Evaluation of Breast Galactography Using Digital Breast Tomosynthesis: A Clinical Exploratory Study
Abstract
1. Introduction
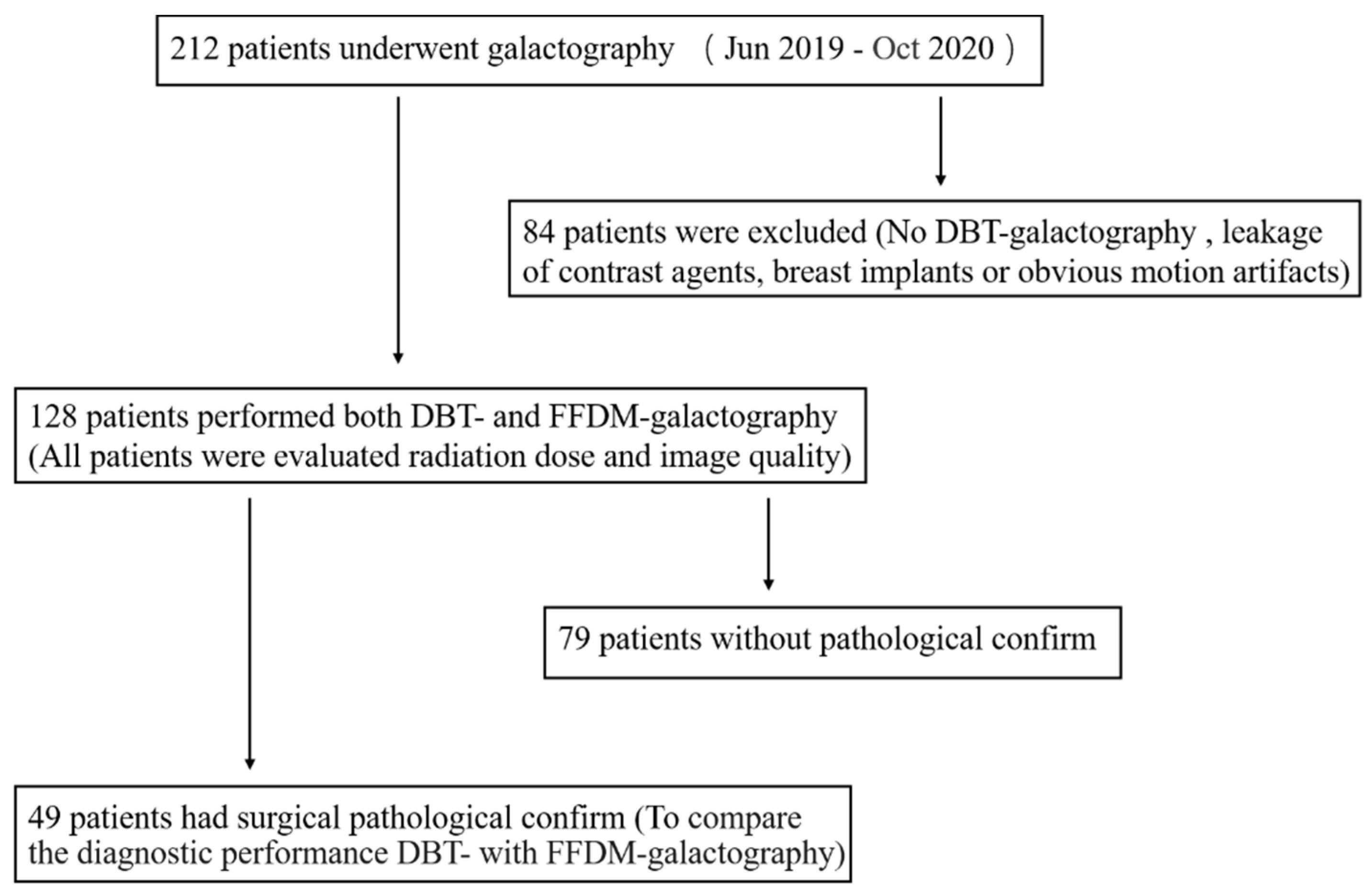
2. Materials and Methods
2.1. Patients
2.2. Galactography
