Minimally Invasive Intracerebral Hemorrhage Evacuation Techniques: A Review
Abstract
1. Introduction
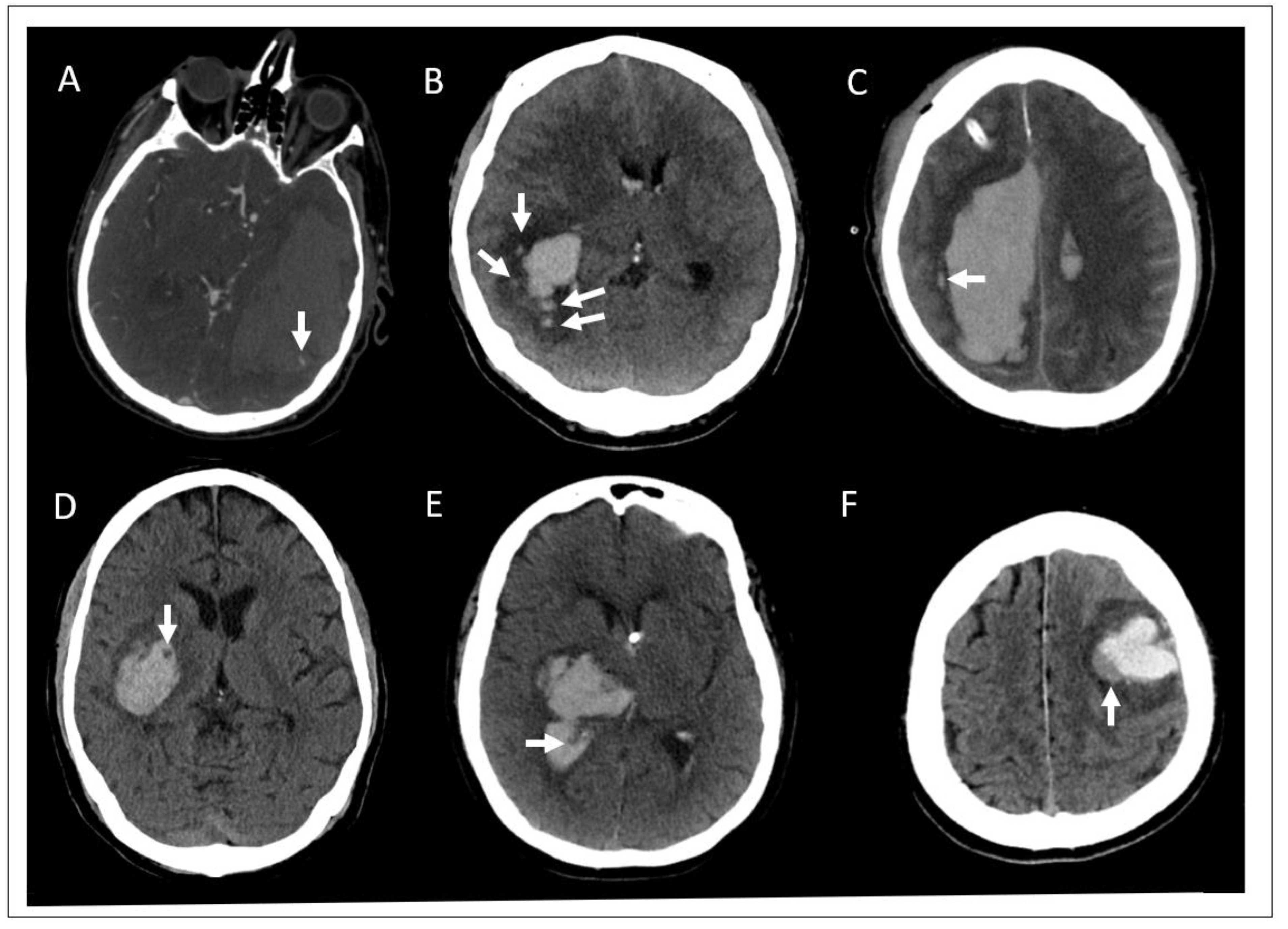
2. Intracerebral Hemorrhage (ICH) Diagnosis and Imaging
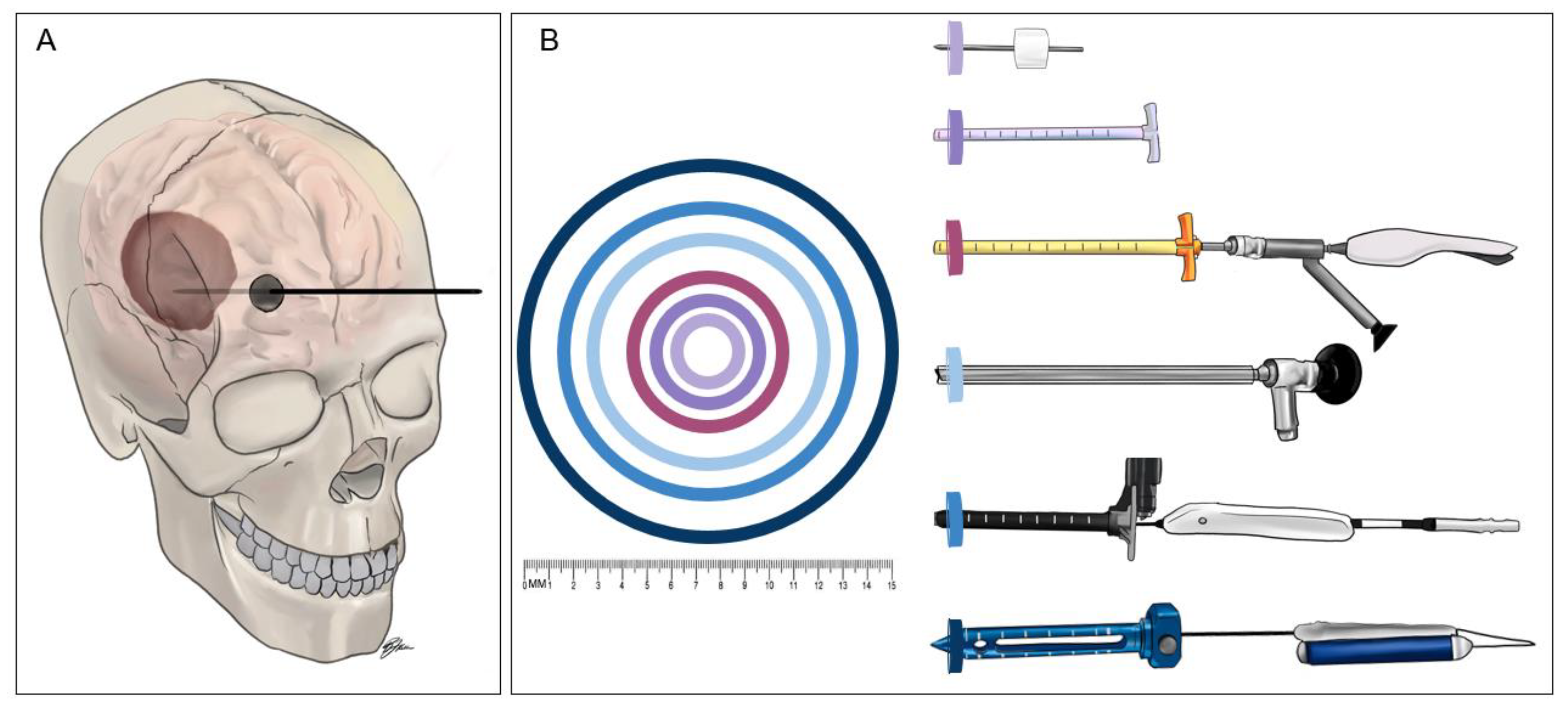
3. Minimally Invasive Surgery (MIS) for ICH Techniques
4. Thrombolytic Techniques
4.1. Craniopuncture
4.2. Stereotactic Aspiration with Thrombolysis
5. Non-Thrombolytic Techniques
5.1. Endoport-Mediated Evacuation
5.2. Endoscope-Assisted Evacuation
5.3. Adjunctive Aspiration Devices
5.4. Surgiscope
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- An, S.J.; Kim, T.J.; Yoon, B.-W. Epidemiology, risk factors, and clinical features of intracerebral hemorrhage: An update. J. Stroke 2017, 19, 3–10. [Google Scholar] [CrossRef]
- Caceres, J.A.; Goldstein, J.N. Intracranial hemorrhage. Emerg. Med. Clin. N. Am. 2012, 30, 771–794. [Google Scholar] [CrossRef]
- Hemphill, J.C.; Greenberg, S.M.; Anderson, C.S.; Becker, K.; Bendok, B.R.; Cushman, M.; Fung, G.L.; Goldstein, J.N.; Macdonald, R.L.; Mitchel, P.H.; et al. Guidelines for the management of spontaneous intracerebral hemorrhage. Stroke 2015, 46, 2032–2060. [Google Scholar] [CrossRef]
- Mendelow, A.D.; Gregson, B.A.; Rowan, E.N.; Murray, G.D.; Gholkar, A.; Mitchel, P.M. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial lobar intracerebral haematomas (STICH II): A randomised trial. Lancet 2013, 382, 397–408. [Google Scholar] [CrossRef]
- Mendelow, A.D.; Gregson, B.A.; Fernandes, H.M.; Murray, G.D.; Teasdale, G.M.; Hope, A.; Larimi, M.; Shaw, D.; Barer, D.H. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial intracerebral haematomas in the international surgical trial in intracerebral haemorrhage (STICH): A randomised trial. Lancet 2005, 365, 387–397. [Google Scholar] [CrossRef]
- Urday, S.; Beslow, L.A.; Dai, F.; Zhang, F.; Battey, T.; Vashkevich, A.; Ayres, A.; Lasure, A.; Selim, M.; Simard, J.; et al. Rate of perihematomal edema expansion predicts outcome after intracerebral hemorrhage. Crit. Care Med. 2016, 44, 790–797. [Google Scholar] [CrossRef]
- Wada, R.; Aviv Richard, I.; Fox Allan, J.; Demetrios, S.; Gladstone, D.; Tomlinson, G.; Symons, S. CT angiography “spot sign” predicts hematoma expansion in acute intracerebral hemorrhage. Stroke 2007, 38, 1257–1262. [Google Scholar] [CrossRef]
- Morotti, A.; Boulouis, G.; Dowlatshahi, D.; Li, Q.; Barras, C.D.; Delcourt, C.; Yu, Z.; Zheng, J.; Zhou, Z.; Aviv, R.I.; et al. Standards for detecting, interpreting, and reporting noncontrast computed tomographic markers of intracerebral hemorrhage expansion. Ann. Neurol. 2019, 86, 480–492. [Google Scholar] [CrossRef]
- Sporns, P.B.; Kemmling, A.; Minnerup, J.; Hanning, U.; Heindel, W. Imaging-based outcome prediction in patients with intracerebral hemorrhage. Acta Neurochir. 2018, 160, 1663–1670. [Google Scholar] [CrossRef]
