Idiosyncratic Drug-Induced Liver Injury (DILI) and Herb-Induced Liver Injury (HILI): Diagnostic Algorithm Based on the Quantitative Roussel Uclaf Causality Assessment Method (RUCAM)
Abstract
1. Introduction
2. Literature Search and Source
3. Definitions
3.1. RUCAM-Based Liver Injury
3.2. RUCAM-Based Liver Injury Pattern
3.3. DILI
3.4. HILI
4. Historical Background of RUCAM and Call to Name RUCAM Correctly
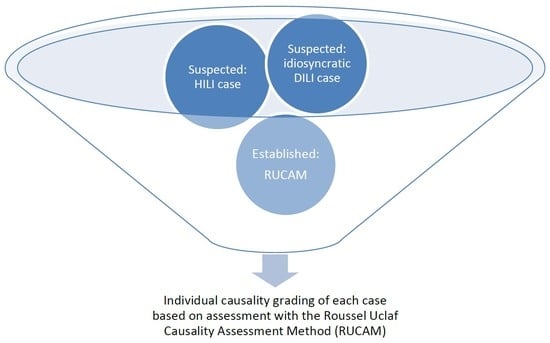
5. Diagnostic RUCAM Algorithm and Artificial Intelligence
6. COVID-19, DILI, HILI, and RUCAM
7. Worldwide Use of RUCAM
8. Worldwide Annual Growth Trend Analysis of RUCAM Publications
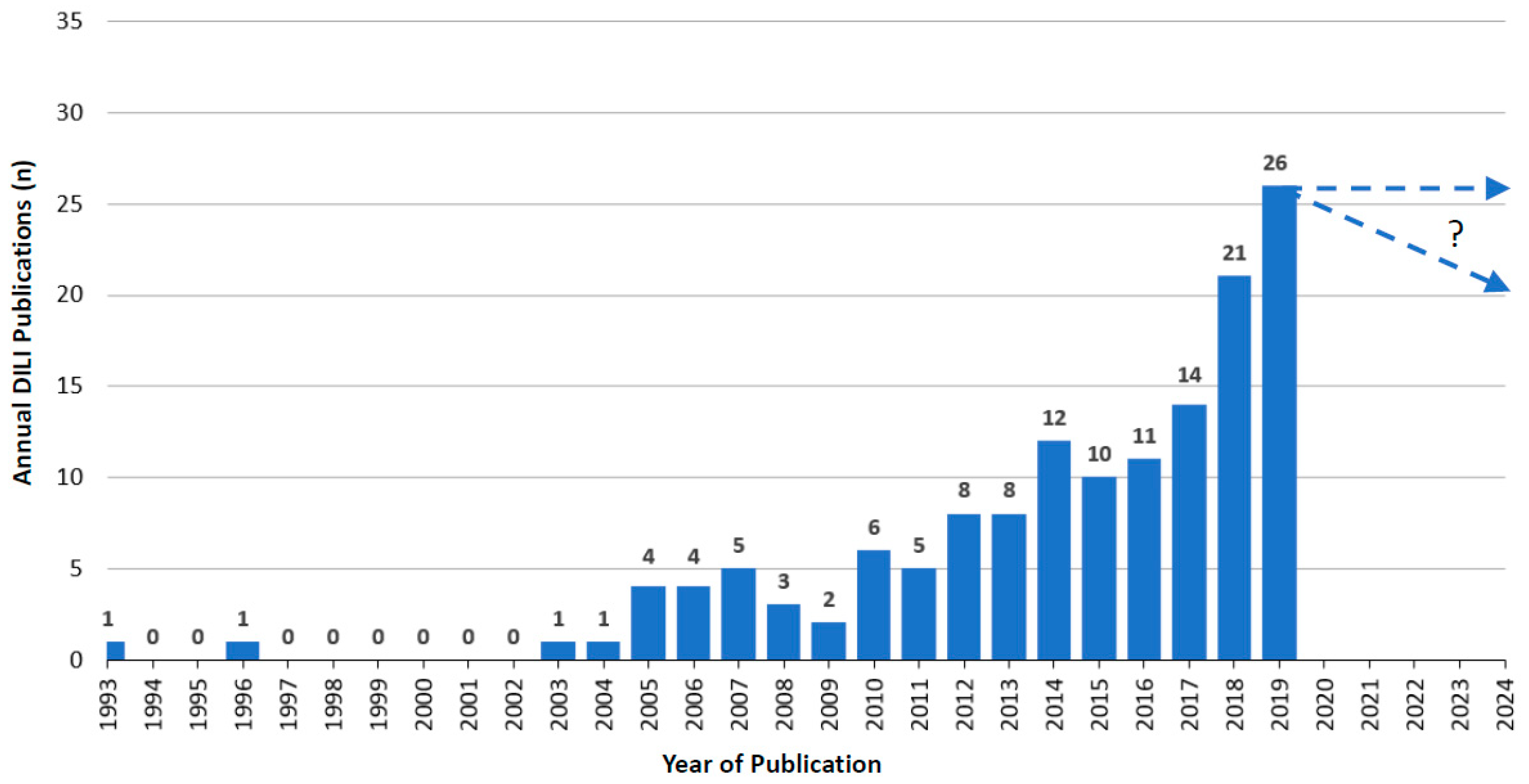
8.1. RUCAM-Based DILI Publications
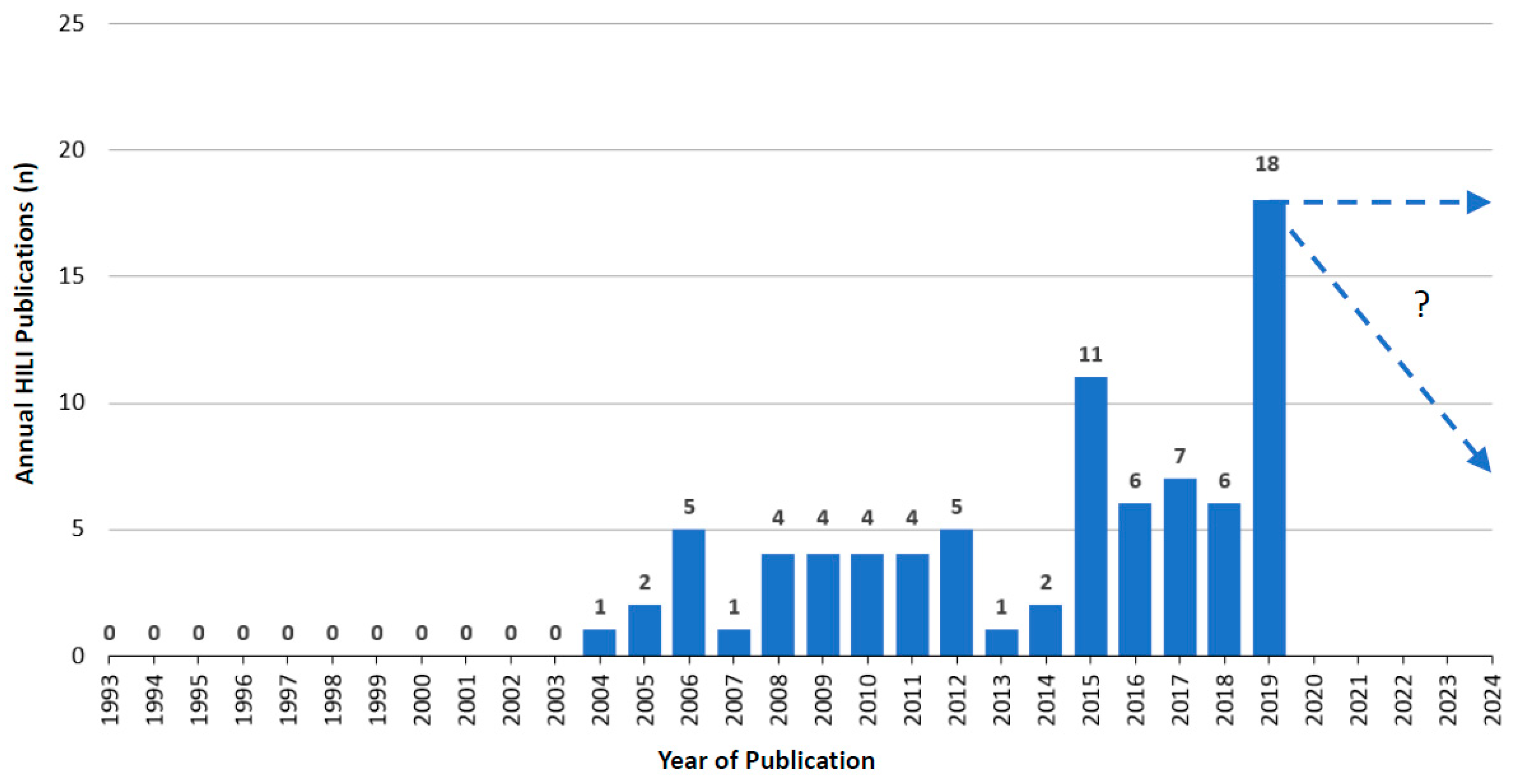
8.2. RUCAM-Based HILI Publications
9. Scientometric Evaluation and RUCAM
10. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Uetrecht, J. Mechanistic Studies of Idiosyncratic DILI: Clinical Implications. Front. Pharmacol. 2019, 10, 837. [Google Scholar] [CrossRef]
- Teschke, R.; Uetrecht, J. Idiosyncratic drug induced liver injury (DILI): Unresolved basic issues. In special issue: Unresolved basic issues in hepatology. Ann. Transl. Med. 2020, 7, 62. [Google Scholar] [CrossRef]
- Ke, L.; Lu, C.; Shen, R.; Lu, T.; Ma, B.; Hua, Y. Knowledge Mapping of Drug-Induced Liver Injury: A Scientometric Investigation (2010–2019). Front. Pharmacol. 2020, 11, 842. [Google Scholar] [CrossRef] [PubMed]
- Danan, G.; Benichou, C. Causality assessment of adverse reactions to drugs—I. A novel method based on the conclusions of international consensus meetings: Application to drug-induced liver injuries. J. Clin. Epidemiol. 1993, 46, 1323–1330. [Google Scholar] [CrossRef]
- Teschke, R.; Zhu, Y.; Jing, J. Herb induced liver injury (HILI) in the Asian region and current role of RUCAM for causality as-sessment in 11,160 published cases: Analysis and outlook. J. Clin. Transl. Hepatol. 2020, 8, 1–15. [Google Scholar] [CrossRef]
- Teschke, R.; Eickhoff, A.; Schulze, J.; Danan, G. Herb-induced liver injury (HILI) with 12,068 worldwide cases published with causality assessments by Roussel Uclaf Causality Assessment Method (RUCAM): An overview. Transl. Gastroenterol. Hepatol. 2020. [Google Scholar] [CrossRef]
