Structured Reporting in the Characterization of Renal Cysts by Contrast-Enhanced Ultrasound (CEUS) Using the Bosniak Classification System—Improvement of Report Quality and Interdisciplinary Communication
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Sample Size Calculation
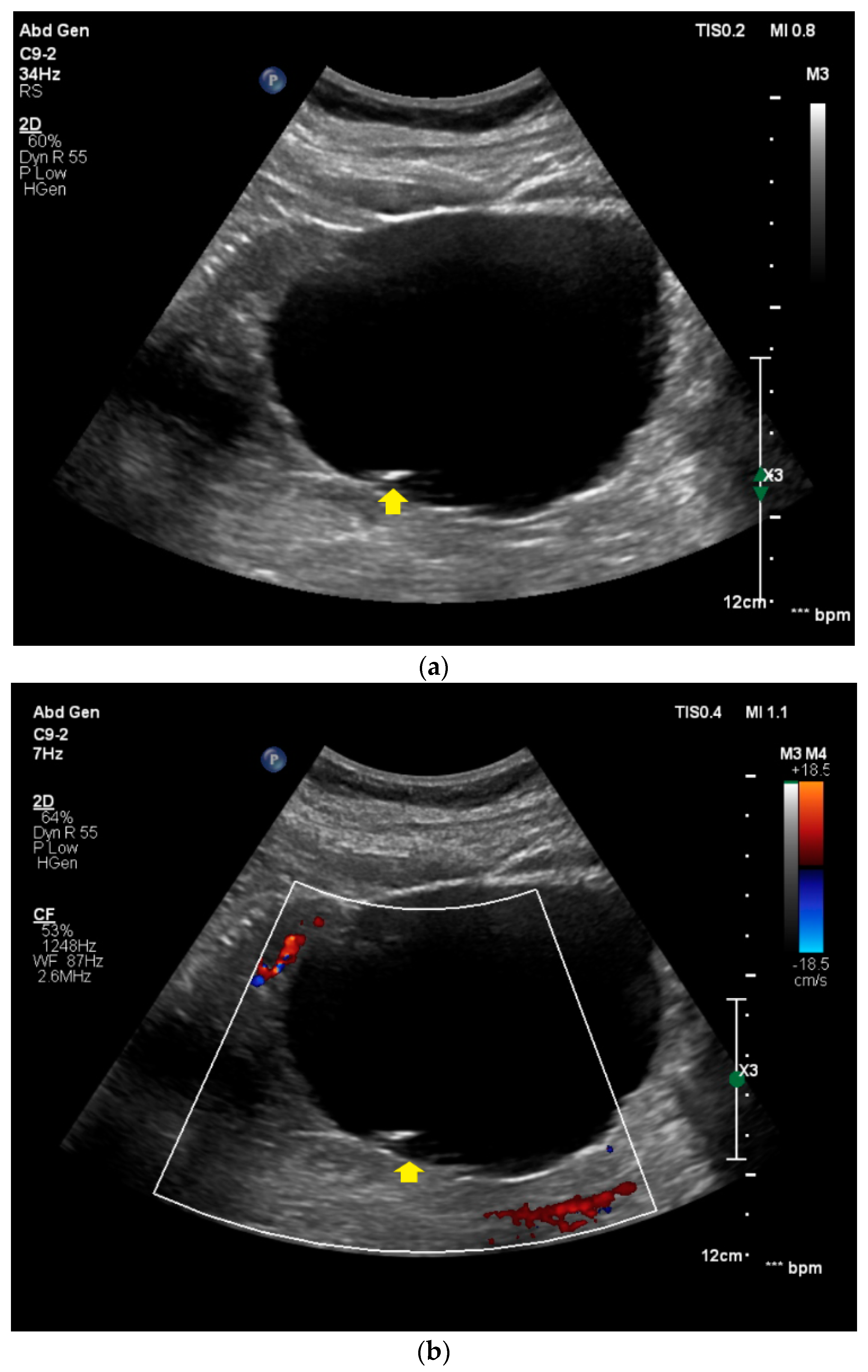
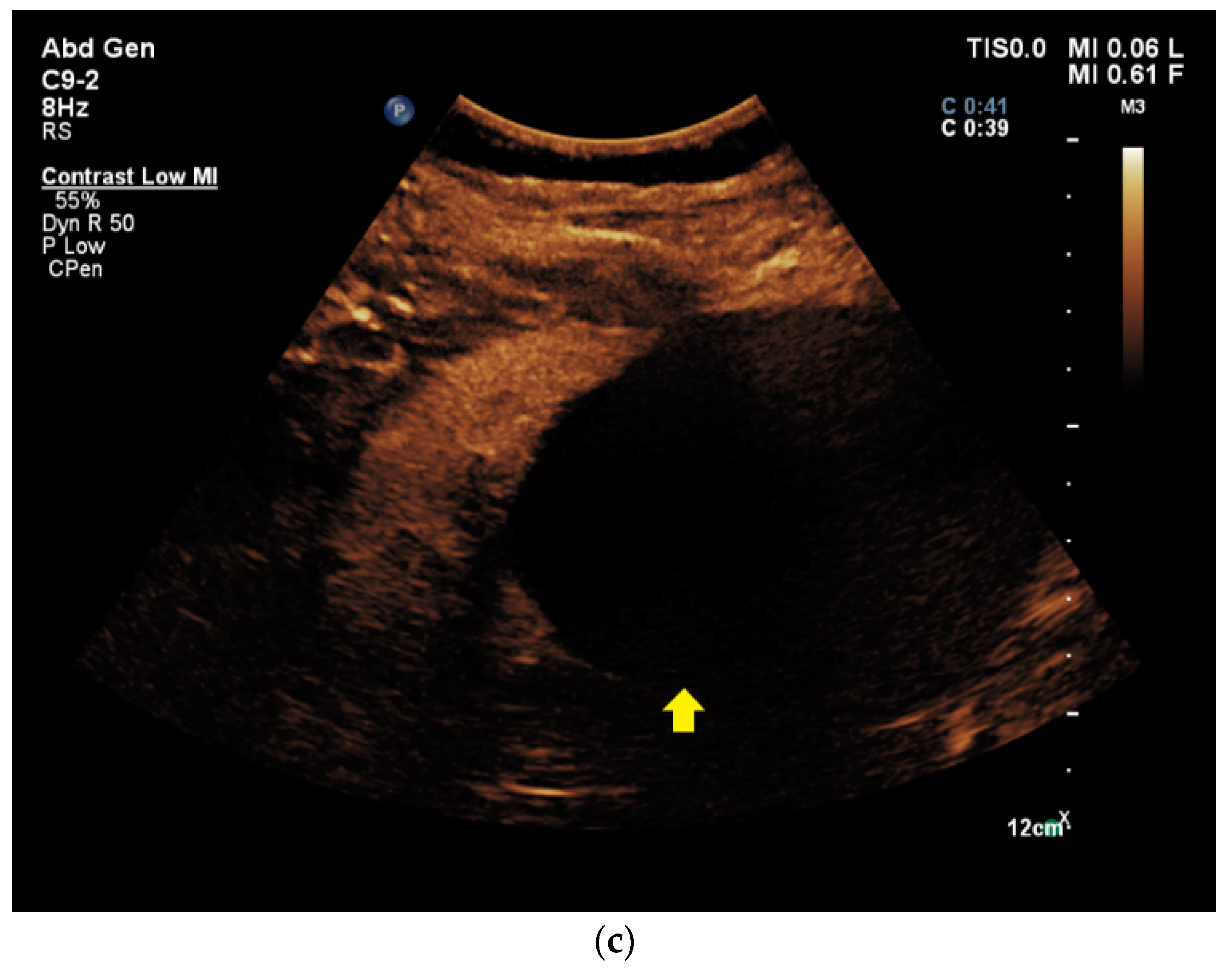
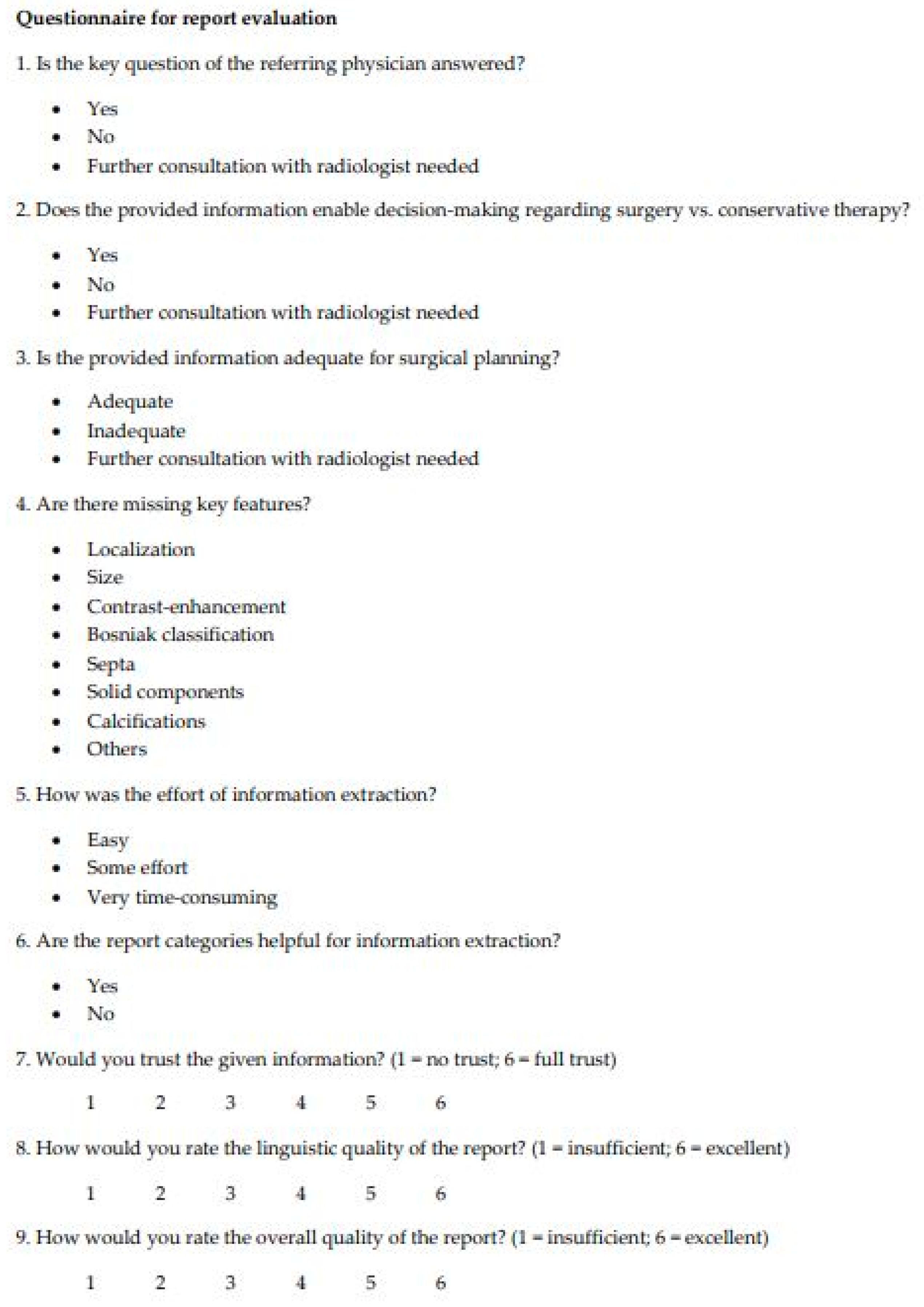
2.3. Image Acquisition and Generation of Free-Text Reports
2.4. Generation of Structured Reports
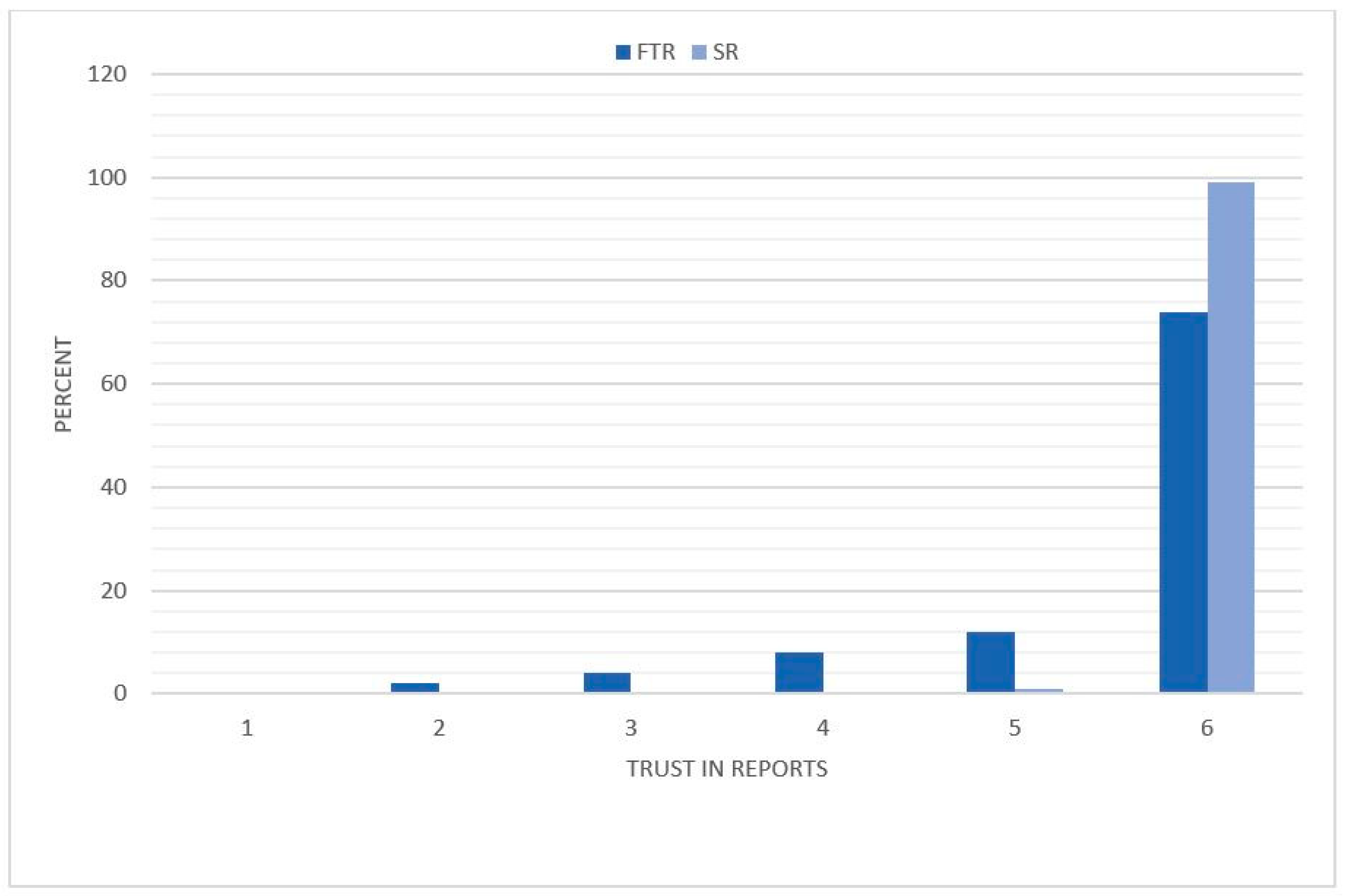
2.5. Evaluation of CEUS Reports
2.6. Statistical Analysis
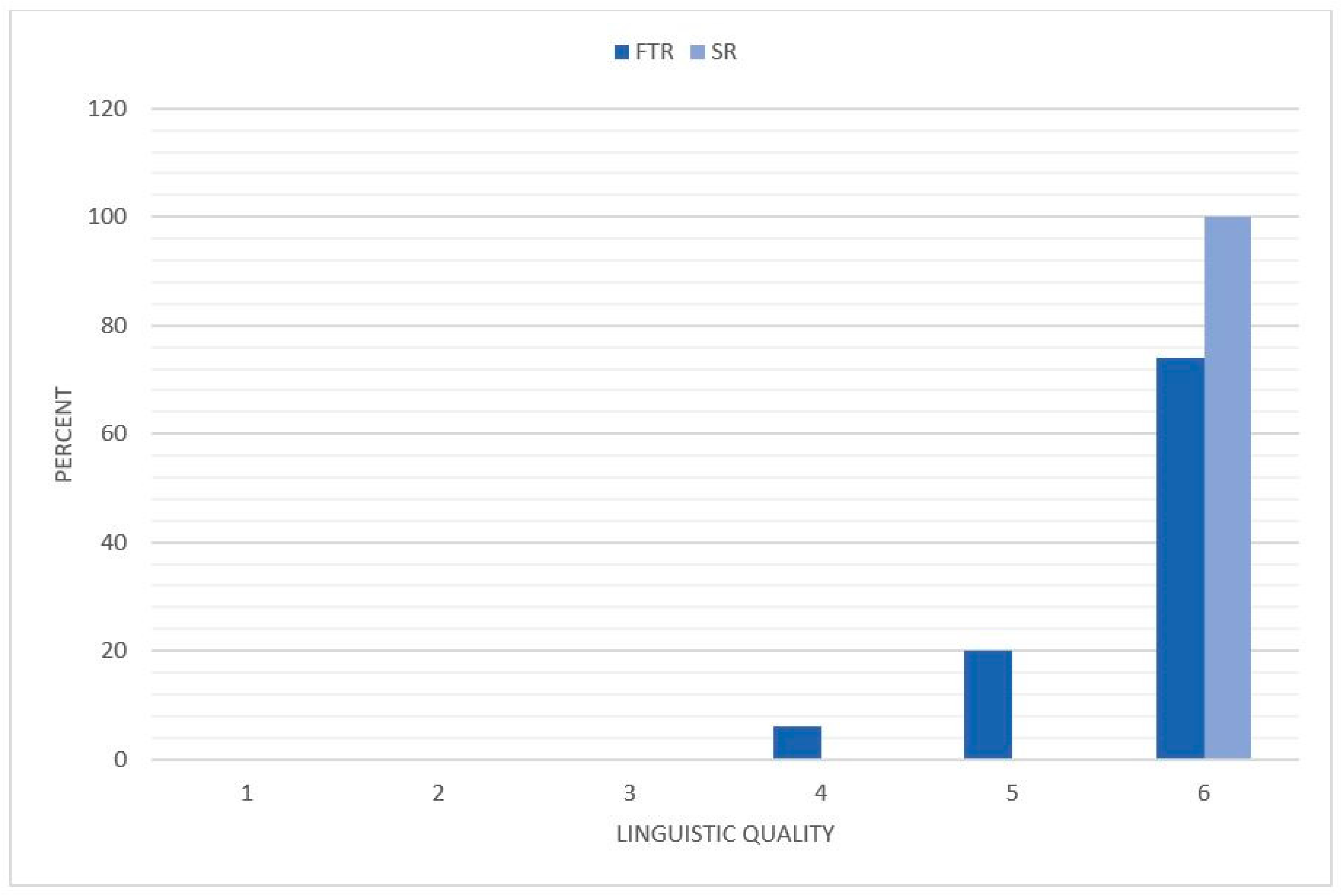
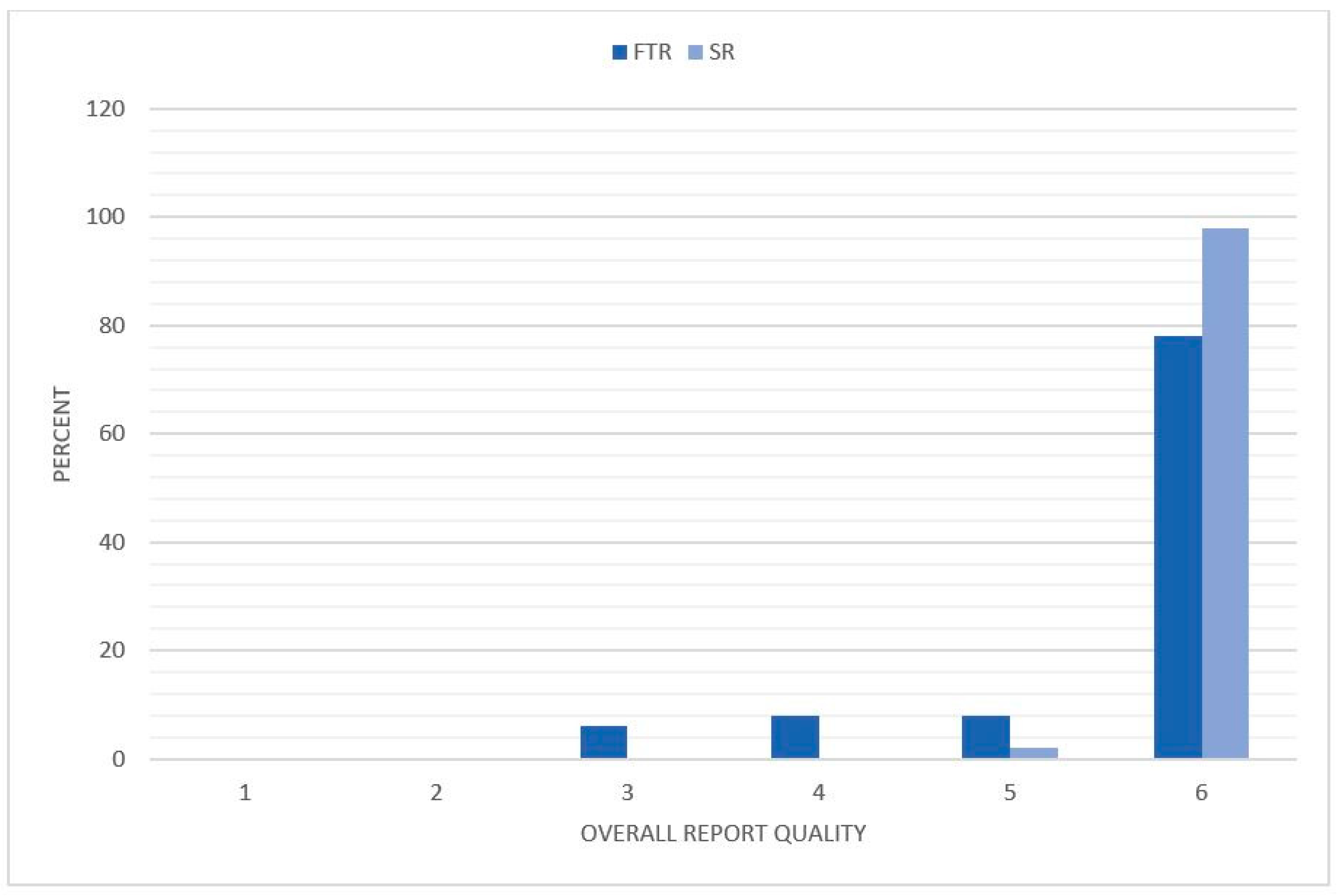
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Bosniak, M.A. Problems in the radiologic diagnosis of renal parenchymal tumors. Urol. Clin. N. Am. 1993, 20, 217–230. [Google Scholar]
- Seppala, N.; Kielar, A.; Dabreo, D.; Duigenan, S. Inter-rater agreement in the characterization of cystic renal lesions on contrast-enhanced MRI. Abdom Imaging 2014, 39, 1267–1273. [Google Scholar] [CrossRef]
- Warren, K.S.; McFarlane, J. The Bosniak classification of renal cystic masses. BJU Int. 2005, 95, 939–942. [Google Scholar] [CrossRef] [PubMed]
- Bosniak, M.A. The current radiological approach to renal cysts. Radiology 1986, 158, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Curry, N.S.; Cochran, S.T.; Bissada, N.K. Cystic renal masses: Accurate Bosniak classification requires adequate renal CT. AJR Am. J. Roentgenol. 2000, 175, 339–342. [Google Scholar] [CrossRef] [PubMed]