- Yu, Z.; Zheng, J.; Ali, H.; Guo, R.; Li, M.; Wang, X.; Ma, L.; Li, H.; You, C. Significance of satellite sign and spot sign in predicting hematoma expansion in spontaneous intracerebral hemorrhage. Clin. Neurol. Neurosurg. 2017, 162, 67–71. [Google Scholar] [CrossRef]
- Shimoda, Y.; Ohtomo, S.; Arai, H.; Okada, K.; Tominaga, T. Satellite sign: A poor outcome predictor in intracerebral hemorrhage. Cerebrovasc. Dis. 2017, 44, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Deng, L.; Zhang, G.; Wei, X.; Yang, W.S.; Li, R.; Shen, Y.Q.; Xie, X.F.; Lv, X.N.; Li, Y.L.; Zhao, L.B.; et al. Comparison of satellite sign and island sign in predicting hematoma growth and poor outcome in patients with primary intracerebral hemorrhage. World Neurosurg. 2019, 127, e818–e825. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Luo, Y.; Chen, S.; Luo, X.; Li, B.; Chen, S.; Zhou, Y.; Xia, Y. The predictive accuracy of satellite sign for hematoma expansion in intracerebral hemorrhage: A meta-analysis. Clin. Neurol. Neurosurg. 2020, 197, 106139. [Google Scholar] [CrossRef]
- Li, Q.; Liu, Q.J.; Yang, W.S.; Wang, X.C.; Zhao, L.B.; Xiong, X.; Li, R.; Cao, D.; Zhu, D.; Wei, X.; et al. Island sign: An imaging predictor for early hematoma expansion and poor outcome in patients with intracerebral hemorrhage. Stroke 2017, 48, 3019–3025. [Google Scholar] [CrossRef]
- Wei, Y.; Zhu, G.; Gao, Y.; Chang, J.; Zhang, H.; Liu, N.; Tian, C.; Jiang, P.; Gao, Y. Island sign predicts hematoma expansion and poor outcome after intracerebral hemorrhage: A systematic review and meta-analysis. Front. Neurol. 2020, 11, 429. [Google Scholar] [CrossRef]
- Zhang, F.; Zhang, S.; Tao, C.; Yang, Z.; You, C.; Yang, M. The comparative study of island sign and the spot sign in predicting short-term prognosis of patients with intracerebral hemorrhage. J. Neurol. Sci. 2019, 396, 133–139. [Google Scholar] [CrossRef]
- Ng, D.; Churilov, L.; Mitchell, P.; Dowling, R.; Yan, B. The ct swirl sign is associated with hematoma expansion in intracerebral hemorrhage. Am. J. Neurorad. 2018, 39, 232–237. [Google Scholar] [CrossRef]
- Xiong, X.; Li, Q.; Yang, W.S.; Wei, X.; Hu, X.; Wang, X.C.; Zhu, D.; Li, R.; Cao, D.; Xie, P. Comparison of swirl sign and black hole sign in predicting early hematoma growth in patients with spontaneous intracerebral hemorrhage. Med. Sci. Monit. 2018, 24, 567–573. [Google Scholar] [CrossRef]
- Park, B.K.; Kwak, H.S.; Chung, G.H.; Hwang, S.B. Diagnostic value of swirl sign on noncontrast computed tomography and spot sign on computed tomographic angiography to predict intracranial hemorrhage expansion. Clin. Neurol. Neurosurg. 2019, 182, 130–135. [Google Scholar] [CrossRef]
- Selariu, E.; Zia, E.; Brizzi, M.; Abul-Kasim, K. Swirl sign in intracerebral haemorrhage: Definition, prevalence, reliability and prognostic value. BMC Neurol. 2012, 12, 109. [Google Scholar] [CrossRef]
