Changes in Blood Potassium after Reperfusion during Living-Donor Liver Transplantation: An Exploratory Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Anesthetic and Surgical Management
2.2. Study Protocol
2.3. Statistical Analysis
3. Results
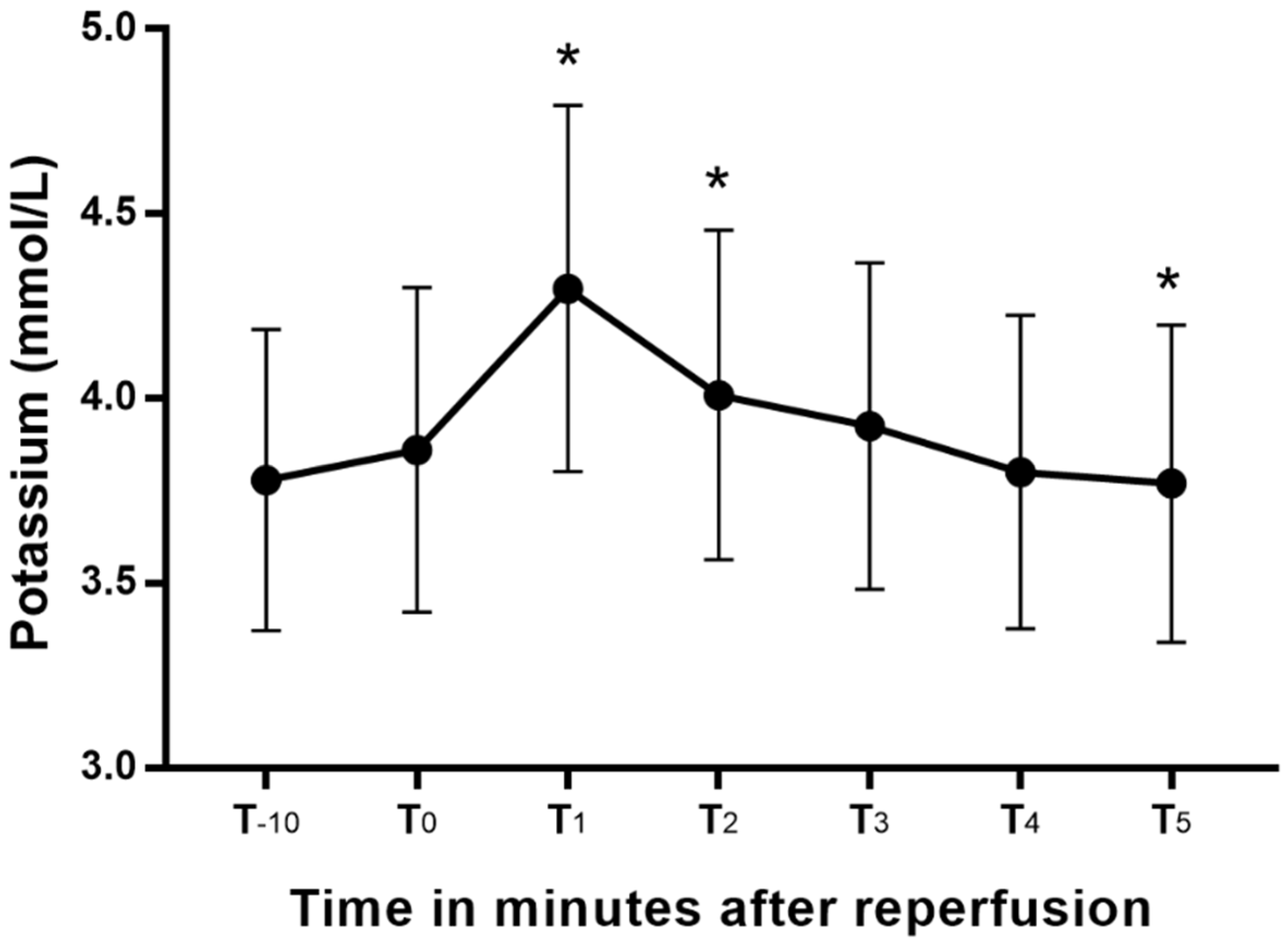
3.1. Primary Outcomes
3.2. Other Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shangraw, R.E. Metabolic Issues in Liver Transplantation. Int. Anesthesiol. Clin. 2006, 44, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Dalal, A. Anesthesia for liver transplantation. Transplant. Rev. 2016, 30, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Matsusaki, T.; Hilmi, I.A.; Planinsic, R.M.; Humar, A.; Sakai, T. Cardiac arrest during adult liver transplantation: A single institution’s experience with 1238 deceased donor transplants. Liver Transplant. 2013, 19, 1262–1271. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Gwak, M.S.; Choi, S.J.; Shin, Y.H.; Ko, J.S.; Kim, G.S.; Lee, S.Y.; Kim, M.; Park, H.G.; Jeon, H.J. Intra-operative cardiac arrests during liver transplantation—A retrospective review of the first 15 yr in Asian population. Clin. Transplant. 2013, 27, E126–E136. [Google Scholar] [CrossRef] [PubMed]
- Nakasuji, M.; Bookallil, M.J. Pathophysiological Mechanisms of Postrevascularization Hyperkalemia in Orthotopic Liver Transplantation. Anesth. Analg. 2000, 91, 1351–1355. [Google Scholar] [CrossRef] [PubMed]
- Xia, V.W.; Ghobrial, R.M.; Du, B.; Chen, T.; Hu, K.-Q.; Hiatt, J.R.; Busuttil, R.W.; Steadman, R.H. Predictors of Hyperkalemia in the Prereperfusion, Early Postreperfusion, and Late Postreperfusion Periods During Adult Liver Transplantation. Anesth. Analg. 2007, 105, 780–785. [Google Scholar] [CrossRef] [PubMed]
- Weinberg, L.; Lee, D.-K.; Koshy, A.N.; Leong, K.W.; Tosif, S.; Shaylor, R.M.; Pillai, P.; Miles, L.F.; Drucker, A.; Pearce, B. Potassium levels after liver reperfusion in adult patients undergoing cadaveric liver transplantation: A retrospective cohort study. Ann. Med. Surg. 2020, 55, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Dawwas, M.F.; Lewsey, J.D.; Watson, C.J.; Gimson, A.E. The Impact of Serum Potassium Concentration on Mortality after Liver Transplantation: A Cohort Multicenter Study. Transplantation 2009, 88, 402–410. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.J.; Brown, D.C.; Murphy, M. Hypokalemia from Beta2-Receptor Stimulation by Circulating Epinephrine. N. Engl. J. Med. 1983, 309, 1414–1419. [Google Scholar] [CrossRef] [PubMed]
