Patients with Spinal Cord Injury: A Mini-Review. Arch. Neurosci. 2019, 6, 4–7. [Google Scholar] [CrossRef]
- Deshmukh, R.; Jadhav, K.; Borude, T.; Lanke, H. A Survey Paper on Patient Health and Saline Level Monitoring System using IoT. IJERT 2019, 8, 807–809. [Google Scholar]
- Vegesna, A.; Tran, M.; Angelaccio, M.; Arcona, S. Remote Patient Monitoring via Non-Invasive Digital Technologies: A Systematic Review. Telemed. J. E-Health 2017, 23, 3–17. [Google Scholar] [CrossRef]
- Iraqi, Y.; Mardini, M.; Agoulmine, N. A Survey of Healthcare Monitoring Systems for Chronically Ill Patients and Elderly. J. Med. Syst. 2019, 43, 50. [Google Scholar]
- Gelogo, Y.E.; Hwang, H.J.; Kim, H. Internet of Things (IoT) Framework for u-healthcare System. Int. J. Smart Home 2015, 9, 323–330. [Google Scholar] [CrossRef]
- Ismail, A.; Abdlerazek, S.; El-Henawy, I.M. Development of Smart Healthcare System Based on Speech Recognition Using Support Vector Machine and Dynamic Time Warping. Sustainability 2020, 12, 2403. [Google Scholar] [CrossRef]
- Jung, M.; Han, K.; Cho, J. Advanced verification on WBAN and cloud computing for u-health environment. Multimed. Tools Appl. 2015, 74, 6151–6168. [Google Scholar] [CrossRef]
- Dhanashri, D.; Dhonde, S.B. A Survey of Cloud Based Healthcare Monitoring System for Hospital Management; Springer: Singapore, 2017; pp. 9–18. [Google Scholar]
- Alaa, A.M.; Moon, K.H.; Hsu, W.; van der Schaar, M. ConfidentCare: A Clinical Decision Support System for Personalized Breast Cancer Screening. IEEE Trans. Multimed. 2016, 18, 1–13. [Google Scholar] [CrossRef]
- Zhang, F.; Gou, L.; Zhou, T. An ontology-based approach to patient follow-up assessment for continuous and personalized chronic disease management. J. Biomed. Inform. 2017, 72, 45–59. [Google Scholar] [CrossRef] [PubMed]
- El-Sappagh, S.; El-Masri, S.; Elmogy, M.; Riad, A.M. A diabetes diagnostic domain ontology for CBR system from the conceptual model of SNOMED CT. In Proceedings of the ICET 2nd International Conference on Engineering and Technology, Cairo, Egypt, 19–20 April 2015. [Google Scholar]
- Jha, M.; Pakhira, D.; Chakraborty, B. Diabetes Detection and Care Applying CBR Techniques. Int. J. Soft Comput. Eng. 2013, 2, 6. [Google Scholar]
- Sahoo, P.K.; Thakkar, H.K.; Lee, M.Y. A cardiac early warning system with multi channel SCG and ECG monitoring for mobile health. Sensors 2017, 17, 711. [Google Scholar] [CrossRef] [PubMed]
- Rotariu, C.; Manta, V. Wireless system for remote monitoring of oxygen saturation and heart rate. In Proceedings of the Federated Conference on Computer Science and Information Systems—FedCSIS 2012, Wrocław, Poland, 9–12 September 2012; pp. 193–196. [Google Scholar]
- Sharma, R. Survey on Interoperability Issues in Development of Smart. Int. J. Adv. Res. Comput. Sci. 2018, 9, 458–459. [Google Scholar] [CrossRef]
- Tripathi, G.; Ahad, M.A.; Paiva, S. Sms: A secure healthcare model for smart cities. Electronics 2020, 9, 7649. [Google Scholar] [CrossRef]
- Kovačević, T.; Perković, T.; Čagalj, M. LIRA: A new key deployment scheme for wireless body area networks. In Proceedings of the SoftCOM 2013: 21th International Conference on Software, Telecommunications and Computer Networks, Split, Croatia, 18–20 September 2013. [Google Scholar]
- Tian, Y.; Peng, Y.; Peng, X.; Li, H. An attribute-based encryption scheme with revocation for fine-grained access control in wireless body area networks. Int. J. Distrib. Sens. Netw. 2014, 2014. [Google Scholar] [CrossRef]
- Shou, Y.; Guyennet, H.; Lehsaini, M. Parallel Scalar Multiplication on Elliptic Curves in Wireless Sensor Networks. In Distributed Computing and Networking; Springer: Berlin/Heidelberg, Germany, 2013; pp. 300–314. [Google Scholar]
- Pathak, G.; Gutierrez, J.; Rehman, S.U. Security in Low Powered Wide Area Networks: Opportunities for Software Defined Network-Supported Solutions. Electronics 2020, 9, 1195. [Google Scholar] [CrossRef]
- Yang, Z.; Zhou, Q.; Lei, L.; Zheng, K.; Xiang, W. An IoT-cloud Based Wearable ECG Monitoring System for Smart Healthcare. J. Med. Syst. 2016, 40. [Google Scholar] [CrossRef]
- Fong, E.M.; Chung, W.Y. Mobile cloud-computing-based healthcare service by Noncontact ECG monitoring. Sensors 2013, 13, 16451–16473. [Google Scholar] [CrossRef]
- Yang, G.; Jiang, M.; Ouyang, W.; Ji, G.; Xie, H.; Rahmani, A.M. IoT-based Remote Pain Monitoring System: From Device to Cloud Platform. IEEE J. Biomed. Health Inform. 2017, 22, 1711–1719. [Google Scholar] [CrossRef]
- Li, C.; Hu, X.; Zhang, L. The IoT-based heart disease monitoring system for pervasive healthcare service. Procedia Comput. Sci. 2017, 112, 2328–2334. [Google Scholar] [CrossRef]
- Guan, K.; Shao, M.; Wu, S. A remote health monitoring system for the elderly based on smart home gateway. J. Healthc. Eng. 2017, 2017. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.A.U.; Roy, N.; Holmes, S.; Gangopadhyay, A.; Galik, E. Automated Functional and Behavioral Health Assessment of Older Adults with Dementia. In Proceedings of the 2016 IEEE First International Conference on Connected Health: Applications, Systems and Engineering Technologies (CHASE), Washington, DC, USA, 27–29 June 2016; pp. 140–149. [Google Scholar]
- Silva, V.J.; Rodrigues, M.A.S.; Barreto, R.; de Lucena, V.F. UbMed: A ubiquitous system for monitoring medication adherence. In Proceedings of the 2016 IEEE 18th International Conference on e-Health Networking, Applications and Services (Healthcom), Munich, Germany, 14–17 September 2016; pp. 16–19. [Google Scholar]
- Hezarjaribi, N.; Fallahzadeh, R.; Ghasemzadeh, H. A machine learning approach for medication adherence monitoring using body-worn sensors. In Proceedings of the 2016 Design, Automation & Test in Europe Conference & Exhibition (DATE), Dresden, Germany, 14–18 March 2016; pp. 842–845. [Google Scholar]
- Wang, J.; Zhang, Z.; Li, B.; Lee, S.; Sherratt, R. An enhanced fall detection system for elderly person monitoring using consumer home networks. IEEE Trans. Consum. Electron. 2014, 60, 23–29. [Google Scholar] [CrossRef]
- Zhang, L.; Xing, B.; Gao, Z.; Wang, J.; Sun, S.; Zhang, K. Smart blood pressure monitoring system based on internet of things. In Proceedings of the CHI’13: CHI Conference on Human Factors in Computing Systems, Paris, France, 27 April–2 May 2013. [Google Scholar]
- Ballari, D.; Manso-callejo, M.A.; Wachowicz, M. The Interoperability of Wireless Sensor Networks; Technical University of Madrid: Madrid, Spain, 2004; pp. 1–4. [Google Scholar]
