Comparison of Innovative and Traditional Cardiometabolic Indices in Estimating Atherosclerotic Cardiovascular Disease Risk in Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Demographic Information and Biochemical Data
2.3. Anthropometry Measurement, Anthropometric and Cardiometabolic Indices
2.4. Definition of 10-Year ASCVD Risk
2.5. Statistical Analyses
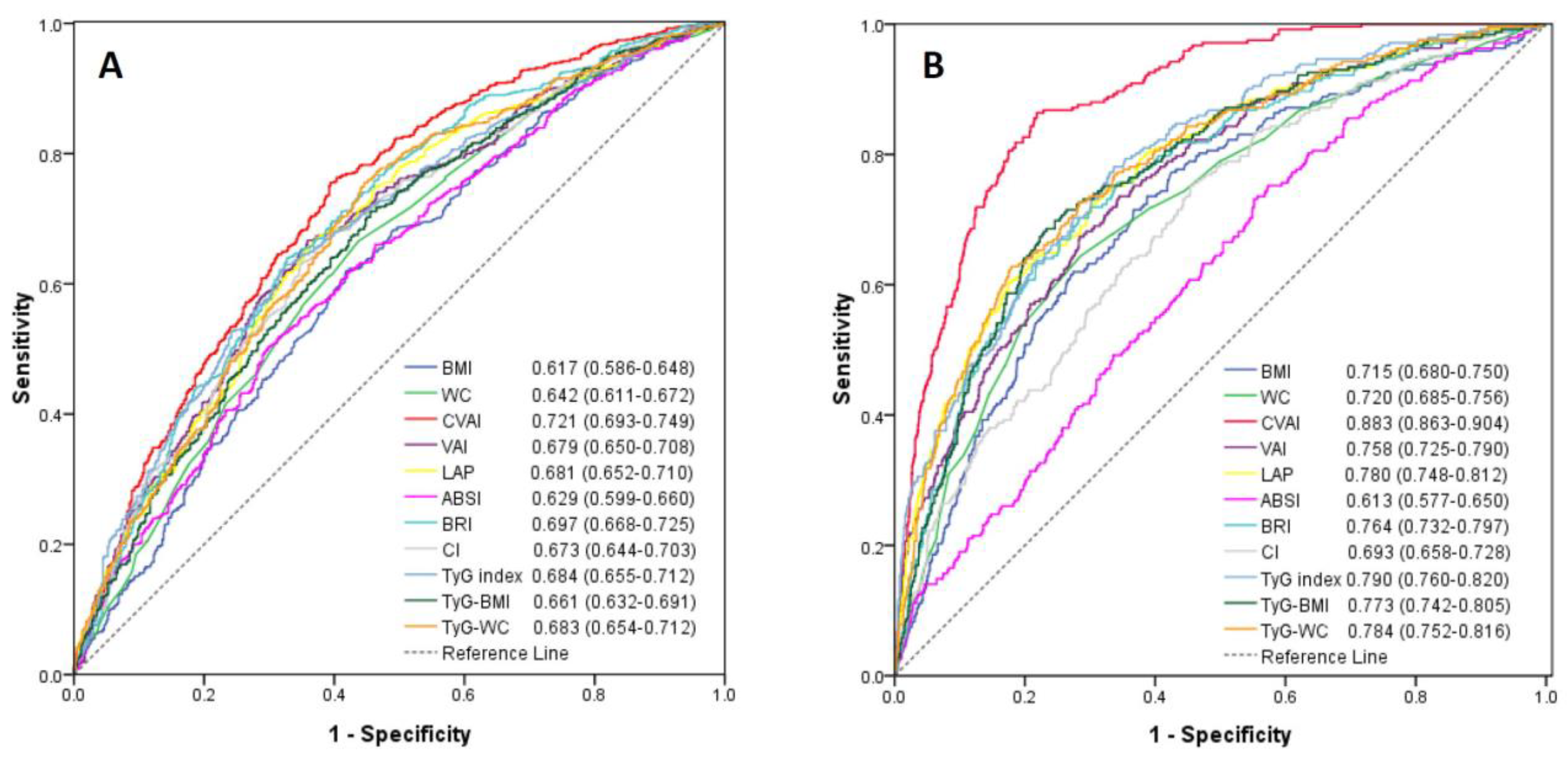
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Roth, G.A.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef]
- Roth, G.A.; Johnson, C.; Abajobir, A.; Abd-Allah, F.; Abera, S.F.; Abyu, G.; Ahmed, M.; Aksut, B.; Alam, T.; Alam, K.; et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J. Am. Coll. Cardiol. 2017, 70, 1–25. [Google Scholar] [CrossRef]
- Greenland, P.; Knoll, M.D.; Stamler, J.; Neaton, J.D.; Dyer, A.R.; Garside, D.B.; Wilson, P.W. Major risk factors as antecedents of fatal and nonfatal coronary heart disease events. JAMA 2003, 290, 891–897. [Google Scholar] [CrossRef] [PubMed]
- Canto, J.G.; Kiefe, C.I.; Rogers, W.J.; Peterson, E.D.; Frederick, P.D.; French, W.J.; Gibson, C.M.; Pollack, C.V., Jr.; Ornato, J.P.; Zalenski, R.J.; et al. Number of coronary heart disease risk factors and mortality in patients with first myocardial infarction. JAMA 2011, 306, 2120–2127. [Google Scholar] [CrossRef]
- Reho, J.J.; Rahmouni, K. Oxidative and inflammatory signals in obesity-associated vascular abnormalities. Clin. Sci. 2017, 131, 1689–1700. [Google Scholar] [CrossRef] [PubMed]
- Van Gaal, L.F.; Mertens, I.L.; De Block, C.E. Mechanisms linking obesity with cardiovascular disease. Nature 2006, 444, 875–880. [Google Scholar] [CrossRef]
- Van de Voorde, J.; Pauwels, B.; Boydens, C.; Decaluwe, K. Adipocytokines in relation to cardiovascular disease. Metabolism 2013, 62, 1513–1521. [Google Scholar] [CrossRef]
- Schinzari, F.; Tesauro, M.; Cardillo, C. Endothelial and Perivascular Adipose Tissue Abnormalities in Obesity-Related Vascular Dysfunction: Novel Targets for Treatment. J. Cardiovasc. Pharmacol. 2017, 69, 360–368. [Google Scholar] [CrossRef]
- Khan, S.S.; Ning, H.; Wilkins, J.T.; Allen, N.; Carnethon, M.; Berry, J.D.; Sweis, R.N.; Lloyd-Jones, D.M. Association of Body Mass Index With Lifetime Risk of Cardiovascular Disease and Compression of Morbidity. JAMA Cardiol. 2018, 3, 280–287. [Google Scholar] [CrossRef]