- Li, Q.; Zhang, G.; Xiong, X.; Wang, X.C.; Yang, W.S.; Li, K.W.; Wei, X.; Xie, P. Black hole sign: Novel imaging marker that predicts hematoma growth in patients with intracerebral hemorrhage. Stroke 2016, 47, 1777–1781. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Yang, W.S.; Chen, S.L.; Lv, F.R.; Lv, F.J.; Hu, X.; Zhu, D.; Cao, D.; Wang, X.C.; Li, R.; et al. Black hole sign predicts poor outcome in patients with intracerebral hemorrhage. Cerebrovasc. Dis. 2018, 45, 48–53. [Google Scholar] [CrossRef]
- Sporns, P.B.; Schwake, M.; Kemmling, A.; Minnerup, J.; Schwindt, W.; Niederstadt, T.; Schmidt, R.; Hanning, U. Comparison of spot sign, blend sign and black hole sign for outcome prediction in patients with intracerebral hemorrhage. J. Stroke 2017, 19, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Yu, Z.; Zheng, J.; Ma, L.; Guo, R.; Li, M.; Wang, X.; Lin, S.; Li, H.; You, C. The predictive accuracy of the black hole sign and the spot sign for hematoma expansion in patients with spontaneous intracerebral hemorrhage. Neurol. Sci. 2017, 38, 1591–1597. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.W.; Yang, M.F. Combining investigation of imaging markers (island sign and blend sign) and clinical factors in predicting hematoma expansion of intracerebral hemorrhage in the basal ganglia. World Neurosurg. 2018, 120, e1000–e1010. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Zhang, G.; Huang, Y.-J.; Dong, M.-X.; Lv, F.-J.; Wei, X.; Chen, J.-J.; Zhang, L.-J.; Qin, X.-Y.; Xie, P. Blend sign on computed tomography: Novel and reliable predictor for early hematoma growth in patients with intracerebral hemorrhage. Stroke 2015, 46, 2119–2123. [Google Scholar] [CrossRef]
- Li, Q.; Yang, W.-S.; Wang, X.-C.; Cao, D.; Zhu, D.; Lv, F.-J.; Liu, Y.; Yuan, L.; Zhang, G.; Xiong, X.; et al. Blend sign predicts poor outcome in patients with intracerebral hemorrhage. PLoS ONE 2017, 12, e0183082. [Google Scholar] [CrossRef]
- Yu, Z.; Zheng, J.; Guo, R.; Ma, L.; Li, M.; Wang, X.; Lin, S.; Li, H.; You, C. Performance of blend sign in predicting hematoma expansion in intracerebral hemorrhage: A meta-analysis. Clin. Neurol. Neurosurg. 2017, 163, 84–89. [Google Scholar] [CrossRef]
- Sporns, P.B.; Schwake, M.; Schmidt, R.; Kemmling, A.; Minnerup, J.; Schwindt, W.; Cnyrim, C.; Zoubi, T.; Heindel, W.; Niederstadt, T.; et al. Computed tomographic blend sign is associated with computed tomographic angiography spot sign and predicts secondary neurological deterioration after intracerebral hemorrhage. Stroke 2017, 48, 131–135. [Google Scholar] [CrossRef]
- Hersh, E.H.; Gologorsky, Y.; Chartrain, A.G.; Mocco, J.; Kellner, C.P. Minimally invasive surgery for intracerebral hemorrhage. Curr. Neurol. Neurosci. Rep. 2018, 18, 34. [Google Scholar] [CrossRef]
- Wang, W.Z.; Jiang, B.; Liu, H.M.; Li, D.; Lu, C.Z.; Zhao, Y.D.; Sander, J.W. Minimally invasive craniopuncture therapy vs. Conservative treatment for spontaneous intracerebral hemorrhage: Results from a randomized clinical trial in China. Int. J. Stroke 2009, 4, 11–16. [Google Scholar] [CrossRef]
