Optical Devices in Tracheal Intubation—State of the Art in 2020
Abstract
1. Introduction
2. The Purpose of the Review
3. Methodology
4. Supraglottic Airway Devices and Optical Intubation
Clinical Evidence
5. Hybrid Devices
Clinical Evidence
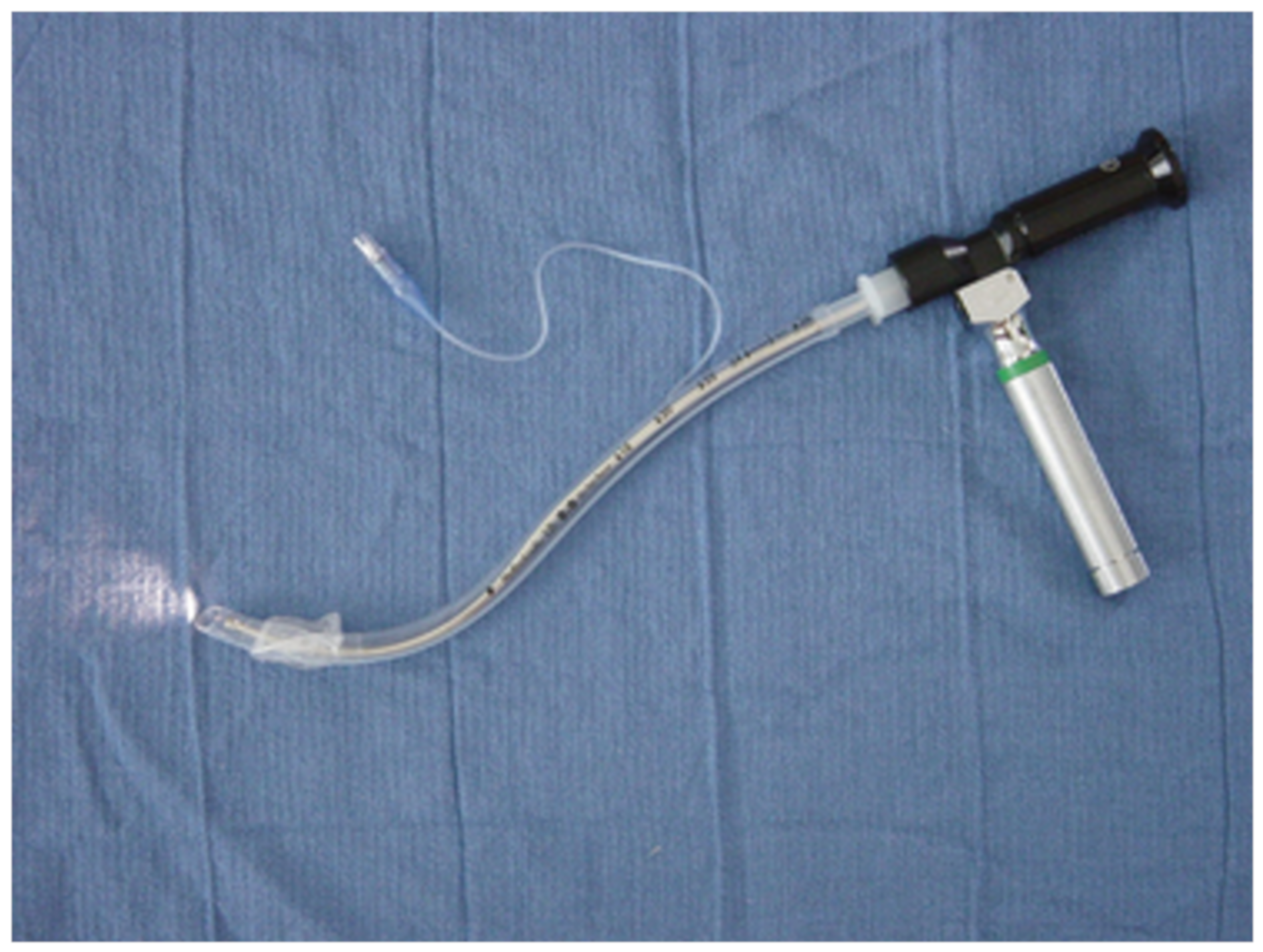
6. Optical Stylets
Clinical Evidence
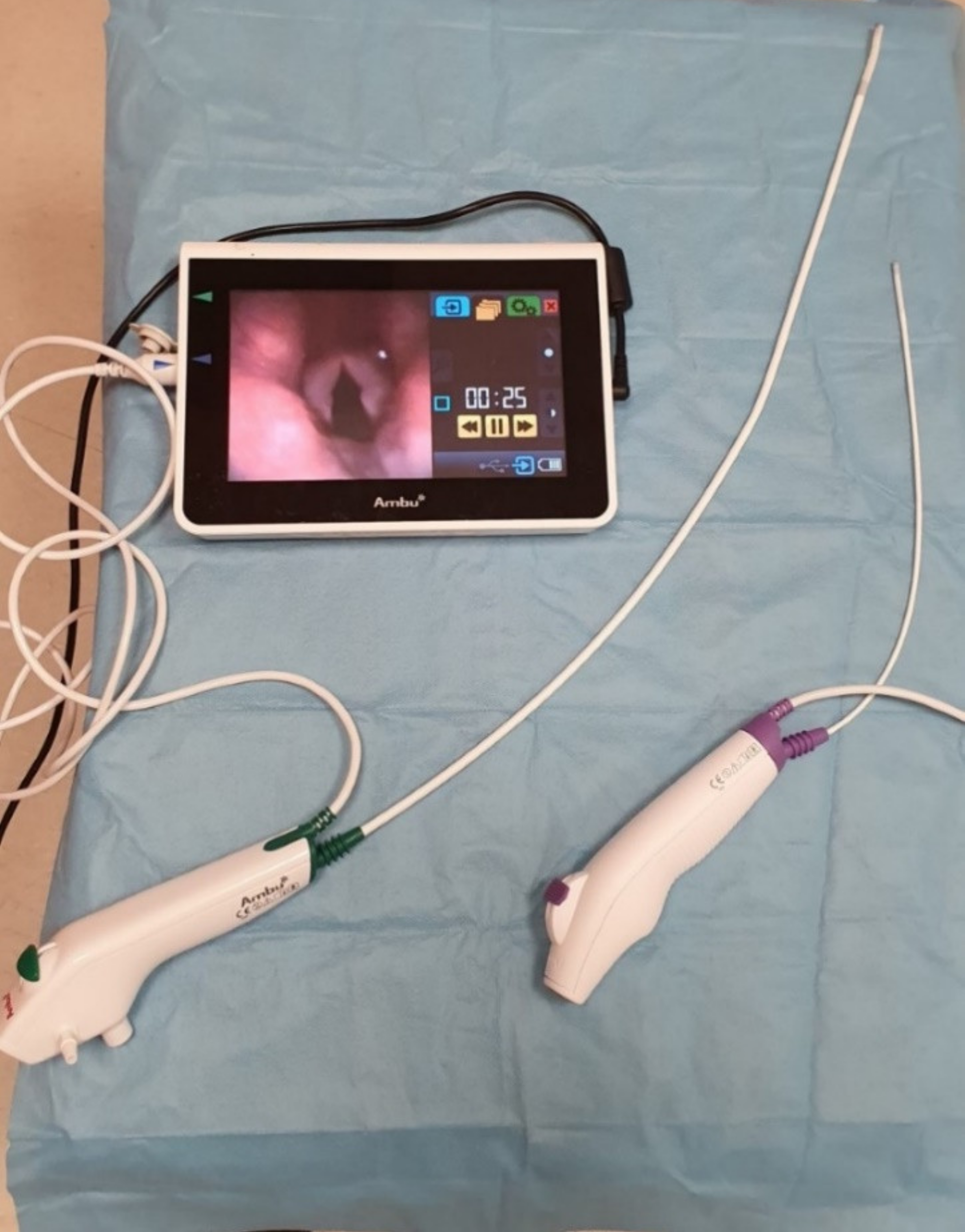
7. Flexible Fiberoptic Intubation
Clinical Evidence
8. Fiberoptic Tracheal Tubes
Clinical Evidence
9. Limitations
10. Directions for the Future Research
11. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Records Identified through Database Search | Records after Duplicates Removed | Records Excluded | Records Included | |||||
|---|---|---|---|---|---|---|---|---|
| Supraglottic airway devices | PubMed | 200 | ||||||
| Scopus | 95 | |||||||
| Web of Science | 63 | Not relevant | 122 | |||||
| Other sources | 10 | Other reasons | 108 | |||||
| Total | 368 | Total | 248 | Total | 230 | Total | 18 | |
| Hybrid devices | PubMed | 76 | ||||||
| Scopus | 120 | |||||||
| Web of Science | 99 | Not relevant | 47 | |||||
| Other sources | 0 | Other reasons | 73 | |||||
| Total | 295 | Total | 139 | Total | 120 | Total | 19 | |
| Optical stylets | PubMed | 114 | ||||||
| Scopus | 109 | |||||||
| Web of Science | 73 | Not relevant | 25 | |||||
| Other sources | 30 | Other reasons | 142 | |||||
| Total | 326 | Total | 212 | Total | 167 | Total | 45 | |
| Single-use fibrescopes | PubMed | 25 | ||||||
| Scopus | 48 | |||||||
| Web of Science | 31 | Not relevant | 15 | |||||
| Other sources | 6 | Other reasons | 35 | |||||
| Total | 110 | Total | 63 | Total | 50 | Total | 13 | |
| Fiberoptic tracheal tubes | PubMed | 33 | ||||||
| Scopus | 23 | |||||||
| Web of Science | 45 | Not relevant | 12 | |||||
| Other sources | 2 | Other reasons | 31 | |||||
| Total | 102 | Total | 56 | Total | 43 | Total | 13 | |

References
- Pahor, A.L. Ear, nose, and throat in Ancient Egypt. J. Laryngol. Otol. 1992, 106, 773–779. [Google Scholar] [CrossRef] [PubMed]
- Szmuk, P.; Ezri, T.; Evron, S.; Roth, Y.; Katz, J. A brief history of tracheostomy and tracheal intubation, from the Bronze Age to the Space Age. Intensiv. Care Med. 2008, 34, 222–228. [Google Scholar] [CrossRef]
- Garcia, M. Observation on the human voice. Laryngoscope 1905, 15, 185–194. [Google Scholar] [CrossRef]
- Rogers, J. Postdiphtheritic stenosis of the larynx (retained intubation instruments and retained tracheal canulae). Ann. Surg. 1900, 31, 547–571. [Google Scholar] [CrossRef] [PubMed]
- Wong, D.T.; Yang, J.J.; Mak, H.Y.; Jagannathan, N. Use of intubation introducers through a supraglottic airway to facilitate tracheal intubation: A brief review. Can. J. Anaesth. 2012, 59, 704–715. [Google Scholar] [CrossRef]
- Collins, S.R.; Blank, R.S. Fiberoptic intubation: An overview and update. Respir. Care 2014, 59, 865–880. [Google Scholar] [CrossRef]
- Liem, E.B.; Bjoraker, D.G.; Gravenstein, D. New options for airway management: Intubating fibreoptic stylets. Br. J. Anaesth. 2003, 91, 408–418. [Google Scholar] [CrossRef] [PubMed]
- Brain, A.I. The laryngeal mask--a new concept in airway management. Br. J. Anaesth. 1983, 55, 801–805. [Google Scholar] [CrossRef] [PubMed]
- Apfelbaum, J.L.; Hagberg, C.A.; Caplan, R.A.; Blitt, C.D.; Connis, R.T.; Nickinovich, D.G. Practice guidelines for the management of the difficult airway: An updated report by the American Society of Anesthesiologists Task Force on the Management of the Difficult Airway. Anesthesiology 2013, 118, 251–270. [Google Scholar] [CrossRef] [PubMed]
- Frerk, C.; Mitchell, V.S.; McNarry, A.F.; Mendonca, C.; Bhagrath, R.; Patel, A.; O’Sullivan, E.P.; Woodall, N.M.; Ahmad, I. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br. J. Anaesth. 2015, 115, 827–848. [Google Scholar] [CrossRef] [PubMed]
- Michalek, P.; Donaldson, W. The use of an i-gel supraglottic airway for the airway management of a patient with subglottic stenosis: A case report. Minerva Anestesiol. 2010, 76, 369–372. [Google Scholar]