- Mongraw-Chaffin, M.L.; Peters, S.A.E.; Huxley, R.R.; Woodward, M. The sex-specific association between BMI and coronary heart disease: A systematic review and meta-analysis of 95 cohorts with 1·2 million participants. Lancet Diabetes Endocrinol. 2015, 3, 437–449. [Google Scholar] [CrossRef]
- Goossens, G.H. The Metabolic Phenotype in Obesity: Fat Mass, Body Fat Distribution, and Adipose Tissue Function. Obes. Facts 2017, 10, 207–215. [Google Scholar] [CrossRef]
- Nazare, J.A.; Smith, J.; Borel, A.L.; Aschner, P.; Barter, P.; Van Gaal, L.; Tan, C.E.; Wittchen, H.U.; Matsuzawa, Y.; Kadowaki, T.; et al. Usefulness of measuring both body mass index and waist circumference for the estimation of visceral adiposity and related cardiometabolic risk profile (from the INSPIRE ME IAA study). Am. J. Cardiol. 2015, 115, 307–315. [Google Scholar] [CrossRef]
- Blüher, M.; Laufs, U. New concepts for body shape-related cardiovascular risk: Role of fat distribution and adipose tissue function. Eur. Heart J. 2019, 40, 2856–2858. [Google Scholar] [CrossRef]
- Xia, M.F.; Chen, Y.; Lin, H.D.; Ma, H.; Li, X.M.; Aleteng, Q.; Li, Q.; Wang, D.; Hu, Y.; Pan, B.S.; et al. A indicator of visceral adipose dysfunction to evaluate metabolic health in adult Chinese. Sci. Rep. 2016, 6, 38214. [Google Scholar] [CrossRef]
- Wu, J.; Gong, L.; Li, Q.; Hu, J.; Zhang, S.; Wang, Y.; Zhou, H.; Yang, S.; Wang, Z. A Novel Visceral Adiposity Index for Prediction of Type 2 Diabetes and Pre-diabetes in Chinese adults: A 5-year prospective study. Sci. Rep. 2017, 7, 13784. [Google Scholar] [CrossRef] [PubMed]
- Amato, M.C.; Giordano, C.; Galia, M.; Criscimanna, A.; Vitabile, S.; Midiri, M.; Galluzzo, A. Visceral Adiposity Index: A reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care 2010, 33, 920–922. [Google Scholar] [CrossRef]
- Kouli, G.M.; Panagiotakos, D.B.; Kyrou, I.; Georgousopoulou, E.N.; Chrysohoou, C.; Tsigos, C.; Tousoulis, D.; Pitsavos, C. Visceral adiposity index and 10-year cardiovascular disease incidence: The ATTICA study. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 881–889. [Google Scholar] [CrossRef] [PubMed]
- Mazidi, M.; Kengne, A.P.; Katsiki, N.; Mikhailidis, D.P.; Banach, M. Lipid accumulation product and triglycerides/glucose index are useful predictors of insulin resistance. J. Diabetes Complicat. 2018, 32, 266–270. [Google Scholar] [CrossRef]