2.2.1. Galactography Operation
2.2.2. Contrast Agent
2.3. Imaging
2.4. Imaging Analysis
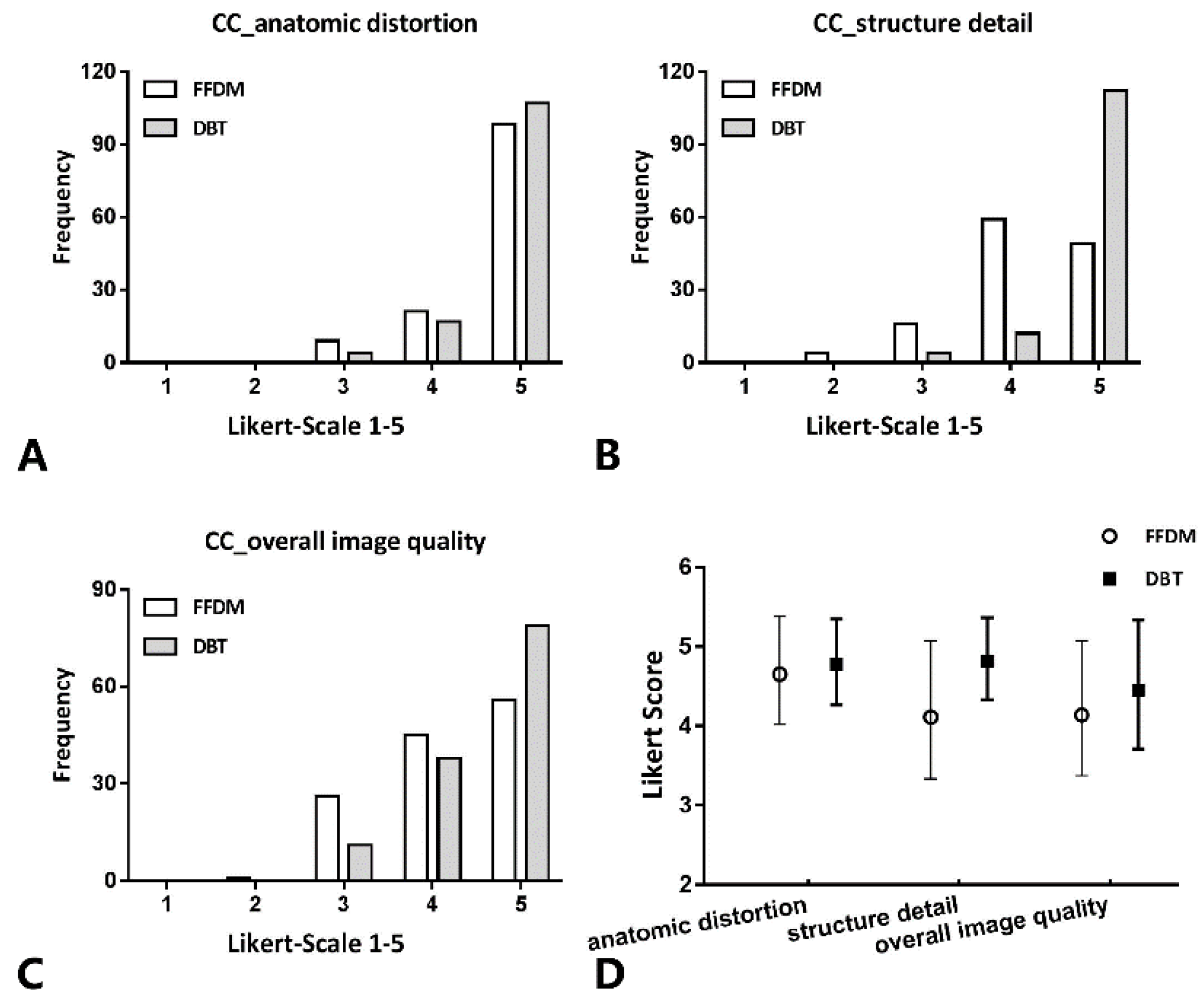
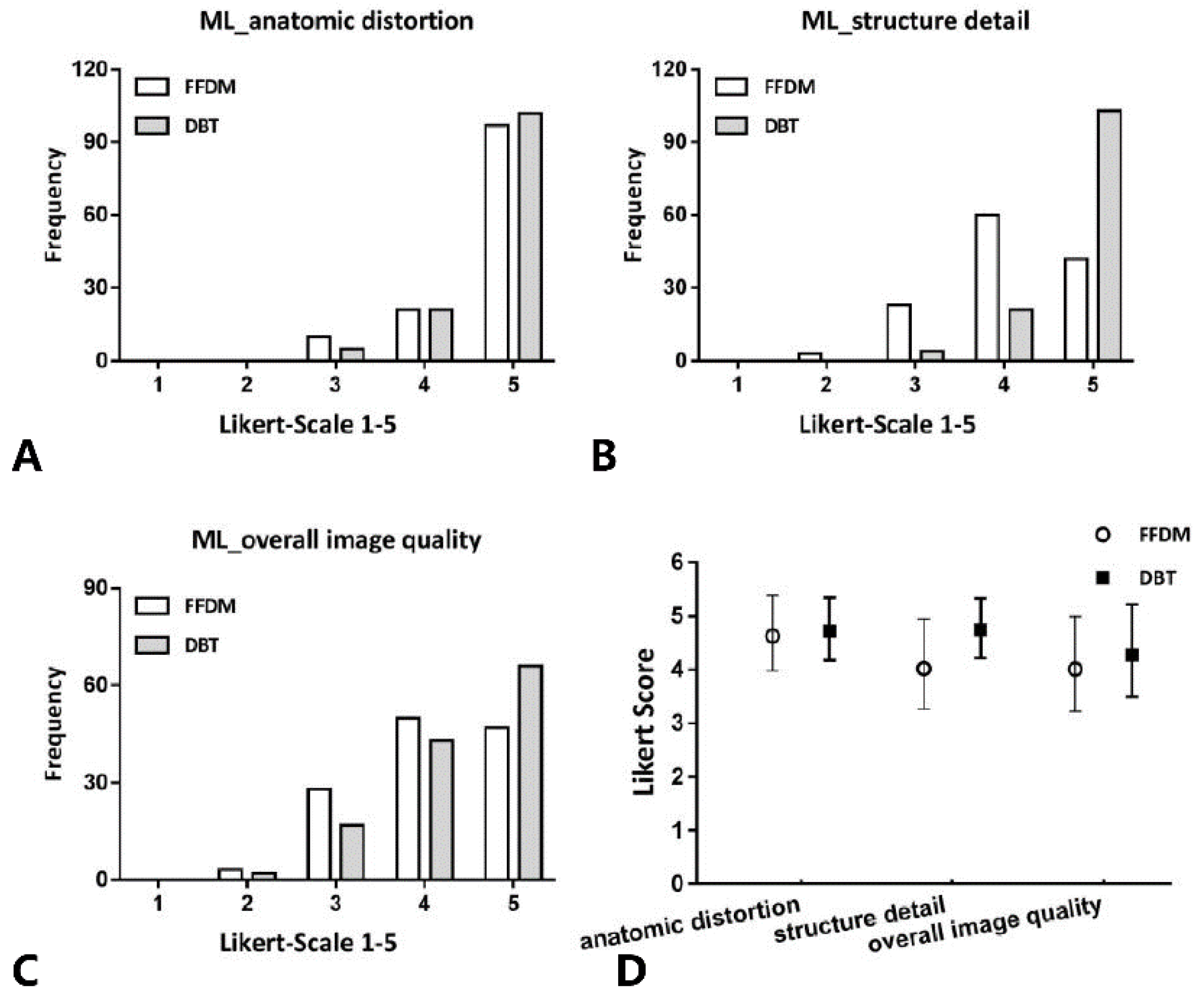
- Catheter anatomic distortion (1 = very strong, 2 = strong, 3 = medium, 4 = small, 5 = negligible)
- Catheter structure detail (1 = not diagnostic, 2 = poor, 3 = moderate, 4 = good, 5 = excellent)
- Overall image quality (1 = not diagnostic, 2 = poor, 3 = moderate, 4 = good, 5 = excellent).