- McAleavey, F.; Michalek, P. Aura-i laryngeal mask as a conduit for elective fibreoptic intubation. Anaesthesia 2010, 65, 1151. [Google Scholar] [CrossRef]
- Ferson, D.Z.; Rosenblatt, W.H.; Johansen, M.J.; Osborn, I.; Ovassapian, A. Use of the intubating LMA-Fastrach in 254 patients with difficult-to-manage airways. Anesthesiology 2001, 95, 1175–1181. [Google Scholar] [CrossRef] [PubMed]
- Gerstein, N.S.; Braude, D.A.; Hung, O.; Sanders, J.C.; Murphy, M.F. The Fastrach™ Intubating Laryngeal Mask Airway®: An overview and update. Can. J. Anesth. 2010, 57, 588–601. [Google Scholar] [CrossRef] [PubMed]
- Joffe, A.M.; Liew, E.C.; Galgon, R.E.; Viernes, D.; Tregglari, M.M. The second-generation Air-Q intubating laryngeal mask for airway maintenance during anaesthesia in adults: A report of the first 70 uses. Anaesth. Intensiv. Care 2011, 39, 40–45. [Google Scholar] [CrossRef]
- Jagannathan, N.; Sohn, L.; Ramsey, M.; Huang, A.; Sawardekar, A.; Sequera-Ramos, L.; Kromrey, L.; De Oliveira, G.S. A randomized comparison between the i-gel and the Air-Q supraglottic airways when used by anesthesiology trainees as conduits for tracheal intubation in children. Can. J. Anaesth. 2015, 62, 587–594. [Google Scholar] [CrossRef]
- Jagannathan, N.; Sohn, L.E.; Sawardekar, A.; Gordon, J.; Shah, R.D.; Mukherji, I.I.; Roth, A.G.; Suresh, S. A randomized trial comparing the Ambu Aura-i with the Air-Q intubating laryngeal airway as conduits for tracheal intubation in children. Paediatr. Anaesth. 2012, 22, 1197–1204. [Google Scholar] [CrossRef]
- Donaldson, W.; Abraham, A.; Deighan, M.; Michalek, P. i-gel™ vs. AuraOnce™ laryngeal mask for general anaesthesia with controlled ventilation in paralyzed patients. Biomed. Pap. 2011, 55, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Kleine-Brueggeney, M.; Theiler, L.; Urwyler, N.; Vogt, A.; Greif, R. Randomized trial comparing the i-gel and Magill tracheal tube with the single-use ILMA™ and ILMA™ tracheal tube for fibreoptic-guided intubation in anaesthetized patients with a predicted difficult airway. Br. J. Anaesth. 2011, 107, 251–257. [Google Scholar] [CrossRef]
- Mendonca, C.; Tourville, C.C.; Jefferson, H.; Nowicka, A.; Patteril, M.; Athanassoglou, V. Fibreoptic-guided tracheal intubation through i-gel® and LMA® Protector™ supraglottic airway devices—A randomised comparison. Anaesthesia 2019, 74, 203–210. [Google Scholar] [CrossRef]
- Gasteiger, L.; Oswald, E.; Keplinger, M.; Putzer, G.; Luger, M.; Neururer, S.; Keller, C.; Moser, B. A randomized trial comparing the Ambu Aura-i™and the Ambu Aura Gain™ laryngeal mask as conduit for tracheal intubation in children. Minerva Anestesiol. 2020, 86, 1143–1150. [Google Scholar] [CrossRef] [PubMed]
- Moser, B.; Keller, C.; Audigé, L.; Dave, M.H.; Bruppacher, H.R. Fiberoptic intubation of severely obese patients through supraglottic airway: A prospective, randomized trial of the Ambu AuraGain™ laryngeal mask vs. the i-gel™ airway. Acta Anaesthesiol. Scand. 2019, 63, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Preece, G.; Ng, I.; Lee, K.; Mezzavia, P.; Krieser, R.; Williams, D.L.; Stewart, O.; Segal, R. A randomised controlled trial comparing fibreoptic-guided tracheal intubation through two supraglottic devices: Ambu AuraGain laryngeal mask and LMA Fastrach™. Anaesth. Intensiv. Care 2018, 46, 474–479. [Google Scholar] [CrossRef]
- Metterlein, T.; Dintenfelder, A.; Plank, C.; Graf, B.; Roth, G. A comparison of various supraglottic airway devices for fiberoptical guided tracheal intubation. Braz. J. Anesthesiol. 2017, 67, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Bergold, M.N.; Kahle, S.; Schultzik, T.; Bücheler, T.; Byhahn, C. Intubating laryngeal tube suction disposable: Initial clinical experiences with a novel device for endotracheal intubation. Anaesthetist 2016, 65, 30–35. (In German) [Google Scholar] [CrossRef] [PubMed]
- Liu, E.H.; Goy, R.W.; Chen, F.G. The LMA CTrach™, a new laryngeal mask airway for endotracheal intubation under vision: Evaluation in 100 patients. Br. J. Anaesth. 2006, 96, 396–400. [Google Scholar] [CrossRef]