- Kyrou, I.; Panagiotakos, D.B.; Kouli, G.M.; Georgousopoulou, E.; Chrysohoou, C.; Tsigos, C.; Tousoulis, D.; Pitsavos, C. Lipid accumulation product in relation to 10-year cardiovascular disease incidence in Caucasian adults: The ATTICA study. Atherosclerosis 2018, 279, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Maessen, M.F.; Eijsvogels, T.M.; Verheggen, R.J.; Hopman, M.T.; Verbeek, A.L.; de Vegt, F. Entering a new era of body indices: The feasibility of a body shape index and body roundness index to identify cardiovascular health status. PLoS ONE 2014, 9, e107212. [Google Scholar] [CrossRef]
- Bertoli, S.; Leone, A.; Krakauer, N.Y.; Bedogni, G.; Vanzulli, A.; Redaelli, V.I.; De Amicis, R.; Vignati, L.; Krakauer, J.C.; Battezzati, A. Association of Body Shape Index (ABSI) with cardio-metabolic risk factors: A cross-sectional study of 6081 Caucasian adults. PLoS ONE 2017, 12, e0185013. [Google Scholar] [CrossRef]
- Andrade, M.D.; Freitas, M.C.; Sakumoto, A.M.; Pappiani, C.; Andrade, S.C.; Vieira, V.L.; Damasceno, N.R. Association of the conicity index with diabetes and hypertension in Brazilian women. Arch. Endocrinol. Metab. 2016, 60, 436–442. [Google Scholar] [CrossRef]
- Lim, J.; Kim, J.; Koo, S.H.; Kwon, G.C. Comparison of triglyceride glucose index, and related parameters to predict insulin resistance in Korean adults: An analysis of the 2007-2010 Korean National Health and Nutrition Examination Survey. PLoS ONE 2019, 14, e0212963. [Google Scholar] [CrossRef] [PubMed]
- Ramdas Nayak, V.K.; Nayak, K.R.; Vidyasagar, S.; Rekha, P. Predictive performance of traditional and novel lipid combined anthropometric indices to identify prediabetes. Diabetes Metab. Syndr. 2020, 14, 1265–1272. [Google Scholar] [CrossRef] [PubMed]
- Zheng, S.; Shi, S.; Ren, X.; Han, T.; Li, Y.; Chen, Y.; Liu, W.; Hou, P.C.; Hu, Y. Triglyceride glucose-waist circumference, a novel and effective predictor of diabetes in first-degree relatives of type 2 diabetes patients: Cross-sectional and prospective cohort study. J. Transl. Med. 2016, 14, 260. [Google Scholar] [CrossRef] [PubMed]
- Shi, W.; Xing, L.; Jing, L.; Tian, Y.; Yan, H.; Sun, Q.; Dai, D.; Shi, L.; Liu, S. Value of triglyceride-glucose index for the estimation of ischemic stroke risk: Insights from a general population. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 245–253. [Google Scholar] [CrossRef]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts)Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar] [CrossRef] [PubMed]