2.5. Statistical Analysis
3. Results
3.1. Patient Information
3.2. Average Glandular Dose (AGD)
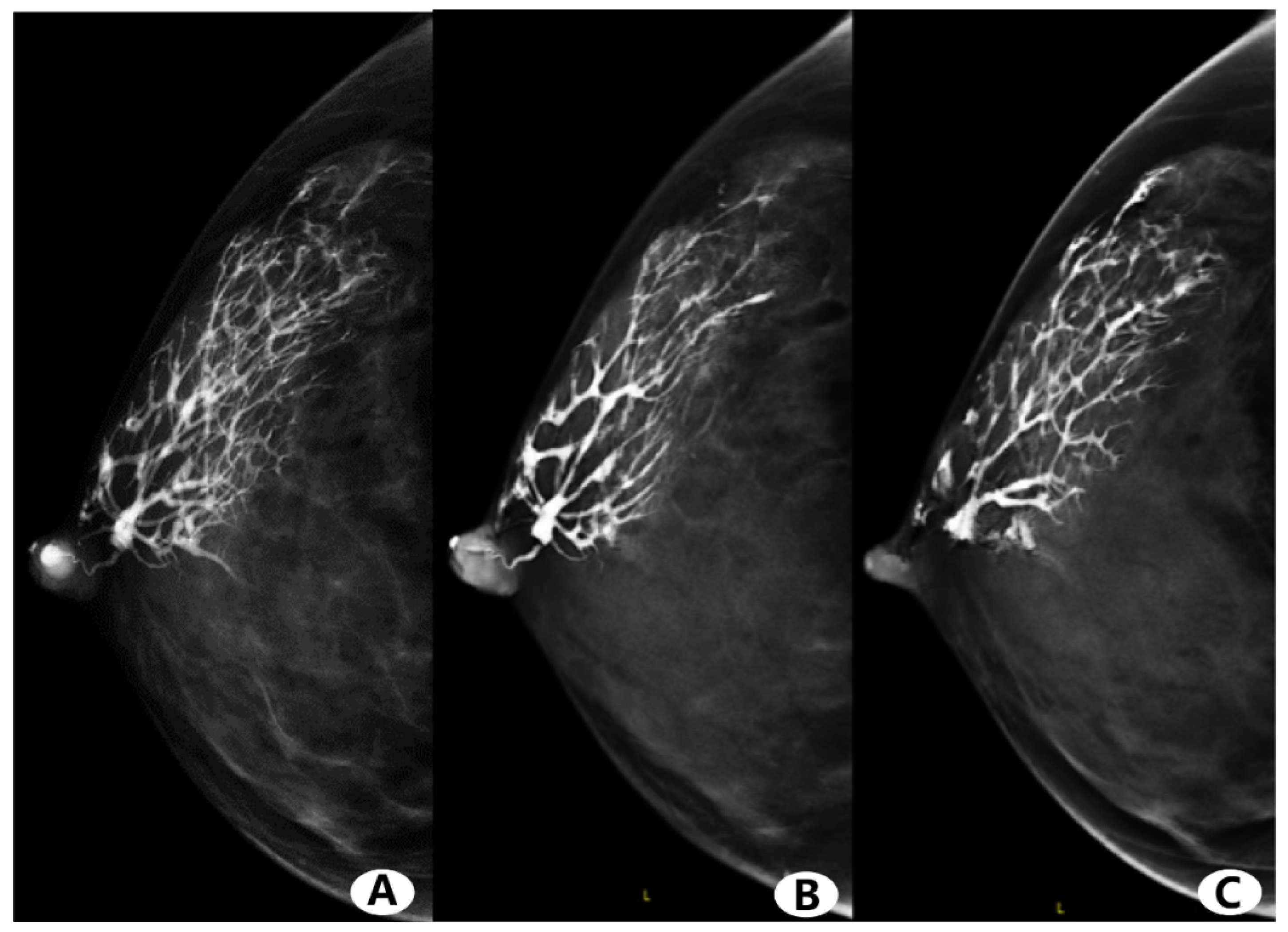
3.3. Visual Image Analysis
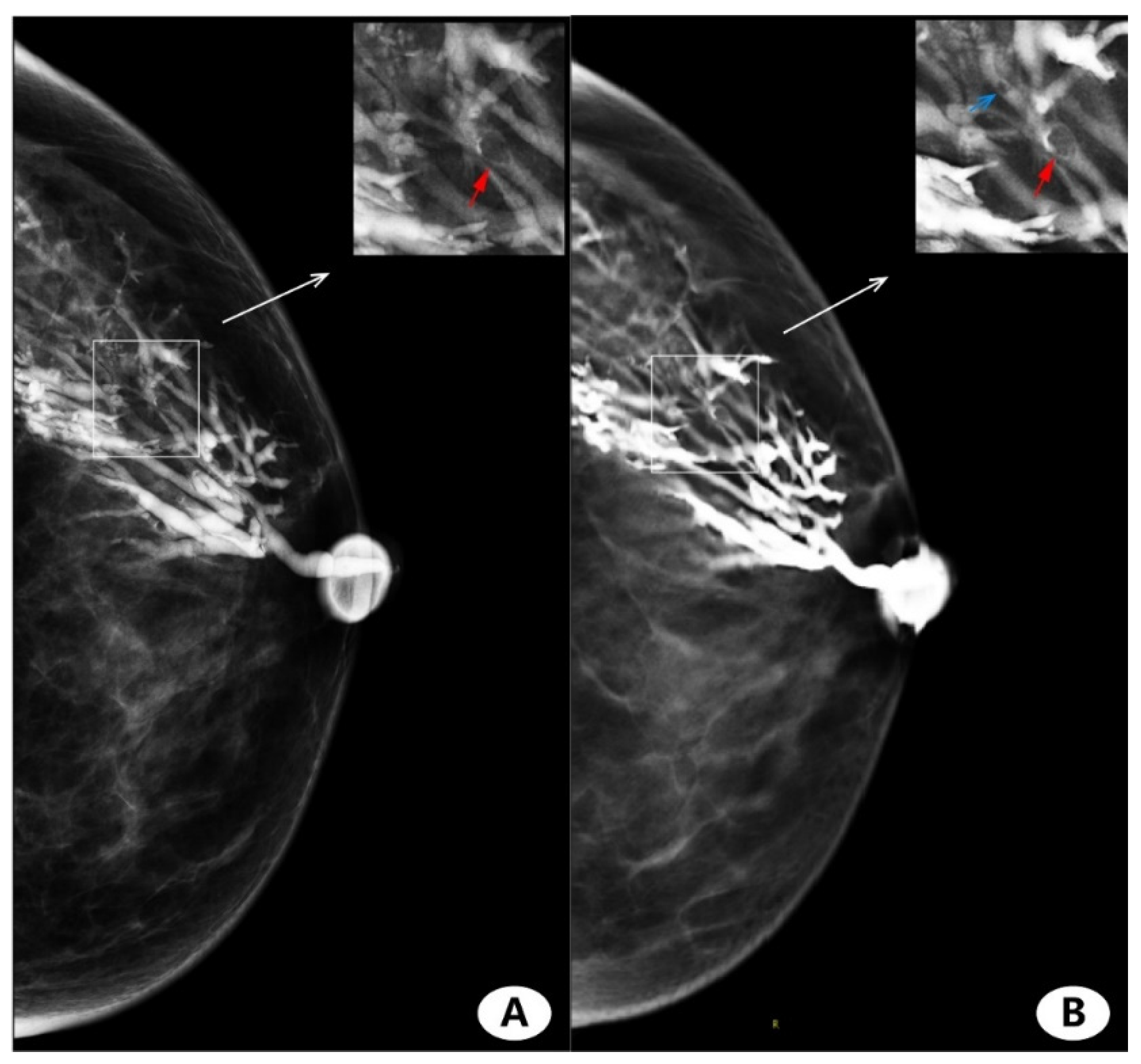
3.4. Imaging Finding
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alcock, C.; Layer, G.T. Predicting occult malignancy in nipple discharge. Anz. J. Surg. 2010, 80, 646–649. [Google Scholar] [CrossRef] [PubMed]
- Berger, N.; Luparia, A.; Di Leo, G.; Carbonaro, L.A.; Trimboli, R.M.; Ambrogi, F.; Sardanelli, F. Diagnostic Performance of MRI Versus Galactography in Women with Pathologic Nipple Discharge: A Systematic Review and Meta-Analysis. AJR Am. J. Roentgenol. 2017, 209, 465–471. [Google Scholar] [CrossRef]
- Seltzer, M.H.; Perloff, L.J.; Kelley, R.I.; Fitts, W.T., Jr. The significance of age in patients with nipple discharge. Surg. Gynecol. Obstet. 1970, 131, 519–522. [Google Scholar] [PubMed]
- Lee, S.; Trikha, S.; Moy, L.; Baron, P.; di Florio, R.M.; Green, E.D.; Heller, S.L.; Holbrook, A.I.; Lewin, A.A.; Lourenco, A.P.; et al. ACR Appropriateness Criteria® Evaluation of Nipple Discharge. J. Am. Coll. Radiol. 2017, 14, S138–S153. [Google Scholar] [CrossRef]
- Cho, N.; Moon, W.K.; Chung, S.Y.; Cha, J.H.; Cho, K.S.; Kim, E.K.; Oh, K.K. Ductographic findings of breast cancer. Korean J. Radiol. 2005, 6, 31–36. [Google Scholar] [CrossRef][Green Version]
- Peters, J.; Thalhammer, A.; Jacobi, V.; Vogl, T.J. Galactography: An important and highly effective procedure. Eur. Radiol. 2003, 13, 1744–1747. [Google Scholar] [CrossRef]
- Berná-Serna, J.D.; Torres-Ales, C.; Berná-Mestre, J.D.; Polo, L. Role of Galactography in the Early Diagnosis of Breast Cancer. Breast Care 2013, 8, 122–126. [Google Scholar] [CrossRef]
- Sheiman, L.S.; Levesque, P.H. The In’s and Out’s of Ductography: A Comprehensive Review. Curr. Probl. Diagn. Radiol. 2016, 45, 61–70. [Google Scholar] [CrossRef]
- Baydoun, S.; Gonzalez, P.; Whitman, G.J.; Dryden, M.; Xi, Y.; Dogan, B. Is Ductography Still Warranted in the 21st century? Breast J. 2019, 25, 654–662. [Google Scholar] [CrossRef]