- Teschke, R.; Danan, G. Worldwide Use of RUCAM for Causality Assessment in 81,856 Idiosyncratic DILI and 14,029 HILI Cases Published 1993–Mid 2020: A Comprehensive Analysis. Medicines 2020, 7, 62. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Qi, X.; Yoshida, E.M.; Mendez-Sanchez, N.; Teschke, R.; Sun, M.; Liu, X.; Su, C.; Deng, J.; Deng, H.; et al. Clinical characteristics and outcomes of traditional Chinese medicine-induced liver injury: A systematic review. Expert Rev. Gastroenterol. Hepatol. 2018, 12, 425–434. [Google Scholar] [CrossRef] [PubMed]
- Real, M.; Barnhill, M.S.; Higley, C.; Rosenberg, J.; Lewis, J.H. Drug-Induced Liver Injury: Highlights of the Recent Literature. Drug Saf. 2019, 42, 365–387. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, J.J.; Higley, C.; Shabazi, S.; Lewis, J.H. Selected highlights and controversies of drug-induced liver injury from the recent literature. World J. Gastroenterol. Hepatol. Endosc. Res. 2020, 1, 1–16. [Google Scholar]
- Teschke, R. Review. Top-ranking drugs out of 3312 drug-induced liver injury cases evaluated by the Roussel Uclaf Causality Assessment Method. Expert. Opin. Drug. Metab. Toxicol. 2018, 14, 1169–1187. [Google Scholar] [CrossRef]
- Björnsson, E.S. Hepatotoxicity by Drugs: The Most Common Implicated Agents. Int. J. Mol. Sci. 2016, 17, 224. [Google Scholar] [CrossRef] [PubMed]
- Björnsson, E.S.; Hoofnagle, J.H. Categorization of drugs implicated in causing liver injury: Critical assessment based on published case reports. Hepatology 2016, 63, 590–603. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R.; Xuan, T.D. Suspected herb induced liver injury by green tea extracts: Critical review and case analysis applying RUCAM for causality assessment. Jpn. J. Gastroenterol. Hepatol. 2019, 1, 1–16. [Google Scholar]
- Oketch-Rabah, H.A.; Roe, A.L.; Rider, C.V.; Bonkovsky, H.L.; Giancaspro, G.I.; Navarro, V.; Paine, M.F.; Betz, J.M.; Marles, R.J.; Casper, S.; et al. United States Pharmacopeia (USP) comprehensive review of the hepatotoxicity of green tea extracts. Toxicol. Rep. 2020, 7, 386–402. [Google Scholar] [CrossRef] [PubMed]