- Hartman, D.S.; Choyke, P.L.; Hartman, M.S. From the RSNA refresher courses: A practical approach to the cystic renal mass. Radiographics 2004, 24 (Suppl. 1), S101–S115. [Google Scholar] [CrossRef] [PubMed]
- Silverman, S.G.; Pedrosa, I.; Ellis, J.H.; Hindman, N.M.; Schieda, N.; Smith, A.D.; Remer, E.M.; Shinagare, A.B.; Curci, N.E.; Raman, S.S.; et al. Bosniak Classification of Cystic Renal Masses, Version 2019: An Update Proposal and Needs Assessment. Radiology 2019, 292, 475–488. [Google Scholar] [CrossRef] [PubMed]
- Edenberg, J.; Gloersen, K.; Osman, H.A.; Dimmen, M.; Berg, G.V. The role of contrast-enhanced ultrasound in the classification of CT-indeterminate renal lesions. Scand. J. Urol. 2016, 50, 445–451. [Google Scholar] [CrossRef] [PubMed]
- Chang, E.H.; Chong, W.K.; Kasoji, S.K.; Dayton, P.A.; Rathmell, W.K. Management of Indeterminate Cystic Kidney Lesions: Review of Contrast-enhanced Ultrasound as a Diagnostic Tool. Urology 2016, 87, 1–10. [Google Scholar] [CrossRef]
- Rubenthaler, J.; Bogner, F.; Reiser, M.; Clevert, D.A. Contrast-Enhanced Ultrasound (CEUS) of the Kidneys by Using the Bosniak Classification. Ultraschall Med. 2016, 37, 234–251. [Google Scholar] [CrossRef]
- Schwarze, V.; Rübenthaler, J.; Čečatka, S.; Marschner, C.; Froelich, M.F.; Sabel, B.O.; Staehler, M.; Knösel, T.; Geyer, T.; Clevert, D.A. Contrast-Enhanced Ultrasound (CEUS) for the Evaluation of Bosniak III Complex Renal Cystic Lesions-A 10-Year Specialized European Single-Center Experience with Histopathological Validation. Medicina 2020, 56, 692. [Google Scholar] [CrossRef] [PubMed]