- Koponen, T.; Karttunen, J.; Musialowicz, T.; Pietiläinen, L.; Uusaro, A.; Lahtinen, P. Vasoactive-inotropic score and the prediction of morbidity and mortality after cardiac surgery. Br. J. Anaesth. 2019, 122, 428–436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shoemaker, W.C. The action of epinephrine and other hormones associated with the stress response on potassium movements with special reference to the development of postoperative depletion states. Rev. Surg. 1968, 25, 9–24. [Google Scholar] [PubMed]
- Fukuzawa, K.; Schwartz, M.E.; Acarli, K.; Katz, E.; Gabrielson, G.; Gettes, M.; Jacobs, E.; Miller, C.M. Flushing with autologous blood improves intraoperative hemodynamic stability and early graft function in clinical hepatic transplantation. J. Am. Coll. Surg. 1994, 178, 541–547. [Google Scholar] [PubMed]
- Acosta, F.; Sansano, T.; Contreras, R.; Reche, M.; Beltran, R.; Roques, V.; Rodriguez, M.; Robles, R.; Bueno, F.; Ramirez, P.; et al. Changes in serum potassium during reperfusion in liver transplantation. Transplant. Proc. 1999, 31, 2382–2383. [Google Scholar] [CrossRef]
- Juang, S.-E.; Chen, C.-L.; Wang, C.-H.; Cheng, K.-W.; Wu, S.-C.; Shih, T.-H.; Yang, S.-C.; Wong, Z.-W.; Jawan, B.; Lee, Y.-E.; et al. Predictive Risk Factors in the Development of Intraoperative Hyperkalemia in Adult Living Donor Liver Transplantation. Transplant. Proc. 2016, 48, 1022–1024. [Google Scholar] [CrossRef] [PubMed]
- Massip-Salcedo, M.; Rosello-Catafau, J.; Prieto, J.; Avila, M.; Peralta, C. The response of the hepatocyte to ischemia. Liver Int. 2007, 27, 6–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, W.-J.; Xia, W.-L.; Pan, H.-Y.; Zheng, S.-S. Postreperfusion hyperkalemia in liver transplantation using donation after cardiac death grafts with pathological changes. Hepatobiliary Pancreat. Dis. Int. 2016, 15, 487–492. [Google Scholar] [CrossRef]
- Homvises, B.; Sirivatanauksorn, Y.; Limsrichamrern, S.; Pongraweewan, O.; Sujirattanawimol, K.; Raksakietisak, M. The Minimal Flush Volume for Washout of Preservation Fluid in Liver Transplantation. Transplant. Proc. 2008, 40, 2123–2126. [Google Scholar] [CrossRef] [PubMed]
- Stoll, W.D.; Hand, W.R.; Chavin, K.D.; Felton, D.H.; Wolf, B.O.; Davis, G.P.; Harvey, N.R.; Whiteley, J.R.; Mester, R.A.; Bolin, E.D. Post-Reperfusion Syndrome in Liver Transplantation: Does a Caval Blood Flush Vent Help? Ann. Transplant. 2019, 24, 631–638. [Google Scholar] [CrossRef] [PubMed]
- Davila, D.; Bartlett, A.; Heaton, N. Temporary portocaval shunt in orthotopic liver transplantation: Need for a standardized approach? Liver Transplant. 2008, 14, 1414–1419. [Google Scholar] [CrossRef] [PubMed]

| Variable | Result | Normal Range |
|---|---|---|
| Male, n (%) | 11 (73.3) | |
| Age, years, mean ± SD | 56.1 ± 10.0 | |