- Goff, D.C., Jr.; Lloyd-Jones, D.M.; Bennett, G.; Coady, S.; D’Agostino, R.B., Sr.; Gibbons, R.; Greenland, P.; Lackland, D.T.; Levy, D.; O’Donnell, C.J.; et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2014, 63, 2935–2959. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., 3rd; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef]
- Kahn, H.S. The “lipid accumulation product” performs better than the body mass index for recognizing cardiovascular risk: A population-based comparison. BMC Cardiovasc. Disord. 2005, 5, 26. [Google Scholar] [CrossRef]
- Krakauer, N.Y.; Krakauer, J.C. A new body shape index predicts mortality hazard independently of body mass index. PLoS ONE 2012, 7, e39504. [Google Scholar] [CrossRef]
- Thomas, D.M.; Bredlau, C.; Bosy-Westphal, A.; Mueller, M.; Shen, W.; Gallagher, D.; Maeda, Y.; McDougall, A.; Peterson, C.M.; Ravussin, E.; et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity 2013, 21, 2264–2271. [Google Scholar] [CrossRef]
- Valdez, R. A simple model-based index of abdominal adiposity. J. Clin. Epidemiol. 1991, 44, 955–956. [Google Scholar] [CrossRef]
- Simental-Mendía, L.E.; Rodríguez-Morán, M.; Guerrero-Romero, F. The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab. Syndr. Relat. Disord. 2008, 6, 299–304. [Google Scholar] [CrossRef] [PubMed]
- Er, L.K.; Wu, S.; Chou, H.H.; Hsu, L.A.; Teng, M.S.; Sun, Y.C.; Ko, Y.L. Triglyceride Glucose-Body Mass Index Is a Simple and Clinically Useful Surrogate Marker for Insulin Resistance in Nondiabetic Individuals. PLoS ONE 2016, 11, e0149731. [Google Scholar] [CrossRef]
- Goff, D.C., Jr.; Lloyd-Jones, D.M.; Bennett, G.; Coady, S.; D’Agostino, R.B.; Gibbons, R.; Greenland, P.; Lackland, D.T.; Levy, D.; O’Donnell, C.J.; et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014, 129, S49–S73. [Google Scholar] [CrossRef] [PubMed]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2019, 74, 1376–1414. [Google Scholar] [CrossRef]
- Benjamin, E.J.; Virani, S.S.; Callaway, C.W.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Chiuve, S.E.; Cushman, M.; Delling, F.N.; Deo, R.; et al. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation 2018, 137, e67–e492. [Google Scholar] [CrossRef] [PubMed]
- Despres, J.P. Body fat distribution and risk of cardiovascular disease: An update. Circulation 2012, 126, 1301–1313. [Google Scholar] [CrossRef]
