Relationship between Axial Length and Corneo-Scleral Topography: A Preliminary Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Ocular Examination
2.3. Parameters Evaluated
- Inner best-fit sphere (iBFS): best-fit sphere obtained by least squares method of all corneal points from the center to the limbus.
- Limbus best-fit sphere (lBFS): best-fit sphere obtained by least squares method of all points conforming to the limbal area, which is determined as the zone delimited by the first intersection of the inner and outer best-fit spheres with the corneal and scleroconjunctival surfaces at the transition area between conjunctiva and cornea, respectively.
- Outer best-fit sphere (oBFS): best-fit sphere obtained by least squares method of all points from the scleroconjunctival surface detected.
- Mean corneal radius (cr) calculated within the area determined by the limbal diameter.
- Mean scleral radii (sr) calculated for the rest of the area covered by the measurement.
- Sagittal height measurements including mean (MSH), minimum (MinSH), and maximum (MaxSH) sagittal heights. It should be considered that the ESP device calculates the sagittal height as the distance from corneal apex to the line defined by any chord selected.
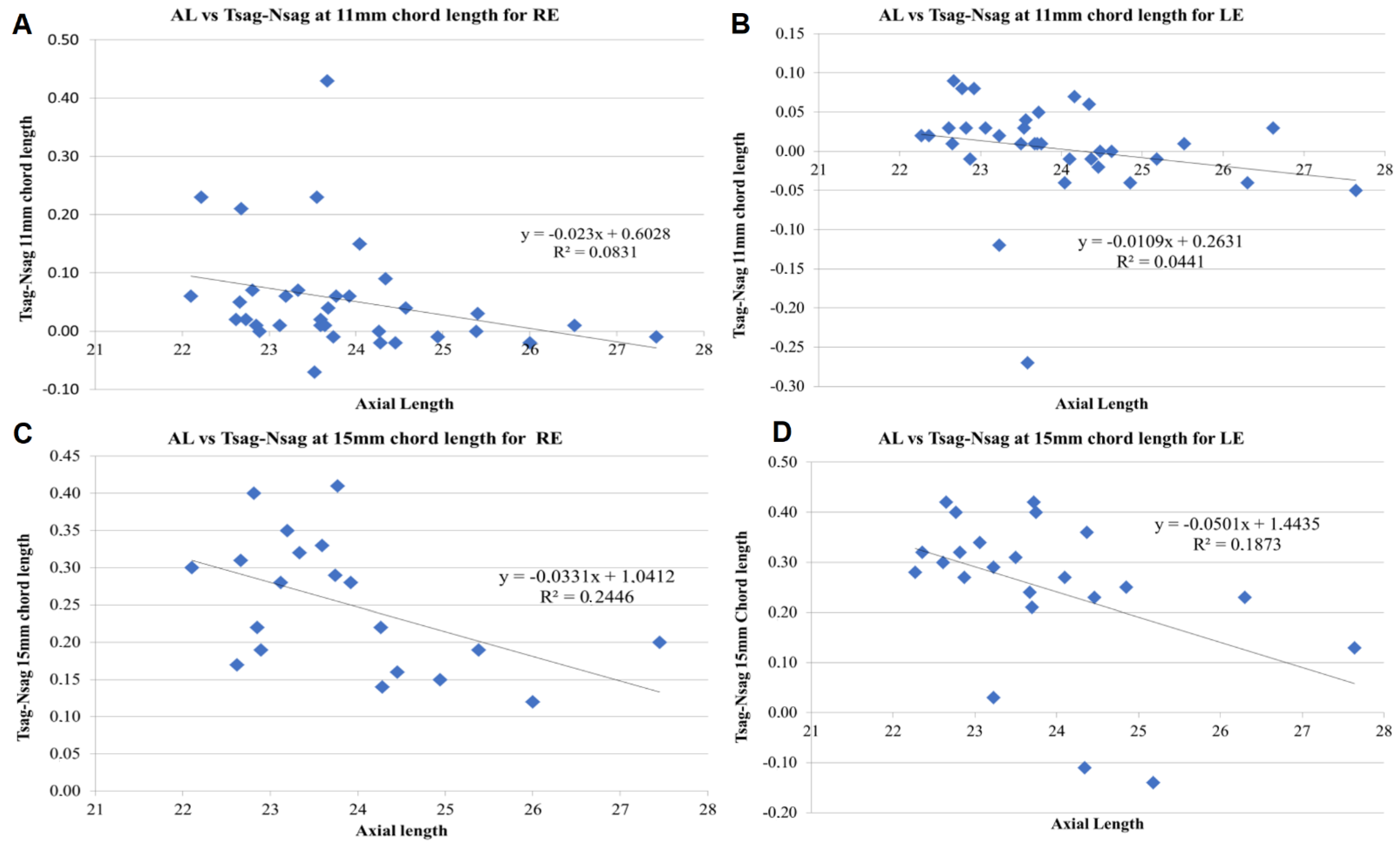
- Difference between temporal and nasal sagittal heights for a specific chord length (T-NSH).