| Body Mass Index, kg/m2, mean ± SD | 25.1 ± 4.7 | |
| Chronic kidney disease, n (%) | 2 (13.3) | |
| Hypertension, n (%) | 4 (26.7) | |
| Diabetes mellitus, n (%) | 5 (33.3) | |
| ABO incompatible liver transplantation, n (%) | 4 (26.7) | |
| MELD score, median (IQR) | 9.0 (7.0–13.5) | |
| Indications for liver transplantation | ||
| Liver cirrhosis, n (%) | 5 (33.3) | |
| Hepatocellular carcinoma, n (%) | 9 (60.0) | |
| Acute liver failure, n (%) | 1 (6.7) | |
| Preoperative laboratory results | ||
| Hemoglobin, g/dL, mean ± SD | 11.0 ± 2.6 | male 13.6–17.4 female 11.2–14.8 |
| Hematocrit, %, mean ± SD | 33.0 ± 7.5 | male 40.4–51.3 female 31.8–43.8 |
| White blood cell count, ×103/μL, median (IQR) | 3.6 (2.7–6.2) | male 3.80–10.58 female 3.15–8.63 |
| Platelets, ×103/μL, mean ± SD | 101.9 ± 58.3 | male 141–316 female 138–347 |
| International Normalized Ratio, mean ± SD | 1.3 ± 0.3 | 0.9–1.1 |
| Sodium, mmol/L, median (IQR) | 139.0 (138.0–141.0) | 136–145 |
| Potassium, mmol/L, mean ± SD | 4.0 ± 0.4 | 3.5–5.1 |
| Chloride, mmol/L, median (IQR) | 105.0 (103.0–107.0) | 98−107 |
| Blood urea nitrogen, mg/dL, median (IQR) | 13.3 (11.7–20.6) | 6–23 |
| Creatinine, mg/dL, median (IQR) | 0.67 (0.60–0.97) | 0.70–1.20 |
| Estimated GFR, mL/min/1.73 m2, mean ± SD | 93.1 ± 26.7 | 60–150 |
| Calcium, mg/dL, mean ± SD | 8.4 ± 0.4 | 8.6–10.2 |
| Magnesium, mg/dL, mean ± SD | 1.9 ± 0.2 | 1.6–2.6 |
| Phosphate, mg/dL, mean ± SD | 3.9 ± 0.6 | 3.0–4.5 |
| Bilirubin, mg/dL, median (IQR) | 1.0 (0.7–1.9) | 0–1.2 |
| Alanine transaminase, U/L, mean ± SD | 29.0 ± 17.4 | 0–40 |
| Aspartate transaminase, U/L, median (IQR) | 33.0 (28.5–39.5) | 0–41 |
| Gamma-glutamyl transferase, U/L, mean ± SD | 75.9 ± 45.9 | 10–71 |
| Alkaline phosphatase, U/L, mean ± SD | 102.1 ± 47.4 | 40–129 |
| Total protein, g/dL, mean ± SD | 6.2 ± 0.7 | 6.4–8.3 |
| Albumin, g/dL, mean ± SD | 3.2 ± 0.6 | 3.5–5.2 |
| Variable | Result |
|---|---|
| GRWR, mean ± SD | 1.12 ± 0.3 |
| Warm ischemia time, min, mean ± SD | 44.1 ± 14.1 |
| Cold ischemia time, min, mean ± SD | 103.8 ± 36.5 |
| Postreperfusion syndrome, n (%) | 7 (46.7) |
| Transient portocaval shunt, n (%) | 1 (6.7) |
| Surgery stage | |
| Total operative time, min, mean ± SD | 418.3 ± 71.6 |
| Dissection, min, median (IQR) | 62.0 (53.0–71.5) |
| Anhepatic, min, mean ± SD | 156.5 ± 36.1 |
| Neohepatic, min, mean ± SD | 191.7 ± 47.0 |
| Prereperfusion blood potassium | |
| 10 min before reperfusion, mmol/L, mean ± SD | 3.8 ± 0.4 |
| Immediately before reperfusion, mmol/L, mean ± SD | 3.9 ± 0.4 |
| Fluid before reperfusion | |
| Plasma solution A, n (%) | 15 (100.0) |
| Volume, mL/kg, mean ± SD | 34.8 ± 14.8 |
