A Growth Differentiation Factor 15-Based Risk Score Model to Predict Mortality in Hemodialysis Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants in the Cohort
2.2. Assessment of Exposures
2.3. Assessment of Covariates
2.4. Ascertainment of Outcomes
2.5. Statistical Analysis
3. Results
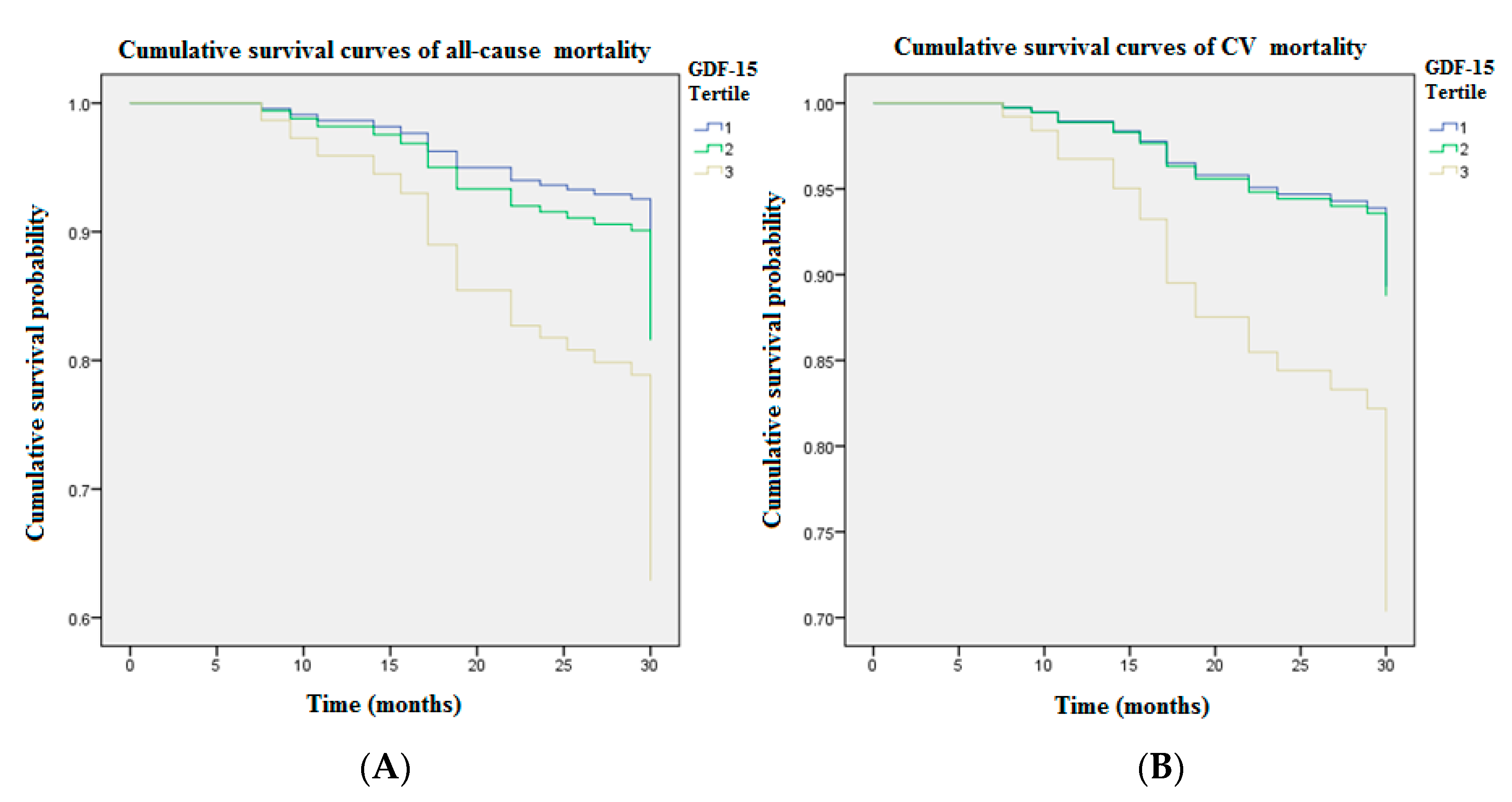
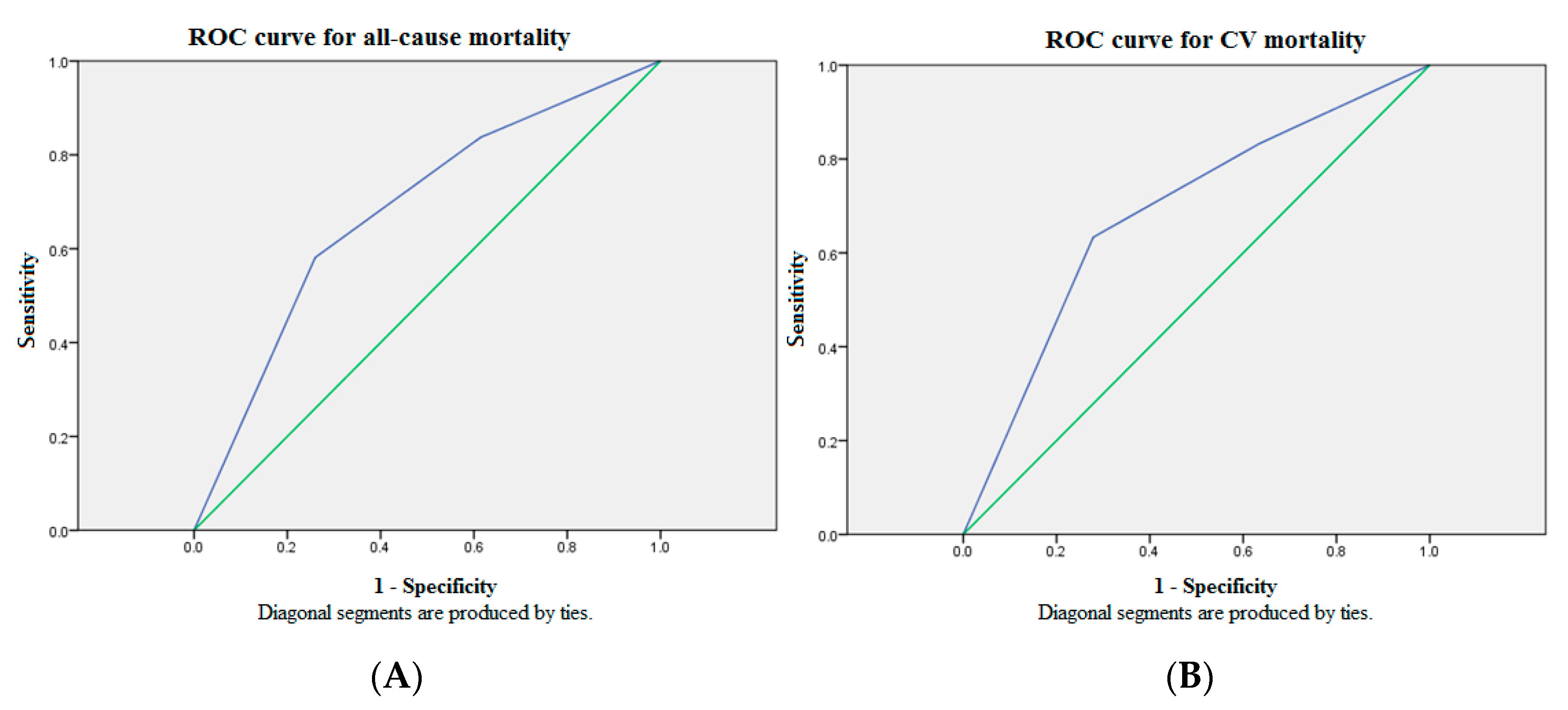
3.1. Primary Analyses: Evaluation of the Clinical Candidate Predictors
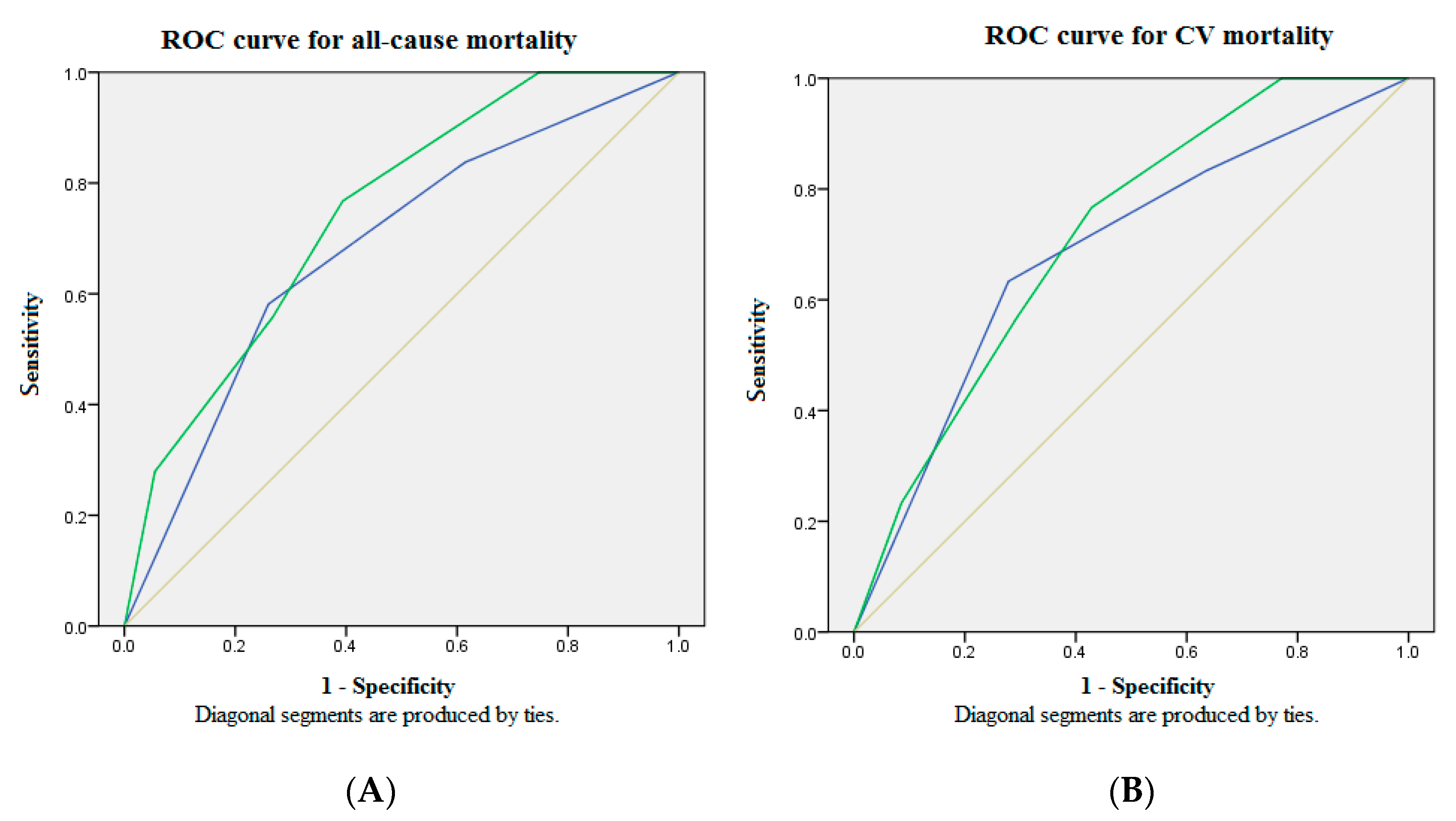
3.2. Secondary Analyses: Evaluation of the GDF15-Based Death Prediction Model
4. Discussion
5. Conclusions
Abbreviation
| aHRs | adjusted hazard ratios |
| AI | artificial intelligence |
| ALT | Alanine aminotransferase |
| AST | aspartate aminotransferase |
| AUC | area under ROC curve |
| BUN | blood urea nitrogen |
| CI | confidence interval |
| CKD | chronic kidney disease |
| Ca-P | Calcium-phosphate |
| CV | cardiovascular |
| CVD | cardiovascular diseases |
| DBP | Diastolic blood pressure |
| DM | Diabetes mellitus |
| GDF15 | growth differentiation factor-15 |
| HD | Hemodialysis |
| iPTH | intact parathyroid hormone |
| LDL | Low-density lipoprotein |
| MHD | maintenance hemodialysis |
| nPCR | normalized protein catabolic rate |
| ROC | receiver operating characteristic |
| SBP | Systolic blood pressure |
| T-Cholesterol | Total Cholesterol |
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ko, W.-C.; Choy, C.-S.; Lin, W.-N.; Chang, S.-W.; Liou, J.-C.; Tung, T.-H.; Hsieh, C.-Y.; Chang, J.-F. Galectin-3 Interacts with Vascular Cell Adhesion Molecule-1 to Increase Cardiovascular Mortality in Hemodialysis Patients. J. Clin. Med. 2018, 7, 300. [Google Scholar] [CrossRef] [PubMed]
- Mihai, S.; Codrici, E.; Popescu, I.D.; Enciu, A.-M.; Albulescu, L.; Necula, L.G.; Mambet, C.; Anton, G.; Tanase, C. Inflammation-Related Mechanisms in Chronic Kidney Disease Prediction, Progression, and Outcome. J. Immunol. Res. 2018, 2018, 2180373. [Google Scholar] [CrossRef]