- Britton, K.A.; Massaro, J.M.; Murabito, J.M.; Kreger, B.E.; Hoffmann, U.; Fox, C.S. Body fat distribution, incident cardiovascular disease, cancer, and all-cause mortality. J. Am. Coll. Cardiol. 2013, 62, 921–925. [Google Scholar] [CrossRef]
- Ponti, F.; Santoro, A.; Mercatelli, D.; Gasperini, C.; Conte, M.; Martucci, M.; Sangiorgi, L.; Franceschi, C.; Bazzocchi, A. Aging and Imaging Assessment of Body Composition: From Fat to Facts. Front. Endocrinol. 2019, 10, 861. [Google Scholar] [CrossRef]
- Zhang, X.; Shu, X.O.; Li, H.; Yang, G.; Xiang, Y.B.; Cai, Q.; Ji, B.T.; Gao, Y.T.; Zheng, W. Visceral adiposity and risk of coronary heart disease in relatively lean Chinese adults. Int. J. Cardiol. 2013, 168, 2141–2145. [Google Scholar] [CrossRef]
- Wei, J.; Liu, X.; Xue, H.; Wang, Y.; Shi, Z. Comparisons of Visceral Adiposity Index, Body Shape Index, Body Mass Index and Waist Circumference and Their Associations with Diabetes Mellitus in Adults. Nutrients 2019, 11, 1580. [Google Scholar] [CrossRef]
- Koloverou, E.; Panagiotakos, D.B.; Kyrou, I.; Stefanadis, C.; Chrysohoou, C.; Georgousopoulou, E.N.; Skoumas, I.; Tousoulis, D.; Pitsavos, C.; The ATTICA Study Group. Visceral adiposity index outperforms common anthropometric indices in predicting 10-year diabetes risk: Results from the ATTICA study. Diabetes Metab. Res. Rev. 2019, 35, e3161. [Google Scholar] [CrossRef] [PubMed]
- Han, M.; Qin, P.; Li, Q.; Qie, R.; Liu, L.; Zhao, Y.; Liu, D.; Zhang, D.; Guo, C.; Zhou, Q.; et al. Chinese visceral adiposity index: A reliable indicator of visceral fat function associated with risk of type 2 diabetes. Diabetes Metab. Res. Rev. 2021, 37, e3370. [Google Scholar] [CrossRef]
- Lee, J.J.; Pedley, A.; Hoffmann, U.; Massaro, J.M.; Fox, C.S. Association of Changes in Abdominal Fat Quantity and Quality with Incident Cardiovascular Disease Risk Factors. J. Am. Coll. Cardiol. 2016, 68, 1509–1521. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Inigo, L.; Navarro-Gonzalez, D.; Fernandez-Montero, A.; Pastrana-Delgado, J.; Martinez, J.A. The TyG index may predict the development of cardiovascular events. Eur. J. Clin. Investig. 2016, 46, 189–197. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Guo, B.; Chen, H.; Shi, Z.; Li, Y.; Tian, Q.; Shi, S. The role of the triglyceride (triacylglycerol) glucose index in the development of cardiovascular events: A retrospective cohort analysis. Sci. Rep. 2019, 9, 7320. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Liu, A.; Zhao, T.; Gong, X.; Pang, T.; Zhou, Y.; Xiao, Y.; Yan, Y.; Fan, C.; Teng, W.; et al. Comparison of anthropometric indices for predicting the risk of metabolic syndrome and its components in Chinese adults: A prospective, longitudinal study. BMJ Open 2017, 7, e016062. [Google Scholar] [CrossRef]
- Baveicy, K.; Mostafaei, S.; Darbandi, M.; Hamzeh, B.; Najafi, F.; Pasdar, Y. Predicting Metabolic Syndrome by Visceral Adiposity Index, Body Roundness Index and a Body Shape Index in Adults: A Cross-Sectional Study from the Iranian RaNCD Cohort Data. Diabetes Metab. Syndr. Obes. 2020, 13, 879–887. [Google Scholar] [CrossRef]

| Variables | Men | Women | ||||
|---|---|---|---|---|---|---|
| ASCVD Risk <7.5% (n = 538) | ASCVD Risk ≥7.5% (n = 810) | p-Value | ASCVD Risk <7.5% (n = 1553) | ASCVD Risk ≥7.5% (n = 242) | p-Value | |
| Age (years) | 41.7 ± 7.1 | 53.9 ± 7.3 | <0.001 | 46.2 ± 8.1 | 58.9 ± 6.6 | <0.001 |
| Diabetes mellitus (%) | 0 | 7.8 | <0.001 | 0.6 | 14.9 | <0.001 |
| Hypertension (%) | 3.0 | 26.4 | <0.001 | 2.1 | 38.4 | <0.001 |
| Dyslipidemia (%) | 1.9 | 2.0 | 0.525 | 1.1 | 0 | 0.151 |
| Current smoking (%) | 3.9 | 19.9 | <0.001 | 0.4 | 0.8 | 0.295 |
| Systolic BP (mmHg) | 119.4 ± 11.0 | 129.3 ± 13.2 | <0.001 | 115.7 ± 12.2 | 137.4 ± 15.0 | <0.001 |
| Diastolic BP (mmHg) | 74.3 ± 9.6 | 80.9 ± 11.1 | <0.001 | 70.3 ± 9.5 | 82.4 ± 11.0 | <0.001 |
| Cardiometabolic Indices | ||||||
| BMI (kg/m2) | 24.5 ± 3.3 | 25.9 ± 3.6 | <0.001 | 22.4 ± 3.2 | 24.8 ± 3.6 | <0.001 |
| WC (cm) | 84.5 ± 8.3 | 88.6 ± 8.8 | <0.001 | 73.3 ± 7.4 | 79.5 ± 8.4 | <0.001 |
| CVAI | 77.9 ± 37.6 | 108.2 ± 38.2 | <0.001 | 48.0 ± 31.4 | 98.8 ± 29.3 | <0.001 |
| VAI | 1.34 ± 1.15 | 2.10 ± 1.90 | <0.001 | 1.25 ± 1.06 | 2.89 ± 3.60 | <0.001 |
| LAP | 26.2 ± 23.5 | 43.2 ± 41.9 | <0.001 | 16.8 ± 16.8 | 43.2 ± 47.7 | <0.001 |
| ABSI | 0.076 ± 0.003 | 0.078 ± 0.003 | <0.001 | 0.073 ± 0.004 | 0.075 ± 0.004 | <0.001 |
| BRI | 3.20 ± 0.88 | 3.82 ± 1.01 | <0.001 | 2.68 ± 0.85 | 3.60 ± 1.07 | <0.001 |
| CI | 1.19 ± 0.06 | 1.23 ± 0.06 | <0.001 | 1.13 ± 0.06 | 1.17 ± 0.07 | <0.001 |
| TyG index | 9.13 ± 0.57 | 9.51 ± 0.60 | <0.001 | 8.91 ± 0.53 | 9.58 ± 0.66 | <0.001 |
| TyG-BMI | 224.6 ± 37.3 | 246.9 ± 42.4 | <0.001 | 199.7 ± 35.0 | 238.5 ± 43.2 | <0.001 |