| 5% Albumin, n (%) | 15 (100.0) |
| Volume, mL/kg, mean ± SD | 7.1 ± 2.3 |
| Hextend, n (%) | 9 (60.0) |
| Volume, mL/kg, median (IQR) | 7.2 (6.1–9.7) |
| Volulyte, n (%) | 7 (46.7) |
| Volume, mL/kg, median (IQR) | 9.4 (7.7–12.7) |
| Transfusion before reperfusion | |
| Allogeneic RBC, n (%) | 5 (33.3) |
| Number of unit, median (IQR) | 2.0 (1.0–2.0) |
| Platelet, n (%) | 0 (0.0) |
| Fresh frozen plasma, n (%) | 1 (6.7) |
| Cryoprecipitate, n (%) | 0 (0.0) |
| Infused salvaged blood, n(%) | 5 (33.3) |
| Total volume, mL, median (IQR) | 291.0 (278–300) |
| Vasoactive drugs at reperfusion | |
| VIS, median (IQR) | 5.0 (0.0–10.0) |
| Norepinephrine, n (%) | 8 (53.3) |
| Dose, mcg/kg/min, median (IQR) | 0.10 (0.05–0.15) |
| Dopamine, n (%) | 4 (26.7) |
| Dose, mcg/kg/min, median (IQR) | 5.00 (4.50–6.25) |
| Vasopressin, n (%) | 1 (6.7) |
| Dose, unit/hr, median (IQR) | 1.2 (1.2–1.2) |
| Correlation Coefficient | Raw p-Value | |
|---|---|---|
| MELD score | 0.20 | 0.47 |
| Preoperative potassium values, mmol/L | 0.70 | 0.004 |
| GRWR | 0.15 | 0.59 |
| Warm ischemia time, min | −0.02 | 0.94 |
| Cold ischemia time, min | 0.07 | 0.79 |
| Total operative time, min | 0.15 | 0.59 |
| Anhepatic time, min | −0.02 | 0.95 |
| Prereperfusion blood potassium | ||
| 10 min before reperfusion, mmol/L | 0.97 | <0.0001 |
| Immediately before reperfusion, mmol/L | 0.95 | <0.0001 |
| Fluid and blood products before reperfusion | ||
| Allogeneic RBC, unit | 0.34 | 0.22 |
| Salvaged blood, mL | 0.27 | 0.33 |
| Plasma solution A, mL/kg | −0.01 | 0.97 |
| Albumin (5%), mL/kg | 0.09 | 0.75 |
| Volulyte, mL/kg | 0.27 | 0.77 |
| Hextend, mL/kg | −0.29 | 0.29 |
| Vasoactive-Inotropic Score | −0.17 | 0.55 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.; Kwon, J.-H.; Kim, G.S. Changes in Blood Potassium after Reperfusion during Living-Donor Liver Transplantation: An Exploratory Study. Diagnostics 2021, 11, 2248. https://doi.org/10.3390/diagnostics11122248
Kim J, Kwon J-H, Kim GS. Changes in Blood Potassium after Reperfusion during Living-Donor Liver Transplantation: An Exploratory Study. Diagnostics. 2021; 11(12):2248. https://doi.org/10.3390/diagnostics11122248
Chicago/Turabian StyleKim, Jeayoun, Ji-Hye Kwon, and Gaab Soo Kim. 2021. "Changes in Blood Potassium after Reperfusion during Living-Donor Liver Transplantation: An Exploratory Study" Diagnostics 11, no. 12: 2248. https://doi.org/10.3390/diagnostics11122248
APA StyleKim, J., Kwon, J.-H., & Kim, G. S. (2021). Changes in Blood Potassium after Reperfusion during Living-Donor Liver Transplantation: An Exploratory Study. Diagnostics, 11(12), 2248. https://doi.org/10.3390/diagnostics11122248