- Brandt, P.; Basten, T.; Stuiik, S.; Bui, V.; de Clercq, P.; Pires, L.F.; van Sinderen, M. Semantic interoperability in sensor applications making sense of sensor data. In Proceedings of the 2013 IEEE Symposium on Computational Intelligence in Healthcare and e-health (CICARE), Singapore, 15–19 April 2013; pp. 1–8. [Google Scholar]
- Mahmoud, N.; El-Sappagh, S.; El-Bakry, H.M.; Abdelrazek, S. A Real-time Framework for Patient Monitoring Systems based on a Wireless Body Area Network. Int. J. Comput. Appl. 2020, 176, 12–21. [Google Scholar] [CrossRef]
- El-rashidy, N.; El-sappagh, S.; Islam, S.M.R.; El-bakry, M.H.; Abdelrazek, S. End-To-End Deep Learning Framework for Coronavirus (COVID-19) Detection and Monitoring. Electronics 2020, 9, 1439. [Google Scholar] [CrossRef]
- Balasubramanian, V.; Stranieri, A. A scalable cloud Platform for Active healthcare monitoring applications. In Proceedings of the IC3e 2014—2014 IEEE Conference on e-Learning, e-Management and e-Services, Melbourne, Australia, 10–12 December 2014; pp. 93–98. [Google Scholar]
- Ahir, P.D.; Bharade, S.; Botre, P.; Nagane, S.; Shah, M. Intelligent Traffic Control System for Smart Ambulance. IRJET 2018, 5, 355–358. [Google Scholar]
- Rana, J.; Bajpayee, A. HealthCare Monitoring and Alerting System Using Cloud Computing. Int. J. Recent Innov. Trends Comput. Commun. 2015, 3, 102–105. [Google Scholar]
- Risso, N.A.; Neyem, A.; Benedetto, J.I.; Carrillo, M.J.; Farías, A.; Gajardo, M.J.; Loyola, O. A cloud-based mobile system to improve respiratory therapy services at home. J. Biomed. Inform. 2016, 63, 45–53. [Google Scholar] [CrossRef]
- Paez, D.G.; Aparicio, F.; de Buenaga, M.; Rubio, M. Highly personalized health services using cloud and sensors. In Proceedings of the 2013 Seventh International Conference on Innovative Mobile and Internet Services in Ubiquitous Computing (IMIS), Taichung, Taiwan, 3–5 July 2013; pp. 451–455. [Google Scholar]
- Hsu, T.C.; Chang, C.H.; Chu, W.C.; Ho, S.Y.; Hsueh, N.L.; Lee, W.B. Applying cloud computing technologies to Gerontology and Geriatrics Health Care System (GGHCS). In Proceedings of the 2013 13th International Conference on Quality Software, Nanjing, China, 29–30 July 2013. [Google Scholar]
- Hidalgo, J.A.; Cajiao, A.; Hern, C.M.; Diego, M.L. VISIGNET: A wireless body area network with cloud data storage for the telemonitoring of vital signs. Health Technol. 2015, 5, 115–126. [Google Scholar] [CrossRef]
- Melillo, P.; Orrico, A.; Scala, P.; Crispino, F.; Pecchia, L. Cloud-Based Smart Health Monitoring System for Automatic Cardiovascular and Fall Risk Assessment in Hypertensive Patients. J. Med. Syst. 2015, 39. [Google Scholar] [CrossRef]
- Rassias, G.; Andrikos, C.O.; Tsanakas, P.; Maglogiannis, I. Versatile Cloud Collaboration Services for Device-Transparent Medical Imaging Teleconsultations. Proc. IEEE Symp. Comput. Med. Syst. 2017, 2017, 306–311. [Google Scholar]
- Saechow, S.; Kamolphiwong, S.; Chandeeying, V. Web-based teleconsultation for clinical diagnosis. In Proceedings of the 13th International Conference on Electronics, Information, and Communication, ICEIC 2014, Kota Kinabalu, Malaysia, 15–18 January 2014; pp. 2–3. [Google Scholar]
- Guo, U.; Chen, L.; Mehta, P.H. Electronic health record innovations: Helping physicians—One less click at a time. Health Inf. Manag. J. 2017, 46, 140–144. [Google Scholar] [CrossRef] [PubMed]
- Bahga, A.; Madisetti, V.K. A cloud-based approach for interoperable electronic health records (EHRs). IEEE J. Biomed. Health Inform. 2013, 17, 894–906. [Google Scholar] [CrossRef] [PubMed]
- Van Eyk, E.; Iosup, A.; Seif, S.; Thömmes, M. The spec cloud group’s research vision on faas and serverless architectures. In Proceedings of the WoSC’17: 2nd International Workshop on Serverless Computing, Las Vegas, NV, USA, 5–11 December 2017; pp. 1–4. [Google Scholar]
- Kim, J.; Park, J.; Lee, K. Network resource isolation in serverless cloud function service. In Proceedings of the 2019 IEEE 4th International Workshops on Foundations and Applications of Self* Systems (FAS* W), Umea, Sweden, 16–20 June 2019; IEEE: Piscataway, NJ, USA, 2019; pp. 182–187. [Google Scholar]
- Leitner, P.; Wittern, E.; Spillner, J.; Hummer, W. A mixed-method empirical study of Function-as-a-Service software development in industrial practice. J. Syst. Softw. 2019, 149, 340–359. [Google Scholar] [CrossRef]
- Al-Ameen, M.; Spillner, J. Systematic and open exploration of FaaS and Serverless Computing research. CEUR Workshop Proc. 2019, 2330, 30–35. [Google Scholar]
- Rajan, R.A.P. A review on serverless architectures-Function as a service (FaaS) in cloud computing. Telkomnika 2020, 18, 530–537. [Google Scholar] [CrossRef]
- Almashaqbeh, G.; Hayajneh, T.; Vasilakos, A.V.; Mohd, B.J. QoS-Aware Health Monitoring System Using Cloud-Based WBANs. J. Med. Syst. 2014, 38. [Google Scholar] [CrossRef] [PubMed]
- Almashaqbeh, G. A Cloud-based interference-aware remote health monitoring system for non-hospitalized patients. In Proceedings of the IEEE Conference and Exhibition on Global Telecommunications (GLOBECOM), Austin, TX, USA, 8–12 December 2014; pp. 2436–2441. [Google Scholar]
- Chen, B.; Varkey, J.P.; Pompili, D.; Li, J.K.-J.; Marsic, I. Patient vital signs monitoring using Wireless Body Area Networks. In Proceedings of the 2010 IEEE 36th Annual Northeast Bioengineering Conference (NEBEC), New York, NY, USA, 26–28 March 2010; pp. 1–2. [Google Scholar]
- Ahnn, J.H.; Potkonjak, M. mHealthMon: Toward Energy-Efficient and Distributed Mobile Health Monitoring Using Parallel Offloading. J. Med. Syst. 2013, 37, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Khan, F.A.; Ali, A.; Abbas, H.; Haldar, N.A.H. A cloud-based healthcare framework for security and patients’ data privacy using wireless body area networks. Procedia Comput. Sci. 2014, 34, 511–517. [Google Scholar] [CrossRef]
- Paper, W. Cisco Fog Computing Solutions: Unleash the Power of the Internet of Things; Cisco: San Jose, CA, USA, 2015; pp. 1–6. [Google Scholar]
- Stojmenovic, I. Fog computing: A cloud to the ground support for smart things and machine-to-machine networks. In Proceedings of the 2014 Australasian Telecommunication Networks and Applications Conference (ATNAC), Melbourne, Australia, 26–28 November 2014; pp. 117–122. [Google Scholar]
- Verma, P.; Sood, S.K. Fog Assisted-IoT Enabled Patient Health Monitoring in Smart Homes. IEEE Internet Things J. 2018. [Google Scholar] [CrossRef]
- Yi, S.; Li, C.; Li, Q. A survey of fog computing: Concepts, applications and issues. In Proceedings of the 2015 Workshop on Mobile Big Data, Mobidata’15, Hangzhou, China, 21 June 2015; pp. 37–42. [Google Scholar]
- Paul, A.; Pinjari, H.; Hong, W.H.; Seo, H.C.; Rho, S. Fog computing-based IoT for health monitoring system. J. Sens. 2018, 2018. [Google Scholar] [CrossRef]