- Björnsson, H.K.; Björnsson, E.S. Database Studies on Drug-Induced Liver Injury. Am. J. Gastroenterol. 2020. [Google Scholar] [CrossRef]
- Teschke, R.; Eickhoff, A.; Brown, A.C.; Neuman, M.G.; Schulze, J. Diagnostic Biomarkers in Liver Injury by Drugs, Herbs, and Alcohol: Tricky Dilemma after EMA Correctly and Officially Retracted Letter of Support. Int. J. Mol. Sci. 2019, 21, 212. [Google Scholar] [CrossRef] [PubMed]
- Danan, G.; Teschke, R. RUCAM in Drug and Herb Induced Liver Injury: The Update. Int. J. Mol. Sci. 2016, 17, 14. [Google Scholar] [CrossRef]
- Teschke, R. Idiosyncratic DILI: Analysis of 46,266 cases assessed for causality by RUCAM and published from 2014 to early 2019. Front. Pharmacol. 2019, 10, 730. [Google Scholar] [CrossRef]
- Yang, H.; Guo, D.; Xu, Y.; Zhu, M.; Yao, C.; Chen, C.; Jia, W. Comparison of Different Liver Test Thresholds for Drug-Induced Liver Injury: Updated RUCAM versus Other Methods. Front. Pharmacol. 2019, 10, 816. [Google Scholar] [CrossRef]
- Hoofnagle, J.H.; Björnsson, E.S. Drug-Induced Liver Injury—Types and Phenotypes. N. Engl. J. Med. 2019, 381, 264–273. [Google Scholar] [CrossRef]
- Teschke, R.; Eickhoff, A.; Wolff, A.; Xuan, T.D. Liver Injury from Herbs and “Dietary Supplements”: Highlights of a Literature Review from 2015 to 2017. Curr. Pharmacol. Rep. 2018, 4, 120–131. [Google Scholar] [CrossRef]
- Van Quan, N.; Xuan, T.D.; Teschke, R. Potential Hepatotoxins Found in Herbal Medicinal Products: A Systematic Review. Int. J. Mol. Sci. 2020, 21, 5011. [Google Scholar] [CrossRef]
- Danan, G. Consensus meetings on: Causality assessment of drug-induced liver injury. J. Hepatol. 1988, 7, 132–136. [Google Scholar] [CrossRef]
- Bénichou, C. Criteria of drug-induced liver disorders. J. Hepatol. 1990, 11, 272–276. [Google Scholar] [CrossRef]
- Benichou, C.; Danan, G.; Flahault, A. Causality assessment of adverse reactions to drugs—II. An original model for validation of drug causality assessment methods: Case reports with positive rechallenge. J. Clin. Epidemiol. 1993, 46, 1331–1336. [Google Scholar] [CrossRef]