- Timmermann, A.; Russo, S.; Graf, B.M. Evaluation of the CTrach—An intubating LMA with integrated fiberoptic system. Br. J. Anaesth. 2006, 96, 516–521. [Google Scholar] [CrossRef]
- Liu, E.H.; Wender, R.; Goldman, A.J. The LMA CTrach in patients with difficult airways. Anesthesiology 2009, 110, 941–943. [Google Scholar] [CrossRef] [PubMed]
- Ojeda, A.; López, A.M.; Borrat, X.; Valero, R. Failed tracheal intubation with the LMA-CTrach in two patients with lingual tonsil hyperplasia. Anesth. Analg. 2008, 107, 601–602. [Google Scholar] [CrossRef] [PubMed]
- Abdi, W.; Ndoko, S.; Amathieu, R.; Dhonneur, G. Evidence of pulmonary aspiration during difficult airway management of a morbidly obese patient with the LMA CTrach. Br. J. Anaesth. 2008, 100, 275–277. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gómez-Ríos, M.Á.; Freire-Vila, E.; Vízcaíno-Martínez, L.; Estévez-González, E. The Totaltrack: An initial evaluation. Br. J. Anaesth. 2015, 115, 799–800. [Google Scholar] [CrossRef]
- Liu, E.H.; Goy, R.W.; Lim, Y.; Chen, F.G. Success of tracheal intubation with intubating laryngeal mask airways: A randomized trial of the LMA Fastrach and LMA CTrach. Anesthesiology 2008, 108, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Mathew, D.G.; Ramachandran, R.; Rewari, V.; Trikha, A. Endotracheal intubation with intubating laryngeal mask airway (ILMA), C-Trach, and Cobra PLA in simulated cervical spine injury patients: A comparative study. J. Anesth. 2014, 28, 655–661. [Google Scholar] [CrossRef]
- Arslan, Z.I.; Yildiz, T.; Baykara, Z.N.; Solak, M.; Toker, K. Tracheal intubation in patients with rigid collar immobilisation of the cervical spine: A comparison of Airtraq and LMA CTrach devices. Anaesthesia 2009, 64, 1332–1336. [Google Scholar] [CrossRef]
- Ng, S.Y.; Ithnin, E.; Lim, Y. Comparison of airway management during anaesthesia using the laryngeal mask airway CTrach and Glidescope. Anaesth. Intensiv. Care 2007, 35, 736–742. [Google Scholar] [CrossRef] [PubMed]
- Arslan, Z.I.; Ozdamar, D.; Yildiz, T.S.; Solak, Z.M.; Toker, K. Tracheal intubation in morbidly obese patients: A comparison of the Intubating Laryngeal Mask Airway™ and Laryngeal Mask Airway CTrach™. Anaesthesia 2012, 67, 261–265. [Google Scholar] [CrossRef]
- Yildiz, T.S.; Ozdamar, D.; Arslan, I.; Solak, M.; Toker, K. The LMA CTrach™ in morbidly obese and lean patients undergoing gynecological procedures: A comparative study. J. Anesth. 2010, 24, 849–853. [Google Scholar] [CrossRef] [PubMed]
- Dhonneur, G.; Ndoko, S.K.; Yavchitz, A.; Foucrier, A.; Fessenmeyer, C.; Pollian, C.; Combes, X.; Tual, L. Tracheal intubation of morbidly obese patients: LMA CTrach vs. direct laryngoscopy. Br. J. Anaesth. 2006, 97, 742–745. [Google Scholar] [CrossRef]
- Mihai, R.; Blair, E.; Kay, H.; Cook, T.M. A quantitative review and meta-analysis of performance of non-standard laryngoscopes and rigid fibreoptic intubation aids. Anaesthesia 2008, 63, 745–760. [Google Scholar] [CrossRef]
- Choonoo, J.O.; Hofmeyr, R.; Evans, N.R.; James, M.F.; Meyersfeld, M.R. A new option in airway management: Evaluation of the TotalTrack video laryngeal mask. S. Afr. J. Anaesth. Analg. 2016, 22, 52–56. [Google Scholar] [CrossRef][Green Version]
- Gaszynski, T. TotalTrack video intubating laryngeal mask in super-obese patients—Series of cases. Ther. Clin. Risk Manag. 2016, 12, 335–338. [Google Scholar] [CrossRef]
- Gómez-Ríos, M.A.; Casans-Francés, R.; Freire-Vila, E.; Sastre, J.A.; López, T.; Garzón, J.C. A prospective evaluation of the Totaltrack video laryngeal mask in paralyzed, anesthetized obese patients. J. Clin. Anesth. 2020, 61, 109688. [Google Scholar] [CrossRef]
- Gómez-Ríos, M.Á.; Freire-Vila, E.; Calvo-Vecino, J.M. Use of the Totaltrack VLM as a rescue device following failed tracheal intubation. Eur. J. Anaesthesiol. 2019, 36, 237–239. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Ríos, M.A.; Freire-Vila, E.; Casans-Francés, R.; Pita-Fernández, S. The Totaltrack video laryngeal mask: An evaluation in 300 patients. Anaesthesia 2019, 74, 751–757. [Google Scholar] [CrossRef]