- Srinivasan, A.; Nia, E.; Gupta, M.; Sun, J.; Leung, J.W. Retrospective statistical analysis on the diagnostic value of ductography based on lesion pathology in patients presenting with nipple discharge. Breast J. 2019, 25, 585–589. [Google Scholar] [CrossRef]
- Kim, S.H.; Cha, E.S.; Kim, H.S.; Kang, B.J.; Choi, J.J.; Jung, J.H. Galactography acquired with digital mammography in patients with nipple discharge: A retrospective analysis. Arch. Gynecol. Obstet. 2009, 280, 217–222. [Google Scholar] [CrossRef] [PubMed]
- Destounis, S. Role of Digital Breast Tomosynthesis in Screening and Diagnostic Breast Imaging. Semin. Ultrasound CT MR 2018, 39, 35–44. [Google Scholar] [CrossRef]
- Akashi-Tanaka, S. Developments in Breast Imaging. Nihon Geka Gakkai Zasshi 2016, 117, 483–490. [Google Scholar] [PubMed]
- Pisano, E.D.; Yaffe, M.J. Digital mammography. Radiology 2005, 234, 353–362. [Google Scholar] [CrossRef]
- Niklason, L.T.; Christian, B.T.; Niklason, L.E.; Kopans, D.B.; Castleberry, D.E.; Opsahl-Ong, B.H.; Landberg, C.E.; Slanetz, P.J.; Giardino, A.A.; Moore, R.; et al. Digital tomosynthesis in breast imaging. Radiology 1997, 205, 399–406. [Google Scholar] [CrossRef]
- Schulz-Wendtland, R.; Preuss, C.; Fasching, P.A.; Loehberg, C.R.; Lux, M.P.; Emons, J.; Beckmann, M.W.; Uder, M.; Mueller-Schimpfle, M. Galactography with Tomosynthesis Technique (Galactomosynthesis)—Renaissance of a Method? Geburtsh Frauenheilk 2018, 78, 493–498. [Google Scholar] [CrossRef] [PubMed]
- Jong, Y.L.; Mijung, J.; Sun, M.K.; Yun, B.L. Galactography Using Digital Breast Tomosynthesis for the Evaluation of Pathologic Nipple Discharge: A Comparison with 2D Synthetic Digital Mammography. J. Korean Soc. Breast Screen. 2019, 16, 60–69. [Google Scholar]
- Moschetta, M.; De Ruvo, V.; Drago, A.; Troiano, N.; Paolicelli, S.; Rubini, G.; Stabile Ianora, A.A.; Telegrafo, M. DBT-galactography: A promising tool for improving the diagnostic workup of nipple discharge. Eur. Radiol. Exp. 2020, 4, 40. [Google Scholar] [CrossRef]
- Olgar, T.; Kahn, T.; Gosch, D. Average glandular dose in digital mammography and breast tomosynthesis. Rofo 2012, 184, 911–918. [Google Scholar] [CrossRef]