- Chang, J.-F.; Chou, Y.-S.; Wu, C.-C.; Chen, P.-C.; Ko, W.-C.; Liou, J.-C.; Hsieh, C.-Y.; Lin, W.-N.; Wen, L.-L.; Chang, S.-W.; et al. A Joint Evaluation of Neurohormone Vasopressin-Neurophysin II-Copeptin and Aortic Arch Calcification on Mortality Risks in Hemodialysis Patients. Front. Med. 2020, 7, 102. [Google Scholar] [CrossRef] [PubMed]
- Jehn, U.; Schütte-Nütgen, K.; Henke, U.; Bautz, J.; Pavenstädt, H.; Suwelack, B.; Reuter, S. Prognostic Value of Growth Differentiation Factor 15 in Kidney Donors and Recipients. J. Clin. Med. 2020, 9, 1333. [Google Scholar] [CrossRef]
- Wischhusen, J.; Melero, I.; Fridman, W.H. Growth/Differentiation Factor-15 (GDF-15): From Biomarker to Novel Targetable Immune Checkpoint. Front. Immunol. 2020, 11, 951. [Google Scholar] [CrossRef]
- Nair, V.; Robinson-Cohen, C.; Smith, M.R.; Bellovich, K.A.; Bhat, Z.Y.; Bobadilla, M.; Brosius, F.; de Boer, I.H.; Essioux, L.; Formentini, I.; et al. Growth Differentiation Factor-15 and Risk of CKD Progression. J. Am. Soc. Nephrol. 2017, 28, 2233–2240. [Google Scholar] [CrossRef]
- Tuegel, C.; Katz, R.; Alam, M.; Bhat, Z.; Bellovich, K.; de Boer, I.; Brosius, F.; Gadegbeku, C.; Gipson, D.; Hawkins, J.; et al. GDF-15, Galectin 3, Soluble ST2, and Risk of Mortality and Cardiovascular Events in CKD. Am. J. Kidney Dis. 2018, 72, 519–528. [Google Scholar] [CrossRef]
- Bansal, N.; Zelnick, L.; Shlipak, M.G.; Anderson, A.; Christenson, R.; Deo, R.; deFilippi, C.; Feldman, H.; Lash, J.; He, J.; et al. Cardiac and Stress Biomarkers and Chronic Kidney Disease Progression: The CRIC Study. Clin. Chem. 2019, 65, 1448–1457. [Google Scholar] [CrossRef]
- Stein, N.R.; Zelnick, L.R.; Anderson, A.H.; Christenson, R.H.; deFilippi, C.R.; Deo, R.; Go, A.S.; He, J.; Ky, B.; Lash, J.P.; et al. Associations Between Cardiac Biomarkers and Cardiac Structure and Function in CKD. Kidney Int. Rep. 2020, 5, 1052–1060. [Google Scholar] [CrossRef]
- You, A.S.; Kalantar-Zadeh, K.; Lerner, L.; Nakata, T.; Lopez, N.; Lou, L.; Veliz, M.; Soohoo, M.; Jing, J.; Zaldivar, F.; et al. Association of Growth Differentiation Factor 15 with Mortality in a Prospective Hemodialysis Cohort. Cardiorenal. Med. 2017, 7, 158–168. [Google Scholar] [CrossRef] [PubMed]