- Piscaglia, F.; Bolondi, L.; Italian Society for Ultrasound in Medicine and Biology (SIUMB) Study Group on Ultrasound Contrast Agents. The safety of Sonovue in abdominal applications: Retrospective analysis of 23188 investigations. Ultrasound Med. Biol. 2006, 32, 1369–1375. [Google Scholar] [CrossRef] [PubMed]
- Schwarze, V.; Marschner, C.; Negrão de Figueiredo, G.; Rübenthaler, J.; Clevert, D.A. Single-Center Study: Evaluating the Diagnostic Performance and Safety of Contrast-Enhanced Ultrasound (CEUS) in Pregnant Women to Assess Hepatic Lesions. Ultraschall Med. 2020, 41, 29–35. [Google Scholar] [CrossRef]
- Geyer, T.; Rübenthaler, J.; Froelich, M.F.; Sabel, L.; Marschner, C.; Schwarze, V.; Clevert, D.A. Contrast-Enhanced Ultrasound for Assessing Abdominal Conditions in Pregnancy. Medicina 2020, 56, 675. [Google Scholar] [CrossRef] [PubMed]
- Schwarze, V.; Froelich, M.F.; Marschner, C.; Knösel, T.; Rübenthaler, J.; Clevert, D.A. Safe and pivotal approaches using contrast-enhanced ultrasound for the diagnostic workup of non-obstetric conditions during pregnancy, a single-center experience. Arch. Gynecol. Obstet. 2020, 1–10. [Google Scholar] [CrossRef]
- Gunderman, R.B.; McNeive, L.R. Is structured reporting the answer? Radiology 2014, 273, 7–9. [Google Scholar] [CrossRef]
- European Society of Radiology. Good practice for radiological reporting. Guidelines from the European Society of Radiology (ESR). Insights Imaging 2011, 2, 93–96. [Google Scholar] [CrossRef]