- Kraemer, F.A.; Braten, A.E.; Tamkittikhun, N.; Palma, D. Fog Computing in Healthcare—A Review and Discussion. IEEE Access 2020, 5, 9206–9222. [Google Scholar] [CrossRef]
- Chiang, M.; Ha, S.; Risso, F.; Zhang, T. Clarifying fog computing and networking: 10 questions and answers. IEEE Commun. Mag. 2017, 55, 18–20. [Google Scholar] [CrossRef]
- Dastjerdi, A.V.; Buyya, R. Fog Computing: Helping the Internet of Things Realize Its Potential. Computer 2016, 49, 112–116. [Google Scholar] [CrossRef]
- Kharel, J.; Reda, H.T.; Shin, S.Y. An architecture for smart health monitoring system based on fog computing. J. Commun. 2017, 12, 228–233. [Google Scholar] [CrossRef][Green Version]
- Gia, T.N.; Jiang, M.; Sarker, V.K.; Rahmani, A.M.; Westerlund, T.; Liljeberg, P.; Tenhunen, H. Low-cost fog-assisted health-care IoT system with energy-efficient sensor nodes. In Proceedings of the 13th International Wireless Communications and Mobile Computing Conference (IWCMC 2017), Valencia, Spain, 26–30 June 2017; pp. 1765–1770. [Google Scholar]
- Gia, T.N.; Jiang, M.; Rahmani, A.; Westerlund, T.; Liljeberg, P.; Tenhunen, H. Fog Computing in Healthcare Internet of Things: A Case Study on ECG Feature Extraction. In Proceedings of the 2015 IEEE International Conference on Computer and Information Technology, Ubiquitous Computing and Communications, Dependable, Autonomic and Secure Computing, Pervasive Intelligence and Computing, Liverpool, UK, 26–28 October 2015; pp. 356–363. [Google Scholar]
- Sareen, S.; Gupta, S.K.; Sood, S.K. An intelligent and secure system for predicting and preventing Zika virus outbreak using Fog computing. Enterp. Inf. Syst. 2017, 11, 1436–1456. [Google Scholar] [CrossRef]
- Pattekari, S.A.; Parveen, A. Prediction system for heart disease using Naive Bayes. Int. J. Adv. Comput. Math. Sci. 2012, 3, 2230–9624. [Google Scholar]
- Rahim, A.; Forkan, M.; Khalil, I. A clinical decision-making mechanism for context-aware and patient-specific remote monitoring systems using the correlations of multiple vital signs. Comput. Methods Programs Biomed. 2017, 139, 1–16. [Google Scholar]
- El-rashidy, N.; El-sappagh, S.; El-Bakry, H.M.; Abuhmed, T.; Abdelrazek, S. Intensive Care Unit Mortality Prediction: An Improved Patient-Specific Stacking Ensemble Model. IEEE Access 2020, 8. [Google Scholar] [CrossRef]
- Caballero-Ruiz, E.; García-Sáez, G.; Rigla, M.; Villaplana, M.; Pons, B.; Hernando, M.E. A web-based clinical decision support system for gestational diabetes: Automatic diet prescription and detection of insulin needs. Int. J. Med. Inform. 2017, 102, 35–49. [Google Scholar] [CrossRef] [PubMed]
- El-Sappagh, S.; el Mogy, M.; Riad, A.M. A standard fragment of EHR relational data model for diabetes mellitus diagnosis. In Proceedings of the 2017 9th International Conference on Informatics and Systems, INFOS 2017, Cairo, Egypt, 15–17 December 2017; pp. DEKM1–DEKM9. [Google Scholar]
- Ganzha, M.; Paprzycki, M.; Pawłowski, W.; Szmeja, P.; Wasielewska, K. Semantic interoperability in the Internet of Things: An overview from the INTER-IoT perspective. J. Netw. Comput. Appl. 2017, 81, 111–124. [Google Scholar] [CrossRef]
- El-Sappagh, S.H.; El-Masri, S.; Riad, A.M.; Elmogy, M. Electronic Health Record Data Model Optimized for Knowledge Discovery. Int. J. Comput. Sci. 2012, 9, 329–338. [Google Scholar]
- El-Sappagh, S.H.; El-Masri, S. A distributed clinical decision support system architecture. J. King Saud. Univ. Comput. Inf. Sci. 2014, 26, 69–78. [Google Scholar] [CrossRef]
- Maxhelaku, S.; Kika, A. Improving interoperability in healthcare using Hl7 Fhir. In Proceedings of the 47th International Academic Conference, Prague, Czech Republic, 17–20 June 2019. [Google Scholar]
- Girardi, F.; de Gennaro, G.; Colizzi, L.; Convertini, N. Improving the healthcare effectiveness: The possible role of EHR, IoMT and Blockchain. Electronics 2020, 9, 884. [Google Scholar] [CrossRef]
- Semenov, I.; Osenev, R.; Gerasimov, S.; Kopanitsa, G.; Denisov, D.; Andreychuk, Y. Experience in developing an FHIR medical data management platform to provide clinical decision support. Int. J. Environ. Res. Public Health 2020, 17, 73. [Google Scholar] [CrossRef] [PubMed]
- Plischke, S.; Machutova, J.; Stasa, P.; Unucka, J. Development of SW interface between healthcare standards-DASTA and HL7. Sustainability 2020, 12, 7649. [Google Scholar] [CrossRef]
- Saripalle, R.; Runyan, C.; Russell, M. Using HL7 FHIR to achieve interoperability in patient health record. J. Biomed. Inform. 2019, 94, 103188. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.L.; Lee, H.A.; Hsu, C.Y.; Kung, H.H.; Chiu, H.W. Implement an international interoperable phr by fhir—A Taiwan innovative application. Sustainability 2021, 13, 198. [Google Scholar] [CrossRef]
- Storck, M.; Hollenberg, L.; Dugas, M.; Soto-Rey, I. Interoperability Improvement of Mobile Patient Survey (MoPat) Implementing Fast Health Interoperability Resources (FHIR). Stud. Health Technol. Inform. 2019, 258, 141–145. [Google Scholar]
- Chen, R.C.; Jiang, H.Q.; Huang, C.Y.; Bau, C.T. Clinical Decision Support System for Diabetes Based on Ontology Reasoning and TOPSIS Analysis. J. Healthc. Eng. 2017, 2017, 9–12. [Google Scholar] [CrossRef] [PubMed]
- El Sappagh, S.; Elmogy, M. A Decision Support System for Diabetes Mellitus Management. Diabetes Case Rep. 2016, 1, 1–13. [Google Scholar] [CrossRef]
- Velickovski, F.; Ceccaroni, L.; Roca, J.; Burgos, F.; Galdiz, J.B.; Marina, N.; Lluch-Ariet, M. Clinical decision support systems (CDSS) for preventive management of COPD patients. J. Transl. Med. 2014, 12, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Lakshmanaprabu, S.; Mohanty, S.N.; Rani, S.; Krishnamoorthy, S.; Uthayakumar, J.; Shankar, K. Online clinical decision support system using optimal deep neural networks. Appl. Soft Comput. 2019, 81, 105487. [Google Scholar]
- Ivascu, T.; Manate, B.; Negru, V. A multi-agent architecture for ontology-based diagnosis of mental disorders. In Proceedings of the 2015 17th International Symposium on Symbolic and Numeric Algorithms for Scientific Computing (SYNASC), Timisoara, Romania, 21–24 September 2015; pp. 423–430. [Google Scholar]
- Sesen, M.B.; Banares-Alcantara, R.; Fox, J.; Kadir, T.; Brady, J.M. Lung cancer assistant: An ontology-driven, online decision support prototype for lung cancer treatment selection. In Proceedings of the CEUR Workshop, Heraklion, Greece, 27–28 May 2012; Volume 849. [Google Scholar]
- Bystrov, J.W.D. Practice. Neuro-Fuzzy Logic Systems Matlab Toolbox Gui. Cross-Cult. Manag. J. 2015, XVII, 69–76. [Google Scholar]