- Hurford, B.E. The video revolution: A new view of laryngoscopy. Respir. Care 2010, 55, 1036–1045. [Google Scholar]
- Berci, G.; Katz, R. Optical stylet: An aid to intubation and teaching. Ann. Otol. Rhinol. Laryngol. 1979, 88, 828–831. [Google Scholar] [CrossRef] [PubMed]
- Katz, R.L.; Berci, G. The optical stylet—A new intubation technique for adults and children with specific reference to teaching. Anesthesiology 1979, 51, 251–254. [Google Scholar] [PubMed]
- Bonfils, P. Difficult intubation in Pierre-Robin children, a new method: The retromolar route. Anaesthetist 1983, 32, 363–367. (In German) [Google Scholar]
- Shikani, A.H. New “seeing” stylet-scope and method for the management of the difficult airway. Otolaryngol. Head Neck Surg. 1999, 120, 113–116. [Google Scholar] [CrossRef]
- Levitan, R.M. Design rationale and intended use of a short optical stylet for routine fiberoptic augmentation of emergency laryngoscopy. Am. J. Emerg. Med. 2006, 24, 490–495. [Google Scholar] [CrossRef] [PubMed]
- Biro, P.; Battig, U.; Henderson, J.; Seifert, B. First clinical experience of tracheal intubation with the SensaScope, a novel steerable semirigid video stylet. Br. J. Anaesth. 2006, 97, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Biro, P. The SensaScope—A new hybrid video intubation stylet. Saudi J. Anaesth. 2011, 5, 411–413. [Google Scholar] [CrossRef]
- Hagberg, C.A. Current concepts in the management of the difficult airway. Anesthesiol. News 2019, 16, 1–32. [Google Scholar] [CrossRef][Green Version]
- Ong, J.; Lee, C.L.; Lai, H.Y.; Lee, Y.; Chen, T.Y.; Shyr, M.H. A new video intubating device: Trachway intubating stylet. Anaesthesia 2009, 64, 1145. [Google Scholar] [CrossRef] [PubMed]
- Pius, J.; Ioanidis, K.; Noppens, R.R. Use of the novel C-MAC video stylet in a case of predicted difficult intubation: A case report. A A Pract. 2019, 13, 88–90. [Google Scholar] [CrossRef]
- Xue, F.S.; Yang, B.Q.; Liu, Y.Y.; Li, H.X.; Yang, G.Z. Current evidences for the use of UEscope in airway management. Chin. Med. J. 2017, 130, 1867–1875. [Google Scholar] [CrossRef]
- Lee, J.Y.; Hur, H.J.; Park, H.Y.; Jung, W.S.; Kim, J.; Kwak, H.J. Comparison between video-lighted stylet (Intular Scope™) and direct laryngoscope for endotracheal intubation in patients with normal airway. J. Int. Med. Res. 2020, 48, 300060520969532. [Google Scholar] [CrossRef]
- Nowakowski, M.; Williams, S.; Gallant, J.; Ruel, M.; Robitaille, A. Predictors of difficult intubation with the Bonfils rigid fiberscope. Anesth. Analg. 2016, 122, 1901–1906. [Google Scholar] [CrossRef] [PubMed]
- Bein, B.; Worthmann, F.; Scholz, J.; Brinkmann, F.; Tonner, P.H.; Steinfath, M.; Dőrges, V. A comparison of the intubating laryngeal mask airway and the Bonfils intubation fibrescope in patients with predicted difficult airways. Anaesthesia 2004, 59, 668–674. [Google Scholar] [CrossRef]
- Faalcetta, S.; Pecora, L.; Orsetti, G.; Gentili, P.; Rossi, A.; Gabbanelli, V.; Adrario, E.; Donati, A.; Pelaia, P. The Bonfils fiberscope: A clinical evaluation of its learning curve and efficacy in difficult airway management. Minerva Anestesiol. 2012, 78, 176–184. [Google Scholar]
- Wahlen, B.M.; Gercek, E. Three-dimensional cervical spine movement during intubation using the Macintosh and Bullard laryngoscopes, the bonfils fiberscope, and the intubating laryngeal mask airway. Eur. J. Anaesthesiol. 2004, 21, 907–913. [Google Scholar] [CrossRef] [PubMed]
- Rudolph, C.; Schneider, J.P.; Wallenborn, J.; Schaffranietz, L. Movement of the upper cervical spine during laryngoscopy: A comparison of the Bonfils intubation fibrescope and the Macintosh laryngoscope. Anaesthesia 2005, 60, 668–672. [Google Scholar] [CrossRef] [PubMed]
- Corbanese, U.; Possamai, C. Awake intubation with the Bonfils fibrescope in patients with difficult airway. Eur. J. Anaesthesiol. 2009, 26, 837–841. [Google Scholar] [CrossRef] [PubMed]