- Morgan, T.A.; Helibrun, M.E.; Kahn, C.E., Jr. Reporting initiative of the Radiological Society of North America: Progress and new directions. Radiology 2014, 273, 642–645. [Google Scholar] [CrossRef]
- Dunnick, N.R.; Langlotz, C.P. The radiology report of the future: A summary of the 2007 Intersociety Conference. J. Am. Coll. Radiol. 2008, 5, 626–629. [Google Scholar] [CrossRef]
- Ernst, B.P.; Hodeib, M.; Strieth, S.; Kunzel, J.; Bischof, F.; Hackenberg, B.; Huppertz, T.; Weber, V.; Bahr, K.; Eckrich, J.; et al. Structured reporting of head and neck ultrasound examinations. BMC Med. Imaging 2019, 19, 25. [Google Scholar] [CrossRef]
- Sabel, B.O.; Plum, J.L.; Kneidinger, N.; Leuschner, G.; Koletzko, L.; Raziorrouh, B.; Schinner, R.; Kunz, W.G.; Schoeppe, F.; Thierfelder, K.M.; et al. Structured reporting of CT examinations in acute pulmonary embolism. J. Cardiovasc. Comput. Tomogr. 2017, 11, 188–195. [Google Scholar] [CrossRef]
- Norenberg, D.; Sommer, W.H.; Thasler, W.; D’Haese, J.; Rentsch, M.; Kolben, T.; Schreyer, A.; Rist, C.; Reiser, M.; Armbruster, M. Structured Reporting of Rectal Magnetic Resonance Imaging in Suspected Primary Rectal Cancer: Potential Benefits for Surgical Planning and Interdisciplinary Communication. Investig. Radiol. 2017, 52, 232–239. [Google Scholar] [CrossRef] [PubMed]
- Gassenmaier, S.; Armbruster, M.; Haasters, F.; Helfen, T.; Henzler, T.; Alibek, S.; Pforringer, D.; Sommer, W.H.; Sommer, N.N. Structured reporting of MRI of the shoulder—Improvement of report quality? Eur. Radiol. 2017, 27, 4110–4119. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Sobez, L.M.; Spiro, J.E.; Curta, A.; Ceelen, F.; Kampmann, E.; Goepfert, M.; Bodensohn, R.; Meinel, F.G.; Sommer, W.H.; et al. Structured reporting has the potential to reduce reporting times of dual-energy x-ray absorptiometry exams. BMC Musculoskelet. Disord. 2020, 21, 248. [Google Scholar] [CrossRef] [PubMed]
- Sahni, V.A.; Silveira, P.C.; Sainani, N.I.; Khorasani, R. Impact of a Structured Report Template on the Quality of MRI Reports for Rectal Cancer Staging. AJR Am. J. Roentgenol. 2015, 205, 584–588. [Google Scholar] [CrossRef] [PubMed]
- Schoeppe, F.; Sommer, W.H.; Norenberg, D.; Verbeek, M.; Bogner, C.; Westphalen, C.B.; Dreyling, M.; Rummeny, E.J.; Fingerle, A.A. Structured reporting adds clinical value in primary CT staging of diffuse large B-cell lymphoma. Eur. Radiol. 2018, 28, 3702–3709. [Google Scholar] [CrossRef]
- Ernst, B.P.; Katzer, F.; Künzel, J.; Hodeib, M.; Strieth, S.; Eckrich, J.; Tattermusch, A.; Froelich, M.F.; Matthias, C.; Sommer, W.H.; et al. Impact of structured reporting on developing head and neck ultrasound skills. BMC Med. Educ. 2019, 19, 102. [Google Scholar] [CrossRef]
- Rübenthaler, J.; Negrão de Figueiredo, G.; Mueller-Peltzer, K.; Clevert, D.A. Evaluation of renal lesions using contrast-enhanced ultrasound (CEUS); a 10-year retrospective European single-centre analysis. Eur. Radiol. 2018, 28, 4542–4549. [Google Scholar] [CrossRef] [PubMed]
- Bertolotto, M.; Cicero, C.; Perrone, R.; Degrassi, F.; Cacciato, F.; Cova, M.A. Renal Masses With Equivocal Enhancement at CT: Characterization With Contrast-Enhanced Ultrasound. AJR Am. J. Roentgenol. 2015, 204, W557–W565. [Google Scholar] [CrossRef] [PubMed]