| TyG-WC | 772.7 ± 103.3 | 844.3 ± 115.1 | <0.001 | 654.2 ± 89.4 | 764.0 ± 113.6 | <0.001 |
| Laboratory Data | ||||||
| Fasting glucose (mg/dL) | 97.7 ± 12.3 | 106.6 ± 24.6 | <0.001 | 94.8 ± 11.4 | 110.6 ± 27.7 | <0.001 |
| Total cholesterol (mg/dL) | 196.4 ± 32.9 | 207.1 ± 38.4 | <0.001 | 202.9 ± 34.3 | 230.2 ± 43.6 | <0.001 |
| HDL-C (mg/dL) | 51.5 ± 12.2 | 45.4 ± 11.0 | <0.001 | 61.6 ± 13.9 | 53.1 ± 13.1 | <0.001 |
| LDL-C (mg/dL) | 119.7 ± 28.6 | 128.2 ± 33.4 | <0.001 | 118.2 ± 30.0 | 139.2 ± 39.4 | <0.001 |
| Triglycerides (mg/dL) | 93.0 (67.0−132.0) | 130.0 (87.0−185.0) | <0.001 | 76.0 (55.0−107.0) | 126.0 (89.0−196.5) | <0.001 |
| Uric acid (mg/dL) | 6.39 ± 1.14 | 6.48 ± 1.30 | 0.166 | 4.70 ± 0.92 | 5.38 ± 1.06 | <0.001 |
| hs-CRP (mg/L) | 0.56 (0.27−1.22) | 0.81 (0.40−1.79) | 0.026 | 0.53 (0.24−1.21) | 1.05 (0.55−2.56) | 0.002 |
| eGFR (mL/min/1.73 m2) | 91.6 ± 10.4 | 85.3 ± 16.3 | 0.001 | 102.5 ± 20.0 | 97.7 ± 20.6 | 0.001 |
| Proteinuria (%) | 4.3 | 8.8 | <0.001 | 4.0 | 4.5 | 0.726 |
| Cardiometabolic Indices | Men | Women | ||
|---|---|---|---|---|
| Unadjusted OR (95% Confidence Interval) | Adjusted OR (95% Confidence Interval) | Unadjusted OR (95% Confidence Interval) | Adjusted OR (95% Confidence Interval) | |
| BMI (per 1 kg/m2) | 1.127 (1.088–1.167) | 1.213 (1.129–1.303) | 1.209 (1.164–1.255) | 1.200 (1.115–1.291) |
| WC (per 1 cm) | 1.060 (1.045–1.075) | 1.105 (1.072–1.138) | 1.096 (1.077–1.114) | 1.064 (1.032–1.096) |
| CVAI (per 10 unit) | 1.250 (1.207–1.294) | 1.399 (1.297–1.510) | 1.644 (1.550–1.744) | 1.451 (1.316–1.601) |
| VAI (per 1 unit) | 1.607 (1.438–1.795) | 2.972 (2.380–3.713) | 1.751 (1.580–1.940) | 1.888 (1.612–2.212) |
| LAP (per 10 unit) | 1.258 (1.194–1.325) | 1.568 (1.414–1.739) | 1.480 (1.388–1.578) | 1.502 (1.358–1.661) |
| ABSI (per 0.01 unit) | 3.959 (2.819–5.561) | 3.151 (1.704–5.828) | 2.533 (1.847–3.473) | 1.026 (0.611–1.720) † |
| BRI (per 1 unit) | 2.178 (1.887–2.514) | 2.427 (1.851–3.181) | 2.458 (2.132–2.834) | 1.825 (1.418–2.349) |
| CI (per 0.1 unit) | 3.071 (2.483–3.799) | 3.275 (2.200–4.874) | 2.719 (2.208–3.350) | 1.374 (0.985–1.916) ‡ |
| TyG index (per 1 unit) | 3.151 (2.554–3.889) | 10.014 (6.228–16.101) | 7.108 (5.408–9.343) | 6.691 (4.205–10.649) |
| TyG-BMI (per 100 unit) | 4.467 (3.252–6.135) | 20.381 (9.854–42.153) | 9.682 (6.837–13.710) | 12.846 (6.385–25.844) |
| TyG WC (per 100 unit) | 1.864 (1.661–2.091) | 3.721 (2.812–4.923) | 2.733 (2.367–3.155) | 2.570 (1.967–3.359) |