- Nazari, S.; Fallah, M.; Kazemipoor, H.; Salehipour, A. A Fuzzy Inference- Fuzzy Analytic Hierarchy Process-Based Clinical Decision Support System for Diagnosis of Heart Diseases. Expert Syst. Appl. 2017, 95, 261–271. [Google Scholar] [CrossRef]
- El Sappagh, S.; Elmogy, M.; Riad, A.E.M. A CBR system for diabetes mellitus diagnosis: Case-base standard data model. Int. J. Med. Eng. Inform. 2015, 7, 191. [Google Scholar] [CrossRef]
- Mekruksavanich, S. Medical expert system based ontology for diabetes disease diagnosis. In Proceedings of the 7th IEEE International Conference on Software Engineering and Service Science (ICSESS), Beijing, China, 26–28 August 2016; pp. 383–389. [Google Scholar]
- Lasierra, N.; Alesanco, A.; Guillén, S.; García, J. A three stage ontology-driven solution to provide personalized care to chronic patients at home. J. Biomed. Inform. 2013, 46, 516–529. [Google Scholar] [CrossRef]
- Hussain, A.; Farooq, K.; Luo, B.; Slack, W. A novel ontology and machine learning inspired hybrid cardiovascular decision support framework. In Proceedings of the 2015 IEEE Symposium Series on Computational Intelligence SSCI 2015, Cape Town, South Africa, 7–10 December 2015; pp. 824–832. [Google Scholar]
- Sesen, M. Evaluating OWL 2 reasoners in the context of clinical decision support in lung cancer treatment selection. In Proceedings of the 2nd OWL Reasoning Evaluation Workshop, Oxford, UK, 22 July 2013. [Google Scholar]
- Huddar, V.; Desiraju, B.K.; Rajan, V. Predicting Complications in Critical Care using Heterogeneous Clinical Data. IEEE Access 2016. [Google Scholar] [CrossRef]
- Alves, R.C.A.; Gabriel, L.B.; de Oliveira, B.T.; Margi, C.B.; dos Santos, F.C.L. Assisting Physical (Hydro)Therapy with Wireless Sensors Networks. IEEE Internet Things J. 2015, 2, 113–120. [Google Scholar] [CrossRef]
- Mishra, A.; Agrawal, D.P. Continuous health condition monitoring by 24 × 7 sensing and transmission of physiological data over 5-G cellular channels. In Proceedings of the 2015 International Conference on Computing, Networking and Communications (ICNC), Anaheim, CA, USA, 16–19 February 2015; pp. 584–590. [Google Scholar]
- Papon, M.T.I.; Ahmad, I.; Saquib, N.; Rahman, A. Non-invasive heart rate measuring smartphone applications using on-board cameras: A short survey. In Proceedings of the 2015 International Conference on Networking Systems and Security (NSysS), Dhaka, Bangladesh, 5–7 January 2015; pp. 1–6. [Google Scholar]
- Ajerla, D.; Mahfuz, S.; Zulkernine, F. A Real-Time Patient Monitoring Framework for Fall Detection. Wirel. Commun. Mob. Comput. 2019, 2019. [Google Scholar] [CrossRef]
- Singh, N.R.; Rothe, P.R.; Rathkanthiwar, A.P. Implementation of safety alert system for elderly people using multi-sensors. In Proceedings of the 2017 International Conference of Electronics, Communication and Aerospace Technology ICECA 2017, Coimbatore, India, 20–22 April 2017; Volume 2017, pp. 282–286. [Google Scholar] [CrossRef]
- Sannino, G.; de Falco, I.; de Pietro, G. A supervised approach to automatically extract a set of rules to support fall detection in an mHealth system. Appl. Soft Comput. 2015, 34, 205–216. [Google Scholar] [CrossRef]
- Naslund, J.A.; Marsch, L.A.; McHugo, G.J.; Bartels, S.J. Emerging mHealth and eHealth interventions for serious mental illness: A review of the literature. J. Ment. Health. 2015, 24, 321–332. [Google Scholar] [CrossRef]
- Wang, X.; Desalvo, N.; Zhao, X.; Feng, T.; Loveland, K.A.; Shi, W.; Gnawali, O. Eye contact reminder system for people with autism. In Proceedings of the 6th International Conference on Mobile Computing, Applications and Services, Austin, TX, USA, 6–7 November 2014. [Google Scholar]
- Moshnyaga, V.; Koyanagi, M.; Hirayama, F.; Takahama, A.; Hashimoto, K. A medication adherence monitoring system for people with dementia. In Proceedings of the 2016 IEEE International Conference on Systems, Man, and Cybernetics SMC 2016, Budapest, Hungary, 9–12 October 2016; pp. 194–199. [Google Scholar]
- Lanata, A.; Valenza, G.; Nardelli, M.; Gentili, C.; Scilingo, E.P. Complexity index from a personalized wearable monitoring system for assessing remission in mental health. IEEE J. Biomed. Health Inform. 2015, 19, 132–139. [Google Scholar] [CrossRef]
- Zhan, A.; Little, M.A.; Harris, D.A.; Abiola, S.O.; Dorsey, E.; Saria, S.; Terzis, A. High Frequency Remote Monitoring of Parkinson’s Disease via Smartphone: Platform Overview and Medication Response Detection. arXiv 2019, arXiv:1601.00960. [Google Scholar]
- El-Sappagh, S.; Abuhmed, T.; Islam, S.R.; Kwak, K.S. Multimodal Multitask Deep Learning Model for Alzheimer’s Disease Progression Detection Based on Time Series Data. Neurocomputing 2020, 412, 197–215. [Google Scholar] [CrossRef]
- Dos Costa, D.S.; Turco, S.H.N.; Ramos, R.P.; Silva, F.M.F.M.; Freire, M.S. Electronic monitoring system for measuring heart rate and skin temperature in small ruminants. Eng. Agric. 2018, 38, 166–172. [Google Scholar] [CrossRef]
- Rghioui, A.; Lloret, J.; Harane, M.; Oumnad, A. A Smart Glucose Monitoring System for Diabetic Patient. Electronics 2020, 9, 678. [Google Scholar] [CrossRef]
- El-Sappagh, S.; Ali, F.; Hendawi, A.; Jang, J.H.; Kwak, K.S. A mobile health monitoring-and-treatment system based on integration of the SSN sensor ontology and the HL7 FHIR standard. BMC Med. Inform. Decis. Mak. 2019, 19, 97. [Google Scholar] [CrossRef]
- Rashidi, P.; Mihailidis, A. A survey on ambient-assisted living tools for older adults. IEEE J. Biomed. Health Inform. 2013, 17, 579–590. [Google Scholar] [CrossRef] [PubMed]
- Avgerinakis, K.; Briassouli, A.; Kompatsiaris, I. Recognition of activities of daily living for smart home environments. In Proceedings of the 9th International Conference on Intelligent Environments, Athens, Greece, 18–19 July 2013; pp. 173–180. [Google Scholar]
- Dawadi, P.N.; Cook, D.J.; Schmitter-Edgecombe, M. Automated Cognitive Health Assessment from Smart Home-Based Behavior Data. IEEE J. Biomed. Health Inform. 2016, 20, 1188–1194. [Google Scholar] [CrossRef] [PubMed]
- Dawadi, P.N.; Member, S.; Cook, D.J.; Fellow, I.; Schmitter-edgecombe, M. Smart Home Monitoring of Complex Tasks. IEEE Trans. Syst. Man Cybern. Part C Appl. Rev. 2013, 43, 1302–1313. [Google Scholar] [CrossRef]
- Liu, C.H.; Wen, J.; Yu, Q.; Yang, B.; Wang, W. HealthKiosk: A family-based connected healthcare system for long-term monitoring. In Proceedings of the 2011 IEEE Conference on Computer Communications Workshops (INFOCOM WKSHPS), Shanghai, China, 10–15 April 2011; pp. 241–246. [Google Scholar]