- For this study, all the sagittal height parameters extracted from the ESP were evaluated for chord lengths of 11, 12, 13, 14, and 15 mm.
- Sphere, cylinder, and spherical equivalent: refraction data at 3-mm pupil diameter.
- Km: average keratometry measurement.
- CCT: central corneal thickness.
- CD: corneal diameter.
- Q: corneal asphericity.
- High order and coma root mean square (RMS) and spherical aberration: ocular aberrations for a 5-mm pupil size.
- IOP: intraocular pressure.
2.4. Statistical Analysis
3. Results
- A significance level of 0.05 was selected to entry in the model.
- The model was fitted with all possible independent predictors.
- The predictor with the highest p-value was considered. If p > 0.10, the predictor was removed.
- The model was fitted without this last variable and the previous step (3) was repeated until the condition became false.
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Baird, P.N.; Saw, S.M.; Lanca, C.; Guggenheim, J.A.; Smith, E.L., III; Zhou, X.; Matsui, K.O.; Wu, P.C.; Sankaridurg, P.; Chia, A.; et al. Myopia. Nat. Rev. Dis. Primers 2020, 6, 99. [Google Scholar] [CrossRef] [PubMed]
- Morgan, I.G.; French, A.N.; Ashby, R.S.; Guo, X.; Ding, X.; He, M.; Rose, K.A. The epidemics of myopia: Aetiology and prevention. Prog. Retin. Eye Res. 2018, 62, 134–149. [Google Scholar] [CrossRef] [PubMed]
- Bullimore, M.A.; Brennan, N.A. Myopia control: Why each diopter matters. Optom. Vis. Sci. 2019, 96, 463–465. [Google Scholar] [CrossRef]
- Consejo, A.; Rozema, J.J. In vivo anterior scleral morphometry, axial length and myopia. Contact Lens Anterior Eye 2020, 43, 21–25. [Google Scholar] [CrossRef]
- Niyazmand, H.; Read, S.A.; Atchison, D.A.; Collins, M.J. Anterior eye shape in emmetropes, low to moderate myopes, and high myopes. Contact Lens Anterior Eye 2020, 21. [Google Scholar] [CrossRef] [PubMed]
- Pekel, G.; Yağcı, R.; Acer, S.; Ongun, G.T.; Çetin, E.N.; Simavlı, H. Comparison of Corneal Layers and Anterior Sclera in Emmetropic and Myopic Eyes. Cornea 2015, 34, 786–790. [Google Scholar] [CrossRef] [PubMed]
- Dhakal, R.; Vupparaboina, K.K.; Verkicharla, P.K. Anterior Sclera Undergoes Thinning with Increasing Degree of Myopia. Investig. Ophthalmol. Vis. Sci. 2020, 61, 6. [Google Scholar] [CrossRef]
- Niyazmand, H.; Read, S.A.; Atchison, D.A.; Collins, M.J. Effects of accommodation and simulated convergence on anterior scleral shape. Ophthalmic Physiol. Opt. 2020, 40, 482–490. [Google Scholar] [CrossRef]
- Woodman-Pieterse, E.C.; Read, S.A.; Collins, M.J.; Alonso-Caneiro, D. Anterior scleral thickness changes with accommodation in myopes and emmetropes. Exp. Eye Res. 2018, 177, 96–103. [Google Scholar] [CrossRef] [PubMed]