- Pan, J.; Chartrain, A.G.; Scaggiante, J.; Spiotta, A.M.; Tang, Z.; Wang, W.; Pradilla, G.; Murayama, Y.; Mori, R.; Mocco, J.; et al. A compendium of modern minimally invasive intracerebral hemorrhage evacuation techniques. Oper. Neurosurg. 2020, 18, 710–720. [Google Scholar] [CrossRef]
- Sun, H.; Liu, H.; Li, D.; Liu, L.; Yang, J.; Wang, W. An effective treatment for cerebral hemorrhage: Minimally invasive craniopuncture combined with urokinase infusion therapy. Neurol. Res. 2010, 32, 371–377. [Google Scholar] [CrossRef]
- Zhou, H.; Zhang, Y.; Liu, L.; Han, X.; Tao, Y.; Tang, Y.; Hua, W.; Xue, J.; Dong, Q. A prospective controlled study: Minimally invasive stereotactic puncture therapy versus conventional craniotomy in the treatment of acute intracerebral hemorrhage. BMC Neurol. 2011, 11, 76. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.F.; Cheng, C.; You, C. A new modified twist drill craniostomy using a novel device to evacuate chronic subdural hematoma. Medicine 2016, 95, e3036. [Google Scholar] [CrossRef]
- Zhao, X.; Jiang, H.; Liu, G.; Wang, T. Efficacy analysis of 33 cases with epidural hematoma treated by brain puncture under ct surveillance. Turk. Neurosurg. 2014, 24, 323. [Google Scholar] [CrossRef]
- Ge, C.; Zhao, W.; Guo, H.; Sun, Z.; Zhang, W.; Li, X.; Yang, X.; Zhang, J.; Wang, D.; Xiang, Y.; et al. Comparison of the clinical efficacy of craniotomy and craniopuncture therapy for the early stage of moderate volume spontaneous intracerebral haemorrhage in basal ganglia: Using the cta spot sign as an entry criterion. Clin. Neurol. Neurosurg. 2018, 169, 41–48. [Google Scholar] [CrossRef]
- Teernstra, O.P.M.; Evers, S.; Lodder, J.; Leffers, P.; Franke, C.; Blaauw, G.J.S. Stereotactic treatment of intracerebral hematoma by means of a plasminogen activator: A multicenter randomized controlled trial (SICHPA). Stroke 2003, 34, 968–974. [Google Scholar] [CrossRef]
- Hanley, D.F.; Thompson, R.E.; Rosenblum, M.; Yenokyan, G.; Lane, K.; McBee, N.; Mayo, S.W.; Bistran-Hall, A.J.; Gandhi, D.; Mould, W.A.; et al. Efficacy and safety of minimally invasive surgery with thrombolysis in intracerebral haemorrhage evacuation (MISTIE III): A randomised, controlled, open-label, blinded endpoint phase 3 trial. Lancet 2019, 393, 1021–1032. [Google Scholar] [CrossRef]
- Auer, L.M.; Deinsberger, W.; Niederkorn, K.; Gell, G.; Kleinert, R.; Schneider, G.; Holzer, P.; Bone, G.; Mokry, M.; Körner, E.; et al. Endoscopic surgery versus medical treatment for spontaneous intracerebral hematoma: A randomized study. J. Neurosurg. 1989, 70, 530–535. [Google Scholar] [CrossRef]
- Hanley, D.F.; Thompson, R.E.; Muschelli, J.; Rosenblum, M.; McBee, N.; Lane, K.; Bistran-Hall, A.J.; Mayo, S.W.; Keyl, P.; Gandhi, D.; et al. Safety and efficacy of minimally invasive surgery plus alteplase in intracerebral haemorrhage evacuation (MISTIE): A randomised, controlled, open-label, phase 2 trial. Lancet Neurol. 2016, 15, 1228–1237. [Google Scholar] [CrossRef]