- Schwarze, V.; Rübenthaler, J.; Marschner, C.; Fabritius, M.P.; Rueckel, J.; Fink, N.; Puhr-Westerheide, D.; Gresser, E.; Froelich, M.F.; Schnitzer, M.L.; et al. Advanced Fusion Imaging and Contrast-Enhanced Imaging (CT/MRI-CEUS) in Oncology. Cancers 2020, 12, 2821. [Google Scholar] [CrossRef] [PubMed]
- Ascenti, G.; Mazziotti, S.; Zimbaro, G.; Settineri, N.; Magno, C.; Melloni, D.; Caruso, R.; Scribano, E. Complex cystic renal masses: Characterization with contrast-enhanced US. Radiology 2007, 243, 158–165. [Google Scholar] [CrossRef]
- Chen, Y.; Wu, N.; Xue, T.; Hao, Y.; Dai, J. Comparison of contrast-enhanced sonography with MRI in the diagnosis of complex cystic renal masses. J. Clin. Ultrasound 2015, 43, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Cantisani, V.; Bertolotto, M.; Clevert, D.A.; Correas, J.M.; Drudi, F.M.; Fischer, T.; Gilja, O.H.; Granata, A.; Graumann, O.; Harvey, C.J.; et al. EFSUMB 2020 Proposal for a Contrast-Enhanced Ultrasound-Adapted Bosniak Cyst Categorization - Position Statement. Ultraschall Med. 2020. [Google Scholar] [CrossRef]
- Bai, X.; Sun, S.M.; Xu, W.; Kang, H.H.; Li, L.; Jin, Y.Q.; Gong, Q.G.; Liang, G.C.; Liu, H.Y.; Liu, L.L.; et al. MRI-based Bosniak Classification of Cystic Renal Masses, Version 2019: Interobserver Agreement, Impact of Readers’ Experience, and Diagnostic Performance. Radiology 2020, 297, 597–605. [Google Scholar] [CrossRef]