- Mazeres, J.E.; Lefranc, A.; Cropet, C.; Steghens, A.; Bachmann, P.; Pérol, O.; Rosay, H. Evaluation of the Bonfils intubating fibrescope for predicted difficult intubation in awake patients with ear, nose and throat cancer. Eur. J. Anaesthesiol. 2011, 28, 646–650. [Google Scholar] [CrossRef]
- Nassar, M.; Zanaty, O.M.; Ibrahim, M. Bonfils fiberscope vs. GlideScope for awake intubation in morbidly obese patients with expected difficult airways. J. Clin. Anesth. 2016, 32, 101–105. [Google Scholar] [CrossRef] [PubMed]
- Kaufmann, J.; Laschat, M.; Engelhardt, T.; Hellmich, M.; Wappler, F. Tracheal intubation with the Bonfils fiberscope in the difficult paediatric airway: A comparison with fiberoptic intubation. Paediatr. Anaesth. 2015, 25, 372–378. [Google Scholar] [CrossRef]
- Kaufmann, J.; Laschat, M.; Hellmich, M.; Wappler, F. A randomised controlled comparison of the Bonfils fiberscope and the GlideScope Cobalt AVL video laryngoscope for visualization of the larynx and intubation of the trachea in infants and small children with normal airways. Paediatr. Anaesth. 2013, 23, 913–919. [Google Scholar] [CrossRef]
- Pfitzner, L.; Cooper, M.G.; Ho, D. The Shikani seeing styletTM for difficult intubation in children: Initial experience. Anaesth. Intensiv. Care 2002, 30, 462–466. [Google Scholar] [CrossRef] [PubMed]
- Turkstra, T.P.; Pelz, D.M.; Shaikh, A.A.; Craen, R.A. Cervical spine motion: A fluoroscopic comparison of Shikani Optical Stylet vs. Macintosh laryngoscope. Can. J. Anaesth. 2007, 54, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Xu, M.; Li, X.X.; Guo, X.Y.; Wang, J. Shikani optical stylet versus Macintosh laryngoscope for intubation in patients undergoing surgery for cervical spondylosis: A randomized controlled trial. Chin. Med. J. 2017, 130, 297–302. [Google Scholar] [CrossRef]
- Mahrous, R.S.; Ahmed, A.M. The Shikani Optical Stylet as an alternative to awake fiberoptic intubation in patients at risk of secondary cervical spine injury: A randomized controlled trial. J. Neurosurg. Anesthesiol. 2018, 30, 354–358. [Google Scholar] [CrossRef]
- Phua, D.S.; Mah, C.L.; Wang, C.F. The Shikani optical stylet as an alternative to the GlideScope videolaryngoscope in simulated difficult intubations—A randomized controlled trial. Anaesthesia 2012, 67, 402–406. [Google Scholar] [CrossRef] [PubMed]
- Sangwan, Y.S.; Palomino, J.; Simeone, F.; Koveleskie, J. Critical airway management. A suggested modification to the rigid fiber-optic stylet based on 301 novice intubations. J. Bronchol. Interv. Pulmonol. 2012, 19, 349–357. [Google Scholar] [CrossRef]
- Liu, X.; Zhang, Y.; Liu, Z.; Zhang, Q.; Wu, W.; Zheng, Z.; Zhang, Z. Application of second-generation Shikani optical stylet in critically ill patients undergoing cerebral aneurysm embolization. J. Int. Med. Res. 2019, 47, 1565–1572. [Google Scholar] [CrossRef]
- Cheng, T.; Wang, L.-K.; Wu, H.-Y.; Yang, X.-D.; Zhang, X.; Jiao, L. Shikani optical stylet for awake nasal intubation in patients undergoing head and neck surgery. Laryngoscope 2020. [Google Scholar] [CrossRef] [PubMed]
- Aziz, M.; Metz, S. Clinical evaluation of the Levitan Optical Stylet. Anaesthesia 2011, 66, 579–581. [Google Scholar] [CrossRef] [PubMed]
- Webb, A.; Kolawole, H.; Leong, S.; Loughnan, T.E.; Crofts, T.; Bowden, C. Comparison of the Bonfils and Levitan optical stylets for tracheal intubation: A clinical study. Anaesth. Intensiv. Care 2011, 39, 1093–1097. [Google Scholar] [CrossRef]
- Gaszynski, T.; Pietrzyk, M.; Szewczyk, T.; Gaszynska, E. A comparison of performance of endotracheal intubation using the Levitan FPS Optical Stylet or Lary-Flex videolaryngoscope in morbidly obese patients. Sci. World J. 2014, 2014, 207591. [Google Scholar] [CrossRef]
- Greif, R.; Kleine-Brueggeney, M.; Theiler, L. Awake tracheal intubation using the Sensascope in 13 patients with an anticipated difficult airway. Anaesthesia 2010, 65, 525–528. [Google Scholar] [CrossRef]