- de Oliveira Manoel, A.L. Surgery for spontaneous intracerebral hemorrhage. Crit. Care. 2020, 24, 45. [Google Scholar] [CrossRef]
- Morgan, T.; Zuccarello, M.; Narayan, R.; Keyl, P.; Lane, K.; Hanley, D. Preliminary findings of the minimally-invasive surgery plus rtpa for intracerebral hemorrhage evacuation (MISTIE) clinical trial. Acta Neurochir. Supp. 2008, 105, 147–151. [Google Scholar] [CrossRef]
- Carhuapoma, J.R.; Barrett, R.J.; Keyl, P.M.; Hanley, D.F.; Johnson, R.R. Stereotactic aspiration-thrombolysis of intracerebral hemorrhage and its impact on perihematoma brain edema. Neurocrit. Care. 2008, 8, 322–329. [Google Scholar] [CrossRef]
- Al-Shahi Salman, R.; Klijn, C.J.M.; Selim, M. Minimally invasive surgery plus alteplase for intracerebral haemorrhage. Lancet 2019, 393, 965–967. [Google Scholar] [CrossRef]
- Li, L.; Li, Z.; Li, Y.; Su, R.; Wang, B.; Gao, L.; Yang, Y.; Xu, F.; Zhang, X.; Tian, Q.; et al. Surgical evacuation of spontaneous cerebellar hemorrhage: Comparison of safety and efficacy of suboccipital craniotomy, stereotactic aspiration, and thrombolysis and endoscopic surgery. World Neurosurg. 2018, 117, e90–e98. [Google Scholar] [CrossRef]
- Shi, J.; Cai, Z.; Han, W.; Dong, B.; Mao, Y.; Cao, J.; Wang, S.; Guan, W. Stereotactic catheter drainage versus conventional craniotomy for severe spontaneous intracerebral hemorrhage in the basal ganglia. Cell Transplant. 2019, 28, 1025–1032. [Google Scholar] [CrossRef]
- Wang, J.-W.; Li, J.-P.; Song, Y.-L.; Tan, K.; Wang, Y.; Li, T.; Guo, P.; Li, X.; Wang, Y.; Zhao, Q.-H. Stereotactic aspiration versus craniotomy for primary intracerebral hemorrhage: A meta-analysis of randomized controlled trials. PLoS ONE 2014, 9, e107614. [Google Scholar] [CrossRef] [PubMed]
- Przybylowski, C.J.; Ding, D.; Starke, R.M.; Webster Crowley, R.; Liu, K.C. Endoport-assisted surgery for the management of spontaneous intracerebral hemorrhage. J. Clin. Neurosci. 2015, 22, 1727–1732. [Google Scholar] [CrossRef]
- Bauer, A.M.; Rasmussen, P.A.; Bain, M.D. Initial single-center technical experience with the brainpath system for acute intracerebral hemorrhage evacuation. Oper. Neurosurg. 2017, 13, 69–76. [Google Scholar] [CrossRef]
- Griessenauer, C.; Medin, C.; Goren, O.; Schirmer, C.M. Image-guided, minimally invasive evacuation of intracerebral hematoma: A matched cohort study comparing the endoscopic and tubular exoscopic systems. Cureus 2018, 10, e3569. [Google Scholar] [CrossRef]
- Labib, M.A.; Shah, M.; Kassam, A.B.; Young, R.; Zucker, L.; Maioriello, A.; Britz, G.; Agbi, C.; Day, J.D.; Gallia, G.; et al. The safety and feasibility of image-guided brainpath-mediated transsulcul hematoma evacuation: A multicenter study. Neurosurgery 2017, 80, 515–524. [Google Scholar] [CrossRef]
- Nagasaka, T.; Tsugeno, M.; Ikeda, H.; Okamoto, T.; Inao, S.; Wakabayashi, T. Early recovery and better evacuation rate in neuroendoscopic surgery for spontaneous intracerebral hemorrhage using a multifunctional cannula: Preliminary study in comparison with craniotomy. J. Stroke Cerebrovasc. Dis. 2011, 20, 208–213. [Google Scholar] [CrossRef]