- European Commission. White Paper on Artificial Intelligence—A European Approach to Excellence and Trust, Released 19 February 2020. Available online: https://ec.europa.eu/info/sites/info/files/commission-white-paper-artificial-intelligence-feb2020_en.pdf (accessed on 17 November 2020).
- Hamlet, P.; Tremblay, J. Artificial intelligence in medicine. Metabolism 2017, 69S, S36–S40. [Google Scholar] [CrossRef] [PubMed]
- Mintz, Y.; Brodie, R. Introduction to artificial intelligence in medicine. Minim. Invasive Ther. Allied Technol. 2019, 28, 73–81. [Google Scholar] [CrossRef] [PubMed]
- CB Insights Research. Healthcare Remains the Hottest AI Category for Deals. 2017. Available online: https://www.cbinsights.com/research/artificial-intelligence-healthcare-startups-investors/ (accessed on 17 November 2020).
- Labovitz, D.L.; Shafner, L.; Gil, M.R.; Virmani, D.; Hanina, A. Using Artificial Intelligence to Reduce the Risk of Nonadherence in Patients on Anticoagulation Therapy. Stroke 2017, 48, 1416–1419. [Google Scholar] [CrossRef] [PubMed]
- Mayo, R.C.; Leung, J. Artificial intelligence and deep learning-Radiology’s next frontier? Clin. Imaging 2018, 49, 87–88. [Google Scholar] [CrossRef]
- Bianconi, G.M.; Mehra, R.; Yeung, S.; Salipur, F.; Jopling, J.; Downing, L.; Haque, A.; Alahi, A.; Campbell, B.; Deru, K.; et al. Vision-Based Prediction of ICU Mobility Care Activities Using Recurrent Neural Networks. Machine Learning for Health Workshop, Neural Information Processing Systems (NIPS). 2017. Available online: https://www.gabrielbianconi.com/public/pdf/vision-based-prediction-of-icu-mobility-care-activities-using-recurrent-neural-networks-nips-ml4h-2017.pdf (accessed on 4 March 2021).
- Amisha, P.M.; Pathania, M.; Rathaur, V.K. Overview of artificial intelligence in medicine. J. Fam. Med. Prim. Care 2019, 8, 2328–2331. [Google Scholar] [CrossRef]
- McCarthy, J.; Minsky, M.L.; Rochester, N.; Shannon, C.E. A Proposal for the Dartmouth Summer Research Project on Artificial Intelligence. 1995. Available online: http://www-formal.stanford.edu/jmc/history/dartmouth/dartmouth.html (accessed on 17 November 2020).