- Majeed, Q.; Hbail, H.; Chalechale, A. A comprehensive mobile e-healthcare system. In Proceedings of the 2015 7th Conference on Information and Knowledge Technology (IKT 2015), Urmia, Iran, 26–28 May 2015; pp. 1–4. [Google Scholar]
- Zhang, J.; Tang, H.; Chen, D.; Zhang, Q. deStress: Mobile and remote stress monitoring, alleviation, and management platform. In Proceedings of the 2012 IEEE Global Communications Conference (GLOBECOM), Anaheim, CA, USA, 3–7 December 2012; pp. 2036–2041. [Google Scholar]
- Duarte, J.M.G.; Cerqueira, E.; Villas, L.A. Indoor patient monitoring through Wi-Fi and mobile computing. In Proceedings of the 2015 7th International Conference on New Technologies, Mobility and Security (NTMS), Paris, France, 26–29 July 2015; pp. 1–5. [Google Scholar]
- Sturiale, A.; Pata, F.; De Simone, V.; Pellino, G.; Campennì, P.; Moggia, E. Internet and social media use among patients with colorectal diseases (ISMAEL): A nationwide survey. Color. Dis. 2020, 22, 1724–1733. [Google Scholar] [CrossRef] [PubMed]
- Ktsui, H. Assistive, Rehabilitation, and Surgical Robots from the Perspective of Medical and Healthcare Professionals; AAAI Press: Menlo Park, CA, USA, 2007. [Google Scholar]
- Shameer, K.; Johnson, K.W.; Yahi, A.; Miotto, R.; Li, L.I.; Ricks, D. Predictive modeling of hospital readmission rates using electronic medical record-wide machine learning: A case-study using mount sinai heart failure cohort. Pac. Symp. Biocomput. 2017, 22, 276–287. [Google Scholar]
- Meyer, A.; Zverinski, D.; Pfahringer, B.; Kempfert, J.; Kuehne, T.; Sündermann, S.H. Machine learning for real-time prediction of complications in critical care: A retrospective study. Lancet Respir. Med. 2018, 6, 905–914. [Google Scholar] [CrossRef]
- Ismail, A.; Abdlerazek, S.; El-Henawy, I. Big data analytics in heart diseases. J. Theor. Appl. Inf. Technol. 2020, 98, 1970–1980. [Google Scholar]
- Boursalie, O.; Samavi, R.; Doyle, T.E. M4CVD: Mobile Machine Learning Model for Monitoring Cardiovascular Disease. Procedia Comput. Sci. 2015, 63, 384–391. [Google Scholar] [CrossRef]
- Alfian, G.; Syafrudin, M.; Ijaz, M.F.; Syaekhoni, M.A.; Fitriyani, N.L.; Rhee, J. A personalized healthcare monitoring system for diabetic patients by utilizing BLE-based sensors and real-time data processing. Sensors 2018, 18, 2183. [Google Scholar] [CrossRef]
- Plis, K.; Bunescu, R.; Marling, C.; Shubrook, J.; Schwartz, F. A machine learning approach to predicting blood glucose levels for diabetes management. In Proceedings of the Workshops at the Twenty-Eighth AAAI Conference on Artificial Intelligence, Québec City, QC, Canada, 27–28 July 2014; pp. 35–39. [Google Scholar]
- Whippy, A. Hospital Deaths in Patients with Sepsis From 2 Independent Cohorts. JAMA 2014, 312, 90–92. [Google Scholar]
- Shashikumar, S.P.; Stanley, M.D.; Sadiq, I.; Li, Q.; Holder, A.; Clifford, G.D.; Nemati, S. Early sepsis detection in critical care patients using multiscale blood pressure and heart rate dynamics. J. Electrocardiol. 2017, 50, 739–743. [Google Scholar] [CrossRef]
- Rello, J.; Leblebicioglu, H. Sepsis and septic shock in low-income and middle-income countries: Need for a different paradigm. Int. J. Infect. Dis. 2016, 48, 120–122. [Google Scholar] [CrossRef]
- Ai, T.; Yang, Z.; Hou, H.; Zhan, C.; Chen, C.; Lv, W. Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology 2020, 296, E32–E40. [Google Scholar] [CrossRef] [PubMed]
- Singh, D.; Kumar, V.; Kaur, M. Classification of COVID-19 patients from chest CT images using multi-objective differential evolution-based convolutional neural networks. Eur. J. Clin. Microbiol. Infect. Dis. 2020. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Kumari, S. Detection of coronavirus Disease (COVID-19) based on Deep Features. Preprints 2020. [Google Scholar] [CrossRef]
- Mshali, H.; Lemlouma, T.; Moloney, M.; Magoni, D. A survey on health monitoring systems for health smart homes. Int. J. Ind. Ergon. 2018, 66, 26–56. [Google Scholar] [CrossRef]
- Nithya, B.; Ilango, V. Predictive analytics in health care using machine learning tools and techniques. In Proceedings of the 2017 International Conference on Intelligent Computing and Control Systems (ICICCS), Madurai, India, 15–16 June 2017; pp. 492–499. [Google Scholar]
- Khianjoom, S.; Usaha, W. Anycast Q-routing in wireless sensor networks for healthcare monitoring. In Proceedings of the 2014 11th International Conference on Electrical Engineering/Electronics, Computer, Telecommunications and Information Technology (ECTI-CON), Nakhon Ratchasima, Thailand, 14–17 May 2014; pp. 1–6. [Google Scholar]
- Jin, M.; Bahadori, M.T.; Colak, A.; Bhatia, P.; Celikkaya, B.; Bhakta, R. Improving Hospital Mortality Prediction with Medical Named Entities and Multimodal Learning. arXiv 2018, arXiv:1811.12276. [Google Scholar]
- Bhattacharya, B.; Mohapatra, S.; Mukhopadhyay, A.P.; Sah, S. Remote cardiovascular health monitoring system with auto-diagnosis. In Proceedings of the 2019 International Conference on Vision Towards Emerging Trends in Communication and Networking (ViTECoN), Vellor, India, 30–31 March 2019; pp. 1–5. [Google Scholar]
- Liu, L.; Wei, W.; Chow, K.H.; Loper, M.; Gursoy, E.; Truex, S.; Wu, Y. Deep Neural Network Ensembles against Deception: Ensemble Diversity, Accuracy and Robustness. arXiv 2019, arXiv:1908.11091. [Google Scholar]
- Tomar, D.; Agarwal, S. A survey on data mining approaches for healthcare. Int. J. Bio-Sci. Bio-Technol. 2013, 5, 241–266. [Google Scholar] [CrossRef]
- Ponsa, P.; Guasch, D. A human-computer interaction approach for healthcare. Univ. Access Inf. Soc. 2018, 17, 1–3. [Google Scholar] [CrossRef]
- Calp, M.H.; Akcayol, M.A. The importance of human computer interaction in the development process of software projects. arXiv 2019, arXiv:1902.02757. [Google Scholar] [CrossRef]
- Liu, P.; Liu, Y. Human computer interaction design for intensive care unit monitors. In Proceedings of the 2nd International Conference on Control, Automation and Artificial Intelligence (CAAI 2017), Sanya, China, 25–26 June 2017; Volume 134, pp. 5–8. [Google Scholar]
- Grespan, L.; Fiorini, P.; Colucci, G. Patient Safety in Robotic Surgery BT—The Route to Patient Safety in Robotic Surgery; Springer International Publishing: Cham, Switzerland, 2019; pp. 7–23. [Google Scholar]
- Kumar, B.; Sharma, L.; Wu, S. Job allocation schemes for Mobile Service Robots in hospitals. In Proceedings of the 2018 IEEE International Conference on Bioinformatics and Biomedicine (BIBM), Madrid, Spain, 3–6 December 2018; pp. 1323–1326. [Google Scholar]
- Twin Robotic X-ray. Available online: https://www.siemens-healthineers.com/robotic-x-ray/twin-robotic-x-ray (accessed on 13 August 2020).