- Carney, E.F. The impact of chronic kidney disease on global health. Nat. Rev. Nephrol. 2020, 16, 251. [Google Scholar] [CrossRef]
- Shoemaker, M.B.; Stevenson, W.G. The ABC death risk score: Is it time to start measuring GDF-15? Eur. Heart J. 2018, 39, 486–487. [Google Scholar] [CrossRef] [PubMed]
- Ramspek, C.L.; Voskamp, P.W.; van Ittersum, F.J.; Krediet, R.T.; Dekker, F.W.; van Diepen, M. Prediction models for the mortality risk in chronic dialysis patients: A systematic review and independent external validation study. Clin. Epidemiol. 2017, 9, 451–464. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Q.; Zhang, H.; Deng, T.; Tang, S.; Yuan, X.; Tang, W.; Xie, Y.; Ge, H.; Wang, X.; Zhou, Q.; et al. Role of Artificial Intelligence in Kidney Disease. Int. J. Med. Sci. 2020, 17, 970–984. [Google Scholar] [CrossRef]
- Chang, J.F.; Wu, C.C.; Hsieh, C.Y.; Li, Y.Y.; Wang, T.M.; Liou, J.C. A Joint Evaluation of Impaired Cardiac Sympathetic Responses and Malnutrition-Inflammation Cachexia for Mortality Risks in Hemodialysis Patients. Front. Med. 2020, 7, 99. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.-L.; Hou, J.-S.; Lai, Y.-H.; Wang, C.-H.; Kuo, C.-H.; Liou, H.-H.; Hsu, B.-G. Association of SARC-F Questionnaire and Mortality in Prevalent Hemodialysis Patients. Diagnostics 2020, 10, 890. [Google Scholar] [CrossRef]
- Hijazi, Z.; Oldgren, J.; Lindbäck, J.; Alexander, J.H.; Connolly, S.J.; Eikelboom, J.W.; Ezekowitz, M.D.; Held, C.; Hylek, E.M.; Lopes, R.D.; et al. A biomarker-based risk score to predict death in patients with atrial fibrillation: The ABC (age, biomarkers, clinical history) death risk score. Eur. Heart J. 2018, 39, 477–485. [Google Scholar] [CrossRef]
- Khan, S.Q.; Ng, K.; Dhillon, O.; Kelly, D.; Quinn, P.; Squire, I.B.; Davies, J.E.; Ng, L.L. Growth differentiation factor-15 as a prognostic marker in patients with acute myocardial infarction. Eur. Heart J. 2009, 30, 1057–1065. [Google Scholar] [CrossRef]