- Amato, F.; López, A.; Peña-Méndez, E.M.; Vaňhara, P.; Hampl, A.; Havel, J. Artificial neural networks in medical diagnosis. J. Appl. Biomed. 2013, 11, 47–58. [Google Scholar] [CrossRef]
- Rodgers, M.; Nixon, J.; Hempel, S.; Aho, T.; Kelly, J.; Neal, D.; Duffy, S.; Ritchie, G.; Kleijnen, J.; Westwood, M. Diagnostic tests and algorithms used in the investigation of haematuria: Systematic reviews and economic evaluation. Heal. Technol. Assess. 2006, 10. [Google Scholar] [CrossRef] [PubMed]
- Hennes, E.M.; Zeniya, M.; Czaja, A.J.; Parés, A.; Dalekos, G.N.; Krawitt, E.L.; Bittencourt, P.L.; Porta, G.; Boberg, K.M.; Hofer, H.; et al. Simplified criteria for the diagnosis of autoimmune hepatitis. Hepatology 2008, 48, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Oztekin, A.; Delen, D.; Kong, Z.J. Predicting the graft survival for heart-lung transplantation patients: An integrated data mining methodology. Int. J. Med. Inform. 2009, 78, e84–e96. [Google Scholar] [CrossRef] [PubMed]
- Mistry, P.K.; Cappellini, M.D.; Lukina, E.; Özsan, H.; Pascual, S.M.; Rosenbaum, H.; Solano, M.H.; Spigelman, Z.; Villarrubia, J.; Watman, N.P.; et al. A reappraisal of Gaucher disease-diagnosis and disease management algorithms. Am. J. Hematol. 2011, 86, 110–115. [Google Scholar] [CrossRef]
- Okanobo, H.; Khurana, B.; Sheehan, S.; Duran-Mendicuti, A.; Arianjam, A.; Ledbetter, S. Simplified diagnostic algorithm for Lauge-Hansen classification of ankle injuries. RadioGraphics 2012, 32, E51–E70. [Google Scholar] [CrossRef]
- Ratzinger, F.; Bruckschwaiger, H.; Wischenbart, M.; Parschalk, B.; Fernandez-Reyes, D.; Lagler, H.; Indra, A.; Graninger, W.; Winkler, S.; Krishna, S.; et al. Rapid Diagnostic Algorithms as a Screening Tool for Tuberculosis: An Assessor Blinded Cross-Sectional Study. PLoS ONE 2012, 7, e49658. [Google Scholar] [CrossRef]
- Schirmacher, P.; Calvisi, D.F. Molecular diagnostic algorithms in hepatocellular carcinoma: Dead-end street or light at the end of the tunnel? Gastroenterology 2013, 145, 49–53. [Google Scholar] [CrossRef]
- Di Rocco, M.; Andria, G.; Deodato, F.; Giona, F.; Micalizzi, C.; Pession, A. Early diagnosis of Gaucher disease in pediatric patients: Proposal for a diagnostic algorithm. Pediatr. Blood Cancer 2014, 61, 1905–1909. [Google Scholar] [CrossRef]
- Robles-Diaz, M.; Lucena, M.I.; Kaplowitz, N.; Stephens, C.; Medina-Caliz, I.; Gonzalez-Jiemenez, A.; Ulzurrun, E.; Gonzalez, A.F.; Fernandez, M.C.; Romero-Gomez, M.; et al. Use of Hy´s law and new composite algorithm to predict acute liver failure in patients with drug-induced liver injury. Gastroenterology 2014, 147, 109–118. [Google Scholar] [CrossRef]
- Cervellin, G.; Mattiuzzi, C.; Bovo, C.; Lippi, G. Diagnostic algorithms for acute coronary syndrome—is one better than another? Ann. Transl. Med. 2016, 4, 193. [Google Scholar] [CrossRef] [PubMed]
- Damato, V. Diagnostic algorithms in autoimmune encephalitis. Neuroimmunol. Neuroinflammation 2016, 3, 93. [Google Scholar] [CrossRef][Green Version]
- George, A.; Lim, N.S.; Jain, N.S.; Chong, C.W.K.; Abedi, F.; Liu, Y.; Wang, S.B.; Govendir, M.; Agar, A.; Francis, I.C. “Diagnostic Algorithm for Patients with Suspected Giant Cell Arteritis” Useful, but No Substitute for Thorough Histopathology. J. Neuro-Ophthalmol. 2016, 36, 343. [Google Scholar] [CrossRef] [PubMed]
- Rudnik-Schöneborn, S.; Tölle, D.; Eggermann, K.; Elbracht, M.; Kornak, U.; von der Hagen, M.; Kirschner, J.; Leube, B.; Müller-Felberg, W.; Scharah, U.; et al. Diagnostic algorithms in Charcot-Marie-Tooth neuropathies: Experiences from a German genetic laboratory on the basis of 1206 index patients. Clin. Genet. 2016, 89, 34–43. [Google Scholar] [CrossRef]
