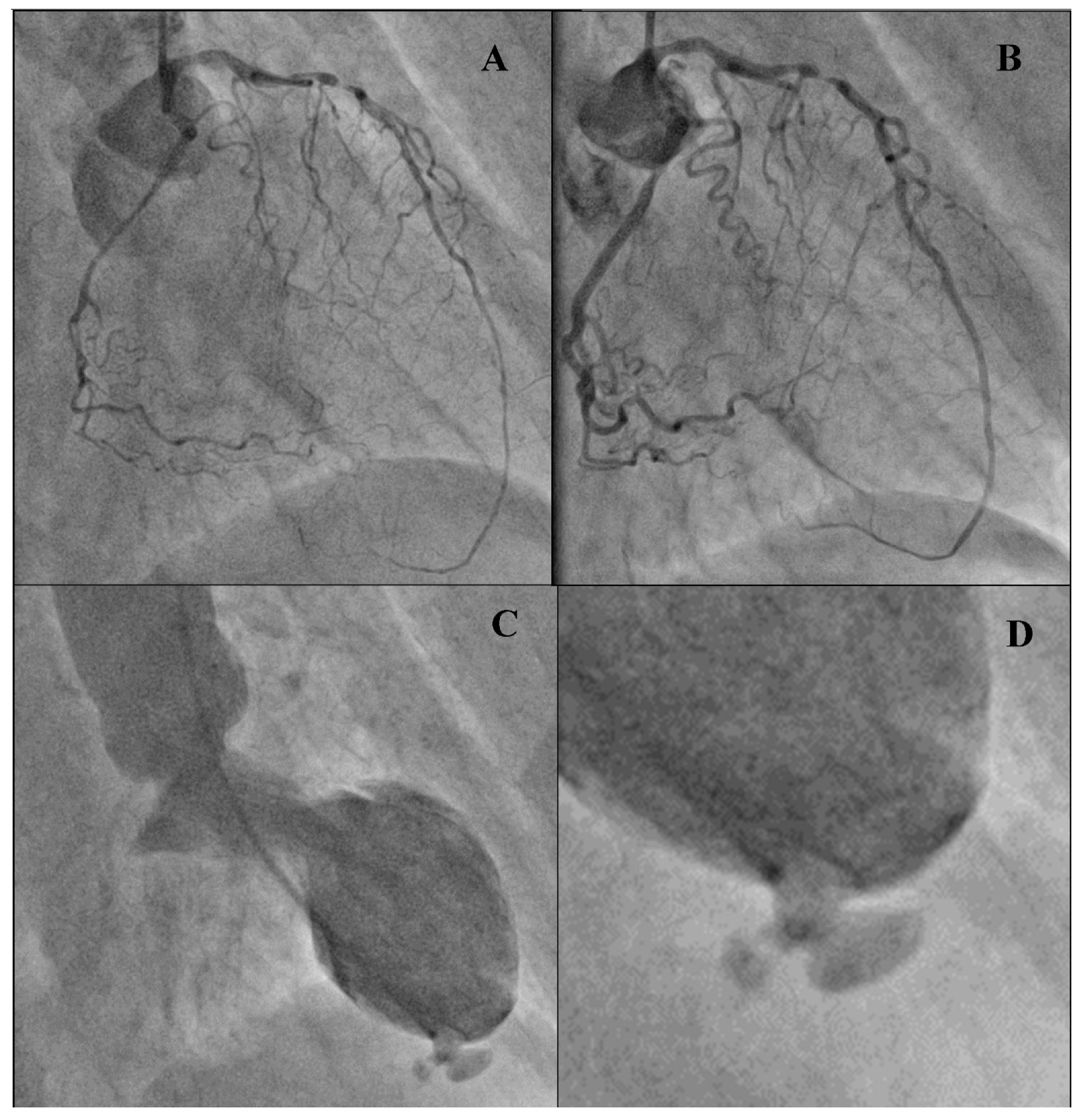
Left Ventricular Rupture as a Complication of Anterior Wall Myocardial Infarction on Computed Tomography Angiography and Ventriculography
Abstract
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Crea, F.; Libby, P. Acute Coronary Syndromes: The way forward from mechanisms to precision treatment. Circulation 2017, 136, 1155–1166. [Google Scholar] [CrossRef] [PubMed]
- Paz, D.O.P.-D.; Rio, J.E.H.-D.; González-Padilla, C.; Esturau-Santaló, R.M.; Romero-Palafox, J.; Grover-Paez, F.; Cardona-Muller, D. Left ventricular free-wall rupture, a potentially lethal mechanical complication of acute myocardial infarction: An unusual and illustrative case report. BMC Cardiovasc. Disord. 2019, 19, 80. [Google Scholar] [CrossRef]
- Varghese, S.; Ohlow, M.-A. Left ventricular free wall rupture in myocardial infarction: A retrospective analysis from a single tertiary center. JRSM Cardiovasc. Dis. 2019, 8, 8. [Google Scholar] [CrossRef]
- Frances, C.; Romero, A.; Grady, D. Left ventricular pseudoaneurysm. J. Am. Coll. Cardiol. 1998, 32, 557–561. [Google Scholar] [CrossRef]
- Matteucci, M.; Fina, D.; Jiritano, F.; Meani, P.; Blankesteijn, W.M.; Raffa, G.M.; Kowaleski, M.; Heuts, S.; Beghi, C.; Maessen, J.; et al. Treatment strategies for post-infarction left ventricular free-wall rupture. Eur. Heart J. Acute Cardiovasc. Care 2019, 8, 379–387. [Google Scholar] [CrossRef] [PubMed]
- Onoda, N.; Nonami, A.; Yabe, T.; Doi, Y.L.; Fujita, Y.; Yamamoto, S.; Ikebuchi, M.; Irie, H. Postinfarct cardiac free wall rupture detected by multidetector computed tomography. J. Cardiol. Cases 2012, 5, e147–e149. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Redfern, A.; Smart, J. Images in clinical medicine. Cardiac rupture. N. Engl. J. Med. 2003, 348, 609. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gać, P.; Macek, P.; Szczepański, A.; Poręba, R. Left Ventricular Rupture as a Complication of Anterior Wall Myocardial Infarction on Computed Tomography Angiography and Ventriculography. Diagnostics 2021, 11, 525. https://doi.org/10.3390/diagnostics11030525
Gać P, Macek P, Szczepański A, Poręba R. Left Ventricular Rupture as a Complication of Anterior Wall Myocardial Infarction on Computed Tomography Angiography and Ventriculography. Diagnostics. 2021; 11(3):525. https://doi.org/10.3390/diagnostics11030525
Chicago/Turabian StyleGać, Paweł, Piotr Macek, Andrzej Szczepański, and Rafał Poręba. 2021. "Left Ventricular Rupture as a Complication of Anterior Wall Myocardial Infarction on Computed Tomography Angiography and Ventriculography" Diagnostics 11, no. 3: 525. https://doi.org/10.3390/diagnostics11030525
APA StyleGać, P., Macek, P., Szczepański, A., & Poręba, R. (2021). Left Ventricular Rupture as a Complication of Anterior Wall Myocardial Infarction on Computed Tomography Angiography and Ventriculography. Diagnostics, 11(3), 525. https://doi.org/10.3390/diagnostics11030525