- Kleine-Brueggeney, M.; Greig, R.; Urwyler, N.; Wirthmüller, B.; Theiler, L. The performance of rigid scopes for tracheal intubation: A randomized, controlled trial in patients with a simulated difficult airway. Anaesthesia 2016, 71, 1456–1463. [Google Scholar] [CrossRef] [PubMed]
- Kriege, M.; Alflen, C.; Strauss, H.; Ott, T.; Noppens, R.R. Usage of a semi-rigid intubation endoscope is not superior to a videolaryngoscope. A prospective, randomized, controlled trial comparing the SensaScope vs. the McGrath Series 5 in surgical patients. Trends Anaesth. Crit. Care 2018, 18, 23–28. [Google Scholar] [CrossRef]
- Cheng, W.C.; Lan, C.H.; Lai, H.Y. The Clarus video system (Trachway) intubating stylet for awake intubation. Anaesthesia 2011, 66, 1178–1180. [Google Scholar] [CrossRef] [PubMed]
- Hsu, H.T.; Chou, S.H.; Chen, C.L.; Tseng, K.Y.; Kuo, Y.W.; Chen, M.K.; Cheng, K.I. Left endobronchial intubation with a double-lumen tube using direct laryngoscopy or the Trachway video stylet. Anaesthesia 2013, 68, 851–855. [Google Scholar] [CrossRef] [PubMed]
- Chan, W.-H.; Cheng, C.-P.; Chiu, Y.-L.; Hsu, Y.-C.; Hu, M.-H.; Huang, G.-S. Two head positions for orotracheal intubation with the trachway videolight intubating stylet wit manual in-line stabilization: A randomized controlled trial. Medicine 2020, 99, e19645. [Google Scholar] [CrossRef]
- Lin, Y.C.; Cho, A.H.; Lin, J.R.; Chung, Y.T. The Clarus video system (Trachway) and direct laryngoscope for endotracheal intubation with cricoid pressure in simulated rapid sequence induction intubation: A prospective randomized controlled trial. BMC Anesthesiol. 2019, 19, 33. [Google Scholar] [CrossRef]
- Lee, M.C.; Tseng, K.Y.; Shen, Y.C.; Lin, C.H.; Hsu, C.W.; Hsu, H.J.; Lu, I.C.; Cheng, K.I. Nasotracheal intubation in patients with limited mouth opening: A comparison between fibreoptic intubation and the Trachway. Anaesthesia 2016, 71, 31–38. [Google Scholar] [CrossRef]
- Ezhar, Y.; D’Aragon, F.; Echave, P. Hemodynamic responses to tracheal intubation with Bonfils compared to C-MAC videolaryngoscope: A randomized trial. BMC Anesthesiol. 2018, 18, 124. [Google Scholar] [CrossRef]
- Ahmad, I.; El-Boghadly, K.; Bhagrath, R.; Hodzovic, I.; McNarry, A.F.; Mir, F.; O’Sullivan, E.P.; Patel, A.; Stacey, M.; Vaughan, D. Difficult Airway Society guidelines for awake tracheal intubation (ATI) in adults. Anaesthesia 2020, 75, 509–528. [Google Scholar] [CrossRef]
- Murphy, P. A fibre-optic endoscope used for nasal intubation. Anaesthesia 1967, 22, 489–491. [Google Scholar] [CrossRef]
- Pritchett, M.A.; Oberg, C.L.; Belanger, A.; De Cardenas, J.; Cheng, G.; Cumbo Nachelli, G.; Franco-Paredes, C.; Singh, J.; Toth, J.; Zgoda, M.; et al. Society for Advanced Bronchoscopy Consensus Statement and Guidelines for bronchoscopy and airway management amid the Covid-19 pandemic. J. Thorac. Dis. 2020, 12, 1781–1798. [Google Scholar] [CrossRef]
- Luo, F.; Darwiche, K.; Singh, S.; Torrego, A.; Steinfort, D.P.; Gasparini, S.; Liu, D.; Zhang, W.; Fernandez-Bussy, S.; Herth, F.J.; et al. Performing bronchoscopy in times of the Covid-19 pandemic: Practice statement from an international expert panel. Respiration 2020, 99, 417–422. [Google Scholar] [CrossRef]
- Orser, B.A. Recommendations for endotracheal intubation of Covid-19 patients. Anesth. Analg. 2020, 130, 1109–1110. [Google Scholar] [CrossRef] [PubMed]
- Cook, T.M.; El-Boghdadly, K.; McGuire, B.; McNarry, A.F.; Patel, A.; Higgs, A. Consensus guidelines for managing the airway in patients with COVID-19: Guidelines from Difficult Airway Society, the Association of Anaesthetists the Intensive Care Society, the Faculty of Intensive Care Medicine and the Royal College of Anaesthetists. Anaesthesia 2020, 75, 785–799. [Google Scholar] [CrossRef] [PubMed]
- Sorbello, M.; Di Giacinto, I.; Corso, R.M.; Cataldo, R. Prevention is better than the cure, but the cure cannot be worse than the disease: Fibreoptic tracheal intubation in COVID-19 patients. Br. J. Anaesth. 2020, 125, e187–e188. [Google Scholar] [CrossRef]