- Ghamloush, M.; LeVee, A.; Hill, N.S. The utility of a diagnostic algorithm in cardiopulmonary exercise testing interpretation in patients with exercise intolerance. Am. J. Resp. Crit. Care. Med. 2017, 195, A6257. [Google Scholar]
- Ley, B.; Urbania, T.; Husson, G.; Vittinghoff, E.; Brush, D.R.; Eisner, M.D.; Iribarren, C.; Collard, H.R. Code-based Diagnostic Algorithms for Idiopathic Pulmonary Fibrosis. Case Validation and Improvement. Ann. Am. Thorac. Soc. 2017, 14, 880–887. [Google Scholar] [CrossRef]
- Szendrői, M.; Antal, I.; Szendrői, A.; Lazáry, Á.; Varga, P.P. Diagnostic algorithm, prognostic factors and surgical treatment of metastatic cancer diseases of the long bones and spine. EFORT Open Rev. 2017, 2, 372–381. [Google Scholar] [CrossRef]
- Tran, T.-T.; Fang, T.-Y.; Pham, V.-T.; Lin, C.; Wang, P.-C.; Lo, M.-T. Development of an Automatic Diagnostic Algorithm for Pediatric Otitis Media. Otol. Neurotol. 2018, 39, 1060–1065. [Google Scholar] [CrossRef]
- Wang, H.-Y.; Zu, Y. Diagnostic Algorithm of Common Mature B-Cell Lymphomas by Immunohistochemistry. Arch. Pathol. Lab. Med. 2017, 141, 1236–1246. [Google Scholar] [CrossRef]
- Brandsma, R.; Verschuuren-Bemelmans, C.; Amrom, D.; Barisic, N.; Baxter, P.; Bertini, E.; Blumkin, L.; Brankovic-Sreckovic, V.; Brouwer, O.; Bürk, K.; et al. A clinical diagnostic algorithm for early onset cerebellar ataxia. Eur. J. Paediatr. Neurol. 2019, 23, 692–706. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.Y.; Jung, C.K.; Woo, J.I.; Lee, S.; Cho, J.; Kim, S.W.; Kwak, T.-Y. Artificial Intelligence in Pathology. J. Pathol. Transl. Med. 2019, 53, 1–12. [Google Scholar] [CrossRef]
- Kraus, L.; Kremmyda, O.; Bremova-Ertl, T.; Barceló, S.; Feil, K.; Strupp, M. An algorithm as a diagnostic tool for central ocular motor disorders, also to diagnose rare disorders. Orphanet J. Rare Dis. 2019, 14, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Parkes, M.D.; Aliabadi, A.Z.; Cadeiras, M.; Crespo-Leiro, M.G.; Deng, M.; Depasquale, E.C.; Goekler, J.; Kim, D.H.; Kobashigawa, J.; Loupy, A.; et al. An integrated molecular diagnostic report for heart transplant biopsies using an ensemble of diagnostic algorithms. J. Heart Lung Transpl. 2019, 38, 636–646. [Google Scholar] [CrossRef]
- Pieske, B.; Tschöpe, C.; De Boer, R.A.; Fraser, A.G.; Anker, S.D.; Donal, E.; Edelmann, F.; Fu, M.; Guazzi, M.; Lam, C.S.P.; et al. How to diagnose heart failure with preserved ejection fraction: The HFA–PEFF diagnostic algorithm: A consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur. Heart J. 2019, 40, 3297–3317. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Fouayzi, H.; Anzuoni, K.; Goldman, L.; Min, J.Y.; Griffin, M.; Grijalva, C.G.; Morrow, J.A.; Whitmore, C.C.; Leonard, C.E.; et al. Diagnostic Algorithms for Cardiovascular Death in Administrative Claims Databases: A Systematic Review. Drug Saf. 2018, 42, 515–527. [Google Scholar] [CrossRef] [PubMed]
- Valent, P.; Akin, C.; Bonadonna, P.; Hartmann, K.; Brockow, K.; Niedoszytko, M.; Nedoszytko, B.; Siebenhaar, F.; Sperr, W.R.; Elberink, J.N.O.; et al. Proposed Diagnostic Algorithm for Patients with Suspected Mast Cell Activation Syndrome. J. Allergy Clin. Immunol. Pract. 2019, 7, 1125–1133.e1. [Google Scholar] [CrossRef]
- Kamdar, J.H.; Praba, J.J.; Georrge, J.J. Artificial Intelligence in Medical Diagnosis: Methods, Algorithms and Applications. In Learning and Analytics in Intelligent Systems; Springer International Publishing: Berlin/Heidelberg, Germany, 2020; Volume 13, pp. 27–37. [Google Scholar]