- Eggers, K.M.; Kempf, T.; Venge, P.; Wallentin, L.; Wollert, K.C.; Lindahl, B. Improving long-term risk prediction in patients with acute chest pain: The Global Registry of Acute Coronary Events (GRACE) risk score is enhanced by selected nonnecrosis biomarkers. Am. Heart J. 2010, 160, 88–94. [Google Scholar] [CrossRef]
- Anand, I.S.; Kempf, T.; Rector, T.S.; Tapken, H.; Allhoff, T.; Jantzen, F.; Kuskowski, M.; Cohn, J.N.; Drexler, H.; Wollert, K.C. Serial measurement of growth-differentiation factor-15 in heart failure: Relation to disease severity and prognosis in the Valsartan Heart Failure Trial. Circulation 2010, 122, 1387–1395. [Google Scholar] [CrossRef]
- Xie, S.; Lu, L.; Liu, L. Growth differentiation factor-15 and the risk of cardiovascular diseases and all-cause mortality: A meta-analysis of prospective studies. Clin. Cardiol. 2019, 42, 513–523. [Google Scholar] [CrossRef]
- Breit, S.N.; Carrero, J.J.; Tsai, V.W.; Yagoutifam, N.; Luo, W.; Kuffner, T.; Bauskin, A.R.; Wu, L.; Jiang, L.; Barany, P.; et al. Macrophage inhibitory cytokine-1 (MIC-1/GDF15) and mortality in end-stage renal disease. Nephrol. Dial. Transplant. 2012, 27, 70–75. [Google Scholar] [CrossRef]
- Yilmaz, H.; Çelik, H.T.; Gurel, O.M.; Bilgic, M.A.; Namuslu, M.; Bozkurt, H.; Ayyildiz, A.; Inan, O.; Bavbek, N.; Akcay, A. Increased serum levels of GDF-15 associated with mortality and subclinical atherosclerosis in patients on maintenance hemodialysis. Herz 2015, 40 (Suppl. S3), 305–312. [Google Scholar] [CrossRef] [PubMed]
- Ravizza, S.; Huschto, T.; Adamov, A.; Böhm, L.; Büsser, A.; Flöther, F.F.; Hinzmann, R.; König, H.; McAhren, S.M.; Robertson, D.H.; et al. Predicting the early risk of chronic kidney disease in patients with diabetes using real-world data. Nat. Med. 2019, 25, 57–59. [Google Scholar] [CrossRef] [PubMed]
- Beam, A.L.; Kohane, I.S. Big Data and Machine Learning in Health Care. JAMA 2018, 319, 1317–1318. [Google Scholar] [CrossRef] [PubMed]
- Rank, N.; Pfahringer, B.; Kempfert, J.; Stamm, C.; Kühne, T.; Schoenrath, F.; Falk, V.; Eickhoff, C.; Meyer, A. Deep-learning-based real-time prediction of acute kidney injury outperforms human predictive performance. NPJ Digit. Med. 2020, 3, 139. [Google Scholar] [CrossRef]