- Schöppe, F.; Sommer, W.H.; Schmidutz, F.; Pförringer, D.; Armbruster, M.; Paprottka, K.J.; Plum, J.L.V.; Sabel, B.O.; Meinel, F.G.; Sommer, N.N. Structured reporting of x-rays for atraumatic shoulder pain: Advantages over free text? BMC Med. Imaging 2018, 18, 20. [Google Scholar] [CrossRef]
- Lambin, P.; Leijenaar, R.T.H.; Deist, T.M.; Peerlings, J.; de Jong, E.E.C.; van Timmeren, J.; Sanduleanu, S.; Larue, R.; Even, A.J.G.; Jochems, A.; et al. Radiomics: The bridge between medical imaging and personalized medicine. Nat. Rev. Clin. Oncol. 2017, 14, 749–762. [Google Scholar] [CrossRef] [PubMed]
- Pinto Dos Santos, D.; Baeßler, B. Big data, artificial intelligence, and structured reporting. Eur. Radiol. Exp. 2018, 2, 42. [Google Scholar] [CrossRef] [PubMed]
- Bosmans, J.M.; Neri, E.; Ratib, O.; Kahn, C.E., Jr. Structured reporting: A fusion reactor hungry for fuel. Insights Imaging 2015, 6, 129–132. [Google Scholar] [CrossRef]
- Johnson, A.J.; Chen, M.Y.; Swan, J.S.; Applegate, K.E.; Littenberg, B. Cohort study of structured reporting compared with conventional dictation. Radiology 2009, 253, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Kohli, M.; Prevedello, L.M.; Filice, R.W.; Geis, J.R. Implementing Machine Learning in Radiology Practice and Research. AJR Am. J. Roentgenol. 2017, 208, 754–760. [Google Scholar] [CrossRef]
- Rubin, D.L.; Kahn, C.E., Jr. Common Data Elements in Radiology. Radiology 2017, 283, 837–844. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schnitzer, M.L.; Sabel, L.; Schwarze, V.; Marschner, C.; Froelich, M.F.; Nuhn, P.; Falck, Y.; Nuhn, M.-M.; Afat, S.; Staehler, M.; et al. Structured Reporting in the Characterization of Renal Cysts by Contrast-Enhanced Ultrasound (CEUS) Using the Bosniak Classification System—Improvement of Report Quality and Interdisciplinary Communication. Diagnostics 2021, 11, 313. https://doi.org/10.3390/diagnostics11020313