| Cardiometabolic Indices | Men | Women | ||||||
|---|---|---|---|---|---|---|---|---|
| Cut-Off Value | Sensitivity (%) | Specificity (%) | Youden Index | Cut-Off Value | Sensitivity (%) | Specificity (%) | Youden Index | |
| BMI (kg/m2) | 24.6 | 62.0 | 58.2 | 0.202 | 22.7 | 71.5 | 63.3 | 0.348 |
| WC (cm) | 84.8 | 66.5 | 56.1 | 0.226 | 76.8 | 64.5 | 71.4 | 0.359 |
| CVAI | 83.7 | 75.6 | 60.6 | 0.362 | 70.8 | 86.3 | 78.2 | 0.645 |
| VAI | 1.23 | 66.7 | 64.1 | 0.308 | 1.26 | 73.6 | 65.6 | 0.392 |
| LAP | 23.9 | 67.0 | 62.8 | 0.298 | 25.5 | 60.3 | 82.5 | 0.428 |
| ABSI | 0.078 | 50.4 | 70.0 | 0.204 | 0.073 | 73.1 | 44.8 | 0.179 |
| BRI | 3.41 | 64.0 | 67.3 | 0.313 | 3.01 | 70.2 | 71.7 | 0.419 |
| CI | 1.20 | 67.9 | 60.6 | 0.285 | 1.13 | 75.2 | 54.6 | 0.298 |
| TyG index | 9.33 | 62.8 | 67.7 | 0.305 | 9.10 | 78.1 | 66.3 | 0.444 |
| TyG-BMI | 222.9 | 71.1 | 54.5 | 0.256 | 218.4 | 68.6 | 76.7 | 0.453 |
| TyG-WC | 770.2 | 75.6 | 55.4 | 0.310 | 726.3 | 62.8 | 82.0 | 0.448 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, Y.-C.; Huang, J.-C.; Lin, C.-I.; Chien, H.-H.; Lin, Y.-Y.; Wang, C.-L.; Liang, F.-W.; Dai, C.-Y.; Chuang, H.-Y. Comparison of Innovative and Traditional Cardiometabolic Indices in Estimating Atherosclerotic Cardiovascular Disease Risk in Adults. Diagnostics 2021, 11, 603. https://doi.org/10.3390/diagnostics11040603
Huang Y-C, Huang J-C, Lin C-I, Chien H-H, Lin Y-Y, Wang C-L, Liang F-W, Dai C-Y, Chuang H-Y. Comparison of Innovative and Traditional Cardiometabolic Indices in Estimating Atherosclerotic Cardiovascular Disease Risk in Adults. Diagnostics. 2021; 11(4):603. https://doi.org/10.3390/diagnostics11040603
Chicago/Turabian StyleHuang, Ya-Chin, Jiun-Chi Huang, Chia-I Lin, Hsu-Han Chien, Yu-Yin Lin, Chao-Ling Wang, Fu-Wen Liang, Chia-Yen Dai, and Hung-Yi Chuang. 2021. "Comparison of Innovative and Traditional Cardiometabolic Indices in Estimating Atherosclerotic Cardiovascular Disease Risk in Adults" Diagnostics 11, no. 4: 603. https://doi.org/10.3390/diagnostics11040603
APA StyleHuang, Y.-C., Huang, J.-C., Lin, C.-I., Chien, H.-H., Lin, Y.-Y., Wang, C.-L., Liang, F.-W., Dai, C.-Y., & Chuang, H.-Y. (2021). Comparison of Innovative and Traditional Cardiometabolic Indices in Estimating Atherosclerotic Cardiovascular Disease Risk in Adults. Diagnostics, 11(4), 603. https://doi.org/10.3390/diagnostics11040603