| Variables | Tertile 1 <1314.8 pg/mL | Tertile 2 1314.8–1707.1 pg/mL | Tertile 3 >1707.1 pg/mL |
|---|---|---|---|
| Patients, n (%) | 56 (32.9) | 56 (32.9) | 58 (41.4) |
| Age (years) | 59.1 ± 6.8 | 60.3 ± 8.1 | 71.1 ± 7.1 |
| Male, n (%) | 31 (55.4) | 27 (48.2) | 24 (41.4) |
| Diabetes mellitus, n (%) | 23 (41.1) | 24 (42.9) | 29 (50.0) |
| Cardiovascular diseases, n (%) | 80 (47.9) | 51 (40.2) | 25 (62.5) |
| Hypertension, n (%) | 26 (46.4) | 32 (57.1) | 34 (58.6) |
| Systolic blood pressure (mmHg) | 135.3 ± 21.4 | 134.1 ± 21.7 | 142.3 ± 22.7 |
| Diastolic blood pressure (mmHg) | 76.4 ± 8.6 | 78.3 ± 11.4 | 79.3 ± 14.2 |
| Hemodialysis vintage (months) | 72.2 ± 58.4 | 62.5 ± 51.8 | 80.9 ± 34.2 |
| nPCR (g/kg/day) | 1.2 ± 0.3 | 1.1 ± 0.3 | 1.1 ± 0.3 |
| GDF15 (pg/mL) | 1046.6 ± 203.0 | 1525.4 ± 112.7 | 2298.6 ± 637.9 |
| Albumin (g/dL) | 4.0 ± 0.4 | 3.9 ± 0.4 | 3.8 ± 0.5 |
| Aspartate aminotransferase (IU/L) | 15.0 ± 5.1 | 15.5 ± 6.8 | 17.8 ± 8.4 |
| Alanine aminotransferase (IU/L) | 13.2 ± 8.3 | 14.8 ± 13.6 | 16.6 ± 13.0 |
| Total cholesterol (mg/dL) | 192.2 ± 51.3 | 184.3 ± 47.6 | 192.5 ± 46.7 |
| Triglyceride (mg/dL) | 243.7 ± 201.4 | 194.4 ± 172.1 | 179.8 ± 23.6 |
| Low-density lipoprotein | 108.1 ± 39.4 | 101.9 ± 34.1 | 111.8 ± 33.5 |
| Blood urea nitrogen (mg/dL) | 55.9 ± 17.8 | 59.5 ± 17.7 | 61.8 ± 20.0 |
| Creatinine (mg/dL) | 9.4 ± 2.0 | 10.0 ± 1.9 | 10.0 ± 1.6 |
| Blood glucose (mg/dL) | 141.7 ± 59.0 | 143.3 ± 65.0 | 135.1 ± 84.5 |
| Uric acid (mg/dL) | 7.4 ± 1.4 | 7.3 ± 1.3 | 7.2 ± 1.1 |
| Potassium (mmol L−1) | 4.6 ± 0.9 | 4.6 ± 0.9 | 4.3 ± 0.8 |
| Calcium (mg/dL) | 9.4 ± 0.8 | 9.3 ± 0.8 | 9.1 ± 0.7 |
| Phosphate (mg/dL) | 4.6 ± 1.7 | 4.3 ± 1.4 | 5.0 ± 1.4 |
| Calcium-phosphate product | 42.1 ± 15.1 | 40.2 ± 12.9 | 45.9 ± 13.6 |
| Intact parathyroid hormone (pg/mL) | 164.1 ± 220.5 | 153.8 ± 145.2 | 184.9 ± 200.2 |
| Hemoglobin (g/dL) | 10.8 ± 1.3 | 10.4 ± 1.2 | 10.6 ± 1.3 |
| Hematocrit (%) | 32.2 ± 3.8 | 31.1 ± 3.5 | 32.0 ± 3.7 |