- Xu, X.; Chen, X.; Li, F.; Zheng, X.; Wang, Q.; Sun, G.; Zhang, J.; Xu, B. Effectiveness of endoscopic surgery for supratentorial hypertensive intracerebral hemorrhage: A comparison with craniotomy. J. Neurosurg. 2018, 128, 553–559. [Google Scholar] [CrossRef]
- Wang, W.-H.; Hung, Y.-C.; Hsu, S.P.C.; Lin, C.-F.; Chen, H.-H.; Shih, Y.-H.; Lee, C.-C. Endoscopic hematoma evacuation in patients with spontaneous supratentorial intracerebral hemorrhage. J. Clin. Med. Assoc. 2015, 78. [Google Scholar] [CrossRef]
- Cai, Q.; Zhang, H.; Zhao, D.; Yang, Z.; Hu, K.; Wang, L.; Zhang, W.; Chen, Z.; Chen, Q. Analysis of three surgical treatments for spontaneous supratentorial intracerebral hemorrhage. Medicine 2017, 96, e8435. [Google Scholar] [CrossRef]
- Li, Y.; Yang, R.; Li, Z.; Yang, Y.; Tian, B.; Zhang, X.; Wang, B.; Lu, D.; Guo, S.; Man, M.; et al. Surgical evacuation of spontaneous supratentorial lobar intracerebral hemorrhage: Comparison of safety and efficacy of stereotactic aspiration, endoscopic surgery, and craniotomy. World Neurosurg. 2017, 105, 332–340. [Google Scholar] [CrossRef]
- Vespa, P.; Hanley, D.; Betz, J.; Hoffer, A.; Engh, J.; Carter, R.; Nakaji, P.; Ogilvy, C.; Jallo, J.; Selman, W.; et al. ICES (intraoperative stereotactic computed tomography-guided endoscopic surgery) for brain hemorrhage. Stroke 2016, 47, 2749–2755. [Google Scholar] [CrossRef]
- Ye, Z.; Ai, X.; Hu, X.; Fang, F.; You, C. Comparison of neuroendoscopic surgery and craniotomy for supratentorial hypertensive intracerebral hemorrhage: A meta-analysis. Medicine 2017, 96, e7876. [Google Scholar] [CrossRef] [PubMed]
- Nam, T.M.; Kim, Y.Z. A meta-analysis for evaluating efficacy of neuroendoscopic surgery versus craniotomy for supratentorial hypertensive intracerebral hemorrhage. J. Cerebrovasc. Endovasc. Neurosurg. 2019, 21, 11–17. [Google Scholar] [CrossRef]
- Rothrock, R.J.; Chartrain, A.G.; Scaggiante, J.; Pan, J.; Song, R.; Hom, D.; Lieber, A.C.; Bederson, J.B.; Mocco, J.; Kellner, C.P. Advanced techniques for endoscopic intracerebral hemorrhage evacuation: A technical report with case examples. Oper. Neurosurg. 2020. [Google Scholar] [CrossRef]
- Fiorella, D.; Arthur, A.; Schafer, S. Minimally invasive cone beam ct-guided evacuation of parenchymal and ventricular hemorrhage using the apollo system: Proof of concept in a cadaver model. J. Neurointerv. Surg. 2015, 7, 569–573. [Google Scholar] [CrossRef]
- Spiotta, A.M.; Fiorella, D.; Vargas, J.; Khalessi, A.; Hoit, D.; Arthur, A.; Lena, J.; Turk, A.S.; Chaudry, M.I.; Gutman, F.; et al. Initial multicenter technical experience with the apollo device for minimally invasive intracerebral hematoma evacuation. Neurosurgery 2015, 11, 243–251. [Google Scholar] [CrossRef]