- Piñero, D.P.; López-Navarro, A.; Cabezos, I.; de Fez, D.; Caballero, M.T.; Camps, V.J. Intrasession repeatability of refractive and ocular aberrometric measurements obtained using a multidiagnostic device in healthy eyes. Clin. Optom. 2017, 9, 91–96. [Google Scholar] [CrossRef]
- Sanchez, I.; Ortiz-Toquero, S.; Martin, R. Intrasession repeatability and intersession reproducibility measurements using VX120 multidiagnostic unit. Eye Contact Lens 2018, 44, S266–S272. [Google Scholar] [CrossRef]
- Gordon-Shaag, A.; Piñero, D.P.; Kahloun, C.; Markov, D.; Parnes, T.; Gantz, L.; Shneor, E. Validation of refraction and anterior segment parameters by a new multi-diagnostic platform (VX120). J. Optom. 2018, 11, 242–251. [Google Scholar] [CrossRef]
- Piñero, D.P.; Cabezos, I.; López-Navarro, A.; de Fez, D.; Caballero, M.T.; Camps, V.J. Intrasession repeatability of ocular anatomical measurements obtained with a multidiagnostic device in healthy eyes. BMC Ophthalmol. 2017, 17, 193. [Google Scholar] [CrossRef] [PubMed]
- Piñero, D.P.; López-Navarro, A.; Cabezos, I.; Fez, D.D.; Caballero, M.T.; Camps, V.J. Corneal topographic and aberrometric measurements obtained with a multidiagnostic device in healthy eyes: Intrasession repeatability. J. Ophthalmol. 2017, 2017, 2149145. [Google Scholar] [CrossRef] [PubMed]
- Shirayama, M.; Wang, L.; Koch, D.D.; Weikert, M.P. Comparison of accuracy of intraocular lens calculations using automated keratometry, a Placido-based corneal topographer, and a combined Placido-based and dual Scheimpflug corneal topographer. Cornea 2010, 29, 1136–1138. [Google Scholar] [CrossRef]
- Rajan, M.S.; Keilhorn, I.; Bell, J.A. Partial coherence laser interferometry vs conventional ultrasound biometry in intraocular lens power calculations. Eye 2002, 16, 552–556. [Google Scholar] [CrossRef]
- Bataille, L.; Molina-Martin, A.; Piñero, D.P. Intrasession repeatability of corneal, limbal and scleral measurements obtained with a Fourier transform profilometer. Contact Lens Anterior Eye 2020, 23. [Google Scholar] [CrossRef]
- Pinero, D.P.; Martinez-Abad, A.; Soto-Negro, R.; Ariza-Gracia, M.A.; Carracedo, G. Characterization of corneoscleral geometry using Fourier transform profilometry in the healthy eye. Eye Contact Lens 2019, 45, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Haładaj, R. Normal Anatomy and Anomalies of the Rectus Extraocular Muscles in Human: A Review of the Recent Data and Findings. Biomed Res. Int. 2019, 2019, 8909162. [Google Scholar] [CrossRef] [PubMed]