| Platelet (k/μL) | 209.3 ± 66.3 | 185.5 ± 71.4 | 199.9 ± 56.1 |
| All-Cause Mortality | CV Mortality | |||
|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| Age | 1.074 (1.037–1.112) | p < 0.01 | 1.086 (1.040–1.133) | p < 0.01 |
| Male | 0.867 (0.476–1.578) | p = 0.64 | 1.139 (0.556–2.335) | p = 0.72 |
| HD vintage | 1.006 (1.001–1.011) | p < 0.05 | 1.004 (0.998–1.011) | p = 0.17 |
| GDF15 | 1.001 (1.000–1.001) | p < 0.01 | 1.001 (1.000–1.001) | p < 0.01 |
| SBP | 1.012 (0.998–1.026) | p = 0.08 | 1.021 (1.005–1.038) | p < 0.05 |
| DBP | 0.981 (0.998–1.026) | p = 0.16 | 0.982 (0.952–1.014) | p = 0.27 |
| Blood glucose | 1.001 (0.996–1.006) | p = 0.72 | 1.003 (0.998–1.008) | p = 0.30 |
| nPCR | 0.840 (0.284–2.488) | p = 0.75 | 0.875 (0.239–3.200) | p = 0.84 |
| Albumin | 0.200 (0.100–0.402) | p < 0.01 | 0.377 (0.160–0.884) | p < 0.05 |
| AST | 0.983 (0.938–1.030) | p = 0.47 | 0.957 (0.898–1.019) | p = 0.17 |
| ALT | 1.014 (0.993–1.036) | p = 0.19 | 1.018 (0.994–1.043) | p = 0.14 |
| T-Cholesterol | 0.999 (0.992–1.005) | p = 0.65 | 1.000 (0.993–1.008) | p = 0.90 |
| Triglyceride | 0.998 (0.996–1.001) | p = 0.15 | 0.998 (0.995–1.001) | p = 0.19 |
| LDL | 0.998 (0.990–1.006) | p = 0.63 | 1.001 (0.991–1.011) | p = 0.83 |
| BUN | 1.008 (0.992–1.023) | p = 0.34 | 1.009 (0.991–1.028) | p = 0.34 |
| Creatinine | 1.029 (0.879–1.204) | p = 0.73 | 1.113 (0.920–1.347) | p = 0.27 |
| Uric acid | 1.077 (0.859–1.350) | p = 0.52 | 1.088 (0.830–1.426) | p = 0.54 |
| Potassium | 0.788 (0.552–1.125) | p = 0.19 | 0.773 (0.504–1.185) | p = 0.24 |
| Calcium | 0.795 (0.515–1.229) | p = 0.30 | 0.602 (0.347–1.045) | p = 0.07 |
| Phosphate | 1.075 (0.897–1.288) | p = 0.44 | 1.038 (0.829–1.300) | p = 0.75 |
| Ca-P product | 1.005 (0.984–1.026) | p = 0.64 | 0.999 (0.973–1.025) | p = 0.92 |
| iPTH | 1.001 (1.000–1.002) | p = 0.07 | 1.001 (0.999–1.002) | p = 0.43 |
| Hemoglobin | 1.066 (0.818–1.390) | p = 0.63 | 1.013 (0.739–1.389) | p = 0.94 |
| Hematocrit | 1.032 (0.939–1.133) | p = 0.51 | 1.017 (0.910–1.137) | p = 0.77 |