- Pokharel, S.; White, L.J.; Aguas, R.; Celhay, O.; Pellé, K.G.; Dittrich, S. Algorithm in the Diagnosis of Febrile Illness Using Pathogen-specific Rapid Diagnostic Tests. Clin. Infect. Dis. 2020, 70, 2262–2269. [Google Scholar] [CrossRef] [PubMed]
- Danan, G.; Teschke, R. Drug-Induced Liver Injury: Why is the Roussel Uclaf Causality Assessment Method (RUCAM) Still Used 25 Years After Its Launch? Drug Saf. 2018, 41, 735–743. [Google Scholar] [CrossRef]
- Danan, G.; Teschke, R. Roussel Uclaf Causality Assessment Method for Drug-Induced Liver Injury: Present and Future. Front. Pharmacol. 2019, 10, 853. [Google Scholar] [CrossRef]
- Teschke, R.; Danan, G. Causality Assessment Methods in Drug-Induced Liver Injury; Springer International Publishing: Berlin/Heidelberg, Germany, 2018; pp. 555–594. [Google Scholar]
- Sarges, P.; Steinberg, J.M.; Lewis, J.H. Drug-Induced Liver Injury: Highlights from a Review of the 2015 Literature. Drug Saf. 2016, 39, 801–821. [Google Scholar] [CrossRef]
- Shahbaz, O.; Mahajan, S.; Lewis, J.H. Highlights of drug- and herb- induced liver injury in the literature from 2016: How best to translate new information into clinical practice? Expert Opin. Drug Metab. Toxicol. 2017, 13, 935–951. [Google Scholar] [CrossRef]
- Chen, F.; Chen, W.; Chen, J.; Xu, D.; Xie, W.; Wang, X.; Xie, Y. Clinical features and risk factors of COVID-19-associated liver injury and function: A retrospective analysis of 830 cases. Ann. Hepatol. 2021, 21, 100267. [Google Scholar] [CrossRef]
- Jiang, S.; Wang, R.; Li, L.; Hong, D.; Ru, R.; Rao, Y.; Miao, J.; Chen, N.; Wu, X.; Ye, Z.; et al. Liver Injury in Critically Ill and Non-critically Ill COVID-19 Patients: A Multicenter, Retrospective, Observational Study. Front. Med. 2020, 7, 347. [Google Scholar] [CrossRef] [PubMed]
- Muhović, D.; Bojović, J.; Bulatović, A.; Vukčević, B.; Ratković, M.; Lazović, R.; Smolović, B. First case of drug-induced liver injury associated with the use of tocilizumab in a patient with COVID-19. Liver Int. 2020, 40, 1901–1905. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Liu, J.; Lu, M.; Yang, D.; Zheng, X. Liver injury during highly pathogenic human coronavirus infections. Liver Int. 2020, 40, 998–1004. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Shi, L.; Wang, F.-S. Liver injury in COVID-19: Management and challenges. Lancet Gastroenterol. Hepatol. 2020, 5, 428–430. [Google Scholar] [CrossRef]
- Guo, T.; Shen, Q.; Guo, W.; He, W.; Li, J.; Zhang, Y.; Wang, Y.; Zhou, Z.; Deng, D.; Ouyang, X.; et al. Clinical Characteristics of Elderly Patients with COVID-19 in Hunan Province, China: A Multicenter, Retrospective Study. Gerontology 2020, 66, 467–475. [Google Scholar] [CrossRef] [PubMed]
- Méndez-Sánchez, N.; Valencia-Rodríguez, A.; Qi, X.; Yoshida, E.M.; Romero-Gómez, M.; George, J.; Eslam, M.; Abenavoli, L.; Xie, W.; Teschke, R.; et al. What Has the COVID-19 Pandemic Taught Us so Far? Addressing the Problem from a Hepatologist’s Perspective. J. Clin. Transl. Hepatol. 2020, 8, 109–112. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, E.M.; Hussaini, T.; Alsahafi, M. COVID-19 in gastroenterology and hepatology: Living with the realities of a historic 21st century pandemic. Saudi J. Gastroenterol. 2020, 26, 223–225. [Google Scholar] [CrossRef] [PubMed]
- Marshall, M. How COVID-19 can damage the brain. Nat. Cell Biol. 2020, 585, 342–343. [Google Scholar] [CrossRef] [PubMed]
- Kostoff, R.N.; Briggs, M.B.; Porter, A.L.; Hernández, A.F.; Abdollahi, M.; Aschner, M.; Tsatsakis, A. The under-reported role of toxic substance exposures in the COVID-19 pandemic. Food Chem. Toxicol. 2020, 145, 111687. [Google Scholar] [CrossRef] [PubMed]