- Emery, A.R.; Saniukovich, O.; Lu Lang, A.; Tannyhil, R.J., III; Wang, J. A novel approach to fiberoptic intubation in patients with coronavirus disease 2019. J. Oral Maxillofac. Surg. 2020, 78, 2182.e1–2182.e6. [Google Scholar] [CrossRef] [PubMed]
- Kriege, M.; Dalberg, J.; McGrath, B.A.; Shimabukuro-Vornhagen, A.; Billgren, B.; Lund, T.K.; Thornberg, K.; Christophersen, A.V.; Dunn, M.J. Evaluation of intubation and intensive care use of the new Ambu aScope™ 4 broncho and Ambu aView™ compared to a customary flexible endoscope: A multicentre prospective, non-interventional study. Trends Anaesth. Crit. Care 2020, 31, 35–41. [Google Scholar] [CrossRef]
- Krugel, V.; Bathory, I.; Frascarolo, P.; Schoettker, P. Comparison of the single-use Ambu aScope™ 2 vs. the conventional fibrescope for tracheal intubation in patients with cervical spine immobilisation by a semirigid collar. Anaesthesia 2013, 68, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, M.S.; Fredensborg, B.B. The disposable Ambu aScope vs. conventional flexible videoscope for awake intubation—A randomised study. Acta Anaesthesiol. Scand. 2013, 57, 888–895. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.K.; Ng, I.; Ang, J.P.; Koh, S.M.; Lee, K.; Mezzavia, P.; Morris, J.; Loh, F.; Segal, R. Randomised controlled trial comparing the Ambu aScope™2 with a conventional fibreoptic bronchoscope in orotracheal intubation of anaesthetised adult patients. Anaesth. Intensive Care 2015, 43, 479–484. [Google Scholar] [CrossRef]
- Perbet, S.; Blanquet, M.; Mourgues, C.; Delmas, J.; Bertran, S.; Longere, B.; Boiko-Alaux, V.; Chennell, P.; Bazin, J.-E.; Constantin, J.-M. Cost analysis of single-use (Ambu aScope™) and reusable bronchoscopes in the ICU. Ann. Intensive Care 2017, 7, 3. [Google Scholar] [CrossRef] [PubMed]
- Tvede, M.F.; Kristensen, M.S.; Nyhus-Andreasen, M. A cost analysis of reusable and disposable flexible optical scopes for intubation. Acta Anaesthesiol. Scand. 2012, 56, 577–584. [Google Scholar] [CrossRef] [PubMed]
- Zaidi, S.R.; Collins, A.M.; Mitsi, E.; Reiné, J.; Davies, K.; Wright, A.D.; Owugha, J.; Fitzgerald, R.; Ganguli, A.; Gordon, S.B.; et al. Single use and conventional bronchoscopes for broncho alveolar lavage (BAL) in research: A comparative study. BMC Pulm. Med. 2017, 17, 83. [Google Scholar] [CrossRef]
- Heitz, J.W.; Shum, P.P.; Grunwald, Z. Use of a tracheoscopic ventilation tube for endotracheal intubation in the difficult airway. J. Clin. Anesth. 2011, 23, 403–406. [Google Scholar] [CrossRef]
- Bicek, V.; Krecmerova, M.; Ungermannova, V.; Vymazal, T. Initial experience with the Vivasight ETView® double-lumen fibreoptic tube in thoracic surgery. Anest. Intenziv. Med. 2014, 25, 274–276. (In Czech) [Google Scholar]
- Saracoglu, A.; Saracoglu, K.T. VivaSight: A new era in the evolution of tracheal tubes. J. Clin. Anesth. 2016, 33, 442–449. [Google Scholar] [CrossRef]
- Massot, J.; Dumand-Nizard, V.; Fischler, M.; Le Guen, M. Evaluation of the double-lumen tube Vivasight-DL (DLT-ETView): A prospective single-center study. J. Cardiothorac. Vasc. Anesth. 2015, 29, 1544–1549. [Google Scholar] [CrossRef]
- Koopman, E.M.; Barak, M.; Weber, E.; Valk, M.J.; de Schepper, R.T.; Bouwman, R.A.; Huitink, J.M. Evaluation of a new double-lumen endobronchial tube with an integrated camera (VivaSight-DL(™)): A prospective multicentre observational study. Anaesthesia 2015, 70, 962–968. [Google Scholar] [CrossRef]
- Schuepbach, R.; Grande, B.; Camen, G.; Schmidt, A.R.; Fischer, H.; Sessler, D.I.; Seifert, B.; Spahn, D.R.; Ruetzler, K. Intubation with VivaSight or conventional left-sided double-lumen tubes: A randomized trial. Can. J. Anaesth. 2015, 62, 762–769. [Google Scholar] [CrossRef]
- Levy-Faber, D.; Malyanker, Y.; Nir, R.R.; Best, L.A.; Barak, M. Comparison of VivaSight double-lumen tube with a conventional double-lumen tube in adult patients undergoing video-assisted thoracoscopic surgery. Anaesthesia 2015, 70, 1259–1263. [Google Scholar] [CrossRef]