- Klein, R.; Aichinger, H.; Dierker, J.; Jansen, J.T.; Joite-Barfus, S.; Sabel, M.; Schulz-Wendtalns, R.; Zoetelief, J. Determination of average glandular dose with modern mammography units for two large groups of patients. Phys. Med. Biol. 1997, 42, 651–671. [Google Scholar] [CrossRef] [PubMed]
- Law, J.; Faulkner, K.; Young, K.C. Risk factors for induction of breast cancer by X-rays and their implications for breast screening. Br. J. Radiol. 2007, 80, 261–266. [Google Scholar] [CrossRef]
- Ohlmeyer, S.; Laun, F.B.; Palm, T.; Janka, R.; Weiland, E.; Uder, M.; Wenkel, E. Simultaneous Multislice Echo Planar Imaging for Accelerated Diffusion-Weighted Imaging of Malignant and Benign Breast Lesions. Investig. Radiol. 2019, 54, 524–530. [Google Scholar] [CrossRef]
- Dang, P.A.; Wang, A.; Senapati, G.M.; Ip, I.K.; Lacson, R.; Khorasani, R.; Giess, C.S. Comparing Tumor Characteristics and Rates of Breast Cancers Detected by Screening Digital Breast Tomosynthesis and Full-Field Digital Mammography. AJR Am. J. Roentgenol. 2020, 214, 701–706. [Google Scholar] [CrossRef] [PubMed]
- Destounis, S.V.; Morgan, R.; Arieno, A. Screening for dense breasts: Digital breast tomosynthesis. AJR Am. J. Roentgenol. 2015, 204, 261–264. [Google Scholar] [CrossRef] [PubMed]
- Prasad, K.N.; Cole, W.C.; Haase, G.M. Radiation protection in humans: Extending the concept of as low as reasonably achievable (ALARA) from dose to biological damage. Br. J. Radiol. 2004, 77, 97–99. [Google Scholar] [CrossRef]
- Fusco, R.; Raiano, N.; Raiano, C.; Maio, F.; Vallone, P.; Raso, M.M.; Setola, S.V.; Granata, V.; Rubulotta, M.R.; Barretta, M.L.; et al. Evaluation of average glandular dose and investigation of the relationship with compressed breast thickness in dual energy contrast enhanced digital mammography and digital breast tomosynthesis. Eur. J. Radiol. 2020, 126, 108912. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.; Woo, O.H.; Shin, H.S.; Cho, K.R.; Seo, B.K.; Choi, G.-Y. Quantitative analysis of radiation dosage and image quality between digital breast tomosynthesis (DBT) with two-dimensional synthetic mammography and full-field digital mammography (FFDM). Clin. Imaging 2019, 55, 12–17. [Google Scholar] [CrossRef]