- Turner, R.D.; Vargas, J.; Turk, A.S.; Chaudry, M.I.; Spiotta, A.M. Novel device and technique for minimally invasive intracerebral hematoma evacuation in the same setting of a ruptured intracranial aneurysm: Combined treatment in the neurointerventional angiography suite. Neurosurgery 2015, 11, 43–50. [Google Scholar] [CrossRef]
- Goyal, N.; Tsivgoulis, G.; Malhotra, K.; Katsanos, A.H.; Pandhi, A.; Alsherbini, K.A.; Chang, J.J.; Hoit, D.; Alexandrov, A.V.; Elijovich, L.; et al. Minimally invasive endoscopic hematoma evacuation vs best medical management for spontaneous basal-ganglia intracerebral hemorrhage. J. Neurointev. Surg. 2019, 11, 579–583. [Google Scholar] [CrossRef] [PubMed]
- Kellner, C.P.; Song, R.; Pan, J.; Nistal, D.A.; Scaggiante, J.; Chartrain, A.G.; Rumsey, J.; Hom, D.; Dangayach, N.; Swarup, R.; et al. Long-term functional outcome following minimally invasive endoscopic intracerebral hemorrhage evacuation. J. Neurointerv. Surg. 2020, 12, 489–494. [Google Scholar] [CrossRef]
- Zahuranec, D.B.; Lisabeth, L.D.; Sánchez, B.N.; Smith, M.A.; Brown, D.L.; Garcia, N.M.; Skolarus, L.E.; Meurer, W.J.; Burke, J.F.; Adelman, E.E.; et al. Intracerebral hemorrhage mortality is not changing despite declining incidence. Neurology 2014, 82, 2180–2186. [Google Scholar] [CrossRef]
| Study | Completed or Ongoing | Device | Dates of Enrollment | Locations | Number of Subjects | Results |
|---|---|---|---|---|---|---|
| Wang et al., 2009 [31] | Completed | Craniopuncture | January 2003–June 2004 | 42 centers in China | 195 Craniopuncture vs. 182 Conservative medical management | Mortality: 6.7% vs. 8.8% (p = 0.44) at 90 days Functional Status: significant improvement in 90-day Barthel Index (BI) (χ2 = 23.13, p = 0.0001) Rebleeding: 9.7% vs. 5.0%, p = 0.08 |
| Sun et al., 2010 [33] | Completed | Craniopuncture | January 2003–July 2005 | 22 centers in China | 159 Craniopuncture with urokinase infusion vs. 145 Craniotomy | Mortality: 14.5% vs. 25.0%, (p = 0.02) at 90 days Functional Status: no difference in 90-day BI (χ2 = 4.166, p = 0.38) Rebleeding: 8.8% vs. 21.4%, p = 0.002 |
| Zhou et al., 2011 [34] | Completed | Craniopuncture | 2005–2008 | China | 90 Craniopuncture vs. 78 Craniotomy | Mortality: 18.9% vs. 24.4% (p = 0.39) at 365 days Functional Status: BI = 79.5 vs. 62 (p = 0.01), at 365 days Rebleeding: 10.0% vs. 15.4%, p = 0.29 |
| Stereotactic treatment of intracerebral hematoma by means of a plasminogen activator (SICHPA) [38] | Completed | Stereotactic aspiration with thrombolytics | March 1996–May 1999 | 13 centers in the Netherlands | 36 Surgical vs. 35 Non-surgical | Mortality: 56% vs. 59% (p = 0.78) at 180 days Functional Status: no difference in likelihood of mRS >4 (OR = 0.52, p = 0.38) Rebleeding: 0% vs. 22%, p = 0.006 |
| Minimally Invasive Surgery Plus Rt-PA for ICH Evacuation Phase III (MISTIE III) [39] | Completed | Stereotactic aspiration with thrombolytics | December 2013–August 2017 | 84 centers Australia, Canada, China, Germany, Hungary, Israel, Spain, UK, USA | 255 MISTIE vs. 251 Standard medical care | Mortality: 19% vs. 26% (p = 0.04), at 365 days Functional Status: no difference in mRS <4 at 365 days (45% vs. 41%, = 0.33) Rebleeding: 2% vs. 1%, p = 0.32 |