Schnitzer ML, Sabel L, Schwarze V, Marschner C, Froelich MF, Nuhn P, Falck Y, Nuhn M-M, Afat S, Staehler M, et al. Structured Reporting in the Characterization of Renal Cysts by Contrast-Enhanced Ultrasound (CEUS) Using the Bosniak Classification System—Improvement of Report Quality and Interdisciplinary Communication. Diagnostics. 2021; 11(2):313. https://doi.org/10.3390/diagnostics11020313
Chicago/Turabian StyleSchnitzer, Moritz L., Laura Sabel, Vincent Schwarze, Constantin Marschner, Matthias F. Froelich, Philipp Nuhn, Yannick Falck, Maria-Magdalena Nuhn, Saif Afat, Michael Staehler, and et al. 2021. "Structured Reporting in the Characterization of Renal Cysts by Contrast-Enhanced Ultrasound (CEUS) Using the Bosniak Classification System—Improvement of Report Quality and Interdisciplinary Communication" Diagnostics 11, no. 2: 313. https://doi.org/10.3390/diagnostics11020313
APA StyleSchnitzer, M. L., Sabel, L., Schwarze, V., Marschner, C., Froelich, M. F., Nuhn, P., Falck, Y., Nuhn, M.-M., Afat, S., Staehler, M., Rückel, J., Clevert, D.-A., Rübenthaler, J., & Geyer, T. (2021). Structured Reporting in the Characterization of Renal Cysts by Contrast-Enhanced Ultrasound (CEUS) Using the Bosniak Classification System—Improvement of Report Quality and Interdisciplinary Communication. Diagnostics, 11(2), 313. https://doi.org/10.3390/diagnostics11020313