- Gennaro, G.; Bernardi, D.; Houssami, N. Radiation dose with digital breast tomosynthesis compared to digital mammography: Per-view analysis. Eur. Radiol. 2018, 28, 573–581. [Google Scholar] [CrossRef]
- Shin, S.U.; Chang, J.M.; Bae, M.S.; Lee, S.H.; Cho, N.; Seo, M.; Kim, W.H.; Moon, W.K. Comparative evaluation of average glandular dose and breast cancer detection between single-view digital breast tomosynthesis (DBT) plus single-view digital mammography (DM) and two-view DM: Correlation with breast thickness and density. Eur. Radiol. 2015, 25, 1–8. [Google Scholar] [CrossRef]
- Chevalier, M.; Moran, P.; Ten, J.I.; Fernandez Soto, J.M.; Cepeda, T.; Vano, E. Patient dose in digital mammography. Med. Phys. 2004, 31, 2471–2479. [Google Scholar] [CrossRef]
- Destouet, J.M.; Bassett, L.W.; Yaffe, M.J.; Butler, P.F.; Wilcox, P.A. The ACR’s Mammography Accreditation Program: Ten years of experience since MQSA. J. Am. Coll. Radiol. 2005, 2, 585–594. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | n = 128 | n = 49 |
|---|---|---|
| Age (years) | 46.53 ± 9.4 (27–81) | 48.78 ± 9.5 (28–71) |
| Gender | female | female |
| Discharge side | ||
| Left side | 65 | 23 |
| Right side | 63 | 26 |
| Discharge color | ||
| Yellowish | 66 (51.6%) | 26 (53.1%) |
| Bloody | 39 (30.5%) | 22 (44.9%) |
| Clear | 15 (11.7%) | 1 (2.0%) |
| White | 8 (6.2%) | 0 (0%) |
| Pathologic findings (n = 49) | ||
| Negative | 4 | |
| Intraductal papilloma | 26 | |
| Intraductal carcinoma in situ | 14 | |
| Invasive carcinoma | 5 |
| Projection | kVp | mAs | Times (ms) | CBT (mm) | Compression Force (daN) | AGD (mGy) | |
|---|---|---|---|---|---|---|---|
| CC | FFDM | 28.9 ± 1.16 | 64.19 ± 16.60 | 937.57 ± 321.80 | 48.78 ± 11.38 | 6.22 ± 2.95 | 1.32 ± 0.34 |
| DBT | 29.12 ± 1.03 | 65.09 ± 20.15 | 987.03 ± 362.14 | 48.73 ± 11.22 | 6.34 ± 3.43 | 1.69 ± 0.55 | |
| T values | −1.982 | −0.613 | −2.289 | 0.602 | −0.731 | −9.590 | |
| p values | 0.050 * | 0.541 | 0.024 * | 0.548 | 0.466 | <0.001 ** | |