| Platelet | 1.002 (0.998–1.007) | p = 0.35 | 1.005 (0.997–1.010) | p = 0.09 |
| All-Cause Mortality | CV Mortality | |||
|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| Age | 1.044 (1.007–1.083) | p < 0.05 | 1.062 (1.015–1.112) | p < 0.01 |
| GDF15 | 1.001 (1.000–1.001) | p < 0.01 | 1.001 (1.000–1.001) | p < 0.05 |
| Albumin | 0.281 (0.141–0.560) | p < 0.01 | 0.550 (0.235–1.289) | p = 0.17 |
| Score = 1 | Score = 2 | Score = 3 | Score = 4 | Score = 5 | |
|---|---|---|---|---|---|
| Patients, n (%) | 32 (18.8) | 55 (32.4) | 25 (14.7) | 39 (22.9) | 19 (11.2) |
| All-cause death, n (%) | 0 (0) | 10 (18.2) | 9 (36.0) | 12 (30.8) | 12 (63.2) |
| CV death, n (%) | 0 (0) | 7 (12.7) | 6 (24.0) | 10 (25.6) | 7 (36.8) |
| Age (years) | 56.3 ± 4.0 | 58.9 ± 6.4 | 61.6 ± 7.1 | 71.2 ± 6.6 | 74.2 ± 4.7 |
| Male, n (%) | 12 (37.5) | 33 (60.0) | 15 (60.0) | 13 (33.3) | 9 (47.4) |
| DM, n (%) | 9 (28.1) | 24 (43.6) | 12 (48.0) | 20 (51.3) | 11 (57.9) |
| CVD, n (%) | 12 (37.5) | 22 (40.0) | 11 (44.0) | 24 (61.5) | 10 (52.6) |
| Hypertension, n (%) | 19 (59.4) | 29 (52.7) | 13 (52.0) | 21 (53.8) | 10 (52.6) |
| SBP (mmHg) | 136.4 ± 16.4 | 134.3 ± 23.2 | 135.0 ± 25.5 | 141.1 ± 21.8 | 143.8 ± 23.7 |
| DBP (mmHg) | 79.1 ± 6.9 | 79.0 ± 10.7 | 71.2 ± 11.2 | 79.7 ± 14.4 | 79.0 ± 13.1 |
| HD vintage (months) | 72.9 ± 49.2 | 59.6 ± 51.9 | 81.9 ± 61.6 | 83.1 ± 41.5 | 70.4 ± 32.4 |
| nPCR (g/kg/day) | 1.2 ± 0.3 | 1.1 ± 0.3 | 1.1 ± 0.3 | 1.0 ± 0.2 | 1.1 ± 0.4 |
| GDF15 (pg/mL) | 1098.3 ± 181.3 | 1303.8 ± 324.3 | 1731.8 ± 638.1 | 2157.2 ± 633.8 | 2266.7 ± 592.8 |
| Albumin (g/dL) | 4.1 ± 0.3 | 4.0 ± 0.4 | 3.8 ± 0.4 | 3.8 ± 0.4 | 3.3 ± 0.4 |
| AST (IU/L) | 15.1 ± 5.0 | 14.7 ± 5.5 | 15.7 ± 6.9 | 18.9 ± 9.1 | 17.3 ± 8.0 |
| ALT (IU/L) | 14.9 ± 8.4 | 14.1 ± 13.5 | 13.2 ± 10.6 | 14.8 ± 11.0 | 19.3 ± 15.3 |
| T-Cholesterol (mg/dL) | 188.5 ± 48.5 | 190.3 ± 51.3 | 186.6 ± 43.1 | 199.4 ± 52.9 | 186.0 ± 41.6 |
| Triglyceride (mg/dL) | 225.7 ± 180.7 | 222.7 ± 203.9 | 198.5 ± 165.0 | 202.1 ± 197.5 | 172.6 ± 141.6 |
| LDL | 107.2 ± 41.4 | 105.8 ± 36.3 | 103.0 ± 29.8 | 114.4 ± 37.4 | 103.5 ± 28.5 |