- Samani, H. Robotic Automated External Defibrillator Ambulance for Emergency Medical Service in Smart Cities. IEEE Access 2016. [Google Scholar] [CrossRef]
- Rahmani, A.M.; Thanigaivelan, N.K.; Gia, T.N.; Granados, J. Smart e-health gateway: Bringing intelligence to internet-of-things based ubiquitous healthcare systems. In Proceedings of the 2015 12th Annual IEEE Consumer Communications and Networking Conference (CCNC), Las Vegas, NV, USA, 9–12 January 2015; pp. 826–834. [Google Scholar]
- Elgazzar, K.; Aboelfotoh, M.; Martin, P.; Hassanein, H.S. Ubiquitous health monitoring using mobile web services. Procedia Comput. Sci. 2012, 10, 332–339. [Google Scholar] [CrossRef]
- Help4Mood Project. Available online: http://www.help4mood.info/site/default.aspx. (accessed on 22 July 2018).
- Hassan, M.K.; el Desouky, A.I.; Elghamrawy, S.M.; Sarhan, A.M. Intelligent hybrid remote patient-monitoring model with cloud-based framework for knowledge discovery. Comput. Electr. Eng. 2018, 70, 1–15. [Google Scholar] [CrossRef]
- Zulj, S.; Seketa, G.; Dzaja, D.; Sklebar, F.; Drobnjak, S.; Celic, L.; Magjarevic, R. Supporting diabetic patients with a remote patient monitoring systems. In II Latin American Congress on Biomedical Engineering CLAIB 2016, Bucaramanga, Santander, Colombia, 26–28 October 2016; Springer: Singapore, 2017; Volume 60, pp. 577–580. [Google Scholar]
- Rani, N.S.; Vimala, K.; Kalaivani, V. A remote healthcare monitoring system for faster identification of cardiac abnormalities from compressed ECG using advanced data mining approach. In Proceedings of the Fourth International Conference on Signal and Image Processing 2012 (ICSIP 2012); Springer: New Delhi, India, 2013; Volume 222. [Google Scholar]
- Msayib, Y.; Gaydecki, P.; Callaghan, M.; Dale, N.; Ismail, S. An Intelligent Remote Monitoring System for Total Knee Arthroplasty Patients. J. Med. Syst. 2017, 41, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Zanjal, S.V.; Talmale, G.R. Medicine Reminder and Monitoring System for Secure Health Using IOT. Procedia Comput. Sci. 2016, 78, 471–476. [Google Scholar] [CrossRef]
- Vivekanandan, S.; Devanand, M. Remote monitoring for diabetes disorder: Pilot study using InDiaTel prototype. Eur. Res. Telemed. 2015, 4, 63–69. [Google Scholar] [CrossRef]
- Delrobaei, M.; Memar, S.; Pieterman, M.; Stratton, T.W.; McIsaac, K.; Jog, M. Towards remote monitoring of Parkinson’s disease tremor using wearable motion capture systems. J. Neurol. Sci. 2018, 384, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Woodbridge, J.; Tu, M.K. A Remote Patient Monitoring System for Congestive Heart Failure. J. Med Syst. 2011, 35, 1165–1179. [Google Scholar]
- HEALTH@HOME Project. Available online: http://www.aal-europe.eu/projects/healthhome/ (accessed on 22 July 2018).
- Neveon Projects. Available online: https://nevonprojects.com/iot-patient-health-monitoring-project (accessed on 19 January 2011).
- Banerjee, A.; Ramanujan, R.A.; Agnihothri, S. Mobile health monitoring: Development and implementation of an app in a diabetes and hypertension clinic. Proc. Annu. Hawaii Int. Conf. Syst. Sci. 2016, 2016, 3424–3436. [Google Scholar]
- Kim, I.; Bhagat, Y.A.; Homer, J.; Lobo, R. Multimodal Analog Front-End for Wearable Bio-Sensors. EEE Sens. J. 2016, 16, 8784–8791. [Google Scholar] [CrossRef]
- Sneha, S.; Varshney, U. A framework for enabling patient monitoring via mobile ad hoc network. Decis. Support Syst. 2013, 55, 218–234. [Google Scholar] [CrossRef]
- Sagahyroon, A. Remote patients monitoring: Challenges. In Proceedings of the CCWC 2017: The 7th IEEE Annual Computing and Communication Workshop and Conference, Las Vegas, NV, USA, 9–11 January 2017. [Google Scholar]
- Zhou, J.; Cao, Z.; Dong, X.; Xiong, N.; Vasilakos, A.V. 4S: A secure and privacy-preserving key management scheme for cloud-assisted wireless body area network in m-healthcare social networks. Inf. Sci. 2015, 314, 255–276. [Google Scholar] [CrossRef]
- Alasaarela, E. Secure key management scheme based on ECC algorithm for patient’s medical information in healthcare system. In Proceedings of the International Conference on Information Networking 2014 (ICOIN2014), Phuket, Thailand, 10–12 February 2014; pp. 453–457. [Google Scholar]
- Al-Janabi, S.; Al-Shourbaji, I.; Shojafar, M.; Shamshirband, S. Survey of main challenges (security and privacy) in wireless body area networks for healthcare applications. Egypt. Inform. J. 2017, 18, 113–122. [Google Scholar] [CrossRef]
- Islam, S.M.R.; Kwak, D.; Kabir, M.H.; Hossain, M.; Kwak, K.S. The internet of things for health care: A comprehensive survey. IEEE Access 2015, 3, 678–708. [Google Scholar] [CrossRef]
- Morón, M.J.; Luque, J.R.; Botella, A.A.; Cuberos, E.J.; Casilari, E.; Diaz-Estrella, A.A.A.; Cuberos, E.J.; Casilari, E.; Diaz-Estrella, A. A smart phone-based personal area network for remote monitoring of biosignals. In 4th International Workshop on Wearable and Implantable Body Sensor Networks (BSN 2007); Springer: Berlin/Heidelberg, Germany, 2007; Volume 13, pp. 116–121. [Google Scholar]
- Elhayatmy, G.; Dey, N.; Ashour, A.S. Internet of Things and Big Data Analytics toward Next-Generation Intelligence; Springer: Berlin/Heidelberg, Germany, 2018; Volume 30, pp. 3–20. [Google Scholar]
- Focsa, M.; Mihalas, G.I. EHR Ecosystem. In Pervasive and Mobile Sensing and Computing for Healthcare: Technological and Social Issues; Mukhopadhyay, S.C., Postolache, O.A., Eds.; Springer: Berlin/Heidelberg, Germany, 2013; pp. 251–268. [Google Scholar]
- El-Sappagh, S.; Ali, F.; El-Masri, S.; Kim, K.; Ali, A.; Kwak, K.-S. Mobile Health Technologies for Diabetes Mellitus: Current State and Future Challenges. IEEE Access 2018, 7, 21917–21947. [Google Scholar] [CrossRef]