| Early Minimally-Invasive Removal of Intracerebral Hemorrhage (ENRICH) | Ongoing | Endoport | December 2016–December 2021 | 36 centers in USA | Expected enrollment: 300 | n/a—study ongoing |
| Auer et al. 1989 [40] | Completed | Endoscope | June 1983–August 1986 | Austria | 50 Endoscopic evacuation vs. 50 Medical management | Mortality: 42% vs. 70% (p < 0.01) at 180 days Functional Status: significant difference in “minimal neurologic deficit” at 180 days (40% vs. 25%, p < 0.05) Rebleeding: 4% vs. 30%, p < 0.05 |
| Intraoperative Stereotactic Computed Tomography-Guided Endoscopic Surgery (ICES) [41] | Completed | Endoscope | August 2005–August 2012 | 29 centers in Canada, Germany, USA, UK | 14 Surgical vs. 4 Medical | Mortality: 0% vs. 7.1% (p = 0.68) Functional Status: no difference in mRS <4 at 180 days (42% vs. 24%, p = 0.19) Rebleeding: no rebleeding in either group |
| Minimally Invasive Endoscopic Surgery with Apollo in Patients with Brain Hemorrhage (INVEST) | Ongoing | Apollo | June 2017–June 2021 | 7 centers in USA | Estimated enrollment: 50 | n/a—study ongoing |
| Artemis in the Removal of Intracerebral Hemorrhage (MIND) | Ongoing | Artemis | February 2018–July 2024 | 20 locations in Germany and USA | Estimated enrollment: 500 | n/a—study ongoing |
| Dutch Intracerebral Hemorrhage Surgery Trial (DIST) | Ongoing | Artemis | November 2018–present | 10 centers in the Netherlands | Estimated enrollment: 400 | n/a—study ongoing |
| Minimally Invasive Intracerebral Hemorrhage Evacuation (MIRROR) | Ongoing | Surgiscope | October 2020–October 2028 | 2 centers in USA | Estimated enrollment: 500 | n/a—study ongoing |
| Ultra-Early, Minimally Invasive Intracerebral Hemorrhage Evacuation Versus Standard Treatment (EVACUATE) | Ongoing | Surgiscope | September 2020–December 2025 | 2 centers in Australia | Estimated enrollment: 240 | n/a—study ongoing |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hannah, T.C.; Kellner, R.; Kellner, C.P. Minimally Invasive Intracerebral Hemorrhage Evacuation Techniques: A Review. Diagnostics 2021, 11, 576. https://doi.org/10.3390/diagnostics11030576
Hannah TC, Kellner R, Kellner CP. Minimally Invasive Intracerebral Hemorrhage Evacuation Techniques: A Review. Diagnostics. 2021; 11(3):576. https://doi.org/10.3390/diagnostics11030576
Chicago/Turabian StyleHannah, Theodore C., Rebecca Kellner, and Christopher P. Kellner. 2021. "Minimally Invasive Intracerebral Hemorrhage Evacuation Techniques: A Review" Diagnostics 11, no. 3: 576. https://doi.org/10.3390/diagnostics11030576
APA StyleHannah, T. C., Kellner, R., & Kellner, C. P. (2021). Minimally Invasive Intracerebral Hemorrhage Evacuation Techniques: A Review. Diagnostics, 11(3), 576. https://doi.org/10.3390/diagnostics11030576