| BUN (mg/dL) | 53.5 ± 16.1 | 57.2 ± 17.1 | 65.1 ± 16.9 | 59.4 ± 18.0 | 65.5 ± 25.8 |
| Creatinine (mg/dL) | 9.6 ± 2.0 | 9.8 ± 2.2 | 10.5 ± 1.4 | 9.5 ± 1.5 | 9.9 ± 1.7 |
| Blood glucose (mg/dL) | 122.0 ± 40.2 | 130.9 ± 57.5 | 152.6 ± 63.2 | 133.6 ± 70.2 | 137.0 ± 69.7 |
| Uric acid (mg/dL) | 7.5 ± 1.3 | 7.3 ± 1.5 | 7.6 ± 1.1 | 6.9 ± 1.1 | 7.2 ± 0.9 |
| Potassium (mmol L-1) | 4.6 ± 1.0 | 4.5 ± 0.9 | 4.8 ± 0.7 | 4.2 ± 0.6 | 4.1 ± 1.0 |
| Calcium (mg/dL) | 9.3 ± 0.7 | 9.2 ± 0.7 | 9.4 ± 0.8 | 9.2 ± 0.7 | 9.1 ± 0.7 |
| Phosphate (mg/dL) | 4.5 ± 1.5 | 4.4 ± 1.7 | 5.1 ± 1.5 | 4.7 ± 1.2 | 5.0 ± 1.7 |
| Ca-P product | 41.6 ± 14.0 | 40.9 ± 15.2 | 47.0 ± 14.4 | 42.8 ± 10.4 | 44.5 ± 16.2 |
| iPTH (pg/mL) | 213.9 ± 254.0 | 177.5 ± 195.8 | 328.8 ± 320.2 | 236.4 ± 230.5 | 198.4 ± 214.2 |
| Hemoglobin (g/dL) | 10.8 ± 1.3 | 10.6 ± 1.3 | 10.7 ± 1.1 | 10.6 ± 1.2 | 10.4 ± 1.6 |
| Hematocrit (%) | 32.0 ± 3.7 | 31.4 ± 3.7 | 31.9 ± 3.2 | 31.9 ± 3.5 | 31.7 ± 4.5 |
| Platelet (k/μL) | 205.2 ± 62.6 | 200.0 ± 68.2 | 192.1 ± 78.7 | 190.4 ± 57.9 | 203.7 ± 64.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, J.-F.; Chen, P.-C.; Hsieh, C.-Y.; Liou, J.-C. A Growth Differentiation Factor 15-Based Risk Score Model to Predict Mortality in Hemodialysis Patients. Diagnostics 2021, 11, 286. https://doi.org/10.3390/diagnostics11020286
Chang J-F, Chen P-C, Hsieh C-Y, Liou J-C. A Growth Differentiation Factor 15-Based Risk Score Model to Predict Mortality in Hemodialysis Patients. Diagnostics. 2021; 11(2):286. https://doi.org/10.3390/diagnostics11020286
Chicago/Turabian StyleChang, Jia-Feng, Po-Cheng Chen, Chih-Yu Hsieh, and Jian-Chiun Liou. 2021. "A Growth Differentiation Factor 15-Based Risk Score Model to Predict Mortality in Hemodialysis Patients" Diagnostics 11, no. 2: 286. https://doi.org/10.3390/diagnostics11020286
APA StyleChang, J.-F., Chen, P.-C., Hsieh, C.-Y., & Liou, J.-C. (2021). A Growth Differentiation Factor 15-Based Risk Score Model to Predict Mortality in Hemodialysis Patients. Diagnostics, 11(2), 286. https://doi.org/10.3390/diagnostics11020286