- Slavíček, K.; Dostál, O.; Lieskovan, T.; Hajný, J. Ensuring security of a telemedicine project in compliance with GDPR. In Proceedings of the 2019 11th International Congress on Ultra Modern Telecommunications and Control Systems and Workshops (ICUMT), Dublin, Ireland, 28–30 October 2019; pp. 1–4. [Google Scholar]
- Mustafa, U.; Pflugel, E.; Philip, N. A novel privacy framework for secure M-Health applications: The Case of the GDPR. In Proceedings of the 2019 IEEE 12th International Conference on Global Security, Safety and Sustainability (ICGS3), London, UK, 16–18 January 2019; pp. 1–9. [Google Scholar]
- Liang, Y.; Chen, Z. Intelligent and Real-Time Data Acquisition for Medical Monitoring in Smart Campus. IEEE Access 2018, 6, 74836–74846. [Google Scholar] [CrossRef]
- Uy, N.Q.; Nam, V.H. A comparison of AMQP and MQTT protocols for Internet of Things. In Proceedings of the 2019 6th NAFOSTED Conference on Information and Computer Science (NICS), Hanoi, Vietnam, 12–13 December 2019; pp. 292–297. [Google Scholar]
| Key Words | Databases | Total Publication Identified | |||||
|---|---|---|---|---|---|---|---|
| # | Science Direct | IEEE | Springer | Scince.gov | PubMed | ||
| 1 | Remote patient monitoring | 326 | 619 | 506 | 699 | 800 | 2950 |
| 2 | Remote patient monitoring AND clinical decision support system | 4 | 160 | 118 | 267 | 29 | 578 |
| 3 | Remote patient monitoring AND ontology | 16 | 18 | 23 | 237 | 44 | 338 |
| 4 | Remote Patient monitoring AND data mining | 24 | 46 | 42 | 84 | 23 | 219 |
| 5 | Remote patient monitoring AND wireless body Area network | 16 | 15 | 30 | 102 | 10 | 173 |
| 6 | Remote patient monitoring AND ontology AND (cloud computing OR Fog computing) | 8 | 7 | 85 | 42 | 2 | 144 |
| 7 | Remote patient monitoring AND ontology AND cloud computing and wireless body area network AND clinical decision support system | 1 | 0 | 5 | 2 | 3 | 11 |
| Total | 395 | 865 | 809 | 1433 | 911 | 4413 | |
| Power Requirement | Frequency | Coverage | Transmission Protocol |
|---|---|---|---|
| Very Low | 2.4 GHz | 70–100 m | Zigbee |
| Medium | 1 MHZ | 10 M | Bluetooth |
| High | 2.4 GHZ | 100 M | Wi-Fi |
| Low | 10 KM | LoRa |
| # | Diseases | Collected Data | Sensor | Transmission Protocol |
|---|---|---|---|---|
| [26] | Heart diseases | ECG | ECG monitor node | Wi-Fi (HTTP, MQTT) |
| [27] | Heart diseases | ECG | ECG fabric sensor embedded on the patient’s chair | Bluetooth |
| [28] | Pain assessment | Facial expression (sEMG) | Wearable sensor with a bio-sensing facial mask | Wi-Fi |
| [29] | Heart diseases | Spo2, blood pressure, ECG | Wi-Fi | |
| [30] | Heart diseases | ECG | Wearable smart clothing | Bluetooth |
| [31] | Dementia | Changes in behaviors and Functional health | Electrodermal Activity (EDA), Photoplenthys (PPG), Accelerometer (ACC) | Wi-Fi |
| [32] | Chronic diseases | Monitor medication adherence | Smart home sensors | Wi-Fi |
| [33] | Chronic diseases | Monitor medication adherence | Wristband wearable sensor | Bluetooth |
| [34] | Fall detection | Monitor mentions and predict falls | Accelerometer, Cardiotachometer | ZigBee |
| [19] | Heart diseases | Spo2, HR | Wireless pulse oximeter | Wi-Fi |
| [35] | Hypertension | Blood pressure | Electronic blood pressure measurement | Bluetooth |
| Factor | Cloud Computing | Fog Computing |
|---|---|---|
| Delaying | High | Low |
| Mobility ability | Limited | Supported |
| Geo-distribution | Centralized | Distributed |
| Bandwidth consumption | High | Low |
| Storage capabilities | Strong | Weak |
| Power consumption | High | Low |
| Location identification | Partially supported | Fully supported |
| Number of servers | Few | Large |
| Real-time interaction | Supported | Supported |
| security | Undefined | Defined |
| Service location | With the Internet | At the edge of the local network |
| Performance | Methods | Data Collection | Diseases | # |
|---|---|---|---|---|
| 99.30% | Ontology, interoperability, CDSS | 115,477 records collected from of 36,162 type 2 diabetic patients | Chronic diseases | [15] |
| - | Ontology, sensors | Ontology tested on “SPARQL” Query | Cardiovascular | [2] |
| 87% | Fuzzy logic, ontology reasoning | The system evaluated in Taichung Hospital in central Taiwan | Diabetes | [89] |
| 97.67% | Fuzzy ontology CBR | 60 real cases from Mansoura university hospitals | Diabetes | [90] |
| Machine learning | 90 patients with gestational diabetes | Diabetes | [77] | |
| 92% | Case base finding | 323 real cases | COPD diseases | [91] |
| 90–95% | Machine learning (24 classifier combination) | 85 patients | Real time monitoring | [92] |
| 89% | Machine learning, ontology | Real-time patient data form Biosensors | Mental disorders | [93] |
| - | Ontology-driven | English lung cancer dataset (LUCADA), approximate (115,000) patient recode | Lung cancer | [94] |
| Factor | HL7 v3 | HL7 FIHR |
|---|---|---|
| Year of initiation | 1997 | 2011 |
| Development Methodology | Top-down | Incremental |
| Semantic ontology | Yes | Yes |
| Architecture | Massages | RESTful web services |
| Tooling required | Yes, just compiler | No |
| Industry support | Weak | Yes |
| Adoption degree | Low | Expected to be high |
| Industry support | Weak | n/a |
| Character support? | Yes (conceptually) | Yes (UTF8) |
| Massage format support | Realm | Global standard |
| # | Diseases | DM | IoT | WBAN | Cloud | Ontology | Interoperability | CDSS |
|---|---|---|---|---|---|---|---|---|
| [15] | Chronic diseases | 🗸 | 🗴 | 🗴 | 🗴 | 🗸 | 🗸 | 🗸 |
| [2] | Cardiovascular | 🗸 | 🗴 | 🗴 | 🗴 | 🗸 | 🗴 | 🗴 |
| [26] | Heart diseases | 🗴 | 🗸 | 🗴 | 🗸 | 🗴 | 🗴 | 🗴 |
| [152] | Ubiquitous monitoring system | 🗸 | 🗸 | 🗸 | 🗸 | 🗴 | 🗸 | 🗸 |