| ML | FFDM | 28.61 ± 1.14 | 63.59 ± 16.92 | 879.60 ± 304.26 | 45.08 ± 9.94 | 6.46 ± 3.77 | 1.32 ± 0.38 |
| DBT | 28.91 ± 1.08 | 59.43 ± 15.61 | 874.80 ± 290.39 | 44.99 ± 9.94 | 6.37 ± 3.80 | 1.54 ± 0.44 | |
| T values | −3.59 | 2.082 | 0.225 | 0.973 | 0.712 | −6.161 | |
| p values | 0.001 * | 0.039 * | 0.822 | 0.332 | 0.478 | <0.001 * | |
| Reader 1 | Reader 2 | Kappa Value | p Value | ||
|---|---|---|---|---|---|
| CC | FFDM | 4.220 ± 0.793 | 4.200 ± 0.787 | 0.855 | <0.001 |
| DBT | 4.530 ± 0.651 | 4.590 ± 0.633 | 0.814 | <0.001 | |
| ML | FFDM | 4.100 ± 0.821 | 4.100 ± 0.831 | 0.754 | <0.001 |
| DBT | 4.370 ± 0.730 | 4.450 ± 0.719 | 0.813 | <0.001 | |
| Sensitivity | Specificity | PPV | NPV | Efficiency | χ2 | p | ROC Area | |
|---|---|---|---|---|---|---|---|---|
| FFDM | 41/45 (91.1%) | 2/4 (50%) | 41/43 (95.3%) | 2/6 (33.3%) | 43/49 (87.8%) | 5.778 | 0.108 | 0.706 |
| DBT | 42/45 (93.3%) | 3/4 (75%) | 42/43 (97.7%) | 3/6 (50%) | 45/49 (91.8%) | 15.963 | 0.001 * | 0.842 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tao, J.; Liao, H.; Liu, Y.; Peng, Q.; Zhu, W.; Peng, S.; Liu, J.; Chen, L.; Yang, F. Evaluation of Breast Galactography Using Digital Breast Tomosynthesis: A Clinical Exploratory Study. Diagnostics 2021, 11, 2060. https://doi.org/10.3390/diagnostics11112060
Tao J, Liao H, Liu Y, Peng Q, Zhu W, Peng S, Liu J, Chen L, Yang F. Evaluation of Breast Galactography Using Digital Breast Tomosynthesis: A Clinical Exploratory Study. Diagnostics. 2021; 11(11):2060. https://doi.org/10.3390/diagnostics11112060
Chicago/Turabian StyleTao, Juan, Hao Liao, Yuan Liu, Qingsong Peng, Wenying Zhu, Shuyi Peng, Jie Liu, Leqing Chen, and Fan Yang. 2021. "Evaluation of Breast Galactography Using Digital Breast Tomosynthesis: A Clinical Exploratory Study" Diagnostics 11, no. 11: 2060. https://doi.org/10.3390/diagnostics11112060
APA StyleTao, J., Liao, H., Liu, Y., Peng, Q., Zhu, W., Peng, S., Liu, J., Chen, L., & Yang, F. (2021). Evaluation of Breast Galactography Using Digital Breast Tomosynthesis: A Clinical Exploratory Study. Diagnostics, 11(11), 2060. https://doi.org/10.3390/diagnostics11112060