- McBrien, N.A.; Gentle, A. Role of the sclera in the development and pathological complications of myopia. Prog. Retin. Eye Res. 2003, 22, 307–338. [Google Scholar] [CrossRef]
- McBrien, N.A.; Jobling, A.I.; Gentle, A. Biomechanics of the sclera in myopia: Extracellular and cellular factors. Optom. Vis. Sci. 2009, 86, E23–E30. [Google Scholar] [CrossRef]
- McMonnies, C.W. An examination of the relation between intraocular pressure, fundal stretching and myopic pathology. Clin. Exp. Optom. 2016, 99, 113–119. [Google Scholar] [CrossRef]
- El-Fayoumi, D.; Bahgat, N.; Khafagy, M.; Hatata, R.; Sabry, D.; Allam, G.; Kasem, M.A.; Sadek, S. Horizontal Extraocular Muscle Insertion Site in Relation to Axial Length Using Swept-Source Anterior Segment OCT. Clin. Ophthalmol. 2020, 14, 3583–3589. [Google Scholar] [CrossRef] [PubMed]
- Clark, R.A.; Demer, J.L. The Effect of Axial Length on Extraocular Muscle Leverage. Am. J. Ophthalmol. 2020, 216, 186–192. [Google Scholar] [CrossRef]
- Touzeau, O.; Allouch, C.; Borderie, V.; Kopito, R.; Laroche, L. Correlation between refraction and ocular biometry. J. Fr. Ophtalmol. 2003, 26, 355–363. [Google Scholar]
- Park, S.H.; Park, K.H.; Kim, J.M.; Choi, C.Y. Relation between axial length and ocular parameters. Ophthalmologica 2010, 224, 188–193. [Google Scholar] [CrossRef] [PubMed]
- Touzeau, O.; Gaujoux, T.; Sandali, O.; Allouch, A.; Laroche, L.; Borderie, V. The cornea in high axial myopia. J. Fr. Ophtalmol. 2014, 37, 449–461. [Google Scholar] [CrossRef] [PubMed]
- Tideman, J.W.L.; Snabel, M.C.C.; Tedja, M.S.; Van Rijn, G.A.; Wong, K.T.; Kuijpers, R.W.A.M.; Vingerling, J.R.; Hofman, A.; Buitendijk, G.H.S.; Keunen, J.E.E.; et al. Association of Axial Length with Risk of Uncorrectable Visual Impairment for Europeans With Myopia. JAMA Ophthalmol. 2016, 134, 1355–1363. [Google Scholar] [CrossRef]
- Llorente, L.; Barbero, S.; Cano, D.; Dorronsoro, C.; Marcos, S. Myopic versus hyperopic eyes: Axial length, corneal shape and optical aberrations. J. Vis. 2004, 4, 288–298. [Google Scholar] [CrossRef] [PubMed]
- Hashemi, H.; Khabazkhoob, M.; Emamian, M.H.; Shariat, M.; Yekta, A.; Fotouhi, A. White-to-white corneal diameter distribution in an adult population. J. Curr. Ophthalmol. 2015, 27, 21–24. [Google Scholar] [CrossRef]
- Hosny, M.; Alio, J.L.; Claramonte, P.; Attia, W.H.; Perez-Santonja, J.J. Relationship between anterior chamber depth, refractive state, corneal diameter, and axial length. J. Refract. Surg. 2000, 16, 336–340. [Google Scholar] [PubMed]
- Lau, J.K.; Vincent, S.J.; Collins, M.J.; Cheung, S.W.; Cho, P. Ocular higher-order aberrations and axial eye growth in young Hong Kong children. Sci. Rep. 2018, 8, 6726. [Google Scholar] [CrossRef] [PubMed]