| [28] | Pain assessment | 🗴 | 🗸 | 🗸 | 🗴 | 🗴 | 🗴 | 🗴 |
| [29] | Heart diseases | 🗴 | 🗸 | 🗸 | 🗸 | 🗴 | 🗴 | 🗴 |
| [40] | Knees rehabilitation | 🗴 | 🗴 | 🗸 | 🗸 | 🗴 | 🗴 | 🗴 |
| [153] | Vital signs gathering and processing | 🗸 | 🗴 | 🗴 | 🗸 | 🗴 | 🗴 | 🗴 |
| [46] | Chronic diseases | 🗴 | 🗴 | 🗸 | 🗸 | 🗴 | 🗸 | 🗸 |
| [47] | Hypertension | 🗸 | 🗴 | 🗸 | 🗸 | 🗴 | 🗴 | 🗸 |
| [57] | Tracking daily activities | 🗴 | 🗴 | 🗸 | 🗸 | 🗴 | 🗴 | 🗴 |
| [61] | EXP carried on healthy volunteers | 🗴 | 🗸 | 🗸 | 🗸 | 🗴 | 🗴 | 🗴 |
| [92] | Context aware monitoring | 🗴 | 🗸 | 🗸 | 🗸 | 🗴 | 🗴 | 🗴 |
| [77] | Diabetes and Diet monitoring | 🗴 | 🗸 | 🗴 | 🗴 | 🗴 | 🗴 | 🗸 |
| [96] | Heart diseases | 🗴 | 🗴 | 🗴 | 🗴 | 🗴 | 🗴 | 🗸 |
| [97] | Diabetes | 🗴 | 🗴 | 🗴 | 🗴 | 🗸 | 🗸 | 🗸 |
| [90] | Diabetes | 🗸 | 🗴 | 🗴 | 🗸 | 🗸 | 🗸 | 🗸 |
| [93] | Mental disorder | 🗸 | 🗴 | 🗴 | 🗴 | 🗸 | 🗴 | 🗸 |
| [154] | Chronic diseases | 🗸 | 🗴 | 🗴 | 🗴 | 🗸 | 🗴 | 🗸 |
| [155] | Monitor patients with depression | 🗸 | 🗴 | 🗸 | 🗸 | 🗴 | 🗸 | 🗸 |
| [131] | Cardiovascular diseases | 🗸 | 🗴 | 🗸 | 🗴 | 🗴 | 🗸 | 🗸 |
| [156] | Hypertension, hypotension | 🗸 | 🗸 | 🗸 | 🗸 | 🗴 | 🗴 | 🗸 |
| [157] | Diabetes | 🗸 | 🗴 | 🗸 | 🗴 | 🗴 | 🗴 | 🗴 |
| [158] | Heart diseases | 🗸 | 🗴 | 🗸 | 🗸 | 🗴 | 🗴 | 🗴 |
| [159] | Knee arthroplasty | 🗸 | 🗴 | 🗸 | 🗸 | 🗴 | 🗴 | 🗴 |
| [160] | Elderly | 🗸 | 🗴 | 🗸 | 🗸 | 🗴 | 🗴 | 🗸 |
| [161] | Diabetes | 🗸 | 🗴 | 🗸 | 🗴 | 🗴 | 🗴 | 🗴 |
| [162] | Parkinson’s disease | 🗸 | 🗴 | 🗸 | 🗴 | 🗴 | 🗴 | 🗸 |
| [106] | Fall detection | 🗸 | 🗴 | 🗸 | 🗴 | 🗴 | 🗴 | 🗸 |
| [117] | Diabetes | 🗸 | 🗴 | 🗸 | 🗴 | 🗸 | 🗸 | 🗸 |
| [116] | Alzheimer’s | 🗴 | 🗴 | 🗴 | 🗴 | 🗴 | 🗸 | 🗸 |
| System | Year | Description | Accuracy |
|---|---|---|---|
| Help4Moodproject [155] | 2014 | Health care system designed to help people with depression to return to their normal life, the system consists of three main component, (1) personal server to monitor patient behavior such as sleep activity, (2) interactive agent that interact and collect information from the user through questionnaire (3) DSS that analyze patient collected | |
| SHARE [47] | 2015 | RPM system based on cloud computing, system propose proactive monitoring based on data mining functions, system combine CDSS that designed to respectively train and test the new data and adapt the system to predict vascular for whole the next year. | 67% |
| VISIGNET [46] | 2014 | RPM system for chronic diseases, system monitor vital signs (Body temperature, blood pressure, and heart rate) then send it to the cloud, the system permits patients and physicians to watch health data. In addition to that, they also provide visualization watch that classifies each vital sign according to special criteria. | 95% |
| M4CVD [131] | 2015 | RPM for monitoring cardiovascular diseases that use wearable sensors to collect vital signs (Blood pressure, galvanic skin response (GSR) that indicate stress level, Electrocardiogram (ECG)), the system proposes a contribution to optimizing system effectiveness by analyzing data in the local device (smartphone), it was done using a machine learning algorithm (SVM) that classify patient data and extract the clinical features to determine patient condition “continued risk” or “no longer risk”. | 90.5% |
| WANDA [163] | 2019 | A monitoring system for Cognitive heart failure (CHF) patients, it consists of three tiers (first layer: biosensors for monitoring patient data. Second layer: a web server that store and maintain data integrity layer between different healthcare providers, this layer also analyze data and sends an alert message via text message or emails. Third layer: back-end server backup and recovery layer by making an offline backup) | ---- |
| Health@Home project [164] | 2016 | A remote monitoring system for cardiovascular diseases, the system has client/server architecture. Client-side: located at the patient side, consists of a set of biomedical sensors that measure patients of vital signs (ECG, SPO2, Chest impedance, respiration, blood pressure), then the measured sensors send through the gateway to the server-side. ADSL or mobile broadband (UTMS/GSM) used to transmit data. Server Side: installed at health service facilities, process and analyze data from gateway using the expert system, and make it available for consultation, and finally patient record in the patient information system (HIS). The system also provides an alarm system that sent by a short message to the physician, patient, and relatives. | |
| Nevonprojects [165] | The system is used to track patient health status via two main sensors (temperature sensor and blood pressure sensor). Sensors are connected to a microcontroller that tracks patient status. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
El-Rashidy, N.; El-Sappagh, S.; Islam, S.M.R.; M. El-Bakry, H.; Abdelrazek, S. Mobile Health in Remote Patient Monitoring for Chronic Diseases: Principles, Trends, and Challenges. Diagnostics 2021, 11, 607. https://doi.org/10.3390/diagnostics11040607
El-Rashidy N, El-Sappagh S, Islam SMR, M. El-Bakry H, Abdelrazek S. Mobile Health in Remote Patient Monitoring for Chronic Diseases: Principles, Trends, and Challenges. Diagnostics. 2021; 11(4):607. https://doi.org/10.3390/diagnostics11040607
Chicago/Turabian StyleEl-Rashidy, Nora, Shaker El-Sappagh, S. M. Riazul Islam, Hazem M. El-Bakry, and Samir Abdelrazek. 2021. "Mobile Health in Remote Patient Monitoring for Chronic Diseases: Principles, Trends, and Challenges" Diagnostics 11, no. 4: 607. https://doi.org/10.3390/diagnostics11040607
APA StyleEl-Rashidy, N., El-Sappagh, S., Islam, S. M. R., M. El-Bakry, H., & Abdelrazek, S. (2021). Mobile Health in Remote Patient Monitoring for Chronic Diseases: Principles, Trends, and Challenges. Diagnostics, 11(4), 607. https://doi.org/10.3390/diagnostics11040607