- da Silva, L.M.; Simonato, L.M.; Ramos, R.R. Phylogeny and pathogenesis of SARS-CoV-2: A systematic study. J. Mod. Med. Chem. 2020, 8, 49–55. [Google Scholar] [CrossRef]
- Teschke, R.; Andrade, R.J. Drug-Induced Liver Injury: Expanding Our Knowledge by Enlarging Population Analysis with Prospective and Scoring Causality Assessment. Gastroenterology 2015, 148, 1271–1273. [Google Scholar] [CrossRef]
| Mechanistic Background | Thresholds of Liver Tests | Criteria and Characteristic Features | Recommended Description |
|---|---|---|---|
| Adaptive | ALT ≤ 5 × ULN ALP ≤ 2 × ULN |
| Liver adaptation |
| Idiosyncratic | ALT ≥ 5 × ULN ALP ≥ 2 × ULN |
| Idiosyncratic DILI |
| Intrinsic | ALT ≥ 5 × ULN ALP ≥ 2 × ULN |
| Intrinsic DILI |
| Reporting Country | Year of Publication | Diseases and Applications | First Author |
|---|---|---|---|
| France | 1993 | DILI and RUCAM | Danan [4] |
| France | 1993 | DILI and RUCAM | Bénichou [26] |
| UK | 2006 | Haematuria | Rodgers [37] |
| Germany | 2008 | Autoimmune hepatitis | Hennes [38] |
| US | 2009 | Heart-lung transplantation | Oztekin [39] |
| US | 2011 | Gaucher disease | Mistry [40] |
| US | 2012 | Ankle injuries | Okanobo [41] |
| Austria | 2012 | Tuberculosis | Ratzinger [42] |
| Germany | 2013 | Hepatocellular carcinoma | Schirmacher [43] |
| Italy | 2014 | Gaucher disease | Di Rocco [44] |
| Spain | 2014 | DILI, RUCAM, and acute liver failure | Robles-Diaz [45] |
| Italy | 2016 | Acute coronary syndrome | Cervellin [46] |
| Italy | 2016 | Autoimmune encephalitis | Damato [47] |
| Australia | 2016 | Giant cell arteritis | George [48] |
| Germany | 2016 | Charcot–Marie–Tooth neuropathies | Rudnik-Schöneborn [49] |
| US | 2017 | Cardiopulmonary diseases | Ghamloush [50] |
| US | 2017 | Cardiopulmonary diseases | Ley [51] |
| Hungary | 2017 | Osseous metastatic cancer diseases | Szendrői [52] |
| China | 2018 | Pediatric otitis media | Tran [53] |
| US | 2018 | B-cell lymphomas | Wang [54] |
| Netherlands | 2019 | Cerebellar ataxia | Brandsma [55] |
| Korea | 2019 | Pathology diagnostics | Chang [56] |
| Germany | 2019 | Central ocular motor disorders | Kraus [57] |
| Canada | 2019 | Heart transplantation | Parkes [58] |
| Germany | 2019 | Heart failure | Pieske [59] |
| US | 2019 | Cardiovascular diseases | Singh [60] |
| Austria | 2019 | Mast cell activation syndrome | Valent [61] |
| India | 2020 | Various | Kamdar [62] |
| UK | 2020 | Febrile illnesses | Pokharel [63] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Teschke, R.; Danan, G. Idiosyncratic Drug-Induced Liver Injury (DILI) and Herb-Induced Liver Injury (HILI): Diagnostic Algorithm Based on the Quantitative Roussel Uclaf Causality Assessment Method (RUCAM). Diagnostics 2021, 11, 458. https://doi.org/10.3390/diagnostics11030458
Teschke R, Danan G. Idiosyncratic Drug-Induced Liver Injury (DILI) and Herb-Induced Liver Injury (HILI): Diagnostic Algorithm Based on the Quantitative Roussel Uclaf Causality Assessment Method (RUCAM). Diagnostics. 2021; 11(3):458. https://doi.org/10.3390/diagnostics11030458
Chicago/Turabian StyleTeschke, Rolf, and Gaby Danan. 2021. "Idiosyncratic Drug-Induced Liver Injury (DILI) and Herb-Induced Liver Injury (HILI): Diagnostic Algorithm Based on the Quantitative Roussel Uclaf Causality Assessment Method (RUCAM)" Diagnostics 11, no. 3: 458. https://doi.org/10.3390/diagnostics11030458
APA StyleTeschke, R., & Danan, G. (2021). Idiosyncratic Drug-Induced Liver Injury (DILI) and Herb-Induced Liver Injury (HILI): Diagnostic Algorithm Based on the Quantitative Roussel Uclaf Causality Assessment Method (RUCAM). Diagnostics, 11(3), 458. https://doi.org/10.3390/diagnostics11030458