- Rajan, M.S.; Bunce, C.; Tuft, S. Interocular axial length difference and age-related cataract. J. Cataract Refract. Surg. 2008, 34, 76–79. [Google Scholar] [CrossRef]
- Hashemi, H.; Khabazkhoob, M.; Emamian, M.H.; Shariati, M.; Abdolahi-nia, T.; Fotouhi, A. All biometric components are important in anisometropia, not just axial length. Br. J. Ophthalmol. 2013, 97, 1586–1591. [Google Scholar] [CrossRef] [PubMed]
| Mean | (SD) | Median | Max | Min | |
|---|---|---|---|---|---|
| Age (years) | 33.09 | 12.86 | 30.55 | 51.90 | 12.01 |
| Sphere (D) | −1.58 | 2.88 | −0.50 | 4.00 | −12.00 |
| Cylinder (D) | −0.79 | 0.73 | −0.50 | 0.00 | −3.00 |
| Spherical equivalent (D) | −1.94 | 2.94 | −0.69 | 2.50 | −13.12 |
| Km (D) | 43.63 | 1.14 | 43.75 | 46 | 41 |
| CCT (µm) | 541.85 | 40.69 | 542.50 | 614 | 438 |
| Q | −0.199 | 0.161 | −0.195 | 0.210 | −0.560 |
| CD (mm) | 12.43 | 0.49 | 12.42 | 13.68 | 11.24 |
| HOA RMS (µm) | 0.1932 | 0.08947 | 0.1900 | 0.45 | 0.05 |
| Coma RMS (µm) | 0.1225 | 0.07724 | 0.11 | 0.36 | 0.01 |
| Spherical aberration (µm) | 0.0311 | 0.07168 | 0.0300 | 0.15 | −0.17 |
| IOP (mm Hg) | 14.26 | 2.518 | 14 | 22 | 9 |
| AL (mm) | 23.88 | 1.244 | 23.66 | 27.64 | 22.10 |
| Mean | (SD) | Median | Max | Min | |
|---|---|---|---|---|---|
| cr (mm) | 8.80 | 0.270 | 8.80 | 9.28 | 8.22 |
| sr (mm) | 13.29 | 1.588 | 13.23 | 20.22 | 11.17 |
| iBFS (mm) | 8.95 | 0.339 | 8.92 | 9.69 | 7.79 |
| oBFS (mm) | 12.50 | 1.171 | 12.24 | 16.70 | 9.67 |
| lBFS (mm) | 6.12 | 0.432 | 6.06 | 7.61 | 5.10 |
| MSH11 (mm) | 1.92 | 0.090 | 1.93 | 2.11 | 1.56 |
| T-NSH11 (mm) | 0.026 | 0.084 | 0.015 | 0.43 | −0.27 |
| MinSH11 (mm) | 1.765 | 0.123 | 1.785 | 2.01 | 1.42 |
| MaxSH11 (mm) | 1.979 | 0.087 | 1.980 | 2.24 | 1.61 |
| MSH12 (mm) | 2.268 | 0.123 | 2.280 | 2.49 | 1.80 |
| T-NSH12 (mm) | 0.059 | 0.108 | 0.050 | 0.63 | −0.14 |
| MinSH12 (mm) | 2.117 | 0.145 | 2.125 | 2.42 | 1.63 |
| MaxSH12 (mm) | 2.334 | 0.112 | 2.340 | 2.57 | 1.81 |
| MSH13 (mm) | 2.630 | 0.132 | 2.635 | 2.96 | 2.11 |
| T-NSH13 (mm) | 0.120 | 0.151 | 0.100 | 0.90 | −0.10 |
| MinSH13 (mm) | 2.482 | 0.159 | 2.495 | 2.79 | 1.86 |
| MaxSH13 (mm) | 2.703 | 0.110 | 2.705 | 3.03 | 2.50 |
| MSH14 (mm) | 2.981 | 0.151 | 3.000 | 3.37 | 2.40 |
| T-NSH14 (mm) | 0.177 | 0.124 | 0.180 | 0.71 | −0.12 |
| MinSH14 (mm) | 2.857 | 0.164 | 2.865 | 3.11 | 2.13 |
| MaxSH14 (mm) | 3.034 | 0.206 | 3.060 | 3.47 | 1.89 |
| MSH15 (mm) | 3.348 | 0.173 | 3.370 | 3.80 | 2.71 |
| T-NSH15 (mm) | 0.252 | 0.124 | 0.280 | 0.42 | −0.14 |
| MinSH15 (mm) | 3.236 | 0.185 | 3.230 | 3.58 | 2.42 |
| MaxSH15 (mm) | 3.413 | 0.159 | 3.430 | 3.91 | 3.06 |
| R2 | Adjusted R2 | Durbin–Watson | Mean Cook Distance ± SD | F (Sig) | Kolmogorov–Smirnov Test | ||