- Heir, J.S.; Guo, S.L.; Purugganan, R.; Jackson, T.A.; Sekhon, A.K.; Mirza, K.; Lasala, J.; Feng, L.; Cata, J.P. A randomized controlled study of the use of video double-lumen endobronchial tubes versus double-lumen endobronchial tubes in thoracic surgery. J. Cardiothorac. Vasc. Anesth. 2018, 32, 267–274. [Google Scholar] [CrossRef] [PubMed]
- Qiu, J.; Feng, M.; Zhang, C.; Yao, W. VivaSight™ single-lumen tube guided bronchial blocker placement for one-lung ventilation in a patient with a tracheal tumor under video-assisted transthoracic surgery: A case report. BMC Anesthesiol. 2019, 19, 2. [Google Scholar] [CrossRef] [PubMed]
- Rispoli, M.; Nespoli, M.R.; Mattiacci, D.M.; Curcio, C.; Casazza, D.; Amore, D. One lung ventilation management in a patients with Reinke’s edema. Int. J. Surg. Case Rep. 2020, 71, 294–296. [Google Scholar] [CrossRef] [PubMed]
- Grensemann, J.; Eichler, L.; Wang, N.; Jarczak, D.; Simon, M.; Kluge, S. Endotracheal tube-mounted camera-assisted intubation versus conventional intubation in intensive care: A prospective, randomised trial (VivalTN). Crit. Care 2018, 22, 235. [Google Scholar] [CrossRef]
- Pandit, J.J.; Popat, M.T.; Cook, T.M.; Wilkes, A.R.; Groom, P.; Cooke, H.; Kapila, A.; O’Sullivan, E. The Difficult Airway Society ‘ADEPT’ guidance on selecting airway devices: The basis of a strategy for equipment evaluation. Anaesthesia 2011, 66, 726–737. [Google Scholar] [CrossRef] [PubMed]
- Abdelmalak, B.B.; Doyle, J.D. Recent trends in airway management. F1000 Res. 2020, 9, 355. [Google Scholar] [CrossRef]




| Device Type | Device | Manufacturer | Level of Evidence |
|---|---|---|---|
| Supraglottic airway | ILMA, Fastrach | Laryngeal Mask Co., Mahé, Seychelles | 1b |
| Air-Q ILA | Mercury Medical, Clearwater, FL, USA | 2b | |
| i-gel | Intersurgical Ltd., Wokingham, UK | 1b | |
| Aura-i | Ambu A/S, Ballerup, Denmark | 2b | |
| AuraGain | Ambu A/S, Ballerup, Denmark | 2b | |
| LMA Protector | Teleflex Medical Ltd., Limerick, Ireland | 2b | |
| Hybrid device | LMA CTrach | The Laryngeal Mask Co., Singapore | 1a |
| TotalTrack VLM | MedComflow S.A., Barcelona, Spain | 2b | |
| Optical stylet | Bonfils stylet | Karl Storz KG, Tuttlingen, Germany | 1a |
| Shikani stylet | Clarus Medical, Minneapolis, MN, USA | 2b | |
| Levitan FPS stylet | Clarus Medical, Minneapolis, MN, USA | 2b | |
| Sensascope | Acutronic AG, Bubikon, Switzerland | 2b | |
| Trachway, | Biotronic Instruments Ltd., Beijing, China | 2b | |
| Stylet Viu | StyletViu Inc., Costa Mesa, CA, USA | 5 | |
| AinCa video stylet | Anesthesia Associates Inc., San Marcos, CA, USA | 5 | |
| C-MAC Video Stylet | Karl Storz KG, Tuttlingen, Germany | 4 | |
| UE Scope Video Stylet | UE Medical Devices Inc., Newton, MA, USA | 5 | |
| Intular Scope | Medical Park, Sinsu-ro, South Korea | 2b | |
| Flexible endoscope | aScope | Ambu A/S, Ballerup, Denmark | 2b |
| (single-use) | C-MAC Five S | Karl Storz KG, Tuttlingen, Germany | 5 |
| Optical tracheal tube | VivaSight-SL | Ambu A/S, Ballerup, Denmark | 2b |
| VivaSight-DL | Ambu A/S, Ballerup, Denmark | 2b |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matek, J.; Kolek, F.; Klementova, O.; Michalek, P.; Vymazal, T. Optical Devices in Tracheal Intubation—State of the Art in 2020. Diagnostics 2021, 11, 575. https://doi.org/10.3390/diagnostics11030575
Matek J, Kolek F, Klementova O, Michalek P, Vymazal T. Optical Devices in Tracheal Intubation—State of the Art in 2020. Diagnostics. 2021; 11(3):575. https://doi.org/10.3390/diagnostics11030575
Chicago/Turabian StyleMatek, Jan, Frantisek Kolek, Olga Klementova, Pavel Michalek, and Tomas Vymazal. 2021. "Optical Devices in Tracheal Intubation—State of the Art in 2020" Diagnostics 11, no. 3: 575. https://doi.org/10.3390/diagnostics11030575
APA StyleMatek, J., Kolek, F., Klementova, O., Michalek, P., & Vymazal, T. (2021). Optical Devices in Tracheal Intubation—State of the Art in 2020. Diagnostics, 11(3), 575. https://doi.org/10.3390/diagnostics11030575