|---|---|---|---|---|---|---|---|
| 13-mm chord length | RE model | 0.890 | 0.866 | 2.172 | 0.063 ± 0.098 | 36.465 (p < 0.001) | p = 0.200 |
| LE model | 0.728 | 0.700 | 2.131 | 0.065 ± 0.105 | 25.447 (p < 0.001) | p = 0.200 | |
| 14-mm chord length | RE model | 0.876 | 0.843 | 1.970 | 0.070 ± 0.083 | 26.513 (p < 0.001) | p = 0.143 |
| LE model | 0.786 | 0.730 | 1.884 | 0.809 ± 3.447 | 13.813 (p < 0.001) | p = 0.200 |
| Predictors | B | SE | Beta | t | Sig. | Tolerance | VIF | ||
|---|---|---|---|---|---|---|---|---|---|
| 13-mm chord length | RE model | SE | −0.291 | 0.035 | −0.712 | −8.216 | <0.001 | 0.812 | 1.232 |
| CD | 0.906 | 0.148 | 0.480 | 6.137 | <0.001 | 0.999 | 1.001 | ||
| HOA RMS | 2.311 | 1.016 | 0.211 | 2.274 | 0.035 | 0.710 | 1.408 | ||
| MinSH13 | −1.959 | 0.619 | −0.267 | −3.166 | 0.005 | 0.861 | 1.162 | ||
| LE model | SE | −0.384 | 0.057 | −0.821 | −6.787 | <0.001 | 0.977 | 1.023 | |
| Km | −0.330 | 0.103 | −0.386 | −3.194 | 0.005 | 0.977 | 1.023 |
| Predictors | B | SE | Beta | t | Sig. | Tolerance | VIF | ||
|---|---|---|---|---|---|---|---|---|---|
| 14 m chord length | RE model | SE | −0.266 | 0.042 | −0.642 | −6.344 | 0.000 | 0.807 | 1.239 |
| CD | 0.989 | 0.168 | 0.554 | 5.895 | 0.000 | 0.934 | 1.070 | ||
| HOA RMS | 2.774 | 1.121 | 0.280 | 2.475 | 0.026 | 0.646 | 1.547 | ||
| MinSH14 | −1.774 | 0.708 | -0.270 | −2.508 | 0.024 | 0.715 | 1.399 | ||
| LE model | SE | −0.399 | 0.058 | −0.977 | −6.920 | 0.000 | 0.715 | 1.400 | |
| Km | −0.329 | 0.090 | −0.476 | −3.672 | 0.002 | 0.845 | 1.183 | ||
| CD | 0.086 | 0.047 | 0.231 | 1.852 | 0.084 | 0.912 | 1.097 | ||
| HOA RMS | −3.964 | 1.475 | −0.380 | −2.687 | 0.017 | 0.711 | 1.407 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bataille, L.; Molina-Martín, A.; Piñero, D.P. Relationship between Axial Length and Corneo-Scleral Topography: A Preliminary Study. Diagnostics 2021, 11, 542. https://doi.org/10.3390/diagnostics11030542
Bataille L, Molina-Martín A, Piñero DP. Relationship between Axial Length and Corneo-Scleral Topography: A Preliminary Study. Diagnostics. 2021; 11(3):542. https://doi.org/10.3390/diagnostics11030542
Chicago/Turabian StyleBataille, Laurent, Ainhoa Molina-Martín, and David P. Piñero. 2021. "Relationship between Axial Length and Corneo-Scleral Topography: A Preliminary Study" Diagnostics 11, no. 3: 542. https://doi.org/10.3390/diagnostics11030542
APA StyleBataille, L., Molina-Martín, A., & Piñero, D. P. (2021). Relationship between Axial Length and Corneo-Scleral Topography: A Preliminary Study. Diagnostics, 11(3), 542. https://doi.org/10.3390/diagnostics11030542








